Abstract
Purpose
A rotating-hinge total knee prosthesis may be utilized for the treatment of global instability or severe bone loss around the knee. The outcome of primary total knee arthroplasty (TKA) using Endo-Modell (Link®) rotating-hinge prosthesis was evaluated.
Methods
Retrospectively, review of 50 cases (40 patients) at a mean follow-up of 15 years (range, 10–18) who underwent primary TKA using Endo-Modell (Link®) was performed. Indications included severe primary osteoarthritis with substantial ligament laxity, severe rheumatic arthritis with extreme ligament instability and bone loss, supracondylar nonunion, charcot arthropathy, and posttraumatic arthritis. Knee Society Score (KSS) and radiographic analysis were done for preoperative and at latest follow-up. Statistical analysis was done using the Student’s t test with the level of significance of p < 0.05.
Results
Overall, the rotating-hinge arthroplasty resulted in improved knee functioning. The KSS improved (p < 0.001) from a preoperative mean of 38 ± 14.3 (SD) points to a postoperative mean of 73 ± 12.8 points; the functional score improved (n.s.) from 36 ± 19.5 points to 47 ± 23.5 points. Mean range of motion at the most recent clinical follow-up evaluation was 102 ± 9°. However, all (100%) patients needed some form of assisted devices for walking and a relatively large number of deep infections (14%) were encountered.
Conclusions
Reconstruction with a rotating-hinge total knee prosthesis provided substantial improvement in function and reduction in pain. However, the possibility of assisted walking and high rate of deep infection should be encountered.
Level of evidence
Retrospective therapeutic study, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Competent and functional collateral ligaments are a prerequisite when performing a conventional total knee arthroplasty (TKA) [22]. In patients undergoing primary surgery for knees with grossly unstable or lost ligament stability and bone integrity, standard condylar implants do not allow for proper stabilization of the joint, even when using models with constraint. Under these circumstances, condylar TKA designs will fail within a short period of time [34].
Rotating-hinge total knee prostheses may be used for the treatment of global instability or severe bone loss around the knee. Hinged prostheses were first designed and used for knee reconstruction after the resection of neoplasms. The first hinge prosthesis was designed in the 1950s by Judet and by Walldius and Shiers [2]. The initial joint mechanism consisted in a fixed hinge with no rotational motion. A second generation modified several aspects (rotational axis with a stop, new design of the patellofemoral joint to facilitate the patella’s displacement, appearance of a metallic tibial baseplate to reduce polyethylene wear, and improvements in the stems to facilitate osteofixation). These improvements led to appearance of several models, with the main models being the GUEPAR implant in 1970 [4, 16], the Stanmore prosthesis in 1971 [8], and the Saint Georg by Engelbrecht, Nieder, Keller, and Strickel prosthesis in 1979 (ancestor of the Endo-Modell (Link®)) [6, 17]. Developers have further introduced a flexing and rotating system such as Endo-Modell (Link®) rotating-hinge knee prosthesis which aimed to avoid the torsional stresses that lead to loosening of the prosthesis [12, 25].
Previous reports treated by modern rotating-hinge prostheses are difficult to compare because several different types of prostheses were often used and with mixed primary/revision cohort [9, 11, 23, 35]. In this report, a long-term (more than 10 years) clinical/radiographic results of primary 50 Endo-Modell (Link®) rotating-hinge TKA performed for patients with severe instability or bone loss are presented. The hypothesis was that the high survival rate of the prosthesis would not necessarily mean high clinical status of the patients.
Materials and methods
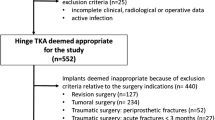
Between 1992 and 2000, 62 primary TKAs using rotating-hinge prosthesis were performed. Fifty cases (80.6%, 40 patients) at a mean follow-up of 15 years (range, 10–18) were possible for review in this retrospective case series. Ten patients had had bilateral surgery. Twelve died (19.4%) from unrelated causes before the minimum follow-up period of 5 years and were excluded from the study. Of the 50 TKAs, 40 were in women and 10 in men, with a median age of 72 years (range, 59–82) at the time of surgery.
Endo-Modell (Link®) rotating-hinge knee prosthesis (Waldemar Link GMBH & Co, Hamburg, Germany) with anterior flange was used in all cases. It is an intercondylar stemmed prosthesis for flexion and tibial rotation, with the stability of a rotating hinge. The T-shaped joint mechanism fixes the axes for flexion and tibial rotation. It helps control movement and transmission of forces with assistance from the replaced runners, plateaus, and the remaining scar tissue of the capsule and collateral ligaments. The rotational degree of freedom allows the reduction in axial shock loads acting at the prosthesis/cement/bone interface. The prosthesis is designed with a range of motion (ROM) from 3° of hyperextension to 165° of flexion. This implant provides a range of rotational movement from 0° at full extension to 25° of both internal and external rotation, when the implant is flexed at angles equal to or greater than 50° [20].
Indications for primary arthroplasty included severe primary osteoarthritis with substantial ligament laxity, severe rheumatic arthritis with extreme ligament instability and bone loss, supracondylar nonunion, charcot arthropathy, and posttraumatic arthritis (Table 1). All knees had extreme ligament imbalance with insufficiency, extraordinary bone loss, or both.
All procedures were performed through a medial parapatellar arthrotomy and under tourniquet control [mean application time 132 min ± 29.2 (range, 90–190 min)]. Non-antibiotic-impregnated Palacos® bone cement (Biomet, Inc, IN, USA) was used in all knees. Finger-packing method was used during cementing. Patellar resurfacing was done (n = 22, 44%) selectively according to the presence of anterior knee pain and the status of patellar cartilage. The diameter of patellar component used was 30 mm in all cases. The system provides with only one type of polyethylene insert with the thickness of 14 mm. In cases of severe bone defect where physiologic tension could be restored by using tibial polyethylene spacers, no cases in this series needed tibial spacer. The postoperative management was similar for all patients, and assisted devices, such as a walker or crutches, were used for several weeks as needed, with partial to full weight-bearing allowed as tolerated. Thrombotic prophylaxis medications were not used.
The clinical outcome of patients was assessed using the Knee Society Score (KSS) [13], which was calculated before surgery and at the time of latest follow-up. A KSS of 90 points was considered an excellent outcome, a score between 80 and 89 points was considered a good outcome, a score between 70 and 79 points was considered a fair outcome, and a score of less than 70 points was considered a poor outcome. Radiographic evaluation was assessed for mechanical alignment of the limb (Hip-Knee-Ankle angle), the position of the components, and the presence and location of radiolucent lines at the bone–cement interface performed by two orthopedic surgeons (JHY, CHO) not involved in the surgery using the Knee Society radiographic evaluation and scoring system [7, 19]. Any radiolucent lines were compared with those on previous radiographs to determine whether there was evidence of progression and possible loosening, or whether the lines were stable and nonprogressive. Migration, subsidence, or radiographic changes in alignment of the components, if any, were recorded. A modified system described by Laurin et al. [18] was used for assessing the axial patellofemoral position. Grade I, normal alignment; Grade II, patellar shift; Grade III, patellar tilt; and Grade IV, patellar shift and tilt.
Statistical analysis
Changes in the KSS and ROM were evaluated via Student’s t test, and the level of significance was set at p < 0.05. Survivorship analysis was performed to determine the cumulative rate of survival of the implant during the period of the study [15, 25]. The end point for analysis was revision surgery for any reason or a recommendation for revision surgery by the senior author. All statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS), version 17.0 (SPSS, Chicago, IL).
Results
Overall, the rotating-hinge arthroplasty resulted in improved knee functioning. The KSS improved (p < 0.001) from a preoperative mean of 38 ± 14.3 (standard deviation) points to a postoperative mean of 73 ± 12.8 points; the functional score improved (p = n.s.) from 36 ± 19.5 points to 47 ± 23.5 points (Table 2). Twelve patients (24%) were walking with one crutch and 25 (50%) with two crutches at the last follow-up. The rest of the patients were wheelchair-bounded (n = 13, 26%) (Table 3). Mean ROM at the most recent clinical follow-up evaluation was 102 ± 9°. In three rheumatoid knees, passive flexion was limited to 90°, with a residual lack of extension of 5°.
In the radiographic analysis, the positions of the components were considered optimal in all knees and the mean femorotibial anatomic axis was 6 ± 1.8° (range 3–9° valgus). The tibiofemoral alignment of all knees was corrected at surgery to the built-in prosthetic angle of 6° of valgus, and there was no evidence of any change in this alignment with time. From the plain postoperative radiographs, there was no evidence of migration of the prosthesis (Fig. 1).
Fifteen (30%) lateral releases were performed to facilitate patellar eversion and to facilitate the quadriceps mechanism in tracking smoothly over the center of the knee intraoperatively. Lateral releases were mainly needed in osteoarthritic valgus knees and severely deformed (mechanical alignment deviation > 15°) varus knees. The mean KSS and the functional score for patients with lateral release were 72 ± 14.2 and 46 ± 13.8, respectively. The mean KSS and the functional score for patients without lateral release were 68 ± 13.7 and 49 ± 14.1, respectively. There was no significant difference between two groups (p = n.s.). Table 4 shows the latest patellar alignment. Thirty-six (72%) cases were either grade I or II.
Radiolucencies were seen in five knees (10%) but were not sclerotic or progressive and always less than 1 mm in thickness. No difference was seen between the bone densities of the medial and lateral femoral condyles. Occasionally, some increased bone density was seen around the stems of the components, but no evidence of cortical hyperostosis was found. Wear of polyethylene, as assessed from plain radiographs, was insignificant.
At the longest follow-up, besides to these favorable findings, 7 deep infections (14%) were observed (Table 5). In 4 cases, the infections required surgical revision to remove the prosthesis, with a new implant and arthrodesis in 3 other cases.
For survival analysis, this series showed survival of 87% (95% confidence interval (CI) 78.6–92.2) at 10 years after surgery. Survival rates then remained stable until the end of follow-up period (mean 15 years). Failure was defined as revision for any cause and included infection (7 cases).
Discussion
In this study, assessment of 50 Endo-Modell (Link®) rotating-hinge TKAs with an average follow-up of 15 years (range, 10–18) with clinical and radiological evaluation was made. The most important finding of the present study was that although this type of prosthesis showed a high survival rate excluding the infection cases, this finding did not necessarily correlate with the clinical status of the patients. Although the KSS improved from a preoperative mean of 38 points to a postoperative mean of 73 points, the functional score did not improve to a statistically significant value (from 36 preoperatively to 47 postoperatively). The mean functional score was low mainly because of patients who were old and had multiple accompanying medical conditions that necessitated the use of walkers/crutches and/or had difficulty in climbing stairs. Thirty-seven (74%) patients were walking with either one or two crutches at the last follow-up. This low functional score may have been contributed to the low incidence of osteolysis and aseptic loosening rate.
The rotating-hinge implant can only be placed in certain specific indications. In primary surgery [1, 26, 29], these are functional loss of lateral ligaments [8, 27], ligaments that cannot be balanced in flexion or extension during surgery, major valgus or varus deformity, a distal femoral or proximal tibial defect resulting from a tumor lesion or mechanical problems, or a comminuted fracture or malunion of the distal femur in the elderly subject [4]. All the specific preoperative clinical and radiologic criteria should be determined in using this type of implant [1, 32]. The clinical examinations including the ligament status and plain radiographs including the stress views should be determined to identify the extent of the bone defect and ligament insufficiency [10].
The outcome of the rotating-hinge TKA has been evaluated in several studies (Table 6). Böhm et al. [3] evaluated 422 consecutive primary TKAs using one specific design of hinged total knee prosthesis at a mean 6 years. The cumulative rates of survival at 20 years were from 86.8 to 96.0% depending on the end points. Barrack [1] reported satisfying clinical results in a study of 23 modern-generation hinged TKAs evaluated at 2- to 9-year follow-up. The clinical results, ROM, and satisfaction were comparable to those of a standard condylar revision knee arthroplasty, despite the fact that the cases were more complex. Joshi et al. [14] reviewed the results of 78 revision TKAs using a rotating-hinge device in patients requiring revision arthroplasty due to aseptic loosening. Fifty-seven (73%) patients showed excellent results, with a ROM of 104° in flexion and complete extension. Pradhan et al. [23] conducted a retrospective study of 51 rotating-hinge prostheses in revision surgery with a maximum follow-up of 6 years. Reasons for revision were infection and aseptic loosening in 46 cases. There was a notable improvement in the pain, stability, ROM, and mobility of the patients. Postoperatively, 33 (72%) presented excellent or good results (better results in patients with aseptic loosening). Pour et al. [22] included in their study 44 knee arthroplasties using modern-generation kinematic rotating-hinge prostheses with a mean follow-up of 4.2 years. The prostheses provided substantial improvement in function and reduction in pain, but a relatively large number (18%) of complications and failures (periprosthetic infection in three knees, aseptic loosening in four, and a periprosthetic fracture in one) were encountered. The rate of prosthetic survival was 68.2% at 5 years with revision or reoperation as the end point. Nieder [20] also published excellent long-term results with the Endo-Modell (Link®) rotating-hinge TKR, the same prosthesis as this study is based on. Although the results of various reports are favorable, routine procedure cannot be advocated in cases when condylar prosthesis could be inserted.
As noted, the results are variable for rotating-hinge total knee arthroplasties [1, 3, 20, 22, 23]. Although recent generation of rotating-hinge devices allowing axial rotation and distraction, suboptimal instrumentation and implant design probably resulted in continued complication rates [1]. A few reports have highlighted the major complications that can arise when using these fully constrained prostheses. Walker et al. [33] reported good short-term results in terms of pain relief and restoration of range of motion in association with early-generation rotating-hinge implants. Despite the early success in terms of functional improvement, a number of serious complications, such as tibial tubercle avulsion, cortical bone perforation, patellar subluxation, and progressive radiolucency were encountered. Rand et al. [24] reviewed the first fifty rotating-hinge knee arthroplasties that were performed at their institution. The complications were numerous and included patellar instability (22%; eleven of fifty), deep infection 16% (eight of fifty), and implant fracture (6%; three of fifty). Shaw et al. [28] reviewed the outcome for thirty-eight knees that had received an early-generation hinged total knee replacement and found an 86% satisfaction rate after a minimum duration of follow-up of 25 months. The major complication in that series was patellar instability, which was found in association with four of twenty primary procedures and six of eighteen revision procedures. In addition, evidence of aseptic radiolucency was found in six of the thirty-eight knees. The results of total knee arthroplasties performed with use of the newer generation of rotating-hinge knee implants have also been reviewed in several studies [1, 21]. Barrack [1] reported satisfying clinical results in a study of twenty-three modern-generation hinged total knee replacements. Although there were no progressive radiolucent lines, complications included one intraoperative distal femoral fracture, one case of patellar subluxation, and one peroneal nerve palsy.
Complication regarding infection should be encountered. Springer et al. [30] recently reported on the early results of distal femoral arthroplasty for nonneoplastic limb salvage in a study of 26 knees and highlighted some of the major complications. In their report, the periprosthetic infection (five knees; 19%) was the main cause of failure. Shaw et al. [28] also had 16% deep infection rate in their 38 knees (primary, revision) with a minimum 25-month follow-up. This complication also appears in this series. Seven (14%) out of 50 patients had deep infection in this series, much higher rate than both primary and revision operations. To explain these results, it seems relevant to detail the inclusion criteria for each group. The studied population presents a high percentage of patients with several risk factors for complications: high mean age, association of comorbidities (diabetes, cardiological, or rheumatoid disease). Similar rates were reported, [12, 28, 30, 31] all of them with similar inclusion criteria.
Hinged prosthesis may not do well in younger patients as compared to older patients. Comparison of outcome between younger patients (less than 65) with older patients may be worthwhile. However, there were only two patients younger than 65 in this series. One female patient (63 years old at the time of surgery) was rheumatic arthritis patient with the latest KSS of 62 and functional score of 42. Another male patient (59 years old) was posttraumatic osteoarthritis, with latest KSS 74 with functional score of 66. Comparative analysis would be beyond the scope in this study.
This study has several limitations. First, it is retrospective and non-controlled. Second, relative small number of patient population sample is another limitation. Finally, the study combined a group of patients with varied preoperative diagnoses, and because of small population size, difference in outcome on the basis of the underlying diagnosis was not possible.
Despite these limitations, it is our opinion that although substantial improvement in function and reduction in pain, Endo-Modell (Link®) rotating-hinge prosthesis has, in our hands, a higher infection rate than those observed with both primary arthroplasties and revisions. Some indications may remain for this type of implant for the deformed or malaligned knee with, perhaps, serious bone and ligament defects but should be reserved for elderly and sedentary patients.
Conclusion
Reconstruction with a rotating-hinge total knee prosthesis provided substantial improvement in function and reduction in pain with relatively high survival rate. However, the possibility of assisted walking (low functional status) and high rate of deep infection should be encountered.
References
Barrack RL (2001) Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res 392:292–299
Barrack RL, Lyons TR, Ingraham RQ, Johnson JC (2000) The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty 15:858–866
Bohm P, Holy T (1998) Is there a future for hinged prostheses in primary total knee arthroplasty? A 20-year survivorship analysis of the Blauth prosthesis. J Bone Joint Surg Br 80:302–309
Davila J, Malkani A, Paiso JM (2001) Supracondylar distal femoral nonunions treated with a megaprosthesis in elderly patients: a report of two cases. J Orthop Trauma 15:574–578
Deehan DJ, Murray J, Birdsall PD, Holland JP, Pinder IM (2008) The role of the rotating hinge prosthesis in the salvage arthroplasty setting. J Arthroplasty 23:683–688
Draganich LF, Whitehurst JB, Chou LS, Piotrowski GA, Pottenger LA, Finn HA (1999) The effects of the rotating-hinge total knee replacement on gait and stair stepping. J Arthroplasty 14:743–755
Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Fuchs S, Sandmann C, Gerdemann G, Skwara A, Tibesku CO, Bottner F (2004) Quality of life and clinical outcome in salvage revision total knee replacement: hinged vs total condylar design. Knee Surg Sports Traumatol Arthrosc 12:140–143
Guenoun B, Latargez L, Freslon M, Defossez G, Salas N, Gayet LE (2009) Complications following rotating hinge Endo-Modell (Link) knee arthroplasty. Orthop Traumatol Surg Res 95:529–536
Gustke KA (2005) Preoperative planning for revision total knee arthroplasty: avoiding chaos. J Arthroplasty 20:37–40
Hernandez-Vaquero D, Sandoval-Garcia MA (2010) Hinged total knee arthroplasty in the presence of ligamentous deficiency. Clin Orthop Relat Res 468:1248–1253
Inglis AE, Walker PS (1991) Revision of failed knee replacements using fixed-axis hinges. J Bone Joint Surg Br 73:757–761
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Joshi N, Navarro-Quilis A (2008) Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty 23:1204–1211
Kaplan E, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Keenan J, Chakrabarty G, Newman JH (2000) Treatment of supracondylar femoral fracture above total knee replacement by custom made hinged prosthesis. Knee 7:165–170
Lachiewicz PF, Falatyn SP (1996) Clinical and radiographic results of the total condylar III and constrained condylar total knee arthroplasty. J Arthroplasty 11:916–922
Laurin CA, Dussault R, Levesque HP (1979) The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res 144:16–26
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56:1391–1396
Nieder E (1991) Sled prosthesis, rotating knee and hinge prosthesis: St. Georg model and ENDO-model. Differential therapy in primary knee joint arthroplasty. Orthopade 20:170–180
Petrou G, Petrou H, Tilkeridis C, Stavrakis T, Kapetsis T, Kremmidas N, Gavras M (2004) Medium-term results with a primary cemented rotating-hinge total knee replacement. A 7- to 15-year follow-up. J Bone Joint Surg Br 86:813–817
Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF (2007) Rotating hinged total knee replacement: use with caution. J Bone Joint Surg Am 89:1735–1741
Pradhan NR, Bale L, Kay P, Porter ML (2004) Salvage revision total knee replacement using the Endo-Model rotating hinge prosthesis. Knee 11:469–473
Rand JA, Chao EY, Stauffer RN (1987) Kinematic rotating-hinge total knee arthroplasty. J Bone Joint Surg Am 69:489–497
Rand JA, Ilstrup DM (1991) Survivorship analysis of total knee arthroplasty. Cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am 73:397–409
Scuderi GR (2001) Revision total knee arthroplasty: how much constraint is enough? Clin Orthop Relat Res 392:300–305
Sculco TP (2006) The role of constraint in total knee arthroplasty. J Arthroplasty 21:54–56
Shaw JA, Balcom W, Greer RB 3rd (1989) Total knee arthroplasty using the kinematic rotating hinge prosthesis. Orthopedics 12:647–654
Springer BD, Hanssen AD, Sim FH, Lewallen DG (2001) The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res 392:283–291
Springer BD, Sim FH, Hanssen AD, Lewallen DG (2004) The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res 421:181–187
Utting MR, Newman JH (2004) Customised hinged knee replacements as a salvage procedure for failed total knee arthroplasty. Knee 11:475–479
Vince KG (2003) Why knees fail. J Arthroplasty 18:39–44
Walker PS, Emerson R, Potter T, Scott R, Thomas WH, Turner RH (1982) The kinematic rotating hinge: biomechanics and clinical application. Orthop Clin North Am 13:187–199
Wang CJ, Wang HE (2000) Early catastrophic failure of rotating hinge total knee prosthesis. J Arthroplasty 15:387–391
Westrich GH, Mollano AV, Sculco TP, Buly RL, Laskin RS, Windsor R (2000) Rotating hinge total knee arthroplasty in severely affected knees. Clin Orthop Relat Res 379:195–208
Acknowledgments
The authors wish to thank Ms. Min-Jung Lee for her assistance with the analysis and statistical assessment of the data. Authors also thank Ms. Hyeran Lee for her assistance with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, JH., Yoon, JR., Oh, CH. et al. Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc 20, 517–523 (2012). https://doi.org/10.1007/s00167-011-1590-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1590-1