Abstract
Objectives
To evaluate the methods and the outcomes of Gustilo type III open distal tibial and tibial shaft fractures with severe anterior and medial soft-tissue injuries, treated with posterolateral minimally invasive plate osteosynthesis (MIPO) technique.
Methods
From May 2015 to May 2016, 10 patients with Gustilo type III open distal tibial and tibial shaft fractures with severe anterior and medial soft-tissue injuries (Gustilo–Anderson classification IIIA, 6; IIIB, 4) were treated with staged protocol using posterolateral minimally invasive plate osteosynthesis (MIPO) technique. The initial wound lavage, debridement, and application of a spanning external fixator were performed within 24 h and the mean interval from injury to definitive surgical treatment was 12.8 (range 4–21) days. An additional bone graft was performed in two patients when definitive internal fixation was performed. All patients were followed to union. Postoperative radiographs, postoperative complications, bone union, ankle joint motion, and limb functional outcome information of AOFAS ankle–hindfoot score were recorded.
Results
The mean follow-up period was 17.8 (range 12–26) months. The mean interval to bony union was 25.8 (range 20–40) weeks. Bone union was achieved in all cases. There were no complications, such as incision breakdown, deep infection, or impingement of the flexor hallucis longus tendon. The average AOFAS score was 90 (range 83–96). In ten patients, two patients had a superficial wound infection and another one patient showed a 6° varus deformity.
Conclusions
Staged treatment using MIPO technique through a posterolateral approach is a reasonable and safe treatment option for open distal tibial and tibial shaft fractures, especially Gustilo type III with severe anterior and medial soft-tissue injuries. However, it should have a higher level of research evidence in more patients to confirm the safety of the clinical application of this technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gustilo type III open distal tibial and tibial shaft fractures are generally a result of high-energy trauma that often associated with soft-tissue injuries, especially in the anterior or medial side of the tibia [1, 2]. Complications such as failure to unite, wound site problems, deep infection, and ankle joint stiffness have been common in these fractures [3]. Recently staged treatment with MIPO technique for open distal tibial and tibial shaft fractures using an anteromedial or anterolateral approach has been widely used, with satisfactory clinical outcomes, as this method has less soft-tissue disruption with preservation of fracture haematoma and blood supply to the bone fragments [4, 5]. However, anterior approach would increase additional damage to the subcutaneous tissues of the anterior and medial tibial and lack of adequate soft-tissue coverage overlying the plate fixation [6,7,8]. In recent years, a posterolateral MIPO technique has been reported by Kritsaneephaiboon et al. [9] and Yamamotoa et al. [10] in cases with anterior soft-tissue problem. The advantage of this approach is that it protects the subcutaneous tissues of the anterior and medial tibia and enables abundant soft-tissue coverage overlying the plate fixation. This study evaluated the staged treatment using posterolateral MIPO technique in patients with Gustilo type III open distal tibial and tibial shaft fractures, and analyzed the treatment results.
Patients and methods
From August 2015 to December 2016, ten cases of Gustilo III open distal tibial and tibial shaft fractures were treated by staged treatment using minimally invasive plate osteosynthesis (MIPO) technique through a posterolateral approach at the Qingpu Branch of Zhongshan Hospital (Shanghai, China). There were six males and four females with an average age of 43 (range 24–68) years. The cause of the fracture was 4 traffic accidents, 3 falls from a height, and 2 machine stretch/contusion injuries. All patients had an associated fibular fracture. In accordance with the Gustilo–Anderson classification, six cases were classified as IIIA and four cases as IIIB. According to the AO/OTA classification, seven cases were classified as A2 and three cases as A3. The treatment involved two or three stages, according to the skin/soft-tissue condition and size of the bone defect.
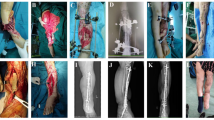
Stage treatment
At the initial treatment, Gustio type IIIA wound injury was managed with direct debridement and suture in six cases. With Gustio type IIIB wound injury, relaxation suture was made in two cases. With another two cases of Gustio type IIIB wound injury, thorough debridement and vacuum sealing drainage (Wuhan VSD Medical Science & Technology Co., Ltd., Wuhan, China) were performed in the first-stage treatment. After the removal of negative pressure on VSD devices, skin graft was performed. In all cases, temporizing ankle-spanning external fixator intervention (Chuangsheng Medical Devices (China) Co., Ltd., Changzhou, China) was performed within 8 h. The fibula was plated depending on the fracture pattern and soft-tissue injury.
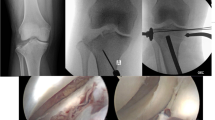
After the initial treatment and a delay for a mean period of 18 days (range 4–42 days), when the status of soft tissue was properly stabilized enough for soft-tissue reconstruction, with no sign of infection, definitive surgical treatment was performed. With the patient under combined spinal and epidural anesthesia, the patient is placed on the operating table in the floating position with external fixator to maintain alignment and reduction. The following surgical techniques was used according to Kritsaneephaiboon’s report [9]. First, a 2.5 cm distal skin incision was made at the midpoint between the posterior border of the distal fibula and lateral boarder of Achilles tendon, beginning at the level of the tip of the distal fibular and extending proximally to the distal fibular shaft (Fig. 1a). Dissection is carried through the subcutaneous tissues to the level of the deep fascia, avoiding damaging sural nerve and lesser saphenous vein which are located under the superficial fascial layer. Exposing the posterior surface of distal tibia was achieved by separating the interval between the peroneal tendons laterally and the muscle of the flexor hallucis longus (FHL) medially. Through a clear dissection of the FHL along its outer edge, the entire posterior portion of the tibial surface was exposed by retracting this muscle medially, which also protected the posterior tibial artery and tibial nerve. Second. a 2–3-cm proximal skin incision at the posteromedial border of the tibial shaft was made according to the location of the proximal screw (Fig. 1b). The posterior surface of mid-tibia was exposed by laterally retracting the soleus. A submuscular extraperiosteal tunnel was created by passing a tunnelling instrument from the distal to the proximal incisions. To avoid injury to the posterior tibial artery and tibial nerve at the medial aspect of the mid-tibia, the tunnelling instrument was passed along the posterior surface of the tibia. Third, 10 holes or 13 holes of Medial Distal Tibia Locking Plate (Double Medical Technology Co., Ltd., Xiamen, China) were fixed directly to the posterior surface of the tibia. At least three bicortical screws were required to placed to the distal and proximal end of the plate (Fig. 2).
a 36-year-old man sustained a left open distal tibia fracture (AO/OTA type A3, Gustilo–Anderson classification IIIB). b Thorough debridement were performed, and then, holes were punched around the wound with a shape blade and relaxation suture was gained finally. Then, ankle-spanning bridge external fixator was applied within 8 h. c When the wound healed with no sign of infection after 16 days, distal tibial fracture was treated with minimally invasive plate osteosynthesis (MIPO) technique through posterolateral approach. d Anteroposterior and lateral radiographs at 12 months of follow-up showing fracture union. AO/OTA: AO/Orthopaedic Trauma Association
a–c 24-year-old man sustained a left open distal tibial and fibula fracture (AO/OTA type A3, Gustilo–Anderson classification IIIA). d Intraoperative retention of external fixation:retaining the external fixator helps to maintain the length of the affected limb with the initial stability and facilitates the reduction of the tibial. e Distal incision: reduction and fixation of both fibula and tibial fractures can be made through one incision. Incision was made between the posterior margin of the fibula and the lateral margin of the Achilles tendon. In the superficial layer of soft tissue, avoiding damaging the gastrocnemius and small saphenous veins should be attended, while attention to protecting the peroneal artery should be noted in the deep layer of soft tissue. The fibula was fixed through the gap between the peroneal muscle and extensor digitorum longus, while the distal tibial was visualized and fixed between the long peroneal tendon and flexor halluces. f Proximal incision: the proximal incision was made according to the location of the proximal screw at the posteromedial border of the tibial. g Reduction order: the fibula was fixed first to maintain the length and alignment of the tibial and the tibial was indirectly restored through anatomical reduction of fibula. When making submuscular tunnel, a periosteal stripper was passed close to the posterior surface of the tibia and periosteum from the distal to the proximal incisions and it should be slow and accurate to avoid rough operation and damaging the peripheral vessels and nerves. h When the plate position was determined, lag screw technique was applied to correct the residual anterior and posterior angle deformity of tibial fracture. i, j Anteroposterior and lateral radiographs after operation. Pay attention to the length of the plate and the proximal end should be located below the bifurcation of the anterior tibial artery and posterior tibial artery
After plate fixation, a bone graft was performed in two cases with a severe metaphyseal bone defect. Autogenous iliac bone was used in both cases.
Postoperative management
Physical therapy begins on the second-to-fifth postoperative day. 1–2 weeks after surgery, partial weight bearing is encouraged depending on reconstruction stability. All patients were evaluated radiographically and clinically. Radiographic evaluation was performed using anteroposterior (AP) and lateral radiographs at the time of patient admission, immediately postoperatively and after at least 1–12 months of follow-up. We evaluated time to union, range of motion of the ankle, wound healing, complications, American Orthopaedic Foot and Ankle Society (AOFAS), ankle–hindfoot score. We defined union as > 50% visible bridging callus across the fracture on the conventional radiographs and no movement or tenderness was present. In addition, an angular deformity was defined as angulation, when there was > 5° angulation. Shortening was defined as > 10 mm shortening compared to the unaffected side. Each angulation was evaluated using the method reported by Milner [11].
Results
10 patients got followed up for 12–26 months with average 17.8 months. At the final follow-up visit, all the fractures showed clinical and radiographic evidence of union. The average time to bone union was 25.8 weeks (range 20–40 weeks). An additional bone graft was required for two cases with a severe metaphyseal bone defect.
The average AOFAS score was 90 (range 83–96) at the last follow-up of patients. The deformities were evaluated radiographically using the picture archiving and communication system measurement tools. During the follow-up period, only 1 deformity was found: a 6° varus deformity. Neither tibial shortness nor restriction of range of motion was observed. No patient showed evidence of neurovascular injury (Table 1).
Superficial wound infections happened in two patients, which resolved with antibiotic treatment orally and care of screw sites. No other complications such as deep infection, incision breakdown, or FHL tendon impingement were observed (Table 1).
Discussion
Treating Gustilo III open distal tibial and tibial shaft fractures resulting from high-energy trauma with severe soft tissue compromise, which remains controversial and challenging for orthopaedic surgeons [12, 13]. The traditional treatment using an external fixator, open reduction, and rigid internal fixation in these fractures does not yield good results. Kellam and Waddell reported that 53% of patients with high-energy compressive fractures had good function compared with 84% in low-energy injuries [14]. Dillin and Slabaugh also advocated rigid internal fixation only for lower energy injuries when they had an alarming 55% infection rate in their series of 11 high-energy trauma patients [15]. Since these reports, reducing soft-tissue damage and minimally invasive operations have become popular. Intramedullary nailing is an alternative minimal invasive treatment for tibial fractures [16]. However, there are some difficulties for treatment of distal tibial fractures and open tibial fractures. The distal tibial fracture line is often extended to the tibial articular surface, and the distal locking screw has a risk of splitting the articular surface [17]. In addition, the soft-tissue injury in this group is mostly in the medial tibial, and the rate of distal locking nail infection is higher [18]. External fixation is another acceptable technique in open tibial fractures because of the advantages of less secondary iatrogenic injury and ease of application [19]. However, the stability provided by the external fixation cannot compared to that created by plate fixation. In addition, it is difficult to insert Schanz screws when distal tibial length is insufficient and dangerous when the fracture line reaches the distal tibial surface. Although ankle-spanning systems can be applied in these cases, loss of reduction commonly occurred in patients treated with spanning frames. Post-operation nail tract infection and ankle stiffness are also common in these patients [20, 21].
A number of studies have reported good results with an MIPO technique using both anteromedial and anterolateral approaches in treating Gustilo III open distal tibial and tibial shaft fractures [8, 22]. However, an open wound with severe soft-tissue injury is usually found in the anterior or medial side of the tibia and anterior approach is not suitable for these cases of distal tibia and tibal shaft fractures. Thus using MIPO through a posterolateral approach for distal tibial and tibial shaft fractures has been first reported by Kritsaneephaiboon in terms of anatomical safety and a case with an excellent outcome [9]. In addition, Yamamotoa reported five cases with no complication [10]. In this study, we further described ten patients of Gustilo III open distal tibial and tibial shaft fractures with severe anterior and medial soft-tissue injuries, treated by MIPO technique through a posterolateral approach. Clinical outcomes were satisfactory, and we gained experience using this technique.
In our experience, the external fixation was strongly recommended to maintain tibial alignment during surgery before tunnelling and plate insertion. Maintaining tibial alignment was not only conductive to preoperative fracture reduction, but also avoided to damage neurovascular structures when submuscular tunnel and plate insertion were performed. In addition, a floating position with the following advantages was suggested for performing posterolateral MIPO technique. It was easy for fracture reduction in the lateral position, while, in the prone position, it was quite convenient for plate insertion and fixation.
Two types of proximal incision methods were used by Kritsaneephaiboon et al [9] and Yamamotoa et al [10], respectively. A proximal incision was made about one finger breadth below the posterolateral border of mid-fibula by Kritsaneephaiboon et al. Another proximal incision described by Yamamotoa et al. is located at the posteromedial border of the tibia. When using the former, the posterior surface of mid-tibia was exposed by splitting between peroneal muscles laterally and FHL medially. The posterior tibial artery and the tibial nerve were very close to the plate at the proximal incision. In the latter, the posterior surface of mid-tibia was easily reached without splitting soft tissues and without retracting neurovascular bundles. Our methods were consistent with Yamamotoa’s, and in all ten cases, the fracture site was fixed without any complications related neurovascular injury. Therefore, we believe that Ogawa’s posterolateral approach is safe.
Complications related to soft-tissue injury were minimized using the posterolateral MIPO method. Satisfactory bony union was achieved in all our patients without delayed union or non-union. In two patients with a severe bone defect, a staged bone graft was performed. Here, the average time to bone union was 25.8 weeks, which was comparable to that reported by others on bone union of open distal tibial and tibial shaft fractures with medial or anterior lateral MIPO technique [23, 24]. We consider that the possible reason is that damage to soft tissues and blood supply on the posterior aspect of the distal tibia is less extensive, and no additional invasive procedures on the medial and anterior aspect were performed and LCPs provide good stability for distal tibial fractures. Our results indicated that posterolateral MIPO method was a biological and effective technique for distal tibial and tibial shaft fractures, especially with critical anterior and medial soft-tissue injury.
Another advantage of this approach was tibial and fibula fractures can be performed through a single distal incision. The traditional double long incisions for distal tibial and fibula fractures can disturb the skin circulation and the rate incision complication is increased if the distance between the medial and lateral incision is < 7cm [25]. Howard et al [26] reported soft-tissue complications in 4 of 46 fractures when the mean distance between incisions was 5.9 cm. Therefore, we suggest that a single incision on the posterolateral side provides sufficient visualization and decreases postoperative wound site complications.
However, compared to the anterior lateral approach, posterolateral incisions enable a limited visualization of the distal tibia joint line and Chaput’s tubercle fractures. Thus, it is not applicable for fractures involved articular surface. Furthermore, posterolateral incisions on the distal tibia also have a risk of cutting the sural nerve and lesser saphenous vein, which are in the superficial layer and run distally from the lateral border of the Achilles tendon to the anterolateral aspect of the foot. Careful dissection is essential to minimize potential complications. Considering these disadvantages, we do not recommend the posterolateral MIPO for routine treatment of Gustilo III open distal tibial or tibial shaft fractures.
Conclusion
In conclusion, our results suggest that complications, such as soft-tissue necrosis and infection, were minimized using staged treatment with MIPO technique through a posterolateral approach. A staged treatment using the MIPO technique through posterolateral approach should be a safe option for fixing Gustilo III open distal tibial and tibial shaft fractures with severe anterior and medial soft-tissue injuries.
References
Lua J, Tan VH, Sivasubramanian H, Kwek E (2017) Complications of open tibial fracture management: risk factors and treatment. Malays Orthop J 11:18–22. https://doi.org/10.5704/MOJ.1703.006
Penn-Barwell JG, Myatt RW, Bennett PM, Sargeant ID (2015) Medium-term outcomes following limb salvage for severe open tibia fracture are similar to trans-tibial amputation. Inj Int J Care Inj 46:288–291. https://doi.org/10.1016/j.injury.2014.12.004
Sheean AJ, Krueger CA, Napierala MA, Stinner DJ, Hsu JR (2014) Evaluation of the mangled extremity severity score in combat-related type III open tibia fracture. J Orthop Trauma 28:523–526. https://doi.org/10.1097/BOT.0000000000000054
Shon OJ, Park CH (2012) Minimally invasive plate osteosynthesis of distal tibial fractures: a comparison of medial and lateral plating. J Orthop Sci 17:562–566. https://doi.org/10.1007/s00776-012-0241-9
Vidovic D, Matejcic A, Ivica M, Jurisic D, Elabjer E, Bakota B (2015) Minimally-invasive plate osteosynthesis in distal tibial fractures: Results and complications. Inj Int J Care Inj 46(Suppl 6):S96–S99. https://doi.org/10.1016/j.injury.2015.10.067
Mushtaq A, Shahid R, Asif M, Maqsood M (2009) Distal tibial fracture fixation with locking compression plate (LCP) using the minimally invasive percutaneous osteosynthesis (MIPO) technique. Eur J Trauma Emerg Surg 35:159–164. https://doi.org/10.1007/s00068-008-8049-1
Beale BS, McCally R (2012) Minimally invasive plate osteosynthesis: tibia and fibula. Vet Clin North Am Small Anim Pract 42:1023–1044. https://doi.org/10.1016/j.cvsm.08.001
Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL (2009) Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg 129:649–659. https://doi.org/10.1007/s00402-006-0219-1
Kritsaneephaiboon A, Vaseenon T, Tangtrakulwanich B (2013) Minimally invasive plate osteosynthesis of distal tibial fracture using a posterolateral approach: a cadaveric study and preliminary report. Int Orthop 37:105–111. https://doi.org/10.1007/s00264-012-1712-5
Yamamoto N, Ogawa K, Terada C, Okazaki Y, Munetomo K, Noda T, Ozaki T (2016) Minimally invasive plate osteosynthesis using posterolateral approach for distal tibial and tibial shaft fractures. Inj Int J Care Inj 47:1862–1866. https://doi.org/10.1016/j.injury.2016.06.017
Milner SA (1997) A more accurate method of measurement of angulation after fractures of the tibia. J Bone Jt Surg Br 79:972–974
Muhlhausser J, Winkler J, Babst R, Beeres F (2017) Infected tibia defect fractures treated with the Masquelet technique. Medicine (Baltimore) 96:e6948. https://doi.org/10.1097/MD.0000000000006948
Thakore RV, Francois EL, Nwosu SK, Attum B, Whiting PS, Siuta MA, Benvenuti MA, Smith AK, Shen MS, Mousavi I, Obremskey WT, Sethi MK (2017) The Gustilo–Anderson classification system as predictor of nonunion and infection in open tibia fractures. Eur J Trauma Emerg Surg 43:651–656. https://doi.org/10.1007/s00068-016-0725-y
Kellam JF, Waddell JP (1979) Fractures of the distal tibial metaphysis with intra-articular extension–the distal tibial explosion fracture. J Trauma 19:593–601
Dillin L, Slabaugh P (1986) Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma 26:1116–1119
De Giacomo AF, Tornetta PR (2016) Alignment after intramedullary nailing of distal tibia fractures without fibula fixation. J Orthop Trauma 30:561–567. https://doi.org/10.1097/BOT.0000000000000637
Vallier HA, Cureton BA, Patterson BM (2011) Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 25:736–741. https://doi.org/10.1097/BOT.0b013e318213f709
Vallier HA, Cureton BA, Patterson BM (2012) Factors influencing functional outcomes after distal tibia shaft fractures. J Orthop Trauma 26:178–183. https://doi.org/10.1097/BOT.0b013e31823924df
Sun LJ, Yu XB, Dai CQ, Hu W, Guo XS, Chen H (2014) A randomised prospective study of two different combined internal and external fixation techniques for distal tibia shaft fractures. Inj Int J Care Inj 45:1990–1995. https://doi.org/10.1016/j.injury.2014.10.044
Golubovic Z, Stojiljkovic P, Macukanovic-Golubovic L, Milic D, Milenkovic S, Kadija M, Matovic Z, Turkovic G, Radenkovic M, Visnjic A, Golubovic I, Stojanovic S, Vidic G, Mitkovic M (2008) External fixation in the treatment of open tibial shaft fractures. Vojnosanitetski Pregled 65:343–348
Beltsios M, Savvidou O, Kovanis J, Alexandropoulos P, Papagelopoulos P (2009) External fixation as a primary and definitive treatment for tibial diaphyseal fractures. Strateg Trauma Limb Reconstr 4:81–87. https://doi.org/10.1007/s11751-009-0062-3
Collinge C, Kuper M, Larson K, Protzman R (2007) Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma 21:355–361. https://doi.org/10.1097/BOT.0b013e3180ca83c7
Hasenboehler E, Rikli D, Babst R (2007) Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Inj Int J Care Inj 38:365–370. https://doi.org/10.1016/j.injury.2006.10.024
Hazarika S, Chakravarthy J, Cooper J (2006) Minimally invasive locking plate osteosynthesis for fractures of the distal tibia–results in 20 patients. Inj Int J Care Inj 37:877–887. https://doi.org/10.1016/j.injury.2006.06.002
Unlu S, Catma MF, Bilgetekin YG, Altay M, Ates Y, Bozkurt M, Kapicioglu MI (2015) Minimally invasive plate osteosynthesis of distal tibia and fibular fractures through a single distal anterolateral incision. J Foot Ankle Surg 54:1081-1084. https://doi.org/10.1053/j.jfas06.009
Howard JL, Agel J, Barei DP, Benirschke SK, Nork SE (2008) A prospective study evaluating incision placement and wound healing for tibial plafond fractures. J Orthop Trauma 22:299–305. https://doi.org/10.1097/BOT.0b013e318172c811 (discussion 305-6)
Acknowledgements
This study was supported by the Grants from Key Project of Shanghai Health Bureau for Kkeletal Trauma (ZK2015B27).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest regarding this paper.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki. This study was conducted with approval from the Ethics Committee of the Qingpu Branch of Zhongshan Hospital. Written informed consent was obtained from all participants.
Rights and permissions
About this article
Cite this article
He, X., Hu, C., Zhou, K. et al. Clinical and radiological outcome of Gustilo type III open distal tibial and tibial shaft fractures after staged treatment with posterolateral minimally invasive plate osteosynthesis (MIPO) technique. Arch Orthop Trauma Surg 138, 1097–1102 (2018). https://doi.org/10.1007/s00402-018-2950-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2950-9