Abstract
Background
There is currently a trend toward minimally invasive total knee arthroplasty (TKA) to decrease the morbidity related to the standard approach. The aim of our study was to clarify whether the mini-subvastus surgical had an advantage over the standard in term of pain level, blood loss, and postoperative recovery, whether the mini-subvastus surgical was prone to radiographic malalignment, prolonged operative time, and increased complications.
Methods
In a prospective randomized study, we compared the clinical and radiological results of primary TKA using a mini-subvastus approach or a standard approach in 68 patients. The mini-subvastus approach was used on 35 patients (group I) and the standard approach on 33 patients (group II).
Results
The mean follow-up was 28 months (range 24–36 months). Patients in group I had less blood loss and better visual analogue scale score at 1 day postoperatively. They achieved active straight leg raise earlier and underwent less lateral retinacular releases. The mean Knee Society function score, Oxford knee score, and range of movement were significantly better in group I up to 9 months after surgery (all, p < 0.05). However, there were no significant differences in these parameters between the groups at final follow-up. Reduced access and visibility in group I prolonged tourniquet time by an average of 22 min and resulted in five technical errors on radiographic evaluation.
Conclusions
Patients can receive marked but temporary benefits from the mini-subvastus technique, with a definite cost: that of component malposition and prolongation of operative time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) through a standard approach consistently yields good long-term results [1–4]. However, the standard approach has resulted in postoperative pain and prolonged rehabilitation periods, which may contribute to patient dissatisfaction or knee stiffness [5, 6].
There is currently a trend toward minimally invasive TKA to decrease the morbidity related to the standard approach, with specific emphasis on preserving as much of the extensor mechanism as possible. A number of minimally invasive surgical approaches for TKA have been described: the mini-medial parapatellar [7], mini-midvastus [8–11], mini-subvastus [12–16], and “quadriceps-sparing” approaches [16–19]. The mini-subvastus approach, which evolves from the traditional subvastus approach, has a limited incision length of 10–14 cm and an arthrotomy without any incision of the extensor mechanism [20, 21]. Previous studies have reported that patients undergoing mini-subvastus surgical TKA have a faster rehabilitation, experience less pain, and obtain increased range of motion (ROM) [12–16, 22]. However, there are few prospective matched-control studies to well document the benefits and potential risks of this technique [14–16]. Two of these trials present results only up to 3 months [15, 16].
In this study, we reported clinical and radiological results of a prospective randomized trial with a minimum of 2-year follow-up, which was designed to clarify whether the mini-subvastus surgical TKA had an advantage over the standard TKA in term of pain level, blood loss, and postoperative recovery. Furthermore, the study was to determine whether the mini-subvastus surgical TKA was prone to radiographic malalignment, prolonged operative time, and increased complications.
Materials and methods
Between September 2007 and June 2008, all patients with osteoarthritis of the knee underwent primary unilateral TKA were considered eligible to participate in our prospective randomized study. The study was approved by our institutional review board, and all patients gave informed consent. Inclusion criteria were mechanical axis alignment less than 10° varus or less than 15° valgus as measured on the full-leg standing radiograph, flexion deformity less than 10°, ROM of greater than 90°, and body mass index (BMI) less than 30. Simultaneous exclusion criteria were rheumatoid arthritis, previously operated joint, patella baja, compromise of soft tissue envelope, and knee required a complex reconstruction with bone graft and/or prosthetic augmentation. A total 68 patients were enrolled in our prospective randomized study. Computer-generated randomization and closed envelopes were used to allocate patients to either the minimally invasive group (group I) or the standard group (group II). Finally, thirty-five patients were randomly assigned to the group I and 33 to the group II. The two groups were matched for age, gender, BMI, diagnose, and knee deformity (Table 1).
Prior to the present study, the senior author (ShiYuan Shi) performed 20 TKAs using the mini-subvastus approach in order to eliminate bias due to the learning curve. In patients from group I, a mini-subvastus approach as described by Boerger et al. [15] was used. A medial parapatellar skin incision was made which began the level of the superior patella pole to 2.5 cm below the joint line. Subsequently, a mini-subvastus capsular incision was made along the medial border of the patella tendon extending at an angle along the inferior vastus medialis obliquus (VMO) border (Fig. 1a). By using differential force, the limited arthrotomy could be moved as a “mobile window” from medial to lateral and from superior to inferior as necessary. The patella was subluxed laterally but not everted, and soft tissue balancing was done in a standard manner. Special attention was paid to avoiding interruption of the suprapatellar pouch. In group II, a standard medial parapatellar approach was used. The surgical approach consisted of a straight anterior midline skin incision extending from 5 to 10 cm proximal to the superior pole of the patella to 2–4 cm distal to the medial extent to the tibial tubercle. The quadriceps tendon was split along its medial one-third, and the incision was continued distally through the medial parapatellar retinaculum, medial to the patellar ligament, and 5 mm medial to the tibial tubercle (Fig. 1b). The Zimmer minimally invasive surgery instrumentation (Zimmer, Warsaw, IN, USA) was used for both groups. The bone resection was performed using instruments with intramedullary referencing on the femoral side and extramedullary on the tibial. All components were the cemented posterior-stabilized prosthesis (LPS-Flex, Zimmer, Warsaw, IN, USA). The patellar aponeurosis at a distance of a 5 mm all around the patella was released with electrocautery rather than resurfaced. After surgery, all patients received epidural anesthesia and followed a patients-controlled epidural analgesia for 48 h postoperatively. The drain remained in situ for 24 h. Low molecular weight heparin sodium was used for prophylaxis against deep-vein thrombosis (DVT) beginning on the day of surgery and continuing during the in-patient stay. Continuous passive motion was started immediately in the recovery room. Twice daily physical therapy for ROM, walking, and strengthening began the day after surgery.
Data recorded from the operation included length of the closed skin incision measured in 90° of flexion, tourniquet time, and lateral retinacular release. Total blood loss was taken as the sum of recorded intraoperative loss and loss from drains during the first 24 h. Clinical outcome data were collected for all patients at regular intervals commencing preoperatively and continuing postoperatively on the 7 days; at 6 weeks; 3, 6, and 9 months; 1 year; and annually thereafter. The following validated rating systems for TKA were used: the Knee Society score [23] and the Oxford knee score [24]. The Knee Society score was divided into the knee score and the function score, with a total of 100 points indicating full function, respectively. The knee score was based on pain, ROM, stability, and alignment of the knee; the function score was based on activities of daily living. The Oxford knee score was used for subjective assessment of pain and functional capacity. It was administered as a patient-administered 12-part questionnaire, with 5 questions relating to the measurement of pain and 7 to the assessment of function. The answer to each question was rated on a scale ranging between 1 and 5 points, with higher scores indicating more severe problems. Knee pain was rated in the form of a 10-point visual analogue scale (VAS), with 0 points indicating no pain and 10 worst pain. Additionally, the first active straight leg raise and the complications were recorded.
For radiographic assessment, full-leg standing, anteroposterior and lateral radiographs, and Merchant views were taken and analyzed preoperatively, postoperatively, and at each follow-up time. Alignment of the knee, the position of components, and the presence and location of radiolucencies at the cement–bone interface were evaluated according to the Knee Society radiological rating system [25]. The clinical and radiographic assessments were undertaken by two independent authors who were blinded to the surgical approach used.
Statistical analysis
Descriptive statistics were calculated for all variables with SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Statistical tests used in comparisons were chosen based on the type of variable being compared. Student’s t test and the paired t test were used for analysis of the continuous variables. The analysis for dichotomous variables was completed using the likelihood ratio chi-squared test. Statistical significance was set at p < 0.05.
Results
All patients in both treatment groups were followed up for minimum 2 years (mean 28 months, range 24–36 months). The mean length of follow-up was 29 months (range 24–36 months) in group I and 27 months (range 24–34 months) in group II. The mean length of the closed skin incision in 90° of flexion was 10.5 cm (range 9.5–12 cm) in group I and 18 cm (range 15–20 cm) in group II, which was statistically significant (p < 0.001; Table 2). The mean tourniquet time was 87 min (range 65–105 min) in group I and 65 min (range 58–95 min) in group II (p < 0.001). The mean total blood loss of 821 ml (range 325–1,200 ml) in group I was significantly less than 1,020 ml (range 420–1,400 ml) in group II (p = 0.028). Active straight leg raise was achieved quicker (p < 0.001) in group I at mean 1.9 days (range 1–4 days) compared with group II at mean 4.2 days (range 3–6 days). Average postoperative pain on day 1, as recorded on the VAS, was 2.1 (range 1–5) in group I significantly lower than 3.8 (range 2–5) in group II (p = 0.015). Two (5.71 %) lateral retinacular releases were required in group I and 7 (21.21 %) in group II (p = 0.042); the rule of no thumb test was used to assess patellar tracking [26].
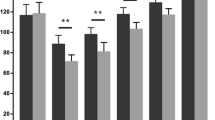
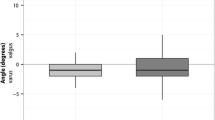
Preoperative and final follow-up results, and differences between and within groups for the objective knee score and function score, and subjective Oxford knee score are shown in Table 3. No significant differences were observed when the knee score was compared between the groups preoperatively (Table 3), at each time interval (Fig. 2) and final follow-up (Table 3). The mean preoperative function score and Oxford knee score between the groups were not significantly different (Table 3). After surgery, statistically significant difference in functional score and Oxford knee score were observed during the first 9-month follow-up only (Figs. 3, 4). At the final follow-up, the difference was not significant (Table 3). The parameter ROM of the knee score increased from a preoperative mean of 104° (90°–133°) to a final mean of 125° (115°–135°) in group I and from a preoperative mean of 105°(90°–125°) to a final mean of 122° (110°–135°) in group II. No statistically significant difference was observed between the groups at final follow-up (p = 0.074). However, patients from group I had a significantly greater ROM at a follow-up of 7 days, 3, 6, and 9 months (Fig. 5).
Preoperatively, fifty-seven knees had different levels of deformity: 27 varus knees in group I, 26 varus knees in group II, and two valgus knees in each group (Table 1). Postoperatively, radiographic evaluation revealed that none of the tibial components were misaligned (neutral ±2°) in varus or valgus on the frontal plane in group II. On the contrary, five patients in group I had tibial component varus malalignment. But the tibial component slope was within 1°–5° in all knees. There were no statistically significant differences between the groups with regard to the femoral implant position in the coronal and sagittal planes, the alignment of the knee, and patellar position. There was no evidence of progressive radiolucent lines around any component or aseptic loosening of the components in either group. None of this series had infections, extensor mechanism, or neurovascular complications. One patient in group I developed superficial wound necrosis that healed uneventfully with dressing changes, and there were no other wound complications.
Discussion
The development of new instrumentations and techniques has stimulated the rapid advancement of minimally invasive TKA. The proposed advantages of minimally invasive TKA technique include less pain, quicker postoperative rehabilitation, and shorter hospitalization [7–11, 14, 15, 17, 18]. The applications of minimally invasive approaches in TKA are now accepted. In general, these approaches are distinguished from traditional exposures by their shorter incisions, avoidance of patellar eversion, and the smaller instruments. However, the extensor mechanism is handled somewhat differently with each minimally invasive approach. The mini-medial parapatellar and mini-midvastus approaches limit the amount of quadriceps tendon or vastus medialis muscle split to a few centimeters. Theoretically, incision into extensor mechanism will affect the postoperative rehabilitation and ROM of the knee. Therefore, the ideal surgery should not violate the extensor mechanism in any way. To avoid incision of the quadriceps tendon above the proximal pole of the patella, Tria and Coon [17] develop so-called the quadriceps-sparing approach. This name, however, is not anatomically correct. In magnetic resonance and cadaver study, most VMO insertions show extension down to the midpole of the patella [27, 28]; therefore, a “quadriceps-sparing” approach invariably violates VOM insertion, even if incision is made only to the proximal patellar pole.
The mini-subvastus approach, an evolution of the standard subvastus technique of Hoffman [29], is the only minimally invasive approach to preserve the entire extensor mechanism. Previous studies of TKA with this minimally invasive approach have demonstrated improvement in the early functional recovery. Kashyap and van Ommeren compared 25 consecutive cases performed through the mini-subvastus approach with 25 cases of standard medial parapatellar approach, and their 2-year experience suggested patients in minimally invasive group had better knee flexion, walk ability, and stair climbing in the early postoperative period, without compromising the alignment of the knee [14]. In a 2-year study of 150 minimally invasive TKAs, Schroer et al. [12] reported a more rapid return of knee function, decreased hospital length of stay, and improved knee flexion were demonstrated in mini-subvastus group when compared with the standard group. To further document the benefit of the mini-subvastus technique, a randomized double-blind comparative study between the mini-subvastus and QS approach was undertaken [16]. This investigation found that there was also no difference in the 3-month recovery and early clinical results between the groups.
Based on our experience with the standard subvastus approach, the mini-subvastus approach was adopted in our department in 2007. Despite the confidence gained after 20 cases were initially performed, several questions were raised concerning the efficacy and safety of this procedure, which leaded to our establishing this randomized controlled study. We found patients undergoing the mini-subvastus surgical TKA achieved more rapid rehabilitation. Avoiding disruption of the extensor mechanism and eversion of the patella, patients in the mini-subvastus group experienced less postoperative pain and regained the active straight leg raise 2.3 days earlier than those in the standard group. Furthermore, the function score and knee ROM, even patient-reported Oxford knee score, were markedly improved at initial 9 months postoperatively in the mini-subvastus group. However, the difference diminished with time. Our results reflected the outcomes of recent studies of the mini-midvastus or “quadriceps-sparing” approach, in which the minimally invasive surgical TKA had greater flexion and better functional outcomes at early assessments than the standard one [10, 18, 19]. This early difference also diminished with time.
Despite there was no significant difference in preoperative knee alignment between the two groups, more lateral retinacular releases were performed in order to optimize patellofemoral tracking in the standard group than in the mini-subvastus group (5.71 vs. 21.21 %), according to the rule of no thumb test. However, the rule of no thumb test may be not clinically accurate tool to predict the need for lateral retinacular release [30], especially in cases undergoing a standard medial parapatellar approach, this test ignores the role of the repaired medial half of the entire arthrotomy in stabilizing patellofemoral tracking and therefore may overestimate the risk of patellofemoral instability. On the contrary, owing to a quadriceps-sparing arthrotomy in the mini-subvastus approach, the rule of no thumb test does not create such a discrepancy between the test and the actual anatomic patellofemoral tracking. Although this difference in the incidence of lateral retinacular release between the groups may be affected by the current assessment test, we still believe the mini-subvastus approach, compared with the standard medial parapatellar approach, preserve the VOM intact and fully attached to the medial patellar border, which contribute to maintain soft tissue balance and decrease the risk of patellofemoral instability.
The price of the above-mentioned benefits obtained from the mini-subvastus approach was an increased operation time of approximately 22 min. Most importantly, technical errors of component positioning in five patients were found in the MIS group, which might adversely affect the long-term performance of the TKR. Boerger et al. also [15] found the mini-subvastus approach offered early but short-lived benefits for patients at the expense of a longer operation and a higher risk of complications. It reflected operation through the mini-subvastus approach was technically more demanding, and access and overall visibility were greatly diminished. These findings were consistent with the outcomes of previous reports where the mini-midvastus approach took longer operation time and affected component alignment than the standard procedure [10, 31].
A weakness of this study is that the follow-up is short-term, with the duration ranging from 24 to 36 months and averaging 28 months. Ongoing follow-up is certainly required. Although the two groups are identical in preoperative demographics, the lack of double-blinded data collection may have led to biased results. Moreover, as reported by King et al. [32], there is a learning curve of as many as fifty TKAs for minimally invasive technique. This is still our initial experience, and there is also a learning curve in this study. Tibial component malposition in five patients in the mini-subvastus approach group can be contributed to the initial experience and the learning curve of the surgeon. Previous studies have demonstrated a learning curve of the mini-subvastus technique that is associated with the complication rate and operative time [13, 15]. In a retrospective study of comparison of 600 mini-subvastus TKAs with that in a historical control group of 150 traditional TKA, Schroer et al. [13] found the mini-subvastus technique did not lead to an increased rate of complications compared with that treated with a traditional TKA. However, the power of this study is negatively affected by its retrospective nature. Therefore, we consider a randomized double-blinded study with the long-term follow-up should be undertaken by an experienced surgeon and a dedicated team, to ascertain the advantages and disadvantages of the mini-subvastus technique.
This prospective randomized controlled study suggests certain patients can receive marked but temporary benefits from the mini-subvastus technique, with a definite cost: that of component malposition and prolongation of operative time. Therefore, we currently perform mini-subvastus TKA in selected cases only.
References
Stern SH, Insall JN (1992) Posterior stabilized prosthesis: results after follow-up of 9–12 years. J Bone Jt Surg Am 74:980–986
Ranawat CS, Flynn WF Jr, Saddler S et al (1993) Long-term results of the total condylar knee arthroplasty: a 15-year survivorship study. Clin Orthop Relat Res 286:94–102
Colizza WA, Insall JN, Scuderi GR (1995) The posterior stabilized total knee prosthesis: assessment of polyethylene damage and osteolysis after a 10-year-minimum follow-up. J Bone Jt Surg Am 77:1713–1720
Buechel FF Sr (2002) Long-term follow-up after mobile-bearing total knee replacement. Clin Orthop Relat Res 404:40–50
Bullens PH, van Loon CJ, de Waal Malefijt MC et al (2001) Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplast 16:740–747
Walton NP, Jahromi I, Dobson PJ et al (2005) Arthrofibrosis following total knee replacement; does therapeutic warfarin make a difference? Knee 12:103–106
Tenholder M, Clarke HD, Scuderi GR (2005) Minimal-incision total knee arthroplasty: the early clinical experience. Clin Orthop Relat Res 440:67–76
Haas SB, Cook S, Beksac B (2004) Minimally invasive total knee replacement through a mini midvastus approach: a comparative study. Clin Orthop Relat Res 428:68–73
Laskin RS, Beksac B, Phongjunakorn A et al (2004) Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res 428:74–81
Karachalios T, Giotikas D, Roidis N et al (2008) Total knee replacement performed with either a mini-midvastus or a standard approach: a prospective randomized clinical and radiological trial. J Bone Jt Surg Br 90:584–591
Haas SB, Manitta MA, Burdick P (2006) Minimally invasive total knee arthroplasty: the mini midvastus approach. Clin Orthop Relat Res 452:112–116
Schroer WC, Diesfeld PJ, Reedy ME et al (2008) Mini-subvastus approach for total knee arthroplasty. J Arthroplast 23:19–25
Schroer WC, Diesfeld PJ, Reedy ME et al (2007) Evaluation of complications associated with six hundred mini-subvastus total knee arthroplasties. J Bone Jt Surg Am 89:76–81
Kashyap SN, van Ommeren JW (2008) Clinical experience with less invasive surgery techniques in total knee arthroplasty: a comparative study. Knee Surg Sports Traumatol Arthrosc 16:544–548
Boerger TO, Aglietti P, Mondanelli N et al (2005) Mini-subvastus versus medial parapatellar approach in total knee arthroplasty. Clin Orthop Relat Res 440:82–87
Aglietti P, Baldini A, Sensi L (2006) Quadriceps-sparing versus mini-subvastus approach in total knee arthroplasty. Clin Orthop Relat Res 452:106–111
Tria AJ Jr, Coon TM (2003) Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res 416:185–190
Chen AF, Alan RK, Redziniak DE et al (2006) Quadriceps sparing total knee replacement: the initial experience with results at 2–4 years. J Bone Jt Surg Br 88:1448–1453
Kim YH, Kim JS, Kim DY (2007) Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Jt Surg Br 89:467–470
Scuderi GR, Tenholder M, Capeci C (2004) Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res 428:61–67
Kim JG, Lee SW, Ha JK et al (2011) The effectiveness of minimally invasive total knee arthroplasty to preserve quadriceps strength: a randomized controlled trial. Knee 18:443–447
Liebensteiner MC, Krismer M, Koller A et al (2012) Does minimally invasive total knee arthroplasty improve isokinetic torque? Clin Orthop Relat Res 470:3233–3239
Insall JN, Dorr LD, Scott RD et al (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Baker PN, van der Meulen JH, Lewsey J et al (2007) The role of pain and function in determining patient satisfaction after total knee replacement: data from the national joint registry for England and Wales. J Bone Jt Surg Br 89:893–900
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Benjamin J, Chilvers M (2006) Correcting lateral patellar tilt at the time of total knee arthroplasty can result in overuse of lateral release. J Arthroplast 21:121–126
Pagnano MW, Meneghini RM, Trousdale RT (2006) Anatomy of the extensor mechanism in reference to quadriceps-sparing TKA. Clin Orthop Relat Res 452:102–105
Holt G, Nunn T, Allen RA et al (2008) Variation of the vastus medialis obliquus insertion and its relevance to minimally invasive total knee arthroplasty. J Arthroplast 23:600–604
Hoffman AA, Plaster RL, Murdock LE (1991) Subvastus (Southern) approach for primary knee arthroplasty. Clin Orthop Relat Res 269:70–77
Bindeglass DF, Vince KG (1996) Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty. J Arthroplast 11:507–511
Dalury DF, Dennis DA (2005) Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res 440:77–81
King J, Stamper DL, Schaad DC et al (2007) Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. Assessment of learning curve and the postoperative recuperative period. J Bone Jt Surg Am 89:1497–1503
Acknowledgments
We thank X. G. Li for linguistic revision and statistical data. We also thank the participating surgeons at the Department of Orthopaedics The First Hospital Affiliated to Suzhou University, J. Y. Sun, Y. Z. Xu, and T. S. Tang.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Archives of Orthopaedic and Trauma Surgery, Springer-Verlag Berlin Heidelberg 2014. This paper, published in Volume 134, Issue 8, pages 1155-1162, DOI 10.1007/s00402-014-1963-2, has been formally withdrawn by the two corresponding authors on ethical grounds because the article contains extensive and repeated instances of plagiarism. Archives of Orthopaedic and Trauma Surgery treats all identified evidence of plagiarism in the published articles most seriously. It is unfortunate that this misconduct was not detected before going to press. The authors apologize to the Editors and readers as well as the authors of the original article.
About this article
Cite this article
Lai, Z., Shi, S., Fei, J. et al. RETRACTED ARTICLE: Total knee arthroplasty performed with either a mini-subvastus or a standard approach: a prospective randomized controlled study with a minimum follow-up of 2 years. Arch Orthop Trauma Surg 134, 1155–1162 (2014). https://doi.org/10.1007/s00402-014-1963-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-1963-2