Abstract
Introduction
The aim of this study is to evaluate the effect of the medial and lateral posterior tibial slope (MPTS, LPTS) in patients with acutely ruptured ACL on the menisci. It was hypothesized that medial and lateral meniscus lesions are seen more often with high PTS (posterior tibial slope). We hypothesized that in case of a high tibial slope a possible meniscus lesion is more often located in the posterior horn of the meniscus than in knees with a low tibial slope.
Materials and methods
We identified 537 patients with ACL insufficiency between 2012 and 2013. Of these, 71 patients were eligible for the study according to the study’s criteria. PTS was measured via MRI and classified into two groups: >10° for high tibial slope and ≤10° for low tibial slope. Any meniscal lesion was documented during arthroscopic ACL reconstruction and evaluated regarding meniscal lesion patterns with high and low PTS, taking into account the type and the location of the tear (anterior horn, intermediate part and posterior horn). Statistical analysis for differences in meniscal lesion was performed using Chi-square tests and McNemar tests for dependent variables. The level of significance was set at p ≤ 0.05.
Results
High PTS (MPTS and LPTS) was associated with a higher incidence of meniscal lesions with an odds ratio of 2.11, respectively, 3.44; however, no statistical significance was found. Among the total number of ACL-insufficient knees studied, the meniscal lesion spread more often to the posterior part in the group with a low PTS. In contrast, less damage of the posterior horn of the meniscus could be found in the group with a high PTS.
Conclusion
High PTS seems to predetermine for meniscal lesion in an acute ACL-insufficient knee. More damage to the posterior part of the menisci could generally be seen but was not associated with a high PTS. There was no statistical significance to support the initial hypothesis. Further research is needed to find out if factors other than tibial slope are risk factors for meniscal lesion in acute ACL injury.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since Butler et al. [6] stated the thesis that the ACL is the primary restrain of anterior tibial translation, it is well accepted that, due to increased anterior tibial translation, more stress is used on the ligamentous structures in the knee [5]. Therefore, with high in situ forces on the ACL, the translatoric movement becomes a possible determinant for an ACL lesion. Increased anterior tibial translation could be determined with axial compression, knee flexion and with steeper posterior tibial slope [10, 14, 42]. This indicates a potential risk factor for increased ligament load and possible ACL lesion with subsequent joint laxity. Various authors have shown higher stress on the ACL or even ACL lesion upon exercise of isolated or combined axial tibiofemoral forces [17, 29, 35] and quadriceps load [11]. Their findings were attributed to the impact of the tibial slope [27, 31].
Recently, a variety of studies have investigated the association between tibial plateau slopes and the risk of undergoing ACL insufficiency. The extent of this association, however, has largely varied between the studies and is still controversially discussed [12, 46, 47]. In addition, recent literature has primarily focused on traumatic non-contact ACL lesion, not taking into account further damage to other structures of the knee joint. It has been shown that acute ACL lesion is generally associated with damage to the lateral meniscus [4, 9, 40] and chronic ACL insufficiency shows more damage to the medial meniscus [4, 8, 13, 36, 40, 45]. The patterns in meniscal lesion for high tibial slope have previously been investigated in chronic ACL-insufficient patients [25], showing more damage on the medial side. The impact of an acute ACL lesion with high tibial slope on meniscal structures in the injured knee has not yet been reported. Therefore, the aim of our study is to further elucidate the influence of high tibial slope on the ACL-insufficient knee, to distinguish if overall high tibial slope causes more meniscal damage in the acute ACL-insufficient patient.
It was hypothesized that with high MPTS (medial posterior tibial slope) and LPTS (lateral posterior tibial slope) there is an increase in meniscal damage.
It was further hypothesized that due to high medial and lateral MPTS and LPTS there is a shift of lesions to the posterior part of the meniscus.
Materials and methods
Patients
537 patients underwent ACL reconstruction between January 2012 and October 2013 (22 months). Inclusion criterion for this retrospective chart view was first-time ACL reconstruction.
Exclusion criteria were posterolateral instability, PCL injury or insufficiency, time from ACL trauma to surgery longer than 3 months, ACL lesion with contact mechanism to the knee, prior (partial) meniscal resection, prior meniscal tears, prior meniscal refixation, chronic meniscal damage before ACL rupture, infection, osteoarthritis and/or a lack of access to high-quality digital MRI imaging. 71 patients met our criteria for this retrospective chart view, 466 patients were excluded (Fig. 1).
The patients’ histories, physical examinations and MRI findings stated the initial diagnosis and the ACL injury mechanism (non-contact). In all patients, ACL insufficiency, meniscal lesion and meniscal treatment were confirmed arthroscopically and documented according to a standardized protocol.
Six different categories of meniscal damage were classified: (1) degeneration (including extrusion, defibrillation and lesion), (2) radial tears, (3) longitudinal tears, (4) flap tear, (5) bucket-handle tears, and (6) root tears. To clarify the exact location of the damage, the meniscus was divided into three parts—the anterior horn, the intermediate part and the posterior horn. Meniscal lesion to the posterior part was defined as damage to the posterior horn and overlapping lesion to the intermediate part and the posterior horn.
Depending on the location and the severity of the lesion, a partial meniscectomy, refixation, or a combination of both was performed.
Measurement of the posterior tibial slope
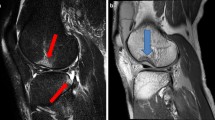
The method described by Hudek et al. [21], in cooperation with a radiologist specializing in MRI, was used to evaluate the posterior tibial slope. In short, this technique defines the tibial axis. This method was used, as in standardized MRI of the knee, only a short proximal part of the tibia can be seen and for the exact placement of the anatomical tibial axis, the malleolus should be visible [28].
After determining the central sagittal image, in which the tibial attachment of the PCL, the intercondylar eminence and the anterior and posterior tibia cortices appear in a concave shape, two circles were placed in the tibial head. The upper one had to touch the anterior, posterior and cranial tibial cortex bone and the lower one had to touch the anterior and posterior cortex border and was centered on the circumference of the cranial circle. Should there have been only vague borders between the cortex and medullary canal, the middle of the transition zone was chosen to set the two circles. The line connecting the two centers of the circles has been defined as an approximation to the real anatomic tibial axis (Fig. 2) [21, 28].
The uppermost part of the anterior and posterior rim of the convex-shaped lateral plateau, respectively, the anterior and posterior rim of the concave-shaped medial tibial plateau were connected, taking into account the cartilage of the joint [16]. The angle between the orthogonal to the tibial axis and these lines was considered to mark the medial and lateral posterior tibial slope (Fig. 3) [21].
All sagittal slices were set manually and the digital measurements were done twice by the same observer for every patient with OsiriX Imaging Software v. 3.8 at an interval of 2 weeks.
Classification of the values for the medial and lateral posterior tibial slope
To further assess the tibial slope, the patients were divided into two groups, depending on whether they were considered to have a high or a low tibial slope. According to Hohmann et al. [18], the cut-off to seperate high and low tibial slope was set at 10°. Within our data, this cut-off is also in accordance to Lee et al. [25], who defined high tibial slope to be the mean + standard deviation.
Statistics
Statistical analyses were performed in correspondence with the Center of Clinical Trials of the University Hospital Regensburg using IBM SPSS Statistics 21.0.0 for Windows.
Data are expressed as median [interquartile range (IQR)] for continuous variables and as absolute numbers (percentage) for categorical variables. Differences between independent groups were assessed using Mann–Whitney tests for continuous variables and Chi-squared tests for nominal variables. If the expected counts were <5, Fisher’s exact test was used. Paired nominal data were analyzed by means of the McNemar test. The odds ratio (OR) for meniscal lesion between high- and low-slope groups was calculated. Intraobserver reliability was assessed by the Intraclass Correlation Coefficient (ICC) and the corresponding 95 % confidence intervals.
All reported p values are two-sided, and a p value of 0.05 was considered the threshold for statistical significance.
Results
The median age of our collective was 27.00 [IQR, 21.00; 40.00] years with 48 male and 23 female patients. Median time from trauma to MRI was 4.50 [IQR, 2.00; 9.25] days and from trauma to surgery 60.00 [IQR, 39.75; 71.25] days. For the patients with meniscal damage, median time to surgery was shorter at 59.50 [IQR, 27.50; 72.00] days, in contrast to 62.50 [IQR, 50.75; 68.75] days for patients without meniscal damage.
ICC for PTS measurements for each patient showed high intraobserver reliability throughout the whole collective with r = 0.987 [0.980; 0.992] for the lateral posterior tibial slope, and r = 0.980 [0.969; 0.988] for the medial posterior tibial slope.
There was no statistical difference between high- and low-slope groups regarding age (LPTS p = 0.720; MPTS p = 0.877) and time to MRI (LPTS p = 0.103; MPTS p = 0.378), however, there was a difference in gender (LPTS p = 1.000; MPTS p = 0.047) with significantly more men having high MPTS. The time to surgery (LPTS p = 0.014; MPTS p = 0.573) was significantly shorter for patients with high LPTS.
The overall incidence of meniscal injuries was 60.6 % (43/71) in the total ACL-deficient knees with 36.6 % (26/71) medial meniscal tears and 32.4 % (23/71) lateral meniscal tears (p = 0.743). 6 patients showed simultaneous damage to both menisci. 41.7 % (20/48) had isolated medial meniscal damage and 37.8 % (17/45) had isolated lateral meniscal damage.
Our results, presented in Table 1, show a continuously higher percentage of meniscal lesion in the high-slope group and an increased OR for damage with this condition.
The overall distribution of meniscal tears is shown in Table 2. Regarding the low-slope group (LPTS: n = 60 and MPTS: n = 63) and the high-slope group (LPTS: n = 11 and MPTS: n = 8), a different distribution of meniscal damage was found.
For steeper LPTS and MPTS, more degeneration of the lateral meniscus was observed; 27.3 % (3/11) to 10.0 % (6/60) for the LPTS and 25.0 % (2/8) to 11.1 % (7/63) for the MPTS, respectively. For steeper LPTS and MPTS, less degeneration of the medial meniscus was observed; 9.1 % (1/11) to 15.0 % (9/60) for the LPTS and 12.5 % (1/8) to 14.3 % (9/63) for the MPTS, respectively.
Also, with both high LPTS and MPTS, an increase in bucket-handle tears for the medial meniscus was shown with 3.3 % (2/60) to 18.2 % (2/11) and 4.8 % (3/63) to 12.5 % (1/8), respectively.
With steeper MPTS, there was an increase in longitudinal tears of the lateral meniscus with 3.2 % (2/63) to 12.5 % (1/8). Radial tears showed no strikingly different pattern. Root tears only appeared with low PTS on the lateral meniscus.
Meniscal lesion spread more frequently to the posterior part of the meniscus. However, as seen in Fig. 4, the proportional number of posterior meniscal lesion decreased from low to high slope.
With 22.5 % (16/71) to 14.1 % (10/71), the medial menisci had been refixated more frequently than resected and were refixated more often than the lateral menisci (14.1 %, 10/71) (p = 0.286). Partial resection was more common with the lateral meniscus (18.3 %, 13/71) (p = 0.678) and was the major technique performed in these cases.
The medial meniscus was refixated more often with high LPTS (80.0 %, 4/5 to 57.1 %, 12/21; p = 0.343) and with high MPTS (66.7 %, 2/3 to 60.9 %, 14/23; p = 0.677). The lateral meniscus only showed more refixation with high MPTS (50.0 %, 2/4 to 42.1 %, 8/19; p = 0.596). However, the results concerning the treatment of the medial and lateral menisci revealed no statistical significance between high- and low-slope groups.
Discussion
The aim of this study was to evaluate the influence of the tibial slope in acute non-contact ACL-insufficient knees on the menisci with associated injury and subsequent treatment. To accomplish this, the intraoperative meniscal findings of ACL-insufficient patients regarding location of the damage and treatment were recorded. The tibial slope was measured on MRI and the patients were divided into low- and high-slope groups.
The association of high tibial slope and ACL insufficiency has been pointed out by previously published biomechanical, case-controlled studies and meta-analysis studies, yet so far, no research has been done to reveal the possible variations of a meniscal lesion due to high tibial slope in the acute ACL-insufficient knee.
We hypothesized that a high tibial slope causes more stress on the menisci in the acute ACL-insufficient knee and is therefore responsible for an increase in the frequency and severity of concurrent meniscal damage and also causes a shift of lesion to the posterior part of the meniscus.
The results of the current study, however, do not seem to support the initial hypothesis entirely.
Meniscal injuries commonly occur in conjunction with ACL tears. Numerous studies have examined the occurrence of these injuries, with their presence being reported as 16–82 % in knees with acute ligament tears [4, 40, 45].
In our study, 60.6 % (43/71) of the patients with an acute ACL lesion showed some meniscal damage, with medial meniscus injuries (36.6 %, 26/71) occurring more often than lateral meniscal injuries (32.4 %, 23/71). Contradictory to our findings, current literature reports lateral meniscal tears to appear more frequently in knees with acute ACL injury than medial meniscal tears, with an average distribution of 56 % lateral to 44 % medial [4, 9, 13, 40]. A possible explanation for our varying findings could be that only patients with non-contact ACL lesion were included in this study, because, due to the contact mechanism in the acute ACL trauma, more damage can be done to the lateral meniscus. Furthermore, our measured results for the PTS are higher than in previous studies using the measuring technique according to Hudek et al. [20, 21, 24]. In general, there is no consensus about when high tibial slope begins. Our cut-off for high tibial slope refers to Lee et al. [25], who defined high tibial slope to be the mean + standard deviation with the values found in literature. For ACL-insufficient patients, measured according to Hudek et al. [21], PTS+ standard deviation has not been reported to be higher than 10° [47]. Increased anterior tibial translation has not only been described in patients with chronic ACL instability, but also in patients with steeper PTS. Both can lead to joint laxity, which is considered to be an independent risk factor for meniscal degeneration next to high sportive activity, higher body mass index and occupational kneeling and squatting [2, 37]. Although our hypothesis, that there is a significant increase in meniscal damage within patients showing steeper PTS, could not be confirmed, the percentages of medial as well as lateral meniscal lesions were steadily higher within the high PTS group.
A reason for the increasing number of medial meniscal tears in the acute ACL-insufficient knee with high tibial slope might be that the medial meniscus acts like a wedge against anterior tibial translation [1, 19, 22, 26] and limits its extendibility. As the medial meniscus is fixed to the tibia, its movement is restricted [40, 44]. That is why the medial meniscus, especially the posterior horn, stabilizes in the sagittal plane and, on the basis of tibial translation occurring with ACL insufficiency and high tibial slope, is exposed to higher stress, thus being responsible for an increased number of medial meniscal damage in chronic ACL lesion [4, 8, 25, 36, 40, 45]. In our study, 84.6 % (22/26) of the medial meniscal lesions and 87.0 % (20/23) of the lateral meniscal lesions spread to its posterior part. For the occurrence of bucket-handle tears, which also spread to the posterior horn, different mechanisms of injury are suggested. With high PTS, more damage was done to the posterior horn, respectively, the intermediate part and posterior horn than to all other parts of the menisci. Since the difference was not statistically significant and the fact that fewer posterior meniscal lesions could be found with high tibial slope than with low tibial slope, it does not support our initial hypothesis of a significantly increased damage to the posterior site of the menisci due to high PTS. This finding might indicate that the mechanism of impingement of the posterior part of the menisci as a major factor of lesion in the acute ACL-insufficient knee is less accurate, and meniscal damage could be better explained with occurring shear forces in those patients.
Moreover, a high tibial slope does not have a statistically significant influence on the incidence of a medial meniscus lesion in an acute ACL-deficient knee. However, there seems to be an impact on the type and severity of the medial meniscus lesion. Bucket-handle tears could be seen more often in patients with high PTS. These kinds of tears usually occur when severe stress is used on the medial compartment.
The lateral meniscus, however, is much more mobile and therefore less prone to meniscal injury due to impingement. For the higher frequency of lateral meniscal lesions in the high-slope group, we support the assumption of Tanaka et al. [38], presuming that steeper slope on the lateral tibial plateau and missing stabilization due to ACL insufficiency can lead to a high-grade pivot shift maneuver using the medial tibial plateau as a pivot point, forcing more stress on the lateral compartment of the knee. It might, therefore, be responsible for higher force transmission onto the lateral meniscus with consecutive higher number of lateral meniscal lesion in the acute ACL-insufficient knee with high LPTS.
If these tears are left untreated, they can lead to premature osteoarthritis with significant pain and morbidity for the patient [2, 23, 30]. As a result, partial meniscectomy and refixation techniques are a common procedure performed for its treatment.
Degenerative joint changes after ACL reconstruction with meniscectomy have been reported before. That is why the preservation of meniscal tissue and its function, which can be achieved best by meniscal refixation, is critical for long-term knee function [34]. Refixation techniques have significantly improved the attempt to restore meniscal integrity in the ACL-insufficient patient when combined with ACL reconstruction [7, 32, 39], showing an estimated >90 % randomized clinical success rate after a 2-year follow-up for both all-inside and inside-out repairs [41]. These results could be explained by a significant release of growth factors during ACL reconstruction [15], which improves the prognosis and internal healing of meniscal tears that have been refixated. That is why the likelihood of a successful meniscal repair might be enhanced enormously when combined with ACL reconstruction, and maximal meniscal preservation could be achieved best immediately after ACL injury with simultaneous repair of coexisting peripheral meniscus tears. But even without ACL reconstruction, meniscal tears in the red–white zone showed an acceptable midterm clinical healing rate in a systematic review by Barber-Westin et al. [3].
In our study, the percentage of repairable meniscal tears in acute ACL-insufficient patients was higher on the medial (61.5 %) than on the lateral side (43.5 %). These percentages further increase in cases of the medial meniscus with high LPTS (from 57.1 to 80.0 %) and MPTS (from 60.9 to 66.7 %) and for the lateral meniscus with high MPTS (from 42.1 to 50.0 %).
These numbers of primary meniscal refixation are significantly higher than reported in previously published literature, with only 27 and 14 % repaired menisci in contrast to 63 and 71 % resected menisci on the medial and on the lateral side, respectively [34]. These contrasting findings might be due to our young patient clientele of only 27 years [33] and the acute state of meniscal tears which, in general, show higher potential of internal healing. Furthermore, all surgeries were done by experienced sports medicine fellowship-trained orthopedic surgeons, who are more likely to perform meniscal repair than a general orthopedic surgeon or other fellowship-trained surgeons [33].
This high rate of meniscal refixation might be an important observation, as Bellabarba et al. [4] found the percentage of repairable meniscal tears decreased overall with the chronicity of ACL insufficiency. This indicates a chance for the acute ACL-insufficient patient with high slope to restore meniscal integrity not only on the medial side, where this technique has been primarily performed in both low and high PTS groups, but also on the lateral side, to prevent the patient from early-onset osteoarthritis. As the menisci undergo severe impact loads in knees with high tibial slope, the tendency of instability in the sagittal plane rises, therefore, the key to successful ACL reconstruction in patients with high tibial slope and subsequent meniscal damage might lie in reducing resulting forces on the menisci [4, 43].
Some limitations apply to the current study. Information regarding previous trauma was gleaned from self-administered patient questionnaires, which is subject to recollection bias on behalf of the patient. Other risk factors for secondary meniscal damage have also not been included, such as BMI and activity level. To define the exact point of meniscal damage, serial MRI would be necessary, including directly after the traumatic incident. However, some patients did not receive an MRI directly after the incident. Due to our strict exclusion criteria and the high number of patients required, it was not possible to obtain the same imaging in all patients, since the diagnostic MRI was performed in various institutions. For our study, the quality guidelines of the German Medical association were applied. These included the minimal three planes (coronal, sagittal and axial) with T1-weighted as well as T2-weighted or fat-suppressed-T2-weighted and/or proton-density-weighted images or fat-suppressed PD images, with layer thickness being 4 mm or less.
Conclusion
The focus of this work was to find out how high tibial slope is associated with a risk of injury to the menisci. This information is necessary to gain a complete understanding of the combinations of risk factors—both modifiable and non-modifiable—for ACL injury and subsequent meniscal damage, from which a comprehensive multivariate model of injury risk can be determined. Supporting the findings in the frequency of concurrent lesions, an increased OR for suffering from meniscal damage in an acute ACL lesion suggests that a high posterior tibial slope is a predetermining factor, but at the same time does not influence the location of the meniscus tear (i.e., there was no tendency towards a more posterior location of the tear in knees with high tibial slope).
These findings are clinically relevant when high slope shows in imaging, especially in MRI. With ACL insufficiency, special focus should be made on detecting hidden lesions of the medial and lateral meniscus during arthroscopy.
However, there was no statistical significance to support the initial hypothesis. Further research is needed to find out if other factors than tibial slope are risk factors for meniscal lesion in acute ACL injury.
References
Allen C, Wong E, Livesay G, Sakane M, Fu F, Woo S (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18(1):109–115
Baker P, Coggon D, Reading I, Barrett D, McLaren M, Cooper C (2002) Sports injury, occupational physical activity, joint laxity, and meniscal damage. J Rheumatol 29(3):557–563
Barber-Westin S, Noyes F (2014) Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy 30(1):134–146
Bellabarba C, Bush-Joseph C, Bach B (1997) Patterns of meniscal injury in the anterior cruciate-deficient knee: a review of the literature. Am J Orthop 26(1):18–23
Bonnin M, Carret J, Dimnet J, Dejour H (1996) The weight-bearing knee after anterior cruciate ligament rupture. An in vitro biomechanical study. Knee Surg Sports Traumatol Arthrosc 3(4):245–251
Butler D, Noyes F, Grood E (1980) Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am 62(2):259–270
Cannon W, Vittori J (1992) The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 20(2):176–181
Church S, Keating J (2005) Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br 87(12):1639–1642
Cipolla M, Scala A, Gianni E, Puddu G (1995) Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees. Classification, staging and timing of treatment. Knee Surg Sports Traumatol Arthrosc 3(3):130–134
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br 76(5):745–749
DeMorat G, Weinhold P, Blackburn T, Chudik S, Garrett W (2004) Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med 32(2):477–483
Feucht M, Mauro C, Brucker P, Imhoff A, Hinterwimmer S (2013) The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 21(1):134–145
Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W (2014) The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy 30(7):833–840
Giffin J, Vogrin T, Zantop T, Woo Savio L Y, Harner C (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2):376–382
de Girolamo L, Galliera E, Volpi P, Denti M, Dogliotti G, Quaglia A, Cabitza P, Corsi Romanelli MM, Randelli P (2015) Why menisci show higher healing rate when repaired during ACL reconstruction? Growth factors release can be the explanation. Knee Surg Sports Traumatol Arthrosc 23(1):90–96
Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck J, Schutt R, Dabezies E, Beynnon B (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62
Herfat S, Boguszewski D, Nesbitt R, Shearn J (2012) Effect of perturbing a simulated motion on knee and anterior cruciate ligament kinetics. J Biomech Eng 134(10):104504
Hohmann E, Bryant A, Reaburn P, Tetsworth K (2010) Does posterior tibial slope influence knee functionality in the anterior cruciate ligament-deficient and anterior cruciate ligament-reconstructed knee? Arthroscopy 26(11):1496–1502
Hsieh H, Walker P (1976) Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am 58(1):87–93
Hudek R, Fuchs B, Regenfelder F, Koch P (2011) Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res 469(8):2377–2384
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch P (2009) Novel Measurement Technique of the Tibial Slope on Conventional MRI. Clin Orthop Relat Res 467(8):2066–2072
Indelicato P, Bittar E (1985) A perspective of lesions associated with ACL insufficiency of the knee. A review of 100 cases. Clin Orthop Relat Res 198:77–80
Kessler M, Behrend H, Henz S, Stutz G, Rukavina A, Kuster M (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16(5):442–448
Khan M, Seon J, Song E (2011) Risk factors for anterior cruciate ligament injury: assessment of tibial plateau anatomic variables on conventional MRI using a new combined method. Int Orthop 35(8):1251–1256
Lee J, Choi Y, Shin K, Choi C (2011) Medial meniscal tears in anterior cruciate ligament-deficient knees: effects of posterior tibial slope on medial meniscal tear. Knee Surg Relat Res 23(4):227
Levy I, Torzilli P, Warren R (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64(6):883–888
Lipps D, Oh Y, Ashton-Miller J, Wojtys E (2012) Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med 40(1):32–40
Lipps D, Wilson A, Ashton-Miller J, Wojtys E (2012) Evaluation of different methods for measuring lateral tibial slope using magnetic resonance imaging. Am J Sports Med 40(12):2731–2736
Lipps D, Wojtys E, Ashton-Miller J (2013) Anterior cruciate ligament fatigue failures in knees subjected to repeated simulated pivot landings. Am J Sports Med 41(5):1058–1066
Lohmander L, Englund P, Dahl L, Roos E (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756–1769
McLean S, Oh Y, Palmer M, Lucey S, Lucarelli D, Ashton-Miller J, Wojtys E (2011) The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am 93(14):1310–1317
Morgan C, Wojtys E, Casscells C, Casscells S (1991) Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med 19(6):632–638
Musahl V, Jordan S, Colvin A, Tranovich M, Irrgang J, Harner C (2010) Practice patterns for combined anterior cruciate ligament and meniscal surgery in the United States. Am J Sports Med 38(5):918–923
Noyes F, Barber-Westin S (2012) Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy 28(1):123–130
Oh Y, Lipps D, Ashton-Miller J, Wojtys E (2012) What strains the anterior cruciate ligament during a pivot landing? Am J Sports Med 40(3):574–583
Smith J, Barrett G (2001) Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med 29(4):415–419
Snoeker Barbara A M, Bakker Eric W P, Kegel Cornelia A T, Lucas C (2013) Risk factors for meniscal tears: a systematic review including meta-analysis. J Orthop Sports Phys Ther 43(6):352–367
Tanaka M, Vyas D, Moloney G, Bedi A, Pearle A, Musahl V (2012) What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc 20(4):737–742
Tenuta J, Arciero R (1994) Arthroscopic evaluation of meniscal repairs: factors that effect healing. Am J Sports Med 22(6):797–802
Thompson W, Fu F (1993) The meniscus in the cruciate-deficient knee. Clin Sports Med 12(4):771–796
Toman C, Dunn W, Spindler K, Amendola A, Andrish J, Bergfeld J, Flanigan D, Jones M, Kaeding C, Marx R, Matava M, McCarty E, Parker R, Wolcott M, Vidal A, Wolf B, Huston L, Harrell F, Wright R (2009) Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med 37(6):1111–1115
Torzilli P, Deng X, Warren R (1994) The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med 22(1):105–112
Vermesan D, Prejbeanu R, Laitin S, Georgianu V, Haragus H, Nitescu S, Tatullo M, Tattoli M, Caprio M, Cagiano R (2014) Meniscal tears left in situ during anatomic single bundle anterior cruciate ligament reconstruction. Eur Rev Med Pharmacol Sci 18(2):252–256
Warren L, Marshall J (1979) The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 61(1):56–62
Wickiewicz T (1990) Meniscal injuries in the cruciate-deficient knee. Clin Sports Med 9(3):681–694
Wordeman S, Quatman C, Kaeding C, Hewett T (2012) In vivo evidence for tibial plateau slope as a risk factor for anterior cruciate ligament injury: a systematic review and meta-analysis. Am J Sports Med 40(7):1673–1681
Zeng C, Cheng L, Wei J, Gao S, Yang T, Luo W, Li Y, Xu M, Lei G (2014) The influence of the tibial plateau slopes on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22(1):53–65
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The study was conducted according to the regulations and guidelines of the ethics committee of the University of Regensburg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markl, I., Zantop, T., Zeman, F. et al. The effect of tibial slope in acute ACL-insufficient patients on concurrent meniscal tears. Arch Orthop Trauma Surg 135, 1141–1149 (2015). https://doi.org/10.1007/s00402-015-2247-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2247-1