Abstract
Background
Lateral clavicle fractures associated with partial or complete injury of the coracoclavicular ligaments have traditionally been treated using a variety of open surgical techniques.
Purpose of the study
The aim of this prospective study was the evaluation of the clinical and radiologic outcome of displaced lateral clavicular fractures with coracoclavicular instability treated in an arthroscopic single TightRope technique including an interfragmentary cerclage.
Methods
From 2008 to 2010, 23 patients [8 women and 15 men; mean age 38 (24–63) years] who sustained a displaced lateral clavicular fracture type II according to Neer were included in this study. The follow-up consisted of a complete physical examination of the shoulder including range of motion, the constant score (CS), and the subjective shoulder value (SSV). The radiological follow-up included an anteroposterior stress view with 10 kg of axial load and bilateral axillary views to evaluate the coracoclavicular distance, the clavicular implant position, and healing of the fracture.
Results
After a mean follow-up of 23.0 (13–38) months, 20 patients (7 women and 13 men; mean age 38.3 (24–53) years) were available for follow-up. On average, patients achieved 95.1 (60–100) % in the SSV, 88.7 (64–99; contralateral side 91.8 points; p > 0.05) points in the CS. Radiologically, 18 of 20 patients (90 %) displayed a bony healing of the fracture. The average coracoclavicular distance of 11.2 (6–14) mm did not differ significantly from the healthy side [9.9 (8–14) mm]. In six cases (30 %), coracoclavicular ossifications appeared. Two of 20 patients had concomitant glenohumeral lesions (10 %). Two patients had secondary surgery [implant removal (N = 1 local implant irritation); plate osteosynthesis (N = 1 early loss of reduction)].
Conclusion
The arthroscopic-assisted and image intensifier-controlled closed reduction and single TightRope fixation with interfragmentary cerclage of displaced lateral clavicular fractures with coracoclavicular instability yields excellent clinical results and is able to recreate stability of the clavicle.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lateral clavicle fractures occur in up to 28 % of all clavicle fractures [29]. However, due to the anatomic relation to the coracoclavicular ligaments partial or complete injury of these ligaments and subsequent vertical instability of the clavicle with an intact, acromioclavicular joint causes a high risk of pseudarthrosis and persisting pain after conservative treatment [4, 15, 23]. Different classification systems are published in the literature, some consider involvement of the CC ligaments and resulting vertical clavicular instability [1, 7, 14, 23, 29]. Traditional open surgical techniques include Kirschner wire osteosynthesis, screw fixation analog to the Bosworth Screw, plate fixation including, e.g., a clavicular hook plate and also polydioxane suture tension band wiring [3, 13, 16, 18, 20, 23, 35]. Besides the need for obligatory implant removal in most of these techniques, a large variety of complications have been described in the literature ranging from periimplantary fractures to intraaortic migration of Kirschner wires [8–10, 18, 21, 24, 36].
Recently, minimal invasive methods have been described [5, 26]. The aim of this prospective study was the evaluation of the clinical and radiologic outcome of patients suffering from displaced lateral clavicular fractures with coracoclavicular instability treated in an arthroscopic single TightRope technique (Arthrex, Naples, Fl) including an interfragmentary cerclage.
Materials and methods
Patient population
The local ethical committee approved of the study protocol (EA 1/187/14).
From 2008 to 2010, 23 patients [8 women and 15 men, mean age 38 (24–63) years] who sustained a displaced lateral clavicular fracture type II according to Neer were included in this study [23]. The follow-up consisted of a complete physical examination of the shoulder including range of motion, the constant score (CS), and the subjective shoulder value (SSV) [6, 11]. The radiological evaluation included an anteroposterior stress view with 10 kg of axial load and bilateral axillary views to evaluate the coracoclavicular distance, the clavicular implant position, and consolidation of the fracture side. Patients were treated in the technique mentioned below if they sustained a displaced lateral clavicle fracture with coracoclavicular instability due to rupture of the coracoclavicular ligaments.
Surgical technique
The patient is placed in the beach chair position under general anesthesia and perioperative antibiotics. The shoulder is prepped and draped. A diagnostic arthroscopy is performed via a standard posterior portal. Possible concomitant glenohumeral lesions are treated first. Second, a transtendinous lateral viewing portal parallel through the tendon fibers of the supraspinatus tendon as well as an anteroinferior working portal is established in an outside-in technique. The arthroscope is switched to the lateral portal and the subcoracoid space and the undersurface of the coracoid are prepared using an electrothermic device. Next, a 1.5–2 cm incision superior of the clavicle approximately 2 cm medial to the fracture side as well as a 1-cm incision directly above the lateral fragment is established (Fig. 1). Hence, the fracture is reduced with the aid of a periosteal elevator (Fig. 2).
Drilling and K-wire placement are carried out with the aid of an anterior cruciate ligament drill guide and under image intensifier control.
The transclavicular-transcoracoidal drill hole for the Tight Rope (Arthrex, Naples, Fl) is established placing the marking hook of the drill guide under direct visualization through the anteroinferior portal into the subcoracoidal space and under the medial part of the coracoid process. The drill sleeve is placed over the clavicle.
Then, a K-wire is placed and overdrilled using a cannulated drill bit (4.0 mm) (Fig. 3a, b). The K-wire and the drill guide are removed and two flexible nitinol suture passing wires are inserted and retrieved via the anteroinferior portal (Fig. 3c).
Establishing the first transclavicular-transcoracoidal drill hole (exterior view, arthroscopic, and image intensifier control). a Placing of the transclavicular-transcoraoidal K-wire. b Overdrilling using a cannulated drill bit (4.0 mm). c Removal of the drill guide and K-wire; insertion of two flexible nitinol suture passing wires
Hence, the drill sleeve of the drill guide is positioned over the lateral fragment and a transfragmentary drill hole is established in the same fashion using a K-wire (1.1 mm) and a cannulated drill bit (2.7 mm) (Fig. 4a, b). A nitinol suture passing wire is inserted (Fig. 4c).
Establishing the transfragmentary drill hole (exterior view, arthroscopic, and image intensifier control). a The drill sleeve of the drill guide is positioned over the lateral fragment and a transfragmentary drill hole is established using a K-wire (1.1 mm). b Overdrilling using a cannulated drill bit (2.9 mm). c A nitinol suture passing wire is inserted
Next, the Tight Rope is inserted via one of the two nitinol wires in the first drill hole (Fig. 4c). The cerclage material (Fiber Tape, Arthrex, Naples, Fl) is shuttled transclavicularly and transcoracoidal using the second nitinol wire of the first drill hole. Via the third transfragmentary nitinol wire the cerclage is then led laterally past the coracoid through the fragment. Finally, both ends of the Fiber Tape are retrieved with a clamp via the incision above the fragment (Fig. 5a–c).
The Tight Rope and the cerclage are knotted securely (Fig. 5d, e).
The clavicular incision is closed in two layers, and the arthroscopic portals were closed in a standard fashion (Fig. 5f).
The patients were immobilized in a sling for 6 weeks postoperatively. Passive physiotherapy started on the first postoperative day including passive range of motion exercises up to 45° for 3 weeks and up to 90° from the fourth to the sixth week. From week 7, passive range of motion was permitted unlimited and active mobilization was started. After 3 months, patients were allowed to participate in non-contact sports and do manual labor.
Statistics
Statistical analysis was performed using SPSS version 16.0 (SPSS Inc, Chicago, IL). Descriptive results are demonstrated as the mean (range). The Kolmogorov–Smirnov test was used on all data to test for normal distribution. Metric data were compared using the Student's t test. The results of the CS, TF, and SSV were correlated using Pearson’s correlation coefficient and compared employing the Mann–Whitney U test. The Chi-square test was used to test for significant differences in dichotome data. The level of significance was defined as p = 0.05.
Results
Patient cohort
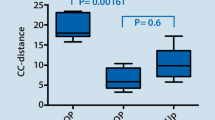
After a mean of 23.0 (13–38) months, 20 patients [7 women and 13 men; mean age 38.3 (24–53) years] were available for follow-up. All patients suffered from a direct trauma to the shoulder girdle, either due to a fall off a bike (N = 9), a car or motorcycle accident (N = 3), a fall during sports (N = 2, inline skating and softball), or domestic activities (N = 6). Initial loaded bilateral stress views revealed an average coracoclavicular distance of 20.5 (15–25) mm on the affected versus 11.2 (8–22) mm on the healthy side.
Concomitant glenohumeral lesions (10 %)
Two of 20 patients had intraarticular concomitant lesions.
Both had an ipsilateral traumatic subscapularis tear (Fox and Romeo type I and II). The type I lesion was debrided. The type II lesion was treated using suture anchor repair.
Overall concomitant lesions
In total, nine patients had additional injuries. Of those five patients were polytraumatized including head trauma with intracranial bleeding in four patients, lung contusion and pneumothorax in two, rib fracture in one, midfacial fractures in two, pubic fracture in one, contralateral AC joint dislocation type V according to Rockwood in one, olecranon fracture in one and anterior cruciate ligament rupture in one patient. Besides that, there were two patients with additional trauma to the upper extremity: one patient suffered from an ipsilateral bony tendon avulsion of the fourth digit and another from a dislocation of the third metacarpophalangeal joint and fracture of the trapezoid bone.
Clinical results
All patients rated their cosmetic result as very good. Two patients complained of implant irritation above the superior Tight Rope button and suture material, one of which necessitated complete implant removal. One patient experienced slight tenderness to palpation (NAS = 2) without radiographic signs of AC joint arthritis and with negative AC joint tests. Mean range of motion averaged 178° (170°–180°) of flexion, 177° (170°–180°) of abduction, 71° (50°–90°) of external rotation in 0° abduction [contralateral 76° (60°–90°), p > 0.05], 83° (70°–90°) of external rotation in 90° abduction, and 55° (30°–80°) internal rotation in 90° abduction. No statistically significant differences in comparison to the contralateral side were observed (p > 0.05). On average, patients achieved 96 (70–100) % in the SSV and 89 (64–99; contralateral side 91.8 points; p > 0.05) points in the CS.
Radiological results
Radiologically, 18 of 20 patients (90 %) had a bony consolidation of the fracture (Fig. 6).
Both patients with non-union were asymptomatic at the time of follow-up (patient 1: SSV = 99 %; CS = 98 points; contralateral 100 points; patient 2: SSV = 100 %; CS = 84 points on both sides). On initial posttraumatic anteroposterior views, the mean fragment length was 22.5 (7–33) mm. There was no significant correlation between fragment size and coracoclavicular distance or score results (p < 0.05).
At the time of final follow-up, the mean coracoclavicular distance of 11.2 (6–14) mm did not differ significantly from the healthy side [9.9 (8–14) mm]. In six cases (30 %), coracoclavicular ossifications appeared. Of those, two had suffered from a polytrauma, of which one had a head injury with intracranial bleeding. The other polytraumatised patients showed no signs of coracoclavicular ossification.
Complications requiring revision
One patient reported of implant irritation above the clavicle, which necessitated a complete implant removal. Furthermore, one patient had to be revised with open reduction and plate osteosynthesis due to early secondary loss of reposition caused by an aggressive physical therapy 6 weeks postoperatively.
Discussion
The spectrum of traditionally open treatment of lateral clavicular fractures includes Kirschner wire osteosynthesis, screw fixation analog to the Bosworth screw, plate fixation, and also polydioxane suture tension band wiring [3, 16, 20]. Most of these open reduction and reconstruction techniques require implant removal. Furthermore, without diagnostic arthroscopy, they lack the potential of diagnosing and treating intraarticular glenohumeral concomitant lesions. In addition to that, various complications are described in the literature ranging from mild to grotesque ones such as intraaortic, pulmonal, or spinal migration of Kirschner wires [12, 27, 28].
Hook plate fixation may lead to impingement syndrome (25 %) and acromial osteolysis (32 %), and requires a secondary procedure for implant removal [34]. Open reduction and internal fixation with locking plates have been shown to provide adequate fracture healing, but lateral screw placement can be challenging in fractures with small and comminuted fragments. High rates of secondary implant removal (43 %) due to plate irritation or intraarticular screw placement have been described [35]. Besides, due to the injury of the CC ligaments, a high mechanical load is placed on the lateral screws that may result in screw loosening [30]. Andersen et al. report a 25 % (N = 4/16) rate of secondary surgery after superior locking plate for distal clavicle fractures [2]. Three of the patients had implant removal due to hardware prominence. One patient had a deep infection that was treated with debridement, irrigation, and implant removal. He subsequently developed a symptomatic non-union and had to undergo distal clavicle resection. Recently, minimal invasive treatment options for lateral clavicle fractures have been described [5, 26].
Besides possible advantages such as minimalization of surgical trauma, the TightRope device lacks the necessity of a regular implant removal. In 2008, Pujol et al. reported of four cases of lateral clavicle fractures treated with coracoclavicular single TightRope stabilization without interfragmentary cerclage. They found good clinical outcomes after a short-term follow-up with bony consolidation in all four cases without peri- or postsurgical complications [26]. These results are in concordance with our excellent clinical results and high patient satisfaction with a good healing rate (90 %). Recently, Pujol et al. described a minimal invasive reconstruction technique using two double-button devices for comminuted lateral clavicle fractures [25]. The first double button is placed transclavicular and transcoracoidal, whereas the second mini-double button is drilled through the superior clavicle and the inferior fragment. However, clinical data are currently lacking.
We found coracoclavicular ossification in line of the coracoclavicular ligaments in six out of 20 patients. However, only two of those patients were polytraumatized and only one suffered from brain injury. Thus, it might be hypothesized that this kind of ossification could be unrelated to described cases of systemic heterotopic ossification, but might rather be a local phenomenon due to injury to the coracoclavicular ligaments as has been described to occur frequently in acromioclavicular joint injuries as well [17, 22, 31, 32].
It has been proposed that in these lateral clavicle fractures the trapezoid ligament remains intact and attached to the lateral fragment [19]. However, Neer described an accompanying injury of both ligaments with at least a partial injury of the trapezoid ligament [23]. Besides, Takase et al. have described the anatomy of the coracoclavicular ligaments [33]. According to his findings, the trapezoid ligament was found from 8.2 (5–13) to 23.6 (17–33) mm distanced from the lateral clavicle edge. We found a mean fragment length of 22.5 (7–33) mm. Four patients even displayed a fragment length of less than 7 mm. These findings suggest at least a partial rupture of the trapezoid ligament in most patients.
This study has some limitations. First, regarding injury to the coracoclavicular ligaments, we did neither obtain MRI nor directly visualize the ligaments. Thus, diagnosis of injury was made indirect using bilateral anteroposterior stress views.
Second, the number of patients is rather small. However, to our knowledge, this is the first and largest study to describe results of patients treated in a Tight Rope technique with an additional interfragmentary cerclage. If this technique presents a definite advantage regarding complications requiring revision and rate of pseudarthrosis is currently unknown as comparable and conclusive data is lacking in the literature. However, we feel that this arthroscopically assisted technique offers the possibility of diagnosing and treating intraarticular glenohumeral lesions, prevents the need of an obligatory implant removal, and allows to repair lateral clavicle fractures with small fragments where screw placement is not feasible.
Conclusion
The arthroscopic-assisted and image intensifier-controlled closed reduction and Single-TightRope fixation with interfragmentary cerclage of displaced lateral clavicular fractures with coracoclavicular instability yields excellent clinical results and is able to recreate stability of the clavicle.
References
Allman FJ (1967) Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 49:774–784
Andersen JR, Willis MP, Nelson R, Mighell MA (2011) Precontoured superior locked plating of distal clavicle fractures: a new strategy. Clin Orthop Relat Res 469:3344–3350
Ballmer F, Gerber C (1991) Coracoclavicular screw fixation for unstable fractures of the distal clavicle. J Bone and Joint Surg 73-B:291–294
Brunner U, Habermeyer P, Schweiberer L (1992) Special status of lateral clavicular fracture. Orthopade 21:163–171
Checchia S, Doneux PS, Miyazaki AN et al (2008) Treatment of distal clavicle fractures using an arthroscopic technique. J Shoulder Elbow Surg 17:395–398
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Craig E (1990) Fractures of the clavicle. In: Rockwood CJ, Matsen FA III (eds) The shoulder. W.B Saunders Company, Philadelphia, pp 367–412
Ding M, Hu J, Ni J, Lv H, Song D, Shu C (2012) Iatrogenic subclavian arteriovenous fistula: rare complication of plate osteosynthesis of clavicle fracture. Orthopedics 35:e287–e289
Ding M, Ni J, Hu J, Song D (2011) Rare complication of clavicular hook plate: clavicle fracture at the medial end of the plate. J Shoulder Elbow Surg 20:e18–e20
Flinkkila T, Ristiniemi J, Hyvonen P, Hamalainen M (2002) Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand 73:50–53
Fuchs B, Jost B, Gerber C (2000) Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am 82:16–25
Hegemann S, Kleining R, Schindler HG, Holthusen H (2005) Kirschner-Draht-migration in die kontralaterale Lunge nach Klavikulafrakturosteosynthese. Unfallchirurg 108:991–993
Herrmann S, Schmidmaier G, Greiner S (2009) Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury 40:236–239
Jäger M, Breitner S (1984) Therapy related classification of lateral clavicula fracture. Unfallheilkunde 87:467–473
Jupiter J, Leibman MI (2007) Supraclavicular nerve entrapment due to clavicular fracture callus. J Shoulder Elbow Surg 16:e13–e14
Kashii M, Inui H, Yamamoto K (2006) Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res 447:159–164
Krueger-Franke M, Siebert CH, Rosemeyer B (1993) Surgical treatment of dislocations of the acromioclavicular joint in the athlete. Br J Sports Med 27:121–124
Lee KW, Lee SK, Kim KJ, Kim YI, Kwon WC, Choy WS (2010) Arthroscopic-assisted locking compression plate clavicular hook fixation for unstable fractures of the lateral end of the clavicle: a prospective study. Int Orthop 34:839–845
Lee SK, Lee JW, Song DG, Choy WS (2013) Precontoured locking plate fixation for displaced lateral clavicle fractures. Orthopedics 36:801–807
Mall J, Jacobs CA, Philipp AW, Peter FJ (2002) Surgical treatment of the distal clavicle with polydioxanone suture tension band wiring: an alternative osteosynthesis. J Orthop Sci 7:535–537
Moneim MS, Balduini FC (1982) Coracoid fracture as a complication of surgical treatment by coracoclavicular tape fixation. A case report. Clin Orthop Relat Res 168:133–135
Mouhsine E, Garofalo R, Crevoisier X, Farron A (2003) Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg 12:599–602
Neer IC (1963) Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma 3:99–110
Nordback I, Markkula H (1985) Migration of Kirschner pin from clavicle into ascending aorta. Acta Chir Scand 151:177–179
Pujol N, Desmoineaux P, Boisrenoult P, Beaufils P (2013) Arthroscopic treatment of comminuted distal clavicle fractures (latarjet fractures) using 2 double-button devices. Arthrosc Tech 2:e61–e63
Pujol N, Philippeau JM, Richou J, Lespagnol F, Graveleau N, Hardy P (2008) Arthroscopic treatment of distal clavicle fractures: a technical note. Knee Surg Sports Traumatol Arthrosc 16:884–886
Regel J, Pospiech J, Aalders TA, Ruchholtz S (2002) Intraspinal migration of a Kirschner wire 3 months after clavicular fracture fixation. Neurosurg Rev 25:110–112
Ring D, Kolovacs T (2005) Brachial Plexus palsy after intramedullary fixation of a clavicular fracture. A report of three cases. J Bone Joint Surg Am 87:1834–1837
Robinson CM (1998) Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 80:476–484
Sajid S, Fawdington R, Sinha M (2013) Locking plates for displaced fractures of the lateral end of clavicle: potential pitfalls. Int J Shoulder Surg 6:126–129
Scheibel M, Droschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 39:1507–1516
Sim E, Schwarz N, Hocker K, Berzlanovich A (1995) Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res 314:134–142
Takase K (2010) The coracoclavicular ligaments: an anatomic study. Surg Radiol Anat 32(7):683–688
Tiren D, van Bemmel AJ, Swank DJ, van der Linden FM (2012) Hook plate fixation of acute displaced lateral clavicle fractures: mid-term results and a brief literature overview. J Orthop Surg Res 7:2
Tiren D, Vroemen JP (2013) Superior clavicle plate with lateral extension for displaced lateral clavicle fractures: a prospective study. J Orthop Traumatol 14:115–120
Wijdicks FJ, Van der Meijden OA, Millett PJ, Verleisdonk EJ, Houwert RM (2012) Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg 132:617–625
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors would like to state that no outside funding or grants were received that assisted in the study.
Rights and permissions
About this article
Cite this article
Kraus, N., Stein, V., Gerhardt, C. et al. Arthroscopically assisted stabilization of displaced lateral clavicle fractures with coracoclavicular instability. Arch Orthop Trauma Surg 135, 1283–1290 (2015). https://doi.org/10.1007/s00402-015-2271-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2271-1