Abstract
Introduction
Aim of this study was to evaluate outcomes of operative as compared to conserveative treatment for two-part humerus fractures at the surgical neck.
Methods
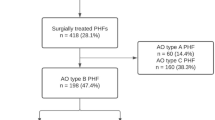
Data from a prospective multi-centre cohort study on four treatment options (conservative treatment and three implants, i.e. LPHP, PHILOS and PHN) for proximal humerus fractures were evaluated in this post hoc analysis. All patients with two-part fractures of the surgical neck (AO types A2, n = 54 and A3, n = 110) were identified and included for the analysis. All operatively treated patients were gathered and compared to those receiving conservative treatment. Primary outcome parameters were pain, range of motion and absolute and relative Constant scores at 3, 6 and 12 months following injury and coronal plane alignment at 12 months.
Results
Operative (n = 133) and non-operative (n = 31) groups were comparable with regard to all parameters assessed including mean age (62.9 vs. 65.6, P = 0.479), gender (27 vs. 29 % male, P = 0.826) and fracture distribution (65 vs. 77 % A3 type, P = 0.207). 26 of the 31 conservatively treated and 103 of the 133 operatively treated patients (84 and 77 %, respectively) were available for final follow-up. There was a continuous improvement for all outcome parameters in both treatment groups (P < 0.001). Operative treatment resulted in a more effective reduction of pain at 3 months (51 vs. 76 % reporting pain at fracture site, P = 0.03) and a reduction of coronal plane malalignment. Both range of motion and Constant scores were, however, comparable in both groups at all follow-up visits. Relative and absolute Constant scores were generally excellent at final follow-up (74 vs. 74, P = 0.528 and 89 vs. 91, P = 0.494, respectively).
Conclusions
Both non-operative treatment and operative treatment using modern implants (LPHP, PHILOS and PHN) can be considered safe and effective treatment options for two-part fractures of the proximal humerus. Operative treatment may result in better range of motion and reduced pain in the early postoperative course of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the proximal humerus can be regarded as common injuries with a reported yearly incidence of ~66/10,000 [13]. Associated with osteoporosis, proximal humerus fractures rarely affect patients under 60 years of age and reduced bone quality poses significant challenges for treatment of these injuries [18, 20]. Operative therapy is prone to inherent and partially unsolved problems and has been shown to be associated with markedly high complication rates [18]. Conservative treatment has proved a safe treatment option associated with reasonable functional outcome for fractures of the proximal humerus of different complexity [5, 6, 8, 22, 23]. Owing to the good results of conservative treatment, operative treatment for two-part fractures of the proximal humerus has been questioned by some authors [6, 8]. However, the most relevant study [6] comparing operative to conservative treatment of this entity had several flaws, namely a small number of operatively treated patients and high rates of incomplete reduction. Moreover, flexible nailing and tension band wiring, techniques that have more and more been abandoned in the presence of modern fixation devices, were used for stabilisation in all cases.
Fostered by advancements in implant design, namely the introduction of locked plates and intramedullary nails with spiral blades (angular stable proximal fixation) promising enhanced stability even in osteopenic cancellous bone and in presence of severe comminution operative treatment has more recently been advocated by various authors, particularly for more displaced fractures and in younger patients [1, 9, 11, 19]. The aim of the present analysis was therefore to compare the outcomes of non-operatively treated patients with two-part fractures of the proximal humerus to those treated operatively using modern implants (intramedullary nails and locking plates).
Materials and methods
Patient inclusion and treatment
Data used in this analysis have been collected prospectively in the context of a large cohort study that was performed as a series of four separate case series (i.e. treatment arms, with similar protocols and case report forms). There was one non-operative group, which was exclusively enrolled in one centre [8], and three operative groups [2, 3, 21] using three different standard AO implants (Synthes, Solothurn, Switzerland) in 27 other level I trauma centres, whereby each centre used only one, i.e. the locking proximal humerus plate (LPHP), the proximal humerus internal locking system (PHILOS) or the proximal humerus nail (PHN). The study was designed in a way that within the study period all patients who met the inclusion criteria were treated with the treatment option assigned to the respective centre, irrespective of displacement or stability, i.e. all patients were treated conservatively in the “conservative” centre and all patients were treated operatively using the assigned implant in the various “operative” centres.
All patients with two-part fractures of the surgical neck (i.e. A2 and A3 type fractures according to AO classification) included in the underlying cohort study were identified and taken for this post hoc analysis. Exclusion criteria included pseudarthrosis, pathological fractures and refractures, open fractures or concomitant fractures of the ipsilateral elbow or distal radius. In addition, patients with existing disorders having a relevant effect on the healing process and function such as multiple sclerosis, paraplegia or other relevant neurological disorders, polytraumatized patients with an Injury Severity Score (ISS) exceeding 16 or patients with pre-existing plexus injury or nerve palsy were excluded.
Eight and 70 surgeons were involved in the non-operative and operative groups, respectively. Treating surgeons were fellowship-trained trauma surgeons and had to have performed at least 30 proximal humerus fracture stabilisation procedures and 5 with the respective Synthes implant used in the study. All operative procedures were performed using standard approaches (i.e. delta-split approach for PHN and anterior deltoideo-pectoral approach for LPHP and PHILOS) and AO reduction techniques and implants were used according to manufacturer’s recommendations. Postoperatively, the arm was immobilised in a sling and passive ROM exercises were started within 2 days after surgery. Controlled active mobilisation with abduction and flexion beyond 90° was started 1–3 weeks postoperatively, depending on the stability of the osteosynthesis and bone quality.
Conservative treatment included immobilisation of the shoulder in an arm sling for 1–3 weeks with passive ROM exercises starting after 1 week. Controlled active mobilisation was allowed after 4 weeks. Initial closed reduction manoeuvres were allowed at discretion of the treating physician.
Data collection
During hospitalisation, patient demographics (i.e. gender, age, dexterity, smoking, concomitant diseases, and medication) and baseline characteristics (i.e. date of accident, accident type, energy level of trauma, concomitant injuries, fracture classification, date of surgery, operation time, c-arm counter time, additional implants and sutures, additional medication, type and duration of immobilisation, and beginning of active assisted and unrestricted mobilisation) were recorded. Fractures were classified according to the AO-Müeller classification [14] by the treating surgeon using plain radiographs and intraoperative fracture visualisation.
Scheduled follow-up visits were performed 3, 6 and 12 months following injury. At each follow-up visit, the patients were examined and interviewed concerning their pain, shoulder mobility and strength and the Constant scores [4] of the injured and the contralateral shoulder were obtained. Isometric muscle strength was assessed using a Nottingham Mecmesin Myometer (Mecmesin Co, Nottingham, UK). The tests were performed with the shoulder at 90° abduction, or, if 90° could not be reached, in maximum active abduction as described by Constant [4]. Patients were asked to maintain this resisted abduction for 5 s. The mean of three tests was recorded as strength of the shoulder. Patients with a history of trauma or prior surgery involving the contralateral shoulder were not taken into consideration for the contralateral Constant scores at follow-up visits. At the 12-month follow-up visit we additionally obtained Neer scores [15] for each patient.
True AP and trans-scapular Y view radiographs were obtained postoperatively (in case of operative treatment) and subsequently at each follow-up visit. The treating surgeon evaluated the radiographs primarily for fracture healing and possible occurrence of complications. All radiographs and collected clinical data were jointly reviewed by two of the authors to validate complication records and define their most likely influencing factors, as well as document final deformity (valgus/varus deviation) at the fracture site.
Data management and statistics
Study monitoring, database management and statistics were carried out at a central monitoring organisation. Patients who had undergone conservative treatment were compared to those operatively treated regarding baseline demographics and injury parameters using standard descriptive statistics and non-parametric univariable tests. Observed differences between the groups were considered carefully by clinical judgement; variables with differences potentially confounding the outcome comparisons were considered for adjustment in multivariable analyses.
Treatment groups were compared regarding shoulder function and health status at 3, 6, and 12 months. For each continuous outcome, any repeated measurements of each patient were pooled and analysed together in one overall multivariable linear regression model. The likelihood ratio test was used to test the null hypothesis that there would be no difference in shoulder function and health status between the two groups. The analyses of absolute Constant score and range of motion values were adjusted for respective contralateral healthy side values, as appropriate. For each patient the mean of contralateral values recorded across follow-up examinations was used as reference value. Four dichotomous parameters (pain at each follow-up examination, occurrence of local complications within 1 year) were analysed by multivariable binomial regression, and adjusted risk ratios (RR) were used to quantify treatment effect.
We made a post hoc power analysis using repeated measures ANOVA and the Constant and Murley score. Group sizes of 26 and 103 patients, respectively (i.e. as examined at 1-year follow-up), provided >99 % power to detect a minimum difference of 10 points in the Constant and Murley score with a known standard deviation of 13; the correlations between contralateral and injured sides, and between follow-ups were set to 0.50 and 0.80, respectively. For achieving a power of 90 %, 14 and 61 patients in both groups would have been required.
Results
This analysis included 31 patients (one clinic) with two-part fracture in the non-operative and 133 patients (21 clinics) in the operative group. Final 1-year follow-up data were available from 26 to 103 patients (84 and 77 %) in non-operative and operative groups, respectively. Both groups were comparable with regard to all demographic parameters assessed (Table 1); analyses, however, were adjusted for age, presence of comorbidities, energy level of injury, dominant arm injured and fracture type to control for a potential confounding effect.
There was a continuous and highly significant improvement over time for all outcome parameters (pain, range of motion, absolute and relative Constant scores) assessed in patients from both non-operative and operative treatment groups (P < 0.001).
Operatively treated patients were less likely to suffer from pain at fracture site at the 3-month follow-up visit as compared to conservatively treated patients (51 vs. 76 %, P = 0.03). This difference was, however, not observed at 6- and 12-month follow-up (Table 2). Shoulder function was generally excellent at 12-month follow-up and average relative Constant scores approximating 90 % of the uninjured side were observed in both treatment groups (Table 3). Mean Neer scores at 12-month follow-up exceeded 80 in both groups and were slightly better in the non-operative group (88.6 vs. 84.7, P = 0.02; Fig. 1). According to Neer’s outcome criteria, 85 and 73 % of patients in the non-operative and operative group were found to have satisfactory or excellent results at final follow-up, respectively (P = 0.28, n.s.). With the exemption of passive external rotation at 3 (in favour of conservative treatment) and 12 months (in favour of operative treatment), operative treatment did not result in superior or inferior ranges of motion at any of the follow-up visits even though there was a tendency towards improved abduction and flexion at 3 months in the operative treatment group (Table 4).
Anatomical reduction defined as varus malalignment of no more than 15° was achieved in 93 of 133 operatively treated patients (70 %). Radiographic analyses at 1-year follow-up revealed that operative treatment resulted in a marked improvement of coronal plane alignment (Fig. 2). In particular, there was a significant reduction of varus malalignment exceeding 15° (OR 0.38, 95 % CI 0.15–0.95, P = 0.038). Interestingly, there was a significant impairment of absolute Constant scoring in the operative group when varus malalignment exceeded 15° (92.2 vs. 83.0, P = 0.0006). On the contrary, varus malalignment did not have a significant effect on Constant scoring in the conservative group (Fig. 3).
Complications are summarised in Table 5. All but one operated fractures showed bony union at 12-month follow-up, there was one case of avascular necrosis and one deep infection in the operative group. Generally, there was a non-significant tendency towards a higher complication rate in surgically treated patients (RR = 4.9; 95 % CI 0.66–36.0, P = 0.1 for operative over non-operative treatment). Moreover, implant-associated complications (such as plate impingement, screw cut out, etc.) correlated with excessive varus malalignment (RR = 2.5; 95 % CI 1.7–3.6; P = 0.0002).
Discussion
The aim of this analysis was to compare the outcomes of operative to non-operative treatment strategies in patients with isolated two-part surgical neck fractures of the proximal humerus. The most important finding of the present analysis was that both operatively and non-operatively treated patients can expect reasonable shoulder function and, if any, superiority of operative over non-operative treatment can only be expected in the first 3 months following injury.
Appreciation for the strengths and limitations of the present study is warranted. First and foremost patients were not randomly assigned to either one of the treatment groups; the choice of therapy was left at discretion of the treating physician and lastly of the patient. Therefore, some selection bias cannot be excluded. Randomisation of patients would have been desirable to increase internal validity. However, the original study behind this post hoc analysis was designed as four separate prospective cohort series (PHN, LPHP, PHILOS and conservative) in which one centre recruited conservatively treated patients and each of the remaining participating centres was to exclusively enrol patients treated with either one of the respective implant to yield the highest possible quality for the individual surgical procedures. Since all conservatively treated patients were recruited at a single institution, the results may not necessarily reflect general results of conservative treatment and be influenced by both patient characteristics and treatment experience. In this context it is, however, important to state that during the study period not a single two-part fracture was treated operatively in the institution that enrolled conservatively treated patients, i.e. there was no selection bias in that more displaced fractures were assigned to operative treatment. Yet of course, it remains unrevealed whether patients had elected not to show up again and move to another (operative) centre. Vice versa, throughout the study period, all patients who met the inclusion criteria and agreed to participate in the study were treated operatively in the hospitals allocated to one of the three operative arms, limiting the possible bias that less displaced fractures were treated conservatively. It, however, remains unclear, whether and if, how many patients opted for conservative treatment and refused to participate in the study. However, both groups were comparable with respect to all demographic parameters assessed. It is a particular strength of the analysis that only two-part fractures of the surgical neck were included resulting in a rather homogenous patient sample despite the fact that initial displacement was not assessed. We, moreover, statistically adjusted for available factors that could have had an influence on the results.
Follow-up rates were reasonably high at all visits. Still, more unfavourable results in patients lost to follow-up cannot be fully excluded—a phenomenon that has been reported for studies on the outcome of patients undergoing total knee replacement [10]. It does, however, not seem unreasonable to presume that if there was an effect of drop-outs, it would comparably have affected both groups. The maximum follow-up of 1 year may seem relatively short. It has, however, been shown that long-term outcome can be predicted fairly well at this time and little improvement nor deterioration of function can be expected after that point [16].
Expectedly and in accordance with most studies on proximal humerus fractures, both subjective and objective outcome parameters improved continuously over the observation period [5, 6, 8, 11]. Constant scores at 1-year follow-up were generally excellent in both groups and in the range of those reported for locking plate fixation of two-part fractures [7, 9, 17]. Neer scores at final follow-up were slightly better than those in the series of Court-Brown et al. [6]. Given the well-known reciprocal correlation of age and outcome of proximal humerus fractures [6], this may most likely be attributed to the younger patient sample in the present analysis as compared to the cohort reported on by Court-Brown et al. [6].
Overall Neer scores at 1-year follow-up were slightly better in the non-operative as compared to the operative treatment group while Constant scores were comparable. Differences were, however, small and most likely reflect that pain at fracture site contributes more points to Neer as compared to Constant scoring. Given the multiplicity of outcomes and statistical tests implemented, such minor difference and marginal significance may also have occurred by chance alone, and thus should be interpreted with caution.
Operative treatment resulted in reduced pain and a tendency towards better range of motion in both flexion, abduction and passive rotation as compared to non-operative treatment at the 3 month follow-up. It is reasonable to conceive that a higher initial stability translating to pain reduction and allowing for more aggressive physiotherapy in the early course of treatment may account for this observation.
Expectedly, radiographic analyses revealed a significant reduction of coronal plane malalignment in the operative group. The improvement of alignment observed in the operative group did, however (at least for two-part fractures), not translate to better overall outcomes. Interestingly, varus malalignment exceeding 15° was associated with an impairment of Constant scores in the operative group. On the contrary, varus malalignment did not have a significant effect on Constant scoring in the non-operative group––an observation that is in accordance with that of Court-Brown et al. [6] who found no correlation of outcome and alignment. We can only speculate why varus malalignment seems to have a detrimental effect on the outcome of operatively treated patients. One possible explanation might be a higher rate of implant-associated complications (such as plate impingement or implant failure) in cases with excessive varus malalignment. In fact, implant related complications were significantly more frequent in cases of excessive varus malalignment. The causality, however, remains unclear. One could argue that such complications lead to a loss of reduction and therefore resulted in malalignment. Secondary dislocation can certainly account for some of the malalignments. Dislocation rates were, however, not high enough to explain for all the malalignments observed. They may more likely be the result of insufficient reduction at time of surgery. We therefore hypothesise that increased implant-associated complications may be a consequence of insufficient restoration of alignment (i.e. insufficient reduction).
Non-union is rarely considered a problem in two-part fractures of the proximal humerus and rates of <5 % have been reported [6]. Accordingly, only one case of non-union was observed in the present series. In accordance with previous reports on operative stabilisation of proximal humerus fractures, most of the complications were implant failures (particularly primary and secondary screw perforation and loss of reduction) and could partially be attributed to an insufficient operative procedure.
Infections are uncommon affecting ~1 % of all operatively treated patients. Accordingly, there was only one case of deep infection in the present series. The overall complication rates were low as compared to other studies on operative treatment of proximal humerus fractures [12, 18–20]. This can, however, almost certainly be attributed to the fact that only two-part fractures were included in the present analysis which are notoriously less frequently associated with complications when compared with three- and four-part fractures or fracture dislocations of the proximal humerus. In summary, with regard to the present analyses both non-operative and operative treatment can be considered viable options for two-part humerus fractures. Further sufficiently powered randomised controlled trials are warranted to identify patients who will benefit most from operative treatment.
Conclusion
Both non-operative treatment and operative treatment using modern implants (LPHP, PHILOS and PHN) can be considered safe and effective treatment options for two-part fractures of the proximal humerus. Operative treatment may result in better range of motion and reduced pain in the early postoperative course of treatment. However, these effects diminish over time and outcome will be similarly good 1 year upon injury regardless of choice of treatment. Varus malalignment, despite more frequently observed in the conservative group, did not affect the outcome of conservatively treated patients. On the contrary, higher complication rates and impaired shoulder function were associated with excessive varus malalignment in the operative group. With regard to the good results achieved by conservative treatment, operative treatment for two-part fractures of the proximal humerus should be indicated with caution, possibly reserved to cases in which early pain reduction and regain of shoulder function is of importance, e.g. younger patients or patients with functional impairment of the contralateral arm. Meticulous restoration of alignment should be aspired whenever opting for operative treatment.
References
Agudelo J et al (2007) Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma 21(10):676–681
Blum J et al (2009) Angle-stable intramedullary nailing of proximal humerus fractures with the PHN (proximal humeral nail). Oper Orthop Traumatol 21(3):296–311
Brunner F et al (2009) Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma 23(3):163–172
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Court-Brown CM et al (2002) Impacted valgus fractures (B1.1) of the proximal humerus. The results of non-operative treatment. J B Jt Surg Br 84(4):504–508
Court-Brown CM et al (2001) The translated two-part fracture of the proximal humerus. Epidemiology and outcome in the older patient. J B Jt Surg Br 83(6):799–804
Handschin AE et al (2008) Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury 39(3):306–313
Hanson B et al (2009) Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoul Elb Surg 18(4):612–621
Helwig P et al (2009) Does fixed-angle plate osteosynthesis solve the problems of a fractured proximal humerus? A prospective series of 87 patients. Acta Orthop 80(1):92–96
Kim J et al (2004) Response bias: effect on outcomes evaluation by mail surveys after total knee arthroplasty. J B Jt Surg Am 1(86-A):15–21
Konrad G et al (2010) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J B Jt Surg Am 92(1 Pt 1):85–95
Kostler W et al (2003) Proximal humerus fracture in advanced age. Treatment with fixed angle plate osteosynthesis. Chirurg 74(11):985–989
Lanting B et al (2008) Proximal humeral fractures: a systematic review of treatment modalities. J Shoul Elb Surg 17(1):42–54
Mueller M, Narzarian S (1990) The comprehensive classification for fractures of long bones. Heidelberg, Springer, New York, Berlin
Neer CS 2nd (1970) Displaced proximal humeral fractures I. Classification and evaluation. J B Jt Surg Am 52(6):1077–1089
Olsson C et al (2005) Long-term outcome of a proximal humerus fracture predicted after 1 year: a 13-year prospective population-based follow-up study of 47 patients. Acta Orthop 76(3):397–402
Siwach R et al (2008) Internal fixation of proximal humeral fractures with locking proximal humeral plate (LPHP) in elderly patients with osteoporosis. J Orthop Traumatol 9(3):149–153
Sproul RC et al. (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42(4):408–413
Strohm PC et al (2007) Locking plates in proximal humerus fractures. Acta Chir Orthop Traumatol Cech 74(6):410–415
Strohm PC et al (2008) Proximal humerus fracture––what to do? Z Orthop Unfall 146(3):312–317
Sudkamp N et al (2009) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J B Jt Surg Am 91(6):1320–1328
Urgelli S et al (2005) Conservative treatment versus prosthetic replacement surgery to treat 3- and 4-fragment fractures of the proximal epiphysis of humerus in the elderly patient. Chir Organi Mov 90(4):345–351
Zyto K (1998) Non-operative treatment of communited fractures of the proximal humerus in elderly patients. Injury 29(5):349–352
Acknowledgments
The authors wish to thank all the following investigators and clinics for their participation in this study: Operative study arm: PHN: Centro Traumatologico Ortopedico, Firenze, Italy (R.Angeloni); UZ Gasthuisberg, Leuven, Belgium (S. Nijs); Royal Liverpool University Hospital, Liverpool, United Kingdom (C. Sinopidis); Johannes Gutenberg Universitätsklinikum, Klinik für Unfallchirurgie, Mainz, Germany (J. Blum); Università di Padova, Ortopedia e Traumatologia, Padova, Italy (A. Olmeda); Vogtlandklinikum Plauen, Plauen, Germany (W. Merbold); Kardinal Schwarzenberg’schen Krankenhaus, Abteilung für Unfallchirurgie, Schwarzach, Austria (F. Genelin); Unfallkrankenhaus Meidling, Wien, Austria (H. Matuschka); Klinikum Worms gGmbH, Worms, Germany (J. Blum) PHILOS: Rätisches Kantons- und Regionalspital, Chur, Switzerland (C. Sommer); Hôpital Cantonal de Fribourg, Fribourg, Switzerland (G. Kohut); Westpfalz-Klinikum GmbH, Unfallchirurgie Klinik, Kaiserslautern, Germany (H. Winkler); Kantonsspital Luzern, Chirurgie/Traumatologie, Luzern, Switzerland (R. Babst); Klinikum Rosenheim, Unfall- und Wiederherstellungschirurgie, Rosenheim, Germany (G. Regel); BG Unfall- und Universitätsklinik, Tübingen, Germany (D. Höntzsch) LPHP: Charité Universitätsmedizin Berlin, Zentrum für Muskuloskeletale Chirurgie, Berlin, Germany (N. Haas); Allgemeines Krankenhaus Celle, Celle, Germany (H-J. Oestern); Albert-Ludwigs-Universität, Orthopädie und Traumatologie, Freiburg, Germany (N. Südkamp); Universitätsklinik für Unfallchirurgie Graz, Graz, Austria (M. Plecko); Evangelisches Diakoniewerk Friederikenstift, Unfallklinik, Hannover, Germany (H. Lill); Universität Leipzig, Klinik für Unfall- und Wiederherstellungschirurgie, Leipzig, Germany (C. Josten). Non-operative study arm: York District Hospital, York, United Kingdom (P. De Boer)
Author information
Authors and Affiliations
Corresponding author
Additional information
O. Hauschild and G. Konrad state that they have contributed equally to this manuscript and therefore apply for shared first authorship.
Rights and permissions
About this article
Cite this article
Hauschild, O., Konrad, G., Audige, L. et al. Operative versus non-operative treatment for two-part surgical neck fractures of the proximal humerus. Arch Orthop Trauma Surg 133, 1385–1393 (2013). https://doi.org/10.1007/s00402-013-1798-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1798-2