Abstract
Purpose
The purpose of this study was to investigate the isokinetic, eccentric and isometric hamstring/quadriceps (HQ) ratios in patients before and after ACL reconstruction (ACLR) using bone–patellar tendon grafts and to establish the relationships between HQ ratio and knee function.
Methods
Forty-four patients (mean age of 26.6 years) underwent isokinetic testing of quadriceps and hamstring muscles before and after ACLR and HQ ratios were calculated. Lysholm, IKDC and Cincinnati Scores were used to assess function. Isokinetic concentric and eccentric peak torque (Nm/kg) was measured at three different speeds: 60, 120, and 180°/s. Isometric strength was tested at 30° and 60° of knee flexion.
Results
For the isometric tests, the HQ ratio between the involved and non-involved limb was not different for the ACLD knee (p = 0.28) at 30° knee flexion, but significant at the 60° flexion angle (p = 0.02) and for the ACLR knees at 30° and 60° (p = 0.02). For the isokinetic tests, the ratio between involved and non-involved limb was significant for ACL-deficient knees at both 60 (p = 0.039) and 120°/s (p = 0.05). There were significant differences between limbs for all speeds in ACLR knees (p = 0.0003–0.01). For the eccentric tests, the HQ ratio between the involved and non-involved limbs was not significant for both the ACLD (p = 0.19) and ACLR knees (p = 0.29) at the speed of 60°/s. At 120 and 180°/s, there were significant differences between limbs for both the ACLD (p = 0.02) and ACLR knees (p = 0.003). Linear regression did not reveal significant relationships between Cincinnati, Lysholm, and IKDC scores and HQ ratios in the ACLD (R2 = 0.35, p = 0.58; R2 = 0.34, p = 0.63; R2 = 0.38, p = 0.49). In contrast, there were significant correlations between the Lysholm and IKDC scores and HQ ratios in the ACLR knees (R2 = 0.84, p = 0.002; R2 = 0.86, p = 0.001).
Conclusions
The findings of this study suggest that the HQ ratio in ACLD patients was not a predictor, but an indicator of patient-perceived knee function following ACLR.
Level of evidence
Level IV, case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quadriceps and hamstring muscles apply antagonist forces to the tibia and play an important role in knee stabilization [1]. The hamstring muscles are considered agonists of the anterior cruciate ligament (ACL) and have a protective function at 15°–30° of knee flexion, which is the most common position for an ACL injury [2]. Deficits of hamstring muscle strength in the ACL-deficient knee can be an indicator of poor knee function [3]. Likewise, neurophysiological responses such as quadriceps inhibition can further result in a relatively stronger agonist, facilitating hamstring strength and activation [4,5,6]. It is well known that strength deficits following ACL injury and reconstruction are common and influence the balance between the quadriceps and hamstring muscle groups [7,8,9,10]. In fact, persistent muscle weakness may cause further alterations in the hamstring–quadriceps ratio (HQ ratio) resulting in dynamic instability, and it may increase the risk of further injury [10, 11].
Myer et al. demonstrated decreased hamstring, but not quadriceps strength in female athletes following ACL injury compared to non-injured athletes [12]. In ACL-reconstructed athletes, HQ ratios remained unbalanced in the affected knee [13]. Hohmann et al. have demonstrated that the peak torque strength value of both the quadriceps and hamstring muscles was not a predictor of knee function [14]. However, limb symmetry indices indicated that the HQ ratio might possibly play an important role when considering whether ACL-deficient athletes can cope with knee strength deficits [14]. These findings further support Kannus and Jarvinnen’s study which suggested more than 25 years ago that function is related to the ideal HQ ratio, which is the HQ ratio of the contralateral uninvolved limb [15].
The ratio between hamstring and quadriceps torque has been investigated for more than three decades, and the conventional HQ ratio of 0.6, with a range from 0.5 to 0.75, has been generally accepted as the normative value [7, 16, 17]. If the HQ ratio is higher, the hamstrings have an increased functional capacity to provide stability to the knee which may reduce both anterior translation and anterolateral subluxation [18, 19]. Moreover, it has been suggested by various authors that the HQ ratio is a determinant of knee function and could possibly be used as a parameter to monitor rehabilitation and return to sports following ACL injury [1, 3, 9, 10, 13, 15].
The purpose of this study was to investigate the isokinetic concentric, eccentric and isometric HQ ratios at three speeds using an isokinetic dynamometer in patients before and after ACL reconstruction using bone–patella tendon grafts. The secondary purpose was to investigate the relationships between HQ ratio and knee function.
Methods
Subjects
For this prospective cohort study, volunteers were recruited from the Orthopaedic Sports Injury Clinic. This clinic captures more than 80% of the sporting community in the region with referrals being made through the emergency department, general practitioner, sports physician, physiotherapist, or a direct referral from the various local sporting codes. ACL-deficient patients are usually seen within 4 weeks of the injury, and referred to the physical therapist for prehabilitation. ACL-deficient patients were recruited if they met the inclusion criteria and were followed up through this clinic. Ethical clearance was obtained from both the Human Ethics Research Review Panel of the University (Clearance no. 02/09-74) and the Regional Health District (Clearance no. 02/11).
Patients were included if they had an isolated ACL injury, presented to the clinic within 4 weeks of injury, completed a 12-week physical therapy program, underwent surgical reconstruction between 4 and 6 months following injury, and were aged between 18 and 50 years. The following exclusion criteria were applied: concomitant injuries to the meniscus, medial and lateral collateral ligaments, posterior cruciate ligament, articular cartilage, or any other injury/fracture to the ipsi- or contralateral lower extremity demonstrated on MR imaging or during the initial arthroscopic examination, and coronal plane deformities of more than 10° either varus or valgus on long leg weight-bearing radiographs. Patients with reported intra- and postoperative complications, additional surgical procedures during follow-up or patients who had additional surgical procedures such as realignment procedures were also excluded.
Surgical procedure and rehabilitation
An arthroscopic-assisted ACL reconstruction with the central third of the patellar tendon and using two interference screws was performed as described previously [20]. Post-operatively, the extremity was placed into an ROM brace for 6 weeks. Immediate weight-bearing as tolerated by the patient was started from day 1 post-surgery, and a previously described accelerated rehabilitation protocol was used for all patients [21].
Outcome measures
Knee scoring systems
The Cincinnati Knee Rating System (CKRS) is a validated outcome instrument that is specifically applicable to ACL and all 13 scales were used in this study [22]. The senior author (EH) performed both the clinical examination and interpreted the radiographs using the CKRS criteria.
Instability testing using a KT-2000, all functional hopping tests, the subjective assessment, and activity level scores were performed by an independent research associate at the university’s Performance Laboratory. For the functional hopping tests (single-leg hop, timed hop for distance, and vertical jump) patients were asked to perform each of the hopping tests until three valid attempts were recorded. Each testing session was conducted with the non-involved leg first, followed by the involved extremity, with results averaged over the three attempts.
The Lysholm score is a patient-administered score and was used in this study [19, 23]. The subjective IKDC knee form was used as a patient-oriented questionnaire to assess the symptoms and function of daily living and activities [24, 25].
Muscle strength
Muscle strength was assessed using a Biodex™ Isokinetic Dynamometer (System 3 BIODEX™, Shirley, New York). Isokinetic concentric/concentric and eccentric/eccentric muscle strength, for both the hamstring and quadriceps muscles, was tested at three different speeds (60,120 and 180°/s), and isometric strength was tested at 30° and 60° of knee flexion for the involved and non-involved limbs. A set of five maximal extension and flexion repetitions were performed at the nominated speeds. Peak torque (Nm/kg) generated by both the quadriceps and hamstring muscles of the involved and non-involved limbs were corrected for body weight, and a mean from the three best trials for each test speed and test mode was calculated. For isometric tests, the highest force generated (Nm/kg) during the two knee extension and flexion trials was recorded for subsequent analysis. The HQ ratio was calculated by dividing the means of the peak torque recorded for the hamstrings and quadriceps, respectively, and presented in numerical values.
Testing protocol
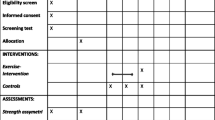
ACL-deficient patients were treated by a physical therapist for 12 weeks. Treatment included ROM exercises, proprioceptive exercises, and anti-inflammatory measures. Patients were tested once the knee effusion had resolved, and full ROM with good subjective quadriceps control was achieved. This typically occurred within 1–2 weeks following the completion of the physical therapy intervention. ACL-reconstructed subjects were tested between 18 and 24 months following ACL reconstruction surgery.
Following a 5-min warm-up session on a Monark™ Friction-Braked Cycle Ergometer at a power output of 50–100 W, the hopping tests were performed as recommended by Barber et al. [22]. The Cincinnati questionnaires as well as the clinical examination were then completed, and the session concluded with the assessment of muscle strength, following a 5-min break between isometric, isokinetic, and eccentric testing to avoid fatigue-related errors.
Statistical analysis
An a priori sample size calculation was performed. The study was powered to detect a 10% difference between limb HQ ratios using a medium effect size (0.5), alpha level of 0.05 and a power level of 0.8, requiring 27 patients. The relationships between HQ ratios and knee function, as assessed by the CKRS, Lysholm and IKDC scores using the above parameters, were able to detect a statistically significant (p = 0.05) correlation of r ≥ 0.50 between the HQ ratio of the involved limb and knee function. The sample size calculation based on these parameters indicated that 37 patients were necessary to achieve 90% statistical power.
Means and standard deviations were calculated for the dependent variables. Data normality was assessed using the Kolmogorov–Smirnov test with Lilliefors corrections. A linear regression model was used to establish the strength of the relationships between the HQ ratios of the involved limbs for all tests, speeds, and knee function as assessed by CKRS, Lysholm, and IKDC scores. The coefficient of correlation “r” was interpreted according to Cohen [26] in the following fashion: 0.0–0.3 weak, 0.31–0.5 moderate, > 0.51 strong.
A level of significance of p < 0.05 was selected in all analyses to limit the chance of type I error to 5%. HQ ratios between the involved and non-involved limbs were analyzed using a two-tailed paired Student’s t test. All analyses were conducted using Systat (version 13; Systat, Chicago, IL, USA).
Results
Forty-four ACL-deficient subjects with a mean age of 26.6 years were included in this study. There were 33 males with a mean age of 26.4 (16–49) years and 11 females with a mean age of 27 (17–38) years. The mean follow-up was 28.5 (+ 4.3) months. The mean Cincinnati score was 62.0 ± 14.5 in the ACL-deficient and 89.3 ± 9.5 in the ACL-reconstructed subjects. The mean Lysholm score was 60.4 ± 19.7 in the ACL-deficient and 91.6 ± 10.1 in the ACL-reconstructed subjects. The mean IKDC score was 53.2 ± 17 in the ACL-deficient and 82.9 ± 9.7 in the ACL-reconstructed subjects.
The HQ ratios for isometric, isokinetic and eccentric muscle strength are shown in Tables 1, 2 and 3. For the isometric tests, the HQ ratio between the involved and non-involved limb was not different for the ACL-deficient knee (p = 0.28) at 30° knee flexion. Significant differences between limbs were observed for the ACL-deficient knees at the 60° flexion angle (p = 0.02) and for the ACL-reconstructed knees at 30° and 60° (p = 0.02) (Table 1). The HQ ratios decreased following ACL reconstruction for the involved and non-involved limbs between 4.3 and 22.5%. These changes were significant for the isometric test at 30° of knee flexion (Table 1).
For the isokinetic tests, the HQ ratio between the involved and non-involved limb was significant for the ACL-deficient knees at both 60 (p = 0.039) and 120°/s (p = 0.05). There were significant differences between limbs for all speeds in the ACL-reconstructed knees (p = 0.0003–0.01) (Table 2). The HQ ratios increased between 7.3 and 25.8% for the involved and non-involved limbs following ACL reconstruction for the tests at both 60 and 120°/s, and was maintained or increased for tests performed at a speed of 180°/s. These changes were only significant at the 120°/s speed (p = 0.02) (Table 2).
For the eccentric tests, the HQ ratio between the involved and non-involved limbs was not significant for both the ACL-deficient (p = 0.19) and ACL-reconstructed knees (p = 0.29) at the speed of 60°/s. At 120 and 180°/s, there were significant differences between the limbs for both the ACL-deficient (p = 0.02) and ACL-reconstructed knees (p = 0.003) (Table 3). The HQ ratios increased marginally between 1.7 and 14% for the involved and non-involved limbs following ACL reconstruction for the tests at all speeds, although these changes were not significant (Table 3).
Linear regression did not reveal significant relationships between Cincinnati, Lysholm, and IKDC scores and HQ ratios in the ACL-deficient knees. The R-squared coefficient of determination was 0.35 (F = 0.89, p = 0.58) for the Cincinnati score, 0.34 (F = 0.84, p = 0.63) for the Lysholm score, and 0.38 (F = 0.987, p = 0.49) for the IKDC score. In contrast, linear regression revealed significant and strong correlations between the Lysholm and IKDC scores and HQ ratios in the ACL-reconstructed knees. The R-squared coefficient of determination was 0.84 (F = 4.971, p = 0.002) for the Lysholm score and 0.86 (F = 5.57, p = 0.001) for the IKDC score. There was a non-significant correlation (R-squared 0.633. F = 1.62, p = 0.18) for the Cincinnati score. Further analysis revealed that these correlations were only significant for all three isokinetic speeds.
Discussion
The most important finding of this study was that the HQ ratios did not predict function in the ACL-deficient knees, but were strong predictors of function in the ACL-reconstructed knees.
However, in the ACL-reconstructed knees, the HQ ratio predicted patient-perceived subjective knee function, with the Lysholm and IKDC scores as the dependent variables. The HQ ratios did not predict knee function with the Cincinnati score. In addition, these correlations were only significant for the isokinetic tests.
A reduction in quadriceps strength in ACL-deficient knees has been observed by many authors [6, 8, 9, 11, 14, 21, 27]. For example, a study by Hohmann et al. demonstrated that quadriceps strength deficits do not appear to significantly influence the perception of knee function in ACL-deficient patients [14]. In fact, the results showed that muscle strength was not an important factor in predicting knee function, but that lower limb symmetry indices were [14]. Despite significant differences between limb HQ ratio in ACL-deficient patients, this study could not demonstrate a correlation with knee function. It appears that neural regulation in the ACL-deficient knees attempts to maintain limb symmetry and a balanced agonist/antagonist ratio to dynamically stabilize unstable joints.
Other studies have suggested that possible reflex and other upper motor neuron-controlled mechanisms, including arthrogenic inhibition of both the involved and non-involved limbs, resulted in downregulation of muscle activation, quadriceps/hamstring co-contractions, and feedforward strategies, ensuring that the HQ ratio remains stable within the normative values [14, 28, 29, 30]. In the current study, the HQ ratio in the ACL-deficient subjects were certainly within the normative values, and this is perhaps a possible prerequisite to perceive the knee as normal [7, 16, 17].
If in fact normal HQ ratios are required in ACL-deficient patients to subjectively perceive knee function as normal, even if both quadriceps and hamstring muscle strength is reduced, we speculate that the neuromuscular system must either downregulate the antagonist or upregulate the agonist. We observed an increase in the HQ ratio following ACL reconstruction, which could be an indication that these mechanisms regulate muscle strength balance. The inevitable increase in quadriceps strength with rehabilitation should have decreased the HQ ratio, which was not observed in our study cohort. These assumptions are supported by St Clair-Gibson et al., who have shown that HQ ratios were similar and normal in both chronic ACL-deficient patients and uninjured individuals [31]. These authors suggested that muscle co-ordination strategies may have been altered to maintain normal limb activity despite muscle strength losses [31]. Similarly, Lee et al. demonstrated a 50% reduction of thigh muscle strength in a group of patients with a chronic ACL tear, but they still observed HQ ratios that were comparable to a normal control group [10].
In a recent meta-analysis, Kim et al. reported that ACL-deficient patients experience an uneven reduction in isokinetic strength of the limb muscles, resulting in a slight increase in HQ ratio in ACL-deficient knees [9]. These increases were mainly observed at a 60° knee flexion. In contrast to Kim et al., we observed an increase in HQ ratios after the ACL was reconstructed [9]. Kim suggested that higher velocities slightly underestimate hamstring strength, because strength is usually measured early after the onset of contraction [9]. One possible explanation for the findings observed in our cohort is that the ACL was reconstructed using a bone–patellar tendon–bone graft, possibly resulting in weakness of the quadriceps muscle. In support of our findings, Zhang et al. has previously demonstrated that the HQ ratio was increased when using patellar tendon grafts for ACL reconstruction [32].
We also observed significant differences between the groups, using the contralateral uninvolved limb as a control, for all speeds and strength tests, as was suggested by Kannus and Jarvinnen [15]. The HQ ratios were higher for almost all velocities and contraction types, although marked systematic variability was observed and were different between contraction types, with HQ ratios still within the reported normal ranges [7, 16, 17]. This was not surprising, since these differences have also been reported by other authors [13, 18, 32].
With surgical reconstruction of the anterior cruciate ligament, static knee stability is restored, and the need to downregulate quadriceps activity reduces with rehabilitation [33,34,35,36]. In our cohort, the HQ ratio increased following ACL reconstruction, clearly favoring the hamstring muscle group, and this was consistent with other studies. Hiemstra et al. demonstrated an increase of the HQ ratio during eccentric contractions for all joint angles and angular velocities [18]. Jordan et al. compared HQ ratios in ACL-reconstructed elite ski racers and reported that ACL-reconstructed athletes had an increased HQ ratio [13]. The authors speculated that significant quadriceps maximal strength deficit was at least partially responsible for this finding. A major limitation of the Jordan study was both the small sample size and the variety of grafts used.
The mechanisms behind strength balances for knee stability are clearly not yet fully understood and are open to speculation. However, similar to other neurogenic-based responses, reflex pathways and neuroregulatory systems require afferent input. There are abundant afferent sensory receptors in the periarticular tissues around the knee that constantly feed information to the higher neurons, allowing alteration and regulation of efferent motor output [37, 38].
Vairo et al. have shown that both neuromuscular and biomechanical adaptations occur to stabilize the knee. These adaptations include co-contraction of quadriceps and hamstring muscles, greater hamstring muscle activation, and increased hip, knee, and ankle joint flexion angles to reduce the vertical ground reaction forces during landing tasks [39]. In an earlier study, we demonstrated that normal knee symmetry indices in ACL-deficient knees are related to function, whereas in ACL-reconstructed knees peak torque values are better correlated with knee function [14]. Interestingly, HQ ratios also play an important role with other knee pathologies. For example, Guney et al. demonstrated a significant relationship between the Kujala score and HQ ratios in patients with patellofemoral pain [40]. Müller et al. showed that HQ ratios following autologous chondrocyte implantation (ACI) in the patellofemoral joint are significantly different to those observed in patients who underwent condylar ACI [41]. These consistent patterns of neuromuscular adaptations seem to have evolved to protect the knee from mechanical overloads.
This study has various limitations. The HQ ratios were calculated from the peak torque values at different velocities and contraction types, and these ratios can vary depending on angular velocity and knee flexion angles. To reduce confounders and sampling bias, we used strict inclusion and exclusion criteria, resulting in a smaller sample size. However, an a priori sample size was performed to minimize the probability of type II error. As a result, the external validity of this study is limited, and caution should be exercised before generalizing these results to patients with concomitant injuries such as meniscal tears, other associated ligamentous injuries or chondral defects.
Conclusion
The findings of this study suggest that the hamstring/quadriceps ratio in ACL-deficient patients was not a predictor of knee function. However, it was an indicator of knee function when using patient-centered subjective outcome scores following ACL reconstruction. Moreover, the HQ ratios increased for all velocities and contraction types following reconstruction surgery, but those ranges were within normal values for both ACL-deficient and ACL-reconstructed knees.
References
Shelbourne KB, Torry MR, Pandy MG (2005) Effect of muscle compensation on knee instability during ACL-deficient gait. Med Sci Sports Exerc 37:642–648
More RC, Karras BT, Neiman R, Fritschy D, Woo SL, Daniel DM (1993) Hamstrings—an anterior cruciate ligament protagonist: an in vitro study. Am J Sports Med 21(2):231–237. https://doi.org/10.1177/036354659302100212
Tsepis E, Vagenas G, Giakas G, Georgoulis A (2004) Hamstring weakness as an indicator of poor knee function in ACL-deficient patients. Knee Surg Sports Traumatol Arthrosc 12(1):22–29. https://doi.org/10.1007/s00167-003-0377-4
Palmieri RM, Weltman A, Edwards JE, Tom JA, Saliba EN, Mistry DJ et al (2005) Pre-synaptic modulation of quadriceps arthrogenic muscle inhibition. Knee Surg Sports Traumatol Arthrosc 13:370–376. https://doi.org/10.1007/s00167-004-0547-z
Palmieri-Smith RM, Thomas AC (2009) A neuromuscular mechanism of osteoarthritis associated with ACL injury. Exerc Sport Sci Rev 37:147–153. https://doi.org/10.1097/JES.0b013e3181aa6669
Snyder-Mackler L, Delitto A, Bailey SL, Stralka SW (1995) Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. J Bone Jt Surg Am 77:1166–1173
Aagaard P, Simonsen EB, Magnusson SP, Larsson B, Dyhre-Poulsen P (1998) A new concept for isokinetic hamstring: quadriceps muscle strength ratio. Am J Sports Med 26:231–237. https://doi.org/10.1177/03635465980260021201
de Jong SN, van Caspel DR, van Haeff MJ, Saris DB (2007) Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy 23:21–28. https://doi.org/10.1016/j.arthro.2006.08.024
Kim HJ, Lee JH, Ahn SE, Park MJ, Lee DH (2016) Influence of anterior cruciate ligament tear on thigh muscle strength and hamstring-to-quadriceps ratio: a meta-analysis. PLoS One 11(1):e0146234. https://doi.org/10.1371/journal.pone.0146234
Lee DH, Lee JH, Jeong HJ, Lee SJ (2015) Lack of correlation between dynamic balance and hamstring-to-quadriceps ratio in patients with chronic anterior cruciate ligament tears. Knee Surg Relat Res 27:101–107. https://doi.org/10.5792/ksrr.2015.27.2.101
Williams GN, Buchanan TS, Barrance PJ, Axe MJ, Snyder-Mackler L (2005) Quadriceps weakness, atrophy and activation failure in predicted non-copers after anterior cruciate ligament injury. Am J Sports Med 33:402–407. https://doi.org/10.1177/0363546504268042
Myer GD, Ford KR, Barber-Foss KD, Liu C, Nick TG, Hewett TE (2009) The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med 19:3–8. https://doi.org/10.1097/JSM.0b013e318190bddb
Jordan MJ, Aagaard P, Herzog W (2015) Rapid hamstrings/quadriceps strength in ACL-reconstructed elite Alpine ski racers. Med Sci Sports Exerc 47(1):109–119. https://doi.org/10.1249/MSS.0000000000000375
Hohmann E, Bryant A, Tetsworth K (2016) Strength does not influence knee function in the ACL-deficient knee but is a correlate of knee function in the and ACL-reconstructed knee. Arch Orthop Trauma Surg 136(4):477–483. https://doi.org/10.1007/s00402-015-2392-6
Kannus P, Jarvinen M (1990) Nonoperative treatment of acute knee ligament injuries. Review with special reference to indications and methods. Sports Med 9:244–260
Coombs R, Garbutt G (2002) Developments in the use of the hamstring/quadriceps ratio for the assessment of muscle balance. J Sports Sci Med 1(3):56–62
Westing SH, Seger JY, Karlson E, Ekblom B (1988) Eccentric and concentric torque-velocity characteristics of the quadriceps femoris in man. Eur J Appl Physiol Occup Physiol 58:100–104
Hiemstra LA, Webber S, MacDonald P, Kriellaars DJ (2004) Hamstring and quadriceps strength balance in normal and hamstring anterior cruciate ligament reconstructed subjects. Clin J Sports Med 14(5):274–280
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154
Hohmann E, Bryant A, Tetsworth K (2010) Tunnel positioning in anterior cruciate ligament reconstruction: how long is the learning curve? Knee Surg Sports Traumatol Arthrosc 18:1576–1582. https://doi.org/10.1007/s00167-010-1183-4
Hohmann E, Tetsworth K, Bryant A (2011) Physiotherapy-guided versus home-based, unsupervised rehabilitation in isolated anterior cruciate injuries following surgical reconstruction. Knee Surg Sports Traumatol Arthrosc 19:1158–1167. https://doi.org/10.1007/s00167-010-1386-8
Barber SD, Noyes FR, Mangine RE, McCloskey JE, Hartman W (1990) Qualitative assessment of functional limitations in normal and anterior cruciate ligament deficient knees. Clin Orthop 255:204–214
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scacle for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37(5):890–897. https://doi.org/10.1177/0363546508330143
Higgins LD, Taylor MK, Park D, Ghohadra N, Marchant M, Pietrobon R, Cook C (2007) International Knee Documentation Committee. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Jt Bone Spine 74:594. https://doi.org/10.1016/j.jbspin.2007.01.036
Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ (2006) International Knee Documentation Committee. The international knee documentation committee subjective knee evaluation form. Am J Sports Med 34(1):128–135. https://doi.org/10.1177/0363546505280214
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates Inc. Publishers, Mahwah
Hurd WJ, Axe MJ, Snyder-Mackler L (2008) A 10 year prospective trial of a patient management algorithm and screening examination for highly active individuals with ACL injury. Part II: determinants of knee stability. Am J Sports Med 36:48–56. https://doi.org/10.1177/0363546507308191
Bryant AL, Newton RU, Steele J (2009) Successful feed-forward strategies following ACL injury and reconstruction. J Electromyogr Kinesiol 19:988–997. https://doi.org/10.1016/j.jelekin.2008.06.001
Hart JA, Pietrosimone B, Hertel J, Ingersoll CD (2010) Quadriceps activation following knee injuries: a systematic review. J Athl Train 45:87–97
Swanik CB, Covassin T, Stearne DJ, Schatz P (2007) The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med 35:943–948. https://doi.org/10.1177/0363546507299532
St Clair Gibson A, Lambert MI, Durandt JJ, Noakes TD (2000) Quadriceps and hamstring peak torque ratio changes in persons with chronic anterior cruciate ligament deficiency. J Orthop Sports Phys Ther 30:418–427. https://doi.org/10.2519/jospt.2000.30.7.418
Zhang LQ, Nuber GW, Bowen MK, Koh JL, Butler JP (2002) Multiaxis muscle strength in ACL deficient and reconstructed knees: compensatory mechanism. Med Sci Sports Exerc 34:2–8
Ardern CL, Pizzari T, Wollin MR, Webster KE (2015) Hamstring strength in professional football (soccer) players in Australia. J Strength Cond Res 29(4):997–1002. https://doi.org/10.1519/JSC.0000000000000747
Myer GD, Paterno MV, Ford KR, Hewett TE (2008) Neuromuscular training techniques to target deficits before return to sports after anterior cruciate ligament reconstruction. J Strength Cond Res 22(3):987–1014. https://doi.org/10.1519/JSC.0b013e31816a86cd
Cappellino F, Paolucci T, Zangrando F, Iosa M, Adriani E, Mancini P, Bellelli A, Saraceni VM (2012) Neurocognitive rehabilative approach effectiveness after anterior cruciate ligament reconstruction with patella tendon. A randomized controlled trial. Eur J Phys Rehabil Med 48(1):17–30
Risberg MA, Holm I, Myklebust G, Engebretsen L (2007) Neuromuscular training versus strength training during the first 6 months after anterior cruciate ligament reconstruction. Phys Ther 87:737–750. https://doi.org/10.2522/ptj.20060041
Baxendale RH, Ferrell WR, Wood L (1988) Responses of quadriceps motor units to mechanical stimulation of the knee joint receptors in the decerebrate cat. Brain Res 453:150–156
Dhaher YY (2004) Joint-afferent-mediated muscle activations yield a near-maximum torque response of the quadriceps. J Neurosci Methods 15(133):1–17
Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM (2008) Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 16(1):2–14. https://doi.org/10.1007/s00167-007-0427-4
Guney H, Yuksel I, Kaya D, Doral MN (2016) Correlation between quadriceps to hamstring ratio and functional outcomes in patellofemoral pain. Knee 23:610–615. https://doi.org/10.1016/j.knee.2016.04.004
Müller S, Hirschmüller A, Ergelet C, Beckman NA, Kreuz PC (2015) Significantly worse isokinetic hamstring–quadriceps ratio in patellofemoral compared to condylar defects 4 years after autologous chondrocyte implantation. Knee Surg Sports Traumatol Arthrosc 23(8):2151–2158. https://doi.org/10.1007/s00167-014-2964-y
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hohmann, E., Tetsworth, K. & Glatt, V. The hamstring/quadriceps ratio is an indicator of function in ACL-deficient, but not in ACL-reconstructed knees. Arch Orthop Trauma Surg 139, 91–98 (2019). https://doi.org/10.1007/s00402-018-3000-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3000-3