Abstract
Introduction
Rotating-hinge knee implants are highly constrained devices able to provide the stability needed for arthroplasty in case of severe bone loss and complex instability. Notable doubts still exist in using rotating-hinge devices, mainly due to risk of mechanical failure and risk of infection.
Materials and methods
We retrospectively evaluated the functional and clinical outcomes in a series of patients treated with the rotating-hinge Endo-Model prosthesis either for primary or revision total knee arthroplasty. Between 1997 and 2009 we implanted 123 Endo-Model prosthesis (118 patients) at our institution. At the time of this study we could evaluate 45 prosthesis (25 primary and 20 revision TKAs) from the clinical and radiological site, with average follow-up of 42.2 months.
Results
During the follow-up period, three patients reported complications, which in two cases finally led to revision with explantation. Mean survival of the implants attested at 93.3 %. The average post-operative clinical Knee Society score in the evaluated series was 94.2, the functional one 78.7. The average range of motion was 0°–108°. No signs of joint instability or misalignment were noted. Pain was present in a minority of patients, but always at a mild/occasional extent. No evidences of loosening or implant failure have been reported. No substantial divergences in the outcomes have been found across different patient categories after stratification in agreement with the Knee Society.
Conclusions
Coherent with previously published works, we confirm the Endo-Model prosthesis to provide excellent pain relief, restoration of walking capacity and intrinsic knee stability both in complex primary and in revision knee arthroplasty, with good or excellent results in the majority of patients and acceptable complication rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Constraint is defined as the effect of elements of the knee implant design that provide stability needed in presence of a deficient soft tissue envelope. The choice of an adequate constraint degree, while planning a total knee arthroplasty, represents one of the fundamental factors upon which the successful outcome depends [1, 2]. In severely affected knee with serious bony and ligamentous defects, a high constrained total knee device represents a treatment option able to restore and maintain the correct anatomical axis as well as to confer the joint stability impossible to obtain with lower constraint implants [3]. Rotating-hinge designs are described to deal with such instances of severe loss of bone stock, gross ligamentous instability, combined deformities, oncologic surgery and salvage situations both in primary and revision surgery. By mean of the rotational degree of freedom and design features these implants provide high constraint and great inherent stability while avoiding patellofemoral instability and torsional stresses to load at the prosthesis/cement/bone interface [1, 3]. This finally leads to longer survival and better clinical outcomes with respect to previous rotating-hinged devices, despite contradictory results are present in the literature.
Notable doubts still exist in using rotating-hinge devices, mainly due to risk of mechanical failure and risk of infection, with variable survival rates and outcomes ranging from excellent to poor [4–7]. Despite recent encouraging reports, a clear answer to the rising question of whether the outcome quality is implant specific, or rather more generally published outcomes are conditioned by the concept itself of a rotating-hinge prosthesis, is still lacking.
The purpose of this study was to retrospectively evaluate the clinical, functional and radiographic outcomes in a series of patients treated with the long-stemmed cemented Endo-Model® rotating-hinge prosthesis (Waldemar Link GMBH & Co, Hamburg, Germany) (Fig. 1) both in complex primary surgery and revision setting.
Patients and methods
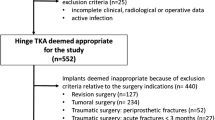
Between January 1997 and December 2009 we performed 123 total knee arthroplasties (TKA) in 118 patients with the Endo-Model prosthesis, at our institution. Of these, 75 were primary implants and 48 revisions. The drop out proportion was 64.4 %, involving 76 patients. Of these patients, 23 died for unrelated causes, 12 were unwilling to participate in the study, 22 were unable to participate because of medical comorbidities, and 19 were lost during follow-up. At the time of this study we could evaluate 42 patients and 45 prosthesis (25 primary and 20 revision TKAs). For the evaluated knees, indications for surgery are summarized in Table 1. When considering both primary and post-traumatic osteoarthritis (OA), we chose the Endo-Model device for those patients showing severe axial deformities and/or gross instability. Rheumatoid patients were always subjected to multiple arthritis, with severely impaired knee joint and ligamentous laxity. In the revision setting, implant loosening with high degree of bone loss, as well as severe residual instability and comminuted periprosthetic fractures were the indications for surgery. The average follow-up was 42.2 months (range 20–128 months). There were 38 female and 4 male in our study. The mean age at the time of surgery was 74 years (range 50–84 years). Informed consent was obtained from all patients for being included in the present study.
All operations were performed using the tourniquet at the tight and a combination of intramedullary femoral and extramedullary tibial alignment guides. We used the same approach in all cases, involving a straight midline incision combined with a medial parapatellar arthrotomy and lateral patella luxation. Both spaces (flexion and extension) had been balanced using spacers to obtain a good range of motion. The patella was never resurfaced. In all cases we used a cemented long-stemmed implant with patellar flange, anti-luxation device and rotational feature. Antibiotic-loaded cement was used in case of revision surgery. All of the procedures were carried out by the senior author (FF), in a standard operating theater. A prophylactic, first-generation cephalosporin was used peri-operatively and for 2 days post-operatively. Thromboprophylaxis was conducted by mean of low-molecular weight heparin administration peri- and post-operatively for 35 days. After removal of the suction drain, usually on the second post-operative day, patients began knee motion using a continuous passive motion machine (Kinetec CPM System, Patterson Medical, Warrenville, IL) for about 2 h daily. Full weight bearing was allowed after 4 days using 2 canes. Patients were discharged soon after the first week and continued the rehabilitation program for three more weeks in a dedicated center.
Besides routine post-operative controls (at 3, 6, 12 months after surgery, and annually thereafter) all of the enrolled patients were further evaluated in a single follow-up solution, in which data were collected for this study, by mean of clinical and functional analysis. In this setting, the post-operative Knee Society rating system (0–100 clinical, 0–100 functional) was determined for each evaluated knee [8] and new radiographs obtained. Complete preoperative and post-operative data were present for the total of the enrolled patients. Three authors (FF, FS, TM) independently examined anteroposterior and lateral radiographs at latest follow-up for gross signs of loosening such as progressive radiolucencies, changes in implant position, dislocation or breakage of the implant, signs of instability or malalignment. No radiographic rating system was used. Data were collected and statistically analyzed. We reported categorical variables as frequencies (percent) and continuous variables as means ± standard deviations (sd). For comparing continuous variables, we used the Mann–Whitney U test for two unpaired groups and the Kruskal–Wallis test for more than two groups. A p value <0.05 was considered to be statistically significant.
Results
Survivorship analysis
Defining failure as revision for any reason, mean prosthesis survival in the evaluated series was 95.5 % (95 % confidential interval CI 89.4–100 %) at 1 year and 93.3 % (95 % CI 85.8–100 %) at 5 years from surgery (96 % for primary, 95 % for revision implants). This value then remained stable until the end of the follow-up period. Failure of the implant was reported in three cases and in two of them resulted in explantation, leaving 43 implants available for subsequent clinical and radiographic evaluation.
Clinical and radiographic findings
Patients enrolled in the study were clinically and functionally evaluated at latest follow-up visit with definition of the Knee Society score and assessing of individual satisfaction degree. A broad analysis of recent and precedent radiographs was carried out. 24 primary implants and 19 revision implants were evaluated.
The mean post-operative active knee flexion was 108º (range 70º–125º). Extension deficits were present in two knees, ranging from 5º to 10º, probably due to femoral component positioning in slight flexion, without consequences on pain and function. No extensor mechanism deficits were found in the evaluated series. Mean Knee Society clinical score was 94.2 (range 71–100). Mean functional score was 78.7 (range 0–100). We did not find significant differences between Knee Society scores in primary and revision implants (outcomes are summarized in Table 2). Stratification of the patients in categories as suggested by the Knee Society also revealed no substantial differences, despite a lower value in the functional score in the C category (Table 2). We found neither evidence of post-operative tibiofemoral instability nor deficiencies at the knee extensor mechanism. Pain was present in 9 out of 43 knees (7 revision and 2 primary implants), but always at a mild or occasional extent, never compromising day-life activities. In one case pain was mainly referred to the patellar bone, despite no evidence of patellar maltracking.
20 out of 40 patients were highly satisfied, 12 moderately satisfied with the outcome. A low satisfaction degree was reported in eight patients: of note, belonging to this group were five patients with extremely low functional outcome often related to multiple arthritis or medical infirmity (i.e. C category patients) and three young and active patients who complained pain or discomfort while walking and climbing the stairs. At the time of the study, 10 patients did not use any aid in outdoor walking, 28 patients had to use one or two canes, and 2 patients where wheelchair bounded.
In the X-rays analysis, there was no evidence of changes in the tibiofemoral alignment in comparison with early post-operative radiographs. No signs of implant loosening (progressive radiolucencies or component migration) or breakage of the implant were found, as well as signs of polyethylene wear. Furthermore, no evidence was found of cortical hyperostosis around the stems of the components.
Complications
One intra-operative complication was observed, with perforation of the femoral shaft and minimal cement effusion, in a revision surgery setting. Passive physical therapy was allowed immediately after surgery, and full weight bearing 1 week later. This patient underwent no consequences from the clinical or functional point of view.
Reported failures include two dislocations and one deep infection. One case of dislocation was due to malposition of the polyethylene tibial plateau during the surgical procedure for primary TKA. Ten months after surgery, this finally led to explantation of the device, but the revision procedure was carried out in other orthopaedic structure and we presently lack any other information about this patient. A second case of dislocation was due to accidental trauma occurring in the rehabilitation period in a patient receiving Endo-Model for aseptic loosening of a primary TKA implant. Early surgical management with substitution of the polyethylene plateau resulted in satisfactory outcome. At the time of this study, 5 years after surgery, the patient was pain free and no sign of instability was present. She received 98 clinical and 100 functional knee score and was completely satisfied of her knee (Fig. 2). The unique case of deep infection was reported in a 56-year-old patient who received the Endo-Model device as a revision implant after septic mobilization of a primary TKA. Four years after surgery, she underwent an infection relapse, and the Endo-Model prosthesis was substituted with a similar constrained implant through a two-staged procedure. No cases of deep-vein thrombosis were reported.
a X-rays of a case of early traumatic dislocation of the prosthetic components treated with surgical reduction and polyethylene substitution; black dots have been used to highlight the dislocated tibial tooth. b Radiographic analysis at the time of the study, 5 years after revision surgery. c–g Clinical evaluation at the time of the study
Discussion
Rotating-hinge total knee prosthesis are widely used implants for the treatment of severely deformed knees as well as in revision knee surgery, when dealing with extensive osteolysis, massive bone loss and persistent complex instability [1, 9–11]. Rotating-hinge devices confer great inherent stability to the knee by mean of a link between the tibial and femoral components that restricts varus–valgus and translational stresses. These components permit rotation of the tibial bearing around a yoke on the tibial platform, then reducing the stresses transmitted to the implant/cement/bone interface and the risk of loosening or early failure as well. Outcomes associated with recent rotating-hinge devices yield a substantially better clinical result and implant survival compared to suboptimal outcomes of earlier designs [11]. However, published results using this kind of implants for nontumor reconstruction have varied from acceptable to poor, leaving unsolved general questions about safety, survival and functional results [2–7, 9, 11–24]. Furthermore, whether these differences relate to specific design features or to the general concept of a rotating-hinged implant is still unclear [4]. Our study was carried out to contribute to this still running controversy while determining survival rate and clinical, functional and radiographic outcomes in a series of patients who received the Endo-Model rotating-hinge knee prosthesis at our institution, either for primary or revision knee surgery.
This study has several shortcomings. First, it is a retrospective study and the number of patients is limited. Similar to other works [3, 4, 11, 17–19, 27], in our series the average age of patients was high at the time of surgery (74 years): the high mortality rate in these patients during the follow-up period as well as the impossibility to participate in the study due to advanced age and medical comorbidities are important factors in determining the consistent drop out proportion. The use of the Endo-Model rotating-hinge is mainly based on surgeon experience, and this could represent an important bias for the use of this device and the associated clinical outcomes. However, the relative ease of the surgical technique and simplicity of the instrumentations with respect to previous rotating-hinge implants should be regarded as important features, allowing a high degree of reproducibility.
The Endo-Model prosthesis we used is a fully cemented non-modular implant with long intramedullary stems, endowed with patellar flange, anti-luxation device and rotational feature. Despite some concerns from several authors, regarding the long cemented stems, our study supports this prosthetic design and confirms its ability in tolerating forces at the bone/cement/prosthesis interface without increasing the aseptic loosening rate. Non-cemented press-fit stems are now available from the manufacturer for both femoral and tibial components; these will avoid the technical complexities with cement removal in case of revision surgery. Despite the high degree of constraint, the implant we used was not associated with cases of early dramatic loosening, massive failures or component ruptures due to abnormal stress transfer: this is in line with other authors’ data [24, 25] and indirectly confirms the biomechanical reliability of the prosthetic design. The average follow-up in our series was 42.2 months. We evaluated 25 primary and 20 revision implants. At the time of the study mean survival rated 93.3 %. Mean clinical and functional KSS were 94.2 and 78.7, respectively, with mean active knee flexion of 108º. Reported data are coherent with previously published results about this kind of implant [3, 11, 22–28]. In line with a recent work from Efe et al. [26], despite a slight flexion in the mean functional score we did not find statistically significant differences when comparing results obtained in the primary surgery group and in the revision group of patients. Similar results were obtained when comparing outcomes after patients’ stratification in agreement with the Knee Society suggested categories. In their works, some authors reported lower values of functional score [3, 22–27]. This could be ascribed to follow-up longer than ours, to different proportion of primary and revision TKAs, and to different incidence and severity of comorbidities in the evaluated series as well [7].
In our series, pain was present in 21 % of patients: it never represented a limiting factor in day-life activities, but greatly influenced the subjective degree of satisfaction, especially in younger and more active patients. We do not routinely resurface the patella, but we always pay great attention in correcting patellofemoral alignment and patellar tracking. Anterior knee pain was present in one patient, in our series, despite no evidence of patellar maltracking. We hypothesize pain could be ascribed, in this case, to the underlying rheumatoid arthritis [3].
Neither sign of residual tibiofemoral instability was noted, nor radiographic signs of component loosening or subsidence. Only one case of deep infection was reported, in a patient who received the Endo-Model prosthesis in a two-stage revision setting for previous septic mobilization. On the other side, no infections occurred in the primary surgery group of patients. Some authors have previously described problems with dislocation of the Endo-Model implant, despite an anti-dislocation feature [5, 6, 20]. In our series we observed two cases of tibiofemoral dislocation. One of these was due to incorrect surgical technique. The other one followed accidental trauma during the rehabilitation program. No cases of dislocation due to imbalance of the flexion–extension gap and consequent instability were noted [3, 6]. Global revision rate attested at 6.7 %.
As the population gets older, the revision burden increase and complex primary knee surgeries as well. Reconstruction with rotating-hinge total knee prosthesis can provide substantial improvement in function and reduction in pain in severely affected knee. Several published works carried out skeptic conclusions about the use of these kind of implants because of high risk of complications due to its constrained characteristics and difficulties in case of revision. We agree with authors suggesting rotating-hinge prosthesis should be reserved to elderly low-demanding patients and salvage situations. Nevertheless, we confirm results observed since the historical work of Engelbrecht et al. [29], and we believe the Endo-Model implant represents a suitable solution both in complex primary and revision surgery, able to provide good or excellent clinical results in the majority of patients. Despite some limitations arising from being a non-modular system, this implant requires limited bone resections with respect to other rotating knees and CCK implants, and shows a high degree of adaptability to the majority of the anatomic and clinical situations. This feature will be further enhanced and the surgical technique further eased by the introduction of modular components [30].
It is difficult to compare different kinds of prosthesis, even if they share the same design, because of heterogeneity in the series and different follow-up times. It is of note, however, that among published results about prosthesis with rotating-hinge design, the Endo-Model prosthesis is commonly associated with excellent survival rates and limited variability among different series (Table 3). Our results support the use of Endo-Model in patients with deformed or malaligned knees, in presence of serious bony and ligamentous defects, both in primary and revision surgery. When considering other authors’ data and ours, we are confident the hypothesis that published variable results could be related to the concept itself of a rotating-hinge device seems at least questionable. Further implant-specific revision studies and indication-oriented revision studies are auspicated. While attention should always be paid to adequate surgical technique and correct indications for surgery, the Endo-Model device remains a viable option in knee surgery for most difficult cases.
References
Morgan H, Battista V, Leopold SS (2005) Constraint in primary total knee arthroplasty. J Am Acad Orthop Surg 13:515–524
Sculco TP (2006) The role of constraint in total knee arthroplasty. J Arthroplasty 21(4 Suppl 1):54–56
Petrou G, Petrou H, Tilkeridis C, Stavrakis T, Kapetsis T, Kremmiddas N, Gavras M (2004) Medium-term results with a primary cemented rotating-hinge total knee replacement. J Bone Jt Surg 86-B:813–817
Berend KD, Lombardi AV (2009) Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res 467:485–492
Pacha-Vincente D, Malik A, Castellet-Feliu E, Nardi-Vilardaga J (2008) Dislocation of rotating hinge knee prosthesis with antidislocation mechanism. J Arthroplasty 23(2):299–303
Wang CJ, Wang HE (2000) Early catastrophic failure of rotating hinge total knee prosthesis. J Arthroplasty 15(3):387–391
Guenoun B, Latargez L, Freslon M, Defossez G, Salas N, Gayet LE (2009) Complications following rotating hinge Endo-Modell (Link) knee arthroplasty. Orthop Traumatol Surg Res 95:529–536
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Barrack RL (2001) Evolution of rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res 392:292–299
Barrack RL (2002) Rise of rotating hinge in revision total knee arthroplasty. Orthopaedics 25(10):1020–1021
Pradhan NR, Bale L, Kay P, Porter ML (2004) Salvage revision total knee replacement using the Endo-Model rotating hinge prosthesis. Knee 11:469–473
Back DL, David L, Hilton A, Blunn G, Briggs TW, Cannon SR (2008) The SMILES prosthesis in salvage revision knee surgery. Knee 15:40–44
Barrack RL, Lyons TR, Ingraham RQ, Johnson JC (2000) The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty 15:858–866
Jones RE, Barrack RL, Skedros J (2001) Modular, mobile-bearing total knee arthroplasty. Clin Orthop Relat Res 392:306–314
Jones RE, Skedros JG, Chan AJ, Beauchamp DH, Harkins PC (2001) Total knee arthroplasty using the S-ROM mobile-bearing hinge prosthesis. J Arthroplasty 16:279–287
Lombardi AV Jr, Mallory TH, Eberle RW, Adams JB (1997) Rotating hinge prosthesis in revision total knee arthroplasty: indications and results. Surg Tech Int 6:379–382
Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF (2007) Rotating hinged knee replacement: use with caution. J Bone Jt Surg 89:1735–1741
Springer BD, Hanssen AD, Sim FH, Lewallen DG (2001) The kinematic rotating hinge prosthesis for complex knee arhtroplasty. Clin Orthop Relat Res 392:283–291
Springer BD, Sim FH, Hanssen AD, Lewallen DG (2004) The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res 421:181–187
Ward WG, Haight D, Ritchie P, Gordon S, EcKardt JJ (2003) Dislocation of rotating hinge total knee prosthesis: a biomechanical analysis. J Bone Jt Surg Am 85:448–453
Westrich GH, Mollano AV, Sculco TP, Buly RL, Laskins RS, Windsor S (2000) Rotating hinge total knee arthroplasty in severely affected knees. Clin Orthop Relat Res 379:195–208
Gudnason A, Milbrink J, Hailer NP (2011) Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg 131(11):1601–1607
Yang JH, Yoon JR, Oh CH, Kim TS (2012) Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc 20(3):517–523
Bistolfi A, Lustig S, Rosso F, Dalmasso P, Crova M, Massazza G (2013) Results with 98 Endo-Modell rotating hinge prostheses for primary knee arthroplasty. Orthopaedics 36(6):e746–e752
Bistolfi A, Rosso F, Crova M, Massazza G (2013) Endo-Modell rotating-hinge total knee for revision total knee arthroplasty. Orthopaedics 36(10):e1299–e1306
Efe T, Roessler PP, Heyse TJ, Hauk C, Pahrmann C, Getgood A, Schmitt J (2012) Mid-term results after implantation of rotating-hinge knee prostheses: primary versus revision. Orthop Rev 4(e35):155–159
Joshi N, Navarro-Quilis A (2008) Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty 23(8):1204–1211
Argenson J, Aubaniac JM (2000) Total knee arthroplasty in femorotibial instability. Orthopäde 29:S45–S47
Engelbrecht E, Nieder E, Strickle E, Keller A (1981) Intracondylare Kniegelenksendo-prosthese mit Rotationsmöglichkeit Endo-Modell. Chirurg 52:368–375
Zhang F, Liu Y, Xiao Y, Liu W (2014) Clinical outcomes of primary rotating-hinge knee arthroplasty for knees with severe deformity. Chin Med J 127(9):1791–1793
Conflict of interest
The authors, their immediate family and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article. The authors state that they have full control of all primary data and that they agree to allow the journal to review their data if requested.
Ethical standards
IRB approval: the IRB and Regional Ethical Committee were made aware of this work and of the submission of our data for publication, and gave formal approval. The study received the registration number 73/2014. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanguineti, F., Mangano, T., Formica, M. et al. Total knee arthroplasty with rotating-hinge Endo-Model prosthesis: clinical results in complex primary and revision surgery. Arch Orthop Trauma Surg 134, 1601–1607 (2014). https://doi.org/10.1007/s00402-014-2061-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2061-1