Abstract
Introduction
The aim of the study was to make a prospective comparison of the radiological and clinical outcomes of patients undergoing single-bundle and double-bundle anterior cruciate ligament (ACL) reconstruction.
Method
This prospective, case-controlled study included 65 patients, separated into 2 groups as 33 patients undergoing single bundle (SB), and 32 patients undergoing double bundle (DB) ACL reconstruction. The patients were evaluated clinically using the International Knee Documentation Committee (IKDC) and the Lysholm knee scores. Stability was evaluated with the KT-1000 Arthrometer Measurement, the Lachman and pivot shift tests. Magnetic resonance images (MRI) at 1 and 5 years postoperatively were evaluated by a musculoskeletal radiologist. All the operations were performed by a single surgeon and the clinical evaluations were made by an independent researcher.
Results
Evaluation was made of a total of 53 patients (SB: 28, DB: 25). No statistically significant difference was determined between the groups regarding the postoperative IKDC and Lysholm scores. The pivot shift tests were negative in the DB group and positive in two patients of the SB group. The Lachman test was negative in all the patients. No significant difference was determined between the groups. No statistically significant difference was determined between the two groups in respect of the arthrometer measurements. In the SB group, revision surgery was performed in two patients due to graft failure. No graft failure findings were determined in the DB group, and no statistically significant difference was determined between the groups in respect of graft failure. On the MRIs taken at 1 year postoperatively, the ACL was seen to be hyperintense in 16 patients in the DB group and 6 patients in the SB group (p = 0.004). On the 5-year MRIs, ACL hypointensity could not be seen in three patients of the SB group and two of the DB group, with no difference determined between the groups (p > 0.05).
Conclusion
In the 5-year follow-up period, no difference was determined between patients undergoing SB ACL reconstruction and those undergoing DB ACL reconstruction regarding clinical scores, knee stability, and MRI findings, but graft maturation occurs later the patients undergoing DB reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) injury is frequently seen in young, active individuals [1]. The current standard treatment is the anatomic reconstruction of the ACL with autograft (semitendinosus, gracilis, or patellar tendon) [2]. There are several studies in the literature that have compared single-bundle (SB) and double-bundle (DB) ACL reconstruction [3,4,5]. In a biomechanical study by Tashman et al., it was reported that as DB ACL reconstruction was more similar to the original anatomy, it was more advantageous than SB ACL reconstruction [6]. Some studies have shown that DB ACL reconstruction is superior to SB regarding knee stability and clinical results [7,8,9]. In contrast, other studies have reported no difference in knee stability and clinical results between the two techniques [10,11,12,13]. There are relatively few studies that have compared mid and long-term results. However, recent studies with 5-year follow-up periods have shown no statistically significant difference between the clinical results and laxity measurements [14, 15].
Magnetic resonance imaging (MRI) is the best radiological method for the evaluation of reconstructed ACLs [16, 17]. ACL is seen as hypointense on T1 and T2-weighted MR images naturally. In the early postoperative period (4–8 months), the grafted ACL is more heterogeneous and is seen at increased intensity because of revascularisation [18]. Therefore, it is difficult to evaluate the integrity of the graft at that postoperative time. After approximately 18 months, when revascularisation has been completed, the ACL is expected to be seen as hypointense like a normal ACL [19].
The aim of this study was to compare the 5-year follow-up results of patients who underwent SB and DB ACL reconstruction in terms of radiological maturation as well as clinical results and knee stability. We hypothesized that the DB ACL reconstruction group's clinical and radiological results would be better than the SB ACL reconstruction group.
Methods
Patients
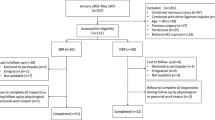
The study initially included 65 patients who underwent surgery because of ACL tear between January 2014 and January 2015. This study was designed as a prospective, case-controlled clinical study, including a 5-year follow-up period. The patients included were aged 20–50 years, with body mass index (BMI) between 18–30 and an ACL tear, for which surgery was performed within the first 6 months after the ACL injury. Patients with meniscal root rupture were not included in the study to make the groups more homogeneous. Patients were excluded from the study if they had multiple ligament injuries, a history of surgery on the same or the contralateral knee, deep cartilage lesion (grade > 2 International Cartilage Repair Society), or if the time from ACL injury to surgery was > 6 months. Approval for the study was granted by the Local Ethics Committee.
Anatomic SB ACL reconstruction was performed to 33 patients and anatomic DB ACL reconstruction to 32 patients. If anatomically inappropriate for DB ACL reconstruction was observed intraoperatively, that patient was included in the SB ACL reconstruction group. Of the total 65 patients, 12 were excluded from the study for various reasons; 3 patients in the SB group and 6 in the DB group could not be contacted during the postoperative follow-up period, 1 in the DB group underwent surgery again because of meniscal root tear, and 2 in the SD group underwent revision surgery because of graft failure.
The ACL injury diagnosis was made from physical examination and preoperative MRI findings. Anatomic ACL reconstruction was applied harvesting semitendinosus and gracilis tendon grafts from the same knee. In both groups, cortical button (Endobutton CL Ultra Fixation device, Smith and Nephew, USA) was used for femoral fixation, a bioabsorbable interference screw (Biorci screws, Smith and Nephew, USA) and a post-fixation screw (Fixation posts, Smith and Nephew, USA) for tibial fixation. All the operations were performed by the same surgeon experienced in ACL surgery.
Evaluations
The patient’s preoperative and postoperative clinical evaluations were made with the International Knee Documentation Committee (IKDC) and Lysholm knee scores. Rotational stability evaluations were made with the pivot shift test, which was classified as 0–3 [20]. The KT-1000 Arthrometer (MEDmetric, San Diego, CA, USA) and Lachman test were applied for evaluating anteroposterior stability. KT-1000 arthrometer was performed with the knee flexed 30 degree at 134 N forces. The results of the stability tests were compared with the non-operated side. The clinical evaluations were performed by a researcher not involved in the study. The MRIs of patients taken at 1 and 5 years postoperatively were evaluated by a musculoskeletal radiologist who was blinded to the clinical data. While evaluating the MRI results of the patients, the graft was examined at 4 degrees according to its volume and intensity [21]. Autograft was evaluated as grade 1 with the same homogeneity and hypointense appearance as patellar tendon and PCL. If more than 50% of the graft volume showed normal intensity, it was recorded as grade 2. If less than 50% of the graft volume was in normal ligament appearance, it was recorded as grade 3. If there was diffuse increased intensity in the autograft and the graft strands did not appear normal, it was evaluated as grade 4. Howell scoring was compared between single-bundle, AM bundle of the double bundle and PL bundle of double bundle.
Surgical technique
In all patients, grafts were taken from the semitendinosus and gracilis tendons as autograft. A far medial portal was used in all patients to be able to open femoral tunnels. Since we only evaluated acute ACL ruptures, the footprint areas could be seen easily intraoperatively. SB ACL reconstruction was performed in patients with an ACL tibial footprint < 14 mm, since DB ACL reconstruction may cause the tunnels to merge. Besides, in patients with notch width < 14 mm, SB ACL reconstruction was applied to avoid impingement.
In the patients undergoing the SB technique, after cleaning the ACL remnants, the bifurcate ridge and lateral intercondylar ridge landmarks were visualised in the femoral tunnel. The autografts were prepared by folding the semitendinosus tendon into 3 and the gracilis tendon into 2 or 3. Using the far medial portal, the femoral tunnel was prepared with the knee at 110–120° flexion with a tunnel diameter of 8–10 mm according to the graft thickness. Placement of the femoral tunnels was made close to the AM bundle femoral attachment point. After preparation of the tibial footprint, the tibial tunnel was formed using the ACL tibial guide (ACUFEX Director ACL Tip Aimer, Smith and Nephew, USA). The autograft was passed through the tunnels then fixed with an endobutton (Endobutton CL Ultra Fixation device, Smith and Nephew, USA) to the femoral side. On the tibial side, a bioabsorbable interference screw 1 mm thicker than the tunnel diameter was used (Biorci screws, Smith and Nephew, USA), and a post-fixation screw (Fixation posts, Smith and Nephew, USA). Tibial fixation was performed with the knee in 20° flexion.
The grafts for DB ACL reconstruction were prepared by folding the semitendinosus tendon into 3 and the gracilis tendon into 2 or 3, and were then used for the AM bundle and the PL bundle, respectively. While applying DB ACL reconstruction, the sites of the femoral tunnels were determined to appropriate to the anatomy by identifying the surgical landmarks. Using the far anteromedial portal with the knee at 110–120° flexion, both femoral tunnels were prepared to be 7–8 mm in diameter for the AM bundle and 5–6 mm for the PL bundle. In the tibia, first the PL tunnel, then the AM tunnel was prepared using the ACL tibial guide (ACUFEX Director ACL Tip Aimer, Smith and Nephew, USA). The autografts were passed through the tunnels then fixed with an endobutton (Endobutton CL Ultra Fixation device, Smith and Nephew, USA) to the femoral side, and on the tibial side, a bioabsorbable interference screw 1 mm thicker than the tunnel diameter was used (Biorci screws, Smith and Nephew, USA), and a post-fixation screw (Fixation posts, Smith and Nephew, USA). Tibial fixation was performed the knee in 40° flexion for the AM bundle and full extension for the PL bundle.
Postoperative rehabilitation
The same rehabilitation program was applied to all patients. As additional treatment for pain and edema in the first 3 weeks, strengthening exercises were started for knee flexion and extension. For patients undergoing meniscus repair, knee flexion was restricted to 90° for 3 weeks. Partial weight-bearing was permitted with underarm crutches, and a brace was not used in any patient. The crutches were used for 3–6 weeks and exercises were predominantly directed to full knee flexion. Balance, proprioception, and isotonic strengthening exercises were performed. In weeks 6–12, walking exercises and mild running were added, and isotonic and strengthening exercises were increased. After 45 days, cycling was permitted. Sports specific exercises such as jumping and changing direction while running were started after 3 months, but return to active sports was not permitted until 9 months.
Statistical analysis
The study data were analysed statistically using IBM SPSS 20.0 (IBM Corp., Armonk, NY, USA) software. Numerical variables showing normal distribution were stated as mean ± standard deviation (SD) values and those not showing normal distribution as median (minimum–maximum) values. Categorical variables were stated as number (n) and percentage (%). The preoperative and final follow-up values were compared with the paired t test. The postoperative clinical scores of the groups were compared with the Student’s t test and MRI findings with the Chi-square test. Spearman’s rho was used to evaluate postoperative stability and MRI findings correlation. Kaplan–Meier survival analysis was performed using failure as endpoint. Power analysis was performed to determine the sample size according to the Lysholm knee score data from similar studies. The minimum sample size was determined as 44 to provide a statistically significant difference with 0.90 power, 0.05 error margin, and 0.5 effect size. A value of p < 0.05 was accepted as statistically significant.
Results
The evaluation was made of the 5-year clinical and radiological findings of 53 patients, comprising the SB group of 28 patients with a mean age of 29.8 ± 2.9 years, and the DB group of 25 patients with a mean age of 28.9 ± 3.7 years. The comparison of the demographic data of the two groups is shown in Table 1. The Kaplan–Meier survival analysis showed no significant difference between the groups regarding failure rates. The IKDC scores were 54.4 ± 11.4 preoperatively and 93.7 ± 1.7 postoperatively in the SB ACL reconstruction group, and 53.6 ± 9.4 preoperatively and 94.2 ± 2.4 postoperatively in the DB ACL reconstruction group. The Lysholm scores were 60.1 ± 20.4 preoperatively and 92.1 ± 2.7 postoperatively in the SB group and 58.8 ± 22.4 preoperatively and 92.5 ± 4.0 postoperatively in the DB group. No statistically significant difference was determined between the groups postoperatively (p > 0.05) (Table 2). In both groups, the postoperative clinical scores were determined to be statistically significantly better than the preoperative values (p < 0.001).
Pivot shift test positivity at grade 1 was determined in two patients in the SB group, and all other patients were negative (grade 0). No significant difference was determined between the groups (p > 0.05). The Lachman test was negative in all patients. No statistically significant difference was determined between the groups in respect of both the preoperative and 5-year postoperative KT-1000 Arthrometer values (p > 0.05) (Table 3).
Meniscal tear was determined in eight patients in the SB ACL reconstruction group (two medial, four lateral, two both). The repair was performed to six patients using the with the all-inside technique. Partial meniscectomy was performed to two patients. Meniscal tear was determined in six patients in the DB ACL reconstruction group (two medial, three lateral, one both). Repair of the meniscus was performed the all-inside technique to five patients, and partial meniscectomy was applied to one patient. Cartilage damage (grade < 3, International Cartilage Repair Society) was observed in two patients in the DB group and three patients in the SB group. No statistically significant difference was determined between the groups in terms of additional injuries (Table 4). Debridement and chondroplasty were performed in these patients.
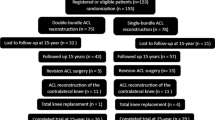
On the 1-year MRIs of the SB group, the ACL was seen at the normal intensity (Grade 1) in 22 patients and hyperintensity (> Grade 1) in 6 patients. In the DB group, the intensity was seen to be increased in both bundles (> Grade 1) in ten patients, and in six patients, the PL bundle was seen to be more heterogeneous and more hyperintense than the AM bundle. When the 12-month MRI findings were examined, it was observed that radiological maturation (ligamentisation) was less complete in the PL bundle compared to the SB group (p = 0.014). On the 5-year MRIs, the ACL was seen to be intact (Grade 1, normal) in 25 patients in the SB group and 23 patients in the DB group (Figs. 1, 2). In the DB group, the PL bundle was seen to be Grade three in four patients, and the PL bundle was seen to be diffuse hyperintense (Grade 4) in two patients (Table 5). Although the hyperintensity of the PL bundle was generally higher than both the AM bundle and the single bundle, no other significant difference was found in the comparisons made according to the Howell score (p > 0.05). These MRI findings were not compatible with the clinical and stability results. There was no significant correlation in the comparison of postoperative MRI results with both pivot shift and KT-1000 Arthrometer results (p > 0.05).
In the SB group, revision surgery was applied to two patients due to graft failure. No graft failure findings were determined in the DB group, and no statistically significant difference was determined between the groups in respect of graft failure (p > 0.05). At 3 years postoperatively, one patient in the DB group underwent surgery because of meniscal tear following a new trauma. A displaced tear was seen in the form of a flap in the medial meniscus and partial meniscectomy was applied.
Discussion
The most important finding of this study was that there was no superiority of DB ACL reconstruction over SB ACL reconstruction regarding clinical results and knee stability, but graft maturation (ligamentisation) was radiologically determined to have occurred later in the DB group. In addition, this study is one of the few studies showing that graft maturation is not compatible with clinical and stability results.
In some previous studies, better results have been reported in respect of stability in patients undergoing DB ACL reconstruction with autograft [22, 23]. However, in a recently published meta-analysis, no statistically significant difference was determined between patients undergoing SB or DB ACL reconstruction with autograft regarding rotational stability [24]. In the current study, pivot shift test positivity (grade 1) was determined in only two patients (7.14%) of the SB group. The pivot shift test was negative in all the patients of the DB group, and there was no significant difference between the two groups (p > 0.05). Also, no significant difference was determined between the KT-1000 Arthrometer measurements of the two groups (p > 0.05).
In a study of 60 patients (SB: 30, DB: 30) by Devgan et al. no significant difference was found between the 2 groups in respect of clinical scores and stability [11]. In another randomized clinical study, Liu et al. followed up two patient groups for approximately seven years after SB and DB ACL reconstruction using autograft, and no superiority of one technique over the other was reported [14]. In another prospective 10-year follow-up study of 81 patients, no significant difference was found regarding clinical results and knee stability. However, there was a higher rate of re-rupture in the patients undergoing SB ACL reconstruction [25]. Hussein et al. compared double-bundle and single-bundle ACL reconstruction in their prospective study. They reconstructed single bundle or double bundle according to the tibial insertion length of the ACL. After 30 months of follow-up, they found no difference between the two groups in terms of clinical result and knee stability [9]. Similarly, in the current study, there was no significant difference in the Lysholm and IKDC clinical scores of the two groups. In parallel with previous studies’ findings, revision surgery was applied to two patients in the current study SB group because of graft failure, but the difference was not statistically significant (p > 0.05).
SB ACL reconstruction is a widely used technique with good clinical results [9]. DB ACL reconstruction with hamstring tendons, which started to be used later, is a technique, which requires more specialist expertise, is more complex, and the operating time may be longer [26]. Although it has been shown in biomechanical studies that DB ACL reconstruction provides better rotational stability [27], in the mid and long-term clinical follow-up of a meta-analysis, no superiority to SB ACL reconstruction was seen [24]. Consistent with the literature findings, no significant difference was determined between the two groups in the current study in respect of clinical results or knee stability.
The most important feature of our study is that it is one of the few studies evaluating the relationship between radiological results and clinical results in 5-year follow-up. In a study by Sonoda et al., a relationship was reported between MRI findings and clinical outcomes [28]. The MRI findings of 97 patients undergoing DB ACL reconstruction were evaluated at the end of 1 year of follow-up. The hyperintense AM bundle was shown to be responsible for anteroposterior laxity and the hyperintense PL bundle for rotational laxity. This can be explained by the fact that the grafts have not fully completed the maturation stage at 1 year postoperatively and therefore could not function as a natural ligament. Biercevicz et al. stated that MRI parameters could be used to predict clinical results in three and 5-year follow-up [29]. Contrary to these studies, Kiekarave et al. showed that the hyperintense appearance of the grafts on MRI is not associated with instability [30]. In a prospective study by Suomalainen et al. patient groups undergoing SB and DB ACL reconstruction were compared, and there was reported to be no relationship between the 2-year follow-up MRI findings and clinical results in both groups [31]. At the end of 5 years, a normal appearance (Grade 1) was determined in the AM bundle of six patients in the DB group and there was hyperintense (> Grade 2) appearance of the PL bundle of these patients. When the ACL’s total integrity was examined in the 5-year follow-up of the current study, there was no grade 1 appearance in three patients in the SB group and two patients in the DB group. However, no significant difference was found between the 5-year follow-up MRI findings and the clinical results or knee stability. It is assumed that the hyperintense appearance of the PL bundle at the postoperative 5th year in some patients may be due to tunnel enlargement, and it has been reported that the hyperintense appearance of the ACL graft may continue for a long time [32].
The other important feature of the current study is that the MRI findings of the patients were evaluated at 1 and 5 years postoperatively. In the 1-year MRI findings, it was observed that maturation (ligamentisation) was ongoing and maturation was later in the DB group. The PL bundle had a more hyperintense appearance on MRI than the AM bundle at 1 year. This could be attributed to the PL bundle being thinner and shorter while performing reconstruction and while the knee is in semi-flexion, it is in contact with the lateral condyle. Also, the PL bundle has greater excursion than the AM bundle. At flexion, it is looser and at extension, it is tighter. Therefore, until the fusion of the tendon graft to the bone, just as it may cause greater loading on the fixation material, it may also be the reason for late ligamentisation of the tendon. The AM bundle is close to greater isometry. When moving from extension to flexion, there is very little loosening, in other words, minimal excursion [33, 34]. As maturation was later in the patients performed DB ACL reconstruction, it may be necessary to follow a more protective protocol in rehabilitation in the early postoperative period. In addition, return to sports may be delayed due to late maturation in the PL bundle after surgery.
There were some limitations to this study, primarily the relatively low number of patients in the groups. During the 5-year follow-up period, ten patients were excluded from the study for various reasons. The clinical outcomes of these excluded patients may also affect the results of the study. Secondly, determining the reconstruction technique according to anatomical features caused the study not to be randomized. In addition, in the current study and other studies, the study groups were formed of patients in the 20–50 years age range and these patients did not all have the same occupations. Future studies comparing the clinical results and graft re-rupture in patients in a narrower age range and with the same or similar occupations would provide more valuable results. One of the other limitations was the lack of histopathological examination, which is the gold standard in the evaluation of graft maturation. In addition, it has been reported that the hyperintense appearance seen in MRI may be due to age and tunnel enlargement and may remain hyperintense for a long time [32, 35]. Tunnel enlargement was not evaluated in the current study. Despite these limitations, a more protective rehabilitation protocol may be required in the early postoperative period due to the hyperintense PL bundle in the first year.
Conclusion
In the 5-year follow-up results of patients undergoing SB ACL reconstruction and those undergoing DB ACL reconstruction, no statistically significant difference was determined in respect of clinical results, knee stability, and MRI findings, but maturation (ligamentisation) was radiologically determined to occur later in the patients undergoing DB reconstruction.
Data availability
Available.
References
Calvert ND, Smith A, Ackland T et al (2020) Kneeling difficulty is common following anterior cruciate ligament reconstruction with hamstring autograft and correlates with outcome measures. Arch Orthop Trauma Surg 140:913–921
Bierke S, Abdelativ Y, Hees T et al (2020) Risk of arthrofibrosis in anatomical anterior cruciate ligament reconstruction: the role of timing and meniscus suture. Arch Orthop Trauma Surg 141(5):743–750
Fujita N, Kuroda R, Matsumoto T et al (2011) Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthrosc J Arthrosc Relat Surg 27:906–913
Adachi N, Ochi M, Uchio Y et al (2004) Reconstruction of the anterior cruciate ligament: single-versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86:515–520
Hemmerich A, van der Merwe W, Batterham M, Vaughan CL (2011) Knee rotational laxity in a randomized comparison of single-versus double-bundle anterior cruciate ligament reconstruction. Am J Sports Med 39:48–56
Tashman S, Collon D, Anderson K et al (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 32:975–983
Morey VM, Nag HL, Chowdhury B et al (2015) A prospective comparative study of clinical and functional outcomes between anatomic double bundle and single bundle hamstring grafts for arthroscopic anterior cruciate ligament reconstruction. Int J Surg 21:162–167
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 24:137–145
Hussein M, van Eck CF, Cretnik A et al (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3-to 5-year follow-up. Am J Sports Med 40:512–520
Ra HJ, Kim J-H, Lee D-H (2020) Comparative clinical outcomes of anterolateral ligament reconstruction versus lateral extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: systematic review and meta-analysis. Arch Orthop Trauma Surg 140:923–931
Devgan A, Rohilla R, Singh A et al (2016) A prospective study to evaluate the clinico-radiological outcomes of arthroscopic single bundle versus double bundle anterior cruciate ligament reconstruction. J Clin Orthop trauma 7:236–242
Zhang Z, Gu B, Zhu W, Zhu L (2014) Double-bundle versus single-bundle anterior cruciate ligament reconstructions: a prospective, randomized study with 2-year follow-up. Eur J Orthop Surg Traumatol 24:559–565
Koken M, Akan B, Kaya A, Armangil M (2014) Comparing the anatomic single-bundle versus the anatomic double-bundle for anterior cruciate ligament reconstruction: a prospective, randomized, single blind, clinical study. Eur Orthop Traumatol 5:247–252
Liu Y, Cui G, Yan H et al (2016) Comparison between single-and double-bundle anterior cruciate ligament reconstruction with 6-to 8-stranded hamstring autograft: a prospective, randomized clinical trial. Am J Sports Med 44:2314–2322
Sasaki S, Tsuda E, Hiraga Y et al (2016) Prospective randomized study of objective and subjective clinical results between double-bundle and single-bundle anterior cruciate ligament reconstruction. Am J Sports Med 44:855–864
Casagranda BC, Maxwell NJ, Kavanagh EC et al (2009) Normal appearance and complications of double-bundle and selective-bundle anterior cruciate ligament reconstructions using optimal MRI techniques. Am J Roentgenol 192:1407–1415
Min BH, Chung WY, Cho JH (2001) Magnetic resonance imaging of reconstructed anterior cruciate ligament. Clin Orthop Relat Res 393:237–243
Miller TT (2009) MR imaging of the knee. Sports Med Arthrosc 17:56–67
Stöckle U, Hoffmann R, Schwedke J et al (1998) Anterior cruciate ligament reconstruction: the diagnostic value of MRI. Int Orthop 22:288–292
Hefti E, Müller W, Jakob RP, Stäubli H-U (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sport Traumatol Arthrosc 1:226–234
Howell SM, Clark JA, Blasier RD (1991) Serial magnetic resonance imaging of hamstring anterior cruciate ligament autografts during the first year of implantation: a preliminary study. Am J Sports Med 19:42–47
Kondo E, Yasuda K, Azuma H et al (2008) Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med 36:1675–1687
Ventura A, Iori S, Legnani C et al (2013) Single-bundle versus double-bundle anterior cruciate ligament reconstruction: assessment with vertical jump test. Arthrosc J Arthrosc Relat Surg 29:1201–1210
Chen H, Chen B, Tie K et al (2018) Single-bundle versus double-bundle autologous anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials at 5-year minimum follow-up. J Orthop Surg Res 13:50
Järvelä S, Kiekara T, Suomalainen P, Järvelä T (2017) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 10-year results. Am J Sports Med 45:2578–2585
Sernert N, Hansson E (2018) Similar cost-utility for double-and single-bundle techniques in ACL reconstruction. Knee Surg Sport Traumatol Arthrosc 26:634–647
Siebold R, Ellert T, Metz S, Metz J (2008) Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry and arthroscopic orientation models for double-bundle bone tunnel placement—a cadaver study. Arthrosc J Arthrosc Relat Surg 24:585–592
Sonoda M, Morikawa T, Tsuchiya K, Moriya H (2007) Correlation between knee laxity and graft appearance on magnetic resonance imaging after double-bundle hamstring graft anterior cruciate ligament reconstruction. Am J Sports Med 35:936–942
Biercevicz AM, Akelman MR, Fadale PD et al (2015) MRI volume and signal intensity of ACL graft predict clinical, functional, and patient-oriented outcome measures after ACL reconstruction. Am J Sports Med 43:693–699
Kiekara T, Järvelä T, Huhtala H et al (2014) Tunnel communication and increased graft signal intensity on magnetic resonance imaging of double-bundle anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg 30:1595–1601
Suomalainen P, Moisala A-S, Paakkala A et al (2011) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med 39:1615–1623
Farshad-Amacker NA, Potter HG (2013) MRI of knee ligament injury and reconstruction. J Magn Reson Imaging 38:757–773
Yonetani Y, Toritsuka Y, Yamada Y et al (2005) Graft length changes in the bi-socket anterior cruciate ligament reconstruction: comparison between isometric and anatomic femoral tunnel placement. Arthrosc J Arthrosc Relat Surg 21:1317–1322
Zavras TD, Race A, Bull AMJ, Amis AA (2001) A comparative study of’isometric’points for anterior cruciate ligament graft attachment. Knee Surg Sport Traumatol Arthrosc 9:28–33
Yanagisawa S, Kimura M, Hagiwara K et al (2018) Patient age as a preoperative factor associated with tunnel enlargement following double-bundle anterior cruciate ligament reconstruction using hamstring tendon autografts. Knee Surg Sport Traumatol Arthrosc 26:1230–1236
Acknowledgements
There is no acknowledgement.
Funding
We have no financial biases.
Author information
Authors and Affiliations
Contributions
RA: conceived and design the analysis, wrote the paper, performed operations. YY: wrote the paper, collected the data. İK performed the analysis, contributed data or analysis tools. MBE: wrote the paper. MMÇ: performed the analysis, collected the data. ZA: collected radiological data and evaluated.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
We obtained ethical approval from review board of Ankara University Faculty of Medicine (No. 08-345-14).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akmeşe, R., Yoğun, Y., Küçükkarapinar, İ. et al. Radiological maturation and clinical results of double-bundle and single-bundle anterior cruciate ligament reconstruction. A 5-year prospective case-controlled trial. Arch Orthop Trauma Surg 142, 1125–1132 (2022). https://doi.org/10.1007/s00402-021-03971-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03971-4