Abstract
Performing minimally invasive (MIS) total knee arthroplasty (TKA) through a subvastus approach makes sense on an anatomic basis, on a scientific basis, and on a practical basis. Anatomically, the subvastus approach is the only approach that saves the entire quadriceps tendon insertion on the patella [1–5] (Fig. 1). Scientifically, the subvastus approach has been shown, in prospective randomized clinical trials, to be superior to the standard medial parapatellar arthrotomy and to the so-called quadriceps-sparing arthrotomy [3, 6, 7] (Table 1). Practically, MIS TKA with a subvastus approach is reliable, reproducible, and efficient and allows the MIS technique to be applied to a broad group of patients, not just a highly selected subgroup [8] (Table 2).
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Subvastus approach, MIS TKA
- Vastus medialis obliquus muscle (VMO)
- Minimally invasive surgery total knee arthroplasty (MIS TKA), subvastus approach
Performing minimally invasive (MIS) total knee arthroplasty (TKA) through a subvastus approach makes sense on an anatomic basis, on a scientific basis, and on a practical basis. Anatomically, the subvastus approach is the only approach that saves the entire quadriceps tendon insertion on the patella [1–5] (Fig. 1).
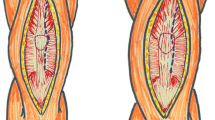
Anatomy of the extensor mechanism. (a) The vastus medialis obliquus (VMO) tendon consistently inserts at the midpole of the patella at a 50° angle relative to the long axis of the femur. (b) When looking through a surgical incision, one could easily misidentify the most prominent part of the VMO (the point closest to the patella, akin to the bow of the ship) as the most inferior part of the VMO. Because that most prominent portion often lies close to the superior pole of the patella, some surgeons might then mistakenly presume that the VMO inserts at the superior pole of the patella. Additional medial dissection will delineate the inferior border of the VMO, which is more inferior and more medial than most surgeons anticipate. (c) The arthrotomy for the subvastus exposure parallels the inferior border of the VMO, intersects the patella at the midpole, and then is turned straight distally to parallel the medial margin of the patellar tendon (Copyright Mayo Foundation, used with permission)
Scientifically, the subvastus approach has been shown, in prospective randomized clinical trials, to be superior to the standard medial parapatellar arthrotomy and to the so-called quadriceps-sparing arthrotomy [3, 6, 7] (Table 1).
Practically, MIS TKA with a subvastus approach is reliable, reproducible, and efficient and allows the MIS technique to be applied to a broad group of patients, not just a highly selected subgroup [8] (Table 2).
It is now accepted widely that the tenets of MIS TKA include a smaller skin incision, no eversion of the patella, minimal disruption of the suprapatellar pouch, and minimal disruption of the quadriceps tendon. To what degree any one of those factors contribute to improvements in postoperative function remains unclear. Our initial attempts at MIS TKA using the short medial arthrotomy (sometimes referred to as the quadriceps-sparing approach) and the mini-midvastus splitting approaches were frustrated by some substantial technical difficulties. We then modified the subvastus approach to the knee to meet the tenets of MIS TKA and found that it markedly facilitated MIS surgery and allowed MIS surgery to be applied to a broader group of patients. When coupled with instruments designed specifically for small incision surgery, the modified subvastus approach is reliable, reproducible, and safe. Using a simple set of retractors, this procedure can be done without making any blind cuts or freehand cuts, and that enhances surgical accuracy and patient safety.
Surgical Technique
The incision starts at the superior pole of the patella, ends at the top of the tibial tubercle, and typically measures 3.5 in. (8.8 cm) in extension. Surgeons should start with a traditional 6–8-in. incision and then shorten the incision length over time. The medial skin flap is elevated to clearly delineate the inferior border of the vastus medialis obliquus muscle (VMO). The fascia overlying the VMO is left intact because this helps maintain the integrity of the muscle belly itself throughout the case. The anatomy in this region is very consistent. The inferior edge of the VMO is always found more inferior and more medial than most surgeons anticipate. The muscle fibers of the VMO are oriented at a 50° angle, and the VMO tendon always attaches to the midpole of the patella. It is very important to save this edge of tendon from the edge of muscle down to the midpole of the patella. That is where the retractor will rest so that the VMO muscle itself is protected throughout the case. The arthrotomy is made along the inferior edge of the VMO down to the midpole of the patella (do not be tempted to cheat this superiorly, because that will hinder, not help, the ultimate exposure) (Fig. 2). The proximal limb of the arthrotomy parallels the inferior edge of the VMO and is made at the same 50° angle relative to the long axis of the femur. At the midpole of the patella, the arthrotomy is directed straight distally along the medial border of the patellar tendon. A 90° bent Hohmann retractor is placed in the lateral gutter and rests against the robust edge of VMO tendon that was preserved during the exposure. Surprisingly little force is needed to completely retract the patella into the lateral gutter. Any substantial medial or inferior osteophytes on the patella are debrided with a rongeur. The knee is then flexed to 90°, providing good exposure of both distal femoral condyles (Fig. 3). If the patella does not slide easily into the lateral gutter, typically it is because a portion of the medial patellofemoral ligament remains attached to the patella. That occurs if the proximal limb of the arthrotomy is made in too horizontal a fashion rather than at the 50° angle that parallels the VMO. By releasing that tight band of tissue, the patella will translate laterally without substantial difficulty.
The distal femur is cut with a modified intramedullary resection guide. Bringing the knee out to 60° of flexion better exposes the anterior portion of the distal femur. When a very small skin incision is used, the distal femur is cut one condyle at a time with the intramedullary portion of the cutting guide left in place for added stability. If a slightly longer skin incision is used, the distal cutting guide can be pinned in place and both condyles cut in a standard fashion.
The proximal tibia is cut next, and, by doing that, more room is made for subsequently sizing and rotating the femoral component (the most difficult part of any MIS TKA). Three retractors are placed precisely to get good exposure of the entire surface of the tibia: a pickle-fork retractor posteriorly provides an anterior drawer and protects the neurovascular structures, and bent Hohmann retractors medially and laterally protect the collateral ligaments and define the perimeter of the tibial bone (Fig. 4). The tibial resection is done with an extramedullary guide optimized for small incision surgery. The tibia is cut in one piece using a narrow but thick saw blade that fits the captured guide. The narrow blade is more maneuverable in the smaller guide and provides better tactile feedback for the surgeon to detect when the posterior and lateral tibial cortices have been cut.
After the distal femur has been cut, the tibia is prepared next, and that is done to provide more working room for subsequently sizing and rotating the femoral component (the most difficult part of any MIS TKA). Good exposure of the entire surface of the tibia is accomplished with three retractors placed precisely: a pickle-fork retractor posteriorly to provide an anterior drawer, and bent Hohmann retractors medially and laterally to protect the collateral ligaments and define the perimeter of the tibial bone
The femoral sizing and rotation guide is thin enough to be pinned to the distal femur, and then the knee can be brought out to 60° of flexion to visualize the anterior femur for accurate sizing (Fig. 5). At 60° of flexion, a retractor is placed anteriorly, and the surgeon can see under direct vision that the femoral cortex will not be notched. Clearing some of the synovium overlying the anterior femoral cortex helps ensure that femoral sizing is accurate. The femoral finishing guide is adjusted medially or laterally. Femoral rotation is confirmed by referencing the surgeon’s choice of the posterior condyles, Whiteside’s line, or the transepicondylar axis, each of which can be defined with this subvastus approach. After the femoral and tibial cuts are made, the surgeon can carry out final ligament releases and check flexion and extension gap balance in whatever fashion is desired.
Patellar preparation with this surgical approach is left until the end. Cutting the patella is not required for exposure, and, by preparing the patella last, the risk of inadvertent damage to the cut surface of the patella is minimized. The patella cut is done freehand or with the surgeon’s choice of cutting or reaming guides. When a patellar cutting guide is used, the trial components are removed because then the entire limb can shorten, taking tension off the extensor mechanism and allowing easier access to the patella for preparation.
The modular tibial tray is cemented first, then the femur, and finally the patella. The tibia is subluxed forward with the aid of the pickle-fork retractor, and the medial and lateral margins of the tibia are exposed well with 90° bent Hohmann retractors. Care is taken to remove excess cement from around the tibial base plate, particularly posterolaterally. The femur is exposed for cementing by placing bent Hohmann retractors on the medial and lateral sides proximal to the collateral ligament insertions on the femur. A third retractor is placed under the VMO, where it overlies the anterior femur. Cement is applied to the entire undersurface of femoral implant prior to impaction. Special attention is paid to removing excess cement from the distal lateral surface of the femur because this area is difficult to see after the patella is cemented in place (Fig. 6). At this point, the real tibial insert can be placed or a trial insert can be used at the surgeon’s discretion. The patella is cemented last. After the cement has hardened, the knee is put through a range of motion, and final balancing and patellar tracking are assessed (Fig. 7).
The tourniquet is deflated so that any small bleeders in the subvastus space can be identified and coagulated. The closure of the arthrotomy starts by reapproximating the corner of capsule to the extensor mechanism at the midpole of the patella. Then three interrupted zero Vicryl sutures are placed along the proximal limb of the arthrotomy (Fig. 8). These sutures can usually be placed deep to the VMO muscle itself and grasp either fibrous tissue or the synovium attached to the distal or undersurface of the VMO instead of the muscle itself. These first four sutures are most easily placed with the knee in extension but are then tied with the knee at 90° of flexion to avoid overtightening the medial side and creating an iatrogenic patella baja postoperatively. A deep drain is placed in the knee joint, and the distal/vertical limb of the arthrotomy is closed with multiple interrupted zero Vicryl sutures placed with the knee in 90° of flexion. The skin is closed in layers. Staples are used, not a subcuticular suture. More tension is routinely placed on the skin during MIS TKA surgery than in standard open surgery, and our experience suggests the potential for wound-healing problems is magnified if the skin is handled multiple times as is the case with a running subcuticular closure.
The tourniquet should be let down, and any small bleeders in the subvastus space should be cauterized. The closure is done by first reapproximating the corner of capsule at the midpole of the patella. Then three interrupted sutures are placed through the deep layer of synovium to close the knee joint itself. Those four sutures are tied with the knee at 90° of flexion to avoid creating iatrogenic patella baja
Discussion
Minimally invasive total knee arthroplasty with a subvastus approach has proved reliable, reproducible, and efficient. The technique is amenable to stepwise surgeon learning and can be applied to a substantial range of patients who require total knee arthroplasty not just a selected subgroup. There are patients who are not good candidates for any MIS TKA procedure, including those with marked knee stiffness, fragile skin, or marked obesity. Similarly, any knee with patella baja will be markedly difficult with an MIS approach because subluxing the patella laterally often is not possible. In those cases, a traditional skin incision and more extensile exposure are in the interest of patient and surgeon alike.
Surgeons should be aware that changes in surgical technique alone are unlikely to provide the dramatic early improvements in postoperative function that some surgeons have described after MIS TKA. Maximizing the early gains after surgery (minimal pain, early ambulation, rapid hospital discharge) typically requires a combination of advanced anesthetic techniques, a multimodal pain management program, a rapid rehabilitation protocol, and appropriate patient expectations. How much each of those contributes versus how much the surgical technique contributes to early functional improvement has not been determined scientifically.
References
Pagnano MW, Meneghini RM, Trousdale RT. Anatomy of the extensor mechanism in reference to quadriceps-sparing TKA. Clin Orthop Relat Res. 2006;(452):102–5.
Chang CH, Chen KH, Yang RS, Liu TK. Muscle torques in total knee arthroplasty with subvastus and parapatellar approaches. Clin Orthop Relat Res. 2002;398:189–95.
Faure BT, Benjamin JB, Lindsey B, Volz RG, Schutte D. Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty. 1993;8(5):511–6.
Gore DR, Sellinger DS, Gassner KJ, Glaeser ST. Subvastus approach for total knee arthroplasty. Orthopedics. 2003;26:33–5.
Hoffman AA, Plaster RL, Murdock LE. Subvastus (southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70–7.
Aglietti P, Baldini A. A prospective, randomized study of the mini subvastus versus quad-sparing approaches for TKA. Presented at the Interim Meeting of the Knee Society. September 8, 2005, New York.
Roysam GS, Oakley MJ. Subvastus approach for total knee arthroplasty: a prospective, randomized, and observer-blinded trial. J Arthroplasty. 2001;16:454–7.
Pagnano MW, Leone JM, Hanssen AD, Lewallen DG. Minimally invasive total knee arthroplasty with an optimized subvastus approach: a consecutive series of 103 patients. Presented at American Academy of Orthopaedic Surgeons Annual Meeting. 2005, Washington, DC.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this entry
Cite this entry
Pagnano, M.W. (2016). MIS TKA with a Subvastus Approach. In: Scuderi, G., Tria, A. (eds) Minimally Invasive Surgery in Orthopedics. Springer, Cham. https://doi.org/10.1007/978-3-319-34109-5_59
Download citation
DOI: https://doi.org/10.1007/978-3-319-34109-5_59
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34107-1
Online ISBN: 978-3-319-34109-5
eBook Packages: MedicineReference Module Medicine