Abstract
We conducted a systematic review of the literature on the use of both resorbable and non-resorbable cement as an adjunct to internal fixation of intertrochanteric hip fractures. Two reviewers independently assessed the methodological quality and extracted relevant data from each included study. In cases in which the outcomes data were similar between studies, data were pooled and analyzed. Seven studies were included after fulfilling all inclusion and exclusion criteria. Two hunderd and eighty patients were treated with augmentation and 175 were treated without augmentation. Studies were variable in their ability to demonstrate better functional outcomes in patients who underwent augmentation. However, radiographic parameters (mean lag screw sliding distance and varus deformity) were better in the augmentation group. In terms of complications, failure to use augmentation with a sliding hip screw device in five studies led to 10.8-fold higher likelihood of construct failure (p < 0.01). Augmentation of intertrochanteric femur fractures with polymethyl methacrylate or calcium–phosphate may provide benefits in terms of radiographic parameters and complication rates; however, more stringent research methodology is necessary to determine the extent of the benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intertrochanteric hip fractures are extra capsular fractures of the proximal femur, occurring between the greater and lesser trochanter. Along with fractures of the femoral neck, the incidence of these fractures is expected to increase to nearly a half million by the year 2040, with intertrochanteric fractures constituting nearly half of this number [1, 2]. The blood supply to the intertrochanteric region of the hip is highly vascular. Biomechanical stability to promote fracture healing can be provided by either a sliding hip screw or cephalomedullary device. Despite this theoretically healthy environment for fracture healing and standardized means of treatment, complications, especially in patients with severe osteoporosis, do occur. Specifically, loss of proximal fixation or cut-out, can occur when adequate fixation is not achieved in the femoral head, predicted by the tip-to-apex distance of the compression screw [3]. When failure occurs because of loss of proximal fixation or lack of an adequate buttress to support compression, the proximal femur collapses into varus with catastrophic failure of the bone implant interface.
In an effort to augment the poor bone quality of osteoporotic patients with intertrochanteric hip fractures, some published series have advocated for the addition of resorbable calcium-phosphate (CP) or non-resorbable polymethyl methacrylate (PMMA) cement to the internal fixation construct to decrease the rates of cutout and collapse. In addition, biomechanical studies in cadaveric specimens have shown decreased rates of femoral head collapse in osteoporotic models supplemented with PMMA [4–7]. As osteoporosis is a pathologic process of bone, the technique of augmentation has been utilized in a limited number of clinical studies to determine whether absorbable or non-absorbable materials have the ability to decrease the complication rate or affect the clinical outcomes of patients with intertrochanteric hip fractures treated with standard techniques.
The purpose of this paper is to systematically review the literature on the use of both resorbable and non-resorbable cement as an adjunct to internal fixation of intertrochanteric hip fractures. We have done this to provide a review of the demographics, surgical techniques, outcomes, and complications of patients in which these techniques were used.
Methods
Search strategy and eligibility
We searched the Medline and EMBASE computerized literature databases from January 1980 to May 2011. Articles were identified using an electronic search of keyword terms and their respective combinations (Table 1). All studies from the mentioned searches were then reviewed. Studies were included in this systematic review if they matched the following criteria: (1) they were in English language; (2) they were randomized trials or observational studies (therapeutic studies level I–IV and prognostic studies level I–IV) with minimum follow-up of 6 months for all patients. Six months follow-up was selected as a time-point by which clinical and radiographic healing would be expected to have taken place. We excluded review articles, case reports, and technique articles without reported patient data. Two authors performed the initial search and then three of the authors independently reviewed the references of the qualifying papers and selected the appropriate studies based on these criteria. If one or more authors selected a paper, it moved on to the next phase. In the final phase of review (elimination by full text review), there was no disagreement over which papers would be ultimately included.
Validity assessments
Data were subsequently extracted from these papers including: demographics, techniques, outcomes, and complications of patients who underwent PMMA or CP augmentation for unstable intertrochanteric femur fractures. In addition, demographic data from each study was obtained. Three reviewers assessed the methodological quality of the studies according to Zaza et al. [8]. Zaza et al. [8] described a systematic quality assessment for observational studies that evaluated preventive medicine interventions. The use of cement in intertrochanteric fractures can be considered a preventive medicine intervention by preventing complications based on supplementation of osteoporotic bone. The method of Zaza et al. [8] of assessing study quality entails a checklist, which spans five major areas of study design: a description of the population and intervention, sampling, measurement, data analysis, and interpretation of results. No summary score is generated for this tool. The reviewers resolved disagreement by discussion and consensus by majority.
Analysis
We assessed for heterogeneity via the Q statistic and the I2 confidence interval. We found that the Q statistic was non-significant (p value = 0.59), however, because we had a small number of studies (n = 7) the I2 confidence interval was wide (0, 71 % variability). As such, we used a random effects model to obtain cumulative meta-analysis results in comparative studies which had the requisite data because it was more conservative. In cases where the data were continuous and mean and standard deviation data were available from the manuscripts, we used the inverse variance method of random effects modeling. In cases where the data of interest were dichotomous, a Der Simonian and Laird random effects model was generated for the purpose of generating p values. A correction factor of 0.5 was added to each cell in the case of zero events in the comparative studies to include the maximum amount of information. In cases where not enough data were present, the results of individual studies were reported, or frequency-weighted means with variance determined by the number of studies were used. We used an Egger’s intercept to determine the evidence of publication bias. MIX software (version 1.7) was used for meta-analysis.
Results
We obtained 13,055 unique articles from a combined Medline and EMBASE search using the criteria listed in Table 1 (Fig. 1). Duplicates were electronically confirmed with use of RefWorks bibliographic software (ProQuest, LLC, Bethesda, MD). We initially excluded articles by title (12,824 excluded) for irrelevance to the topic in question, if they were picked up by chance, or if they were designated as reviews, editorials, or commentaries. An additional 152 articles were eliminated after reviewing the abstracts; we eliminated articles by abstract only if they were case reports, erratum, or reviews. If there was any question over inclusion, we undertook a review of the full text of the work. We then reviewed the full text of the remaining 79 articles, of which 73 articles failed to meet our inclusion and exclusion criteria. This systematic review left six articles for analysis. The references of these articles (along with the prior individual searches) were manually searched for other potential articles of interest. The references were screened in the same manner as the articles from the original search (title review followed by abstract review, then full text review). One additional article meeting the inclusion and exclusion criteria was included from the references. This resulted in a total of seven articles to be included in this systematic review [9–15].
Five studies included a control group of patients treated without PMMA or CP augmentation and all studies evaluated a uniform cohort of patients who had undergone fixation of unstable intertrochanteric femur fractures [9, 11–14]. No other materials were used for augmentation. Three studies were retrospective [9, 10, 15] and four studies [11–14] were prospective in nature. Two studies [9, 13] were performed at more than one institution and all seven studies [9–15] were published between the years 1985 and 2010. The years in which surgery was performed was recorded in six studies [9–12, 14, 15] and fell between the years from 1977 to 2010. All studies reported minimum of 6 months follow-up in all patients. However, studies were variable in reporting data on mean and maximum follow-up. The greatest reported mean and maximum follow-up was 34 months and 62 months, respectively [9].
Quality/publication bias assessment
Of the studies reviewed, there were four prospective randomized controlled studies (level II) [11–14], one case control study (level III) [9], and two case series (level IV) [10, 15]. Six [9–12, 14, 15] of the seven studies described their population well, with one series [13] unclear as to how the patients were selected, and whether or not the entire population was used. All studies described their surgical technique well, though of note, the placement of the cement varied from study to study, as was the specific surgical technique [9–15]. Only two studies [11, 15] used the entire population available, though three of the remaining studies comprehensively described their exclusion of patients [9, 10, 12]. Four studies [11–14] employed randomization. One study [12] used randomization by patient medical record number (even or odd), and the remaining studies [11, 13, 14] used sealed envelope randomization. One of the seven studies employed specially trained physiotherapists to perform clinical assessments (a method of blinding) [13]. Two studies [10, 15] employed no statistical analysis at all, two reported p values [9, 11] but did not describe how they formulated those values, and the remaining studies described their statistical analysis adequately. One study was underpowered [14]. One study did not have 80 % follow-up [15]. Only one study employed statistical adjustment for multiple tests [12]. We found no significant publication bias in either of the two meta-analyses we were able to perform with the data available (p = 0.98 and 0.94), though our assessment is somewhat limited by the small number of studies.
Demographics
Six studies [9, 10, 12–15] utilized a dynamic hip screw (DHS) as the primary mode of fixation and one study [11] utilized an intramedullary device in all patients. Ages ranged from 54 to 99 years across all studies. Average ages ranged from 78.4 years of age to 85.3 years of age within each study. 35.7 % of the patients were male, 64.3 % were female. In total, the seven studies incorporated a total of 569 intertrochanteric femur fractures in adult patients, with 419 having adequate follow-up for outcomes evaluation. 280 were treated with augmentation and 175 were treated without augmentation. 121 were treated with DHS and PMMA augmentation, 3 were treated with a Holt nail and PMMA augmentation, 56 were treated with DHS and CP augmentation, 35 were treated with an intramedullary device and PMMA augmentation, 139 were treated with a DHS and no augmentation, and 36 were treated with an intramedullary nail and no augmentation. Each of the published studies utilized different techniques for augmentation of the internal fixation construct with resorbable or non-resorbable cement. Full demographic data for patients who underwent augmentation are available in Table 2.
Operative time and blood loss
Five studies [9, 10, 12, 13, 15] considered operative time and blood loss in patients undergoing DHS fixation with augmentation with either PMMA (four studies) or CP (n = 1 study). Augmentation trended to but did not significantly increase operative time (92.3 vs. 64.5 min, p = 0.117). It did, however, lead to an increased blood loss (422.2 vs. 318.3 ml, p = 0.049).
Functional outcomes
Three studies (n = 145) of PMMA augmentation and DHS fixation utilized the modified Salvati and Wilson rating system and showed 47 excellent, 66 good, 26 fair, and 6 poor results (Table 3) [10, 12, 15]. One study utilized the Iowa Hip Rating scale and noted lower scores in the group that underwent PMMA augmentation and DHS fixation compared to the control group (76 vs. 92, p = 0.01). One study [12] evaluated hip pain on a four-point scale: (1) no pain; (2) mild pain not affecting walking or requiring analgesic medication; (3) moderate pain affecting walking and/or requiring regular medication; (4) severe pain, even at rest, requiring stronger analgesics. At one-year follow-up, mean pain score was 1.6 in the group that underwent PMMA augmentation and DHS fixation, compared to 2.2 in the group that did not undergo augmentation (p = 0.008). The same study also evaluated walking ability via the mobility score of Parker and Palmer: a value of 0 indicates complete disability and a value of 9 indicates no difficulty. At one-year follow-up, mean mobility score was 5.3 in the PMMA augmented group and 4.2 in the control group (p = 0.073). One study [13] considered global pain and functional pain at 6 weeks and 6 months. They noted lower global pain scores (p < 0.003) and lower functional pain scores with walking 10 feet (p < 0.003) and 50 feet (p < 0.01) at 6 weeks with CP augmentation compared to controls. There was no difference at 6 months. The augmented group also demonstrated significant (p < 0.05) improvement compared to the control group on three SF-36 subscales (pain, general health, and vitality) at 6 weeks and five SF-36 subscales (physical functioning, vitality, social functioning, mental health, and general health) at 6 months. The one study [11] that utilized an intramedullary nail for fixation used the Harris Hip Score as their outcomes measure and noted a score of 57.91 in the PMMA augmented group compared to 59.86 in the control group at one-year follow-up. One study [14] with calcium-phosphate augmentation did not evaluate functional outcomes.
Radiographic outcomes
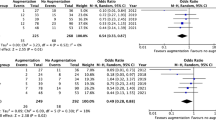
In one study, patients treated with and without PMMA augmentation and DHS fixation were compared by radiographic parameters at 1-year follow-up (Table 3) [12]. Amount of lag screw sliding (1.7 vs. 10.5 mm, p < 0.001), femoral shortening (3.8 vs. 14 mm, p < 0.001), and varus collapse (1.8° vs. 8.1°, p < 0.001) were greater in the non-cemented group. Both studies of CP augmentation evaluated follow-up radiographic parameters. Mattsson et al. note that at 6 months follow-up, the mean sliding distance of the screw in the CP augmented group was 13.5 mm compared with 15.9 mm in the control group. Mattsson and Larsson [14] evaluated radiographic parameters (translation and rotation) utilizing radiostereometry at 6 months follow-up. They noted statistically significant less total (7.77 vs. 13.24 mm, p < 0.05), lateral (4.84 vs. 10.66 mm, p < 0.05), and distal translation (6.21 vs. 11.96 mm, <0.01) in the CP augmented group compared to the control group. Similarly, they noted statistically significant decreased varus (5.89° vs. 10.57°, p < 0.05) in the CP augmented group compared to the control group. There were no statistically significant differences in anterior/posterior translation, forward/backward rotation, or retroversion/anteversion. The one study [11] that utilized an intramedullary nail for fixation noted a mean sliding distance of the femoral head screw of 12.7 mm in the PMMA augmented group compared to 14.2 mm in the control group (p = 0.09). Three studies met the criteria of having data regarding mean and standard deviation data for sliding on the hip screw [12–14]. Of these studies, the inverse variance weighted mean difference of −5.1 mm (favoring cementation) 95 % confidence interval −0.2, −10 (p = 0.04).
Complications
Each study considered complications, but there was variability in which complications were recorded and reported. The overall complication rate for all patients who underwent PMMA or CP augmentation was 8.6 % (24/280) (Table 4). When considering only studies that included a control group, the complication rate was 5.8 % (10/173) versus 22.3 % (39/175) in controls (p < 0.001). Augmented fractures demonstrated 13 screw cut-outs and no malunions while controls had 16 screw cut-outs and 18 malunions. Failure to use augmentation with a sliding hip screw device in five studies [10, 12–15] led to 10.8-fold higher likelihood of construct failure (p < 0.01).
Discussion
In elderly patients, intertrochanteric fractures of the femur are often associated with osteoporosis making it difficult to achieve stable and reliable fixation. Optimization of osteoporotic bone architecture prior to fracture surgery is not possible. Physicians have attempted to address poor bone quality and comminution with fixed angled devices, and in some cases, with PMMA or CP augmentation. This systematic review aimed to comprehensively assess the literature to determine the reported techniques, outcomes, and complications associated with bone augmentation during fixation of intertrochanteric femur fractures.
Techniques for introduction of PMMA or CP and for fracture fixation, with or without an osteotomy, are not standardized and an optimal delivery mechanism has not been established. Furthermore, the location of augmentation has been variable, with some investigators introducing PMMA into the femoral head while others have introduced CP, via curved needles, into the posteromedial aspect of the proximal femur. Several cadaveric, biomechanical studies have demonstrated increased rotational stability, pull-out resistance, cycles to failure with 3 and 5 ml of PMMA cement augmentation via a perforated blade in an intramedullary nail [5–7]. However, as these studies do not compare different techniques, the most biomechanically favorable location and volume of material used for augmentation has not been established.
Six of seven studies included an assessment of functional outcome; however, only three studies [10, 12, 15] utilized the same outcome variable. As a result, we were unable to pool functional outcome data between studies to generate frequency-weighted means across all studies. As a result, studies must be viewed independently. Studies that compared augmentation to a group of control patients were variable in their outcomes. One study [9] reported worse Iowa Hip Scores in the augmented group, another study [11] noted similar Harris Hip Scores between groups, and two studies [12, 13] noted improved pain and walking scores in the augmented group. As a result, it is unclear whether augmentation yields a distinct benefit in functional outcomes, and this data is difficult to interpret given the lack of data on bone mass density. It is possible that studies that demonstrated an improvement in function after augmentation had a greater number of severely osteoporotic patients in the control group; whereas, studies that demonstrated worse outcomes with augmentation had a greater number of severely osteoporotic patients in the augmentation group. Future studies should ensure case–control matching in terms of bone mineral density.
Radiographic outcomes favored the augmentation group in all studies that considered radiographic parameters. Two studies evaluated lag screw sliding distance with both demonstrating significantly less sliding in the augmented group [11, 13]. Similarly, two studies examined varus rotation and both reported significantly less rotation in the augmented group [12, 14]. Mattsson and Larsson [14] conducted the most complete radiographic assessment by press-fitting tantalum markers into predrilled holes in the proximal femur on each side of the main fracture line, for subsequent radiostereometric analysis. The three-dimensional position of each marker and the relative movement of the femoral head and neck fragment were calculated using specially designed software. Movements were recorded as translations and rotations of the center of the femoral head and rotations around three orthogonal axes. There is no established gold standard for assessment of radiographic outcome after intertrochanteric fracture fixation; however, it is clear that studies should all, at the least, include an assessment of varus rotation and lag screw sliding distance.
All studies considered complications; however, three studies [13–15] did not report any complications in their cases or controls. It is evident that these studies lack the power necessary to adequately evaluate complications. Also, given the short follow-up of the studies reviewed, complications, especially avascular necrosis from the heat generated by cement, may be underestimated and require longer-term follow-up to appropriately study. Most importantly, when pooling data from all studies that included a control group, the complication rate was significantly lower in the augmented group (5.8 %) compared to the non-augmented (control) group (22.3 %). This provides perhaps the most compelling evidence that augmentation may serve a beneficial role in the treatment of intertrochanteric femur fractures. When considering the radiographic data that demonstrates significantly decreased varus rotation and the clinical data that demonstrates a lower complications rate, with less episodes of screw cut-out and/or malunion, augmentation of intertrochanteric femur fractures should be considered a viable option when there is concern for poor bone quality and inadequate fixation to allow for early mobilization. In a recent publication, Kammerlander et al. [16] reported a standardized technique for PMMA cement augmentation of pertrochanteric femur fractures via perforations within a perforated blade. This study did not qualify for inclusion in this systematic review due to the short duration of follow-up (minimum 4 months); however, the authors reported fracture healing in all cases with no cases of cut-out, avascular necrosis, unexpected blade migration implant loosening, or implant breakage.
This study has a number of weaknesses. As is typical of any systematic review, the inherent weaknesses of each individual study (retrospective, case series, short-term follow-up, etc.) translate into limitations of this review. The methodologies of the papers reviewed did not provide controls for bias, confounding, or chance as articles were mainly descriptive in nature. As such, our study is simply an observational study of mostly observed studies but does provide an overview of the literature available. Weaknesses inherent to the member studies are not improved by aggregating them. In addition, the studies reviewed utilized different methods of outcomes evaluation and most did not present raw data for each patient included in the analysis. Furthermore, though we utilized a systematic methodology that we believe to be reproducible, it is possible that different search terms and different search engines would have provided additional studies that would have met our inclusion criteria. Surgeries were performed over a 23-year period, and so, improved techniques and technology over this time frame may have influenced the outcomes; although a post-study sensitivity analysis did not demonstrate greater complications in more historic studies. Finally, due to the limitations of the data available, we are unable to compare outcomes in patients who undergo augmentation with PMMA versus calcium–phosphate.
It is evident that fixation of the elderly intertrochanteric femur fractures is often fraught with challenges, including poor bone quality and comminution. Augmentation with PMMA or CP has been utilized to help provide structural support to the fixation construct. With an aging, more active population, these types of fractures will continue to increase in incidence and will require new and innovative means of achieving stable fixation. Though augmentation with PMMA and calcium–phosphate may be important in this regard, more stringent research methodology is necessary to determine the extent of their benefit.
References
Cummings SR, Rubin SM, Black D (1990) The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res 163–166
Koval KJ, Aharonoff GB, Rokito AS, Lyon T, Zuckerman JD (1996) Patients with femoral neck and intertrochanteric fractures. Are they the same? Clin Orthop Relat Res 166–172
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of the tip–apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 77:1058–1064
Heini PF, Franz T, Fankhauser C, Gasser B, Ganz R (2004) Femoroplasty-augmentation of mechanical properties in the osteoporotic proximal femur: a biomechanical investigation of PMMA reinforcement in cadaver bones. Clin Biomech (Bristol, Avon) 19:506–512
Erhart S, Schmoelz W, Blauth M, Lenich A (2011) Biomechanical effect of bone cement augmentation on rotational stability and pull-out strength of the Proximal Femur Nail Antirotation™. Injury 42(11):1322–1327
Sermon A, Boner V, Boger A, Schwieger K, Boonen S, Broos PL, et al (2011) Potential of polymethylmethacrylate cement-augmented helical proximal femoral nail antirotation blades to improve implant stability—a biomechanical investigation in human cadaveric Femoral Heads. J Trauma (Epub ahead of print)
Sermon A, Boner V, Schwieger K, Boger A, Boonen S, Broos P et al (2012) Biomechanical evaluation of bone-cement augmented Proximal Femoral Nail Antirotation blades in a polyurethane foam model with low density. Clin Biomech (Bristol, Avon) 27(1):71–76
Zaza SW-DAL, Briss PA (2000) Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med 18(1S):44–74
Bartucci EJ, Gonzalez MH, Cooperman DR, Freedberg HI, Barmada R, Laros GS (1985) The effect of adjunctive methylmethacrylate on failures of fixation and function in patients with intertrochanteric fractures and osteoporosis. J Bone Joint Surg Am 67:1094–1107
Chow SP, Tang SC, Pun WK et al (1987) Treatment of unstable trochanteric fractures with Dimon-Hughston osteotomy displacement fixation and acrylic cement. Injury 18:123–127
Dall’Oca C, Maluta T, Moscolo A, Lavini F, Bartolozzi P (2010) Cement augmentation of intertrochanteric fractures stabilised with intramedullary nailing. Injury 41:1150–1155
Lee PC, Hsieh PH, Chou YC, Wu CC, Chen WJ (2010) Dynamic hip screws for unstable intertrochanteric fractures in elderly patients—encouraging results with a cement augmentation technique. J Trauma 68:954–964
Mattsson P, Alberts A, Dahlberg G, Sohlman M, Hyldahl HC, Larsson S (2005) Resorbable cement for the augmentation of internally-fixed unstable trochanteric fractures. A prospective, randomised multicentre study. J Bone Joint Surg Br 87:1203–1209
Mattsson P, Larsson S (2004) Unstable trochanteric fractures augmented with calcium phosphate cement. A prospective randomized study using radiostereometry to measure fracture stability. Scand J Surg 93:223–228
Pun WK, Chow SP, Chan KC et al (1987) Treatment of unstable intertrochanteric fractures with Sarmiento valgus osteotomy and acrylic cement augmentation. Injury 18:384–389
Kammerlander C, Gebhard F, Meier C et al (2011) Standardised cement augmentation of the PFNA using a perforated blade: a new technique and preliminary clinical results. A prospective multicentre trial. Injury 42(12):1484–1490
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Namdari, S., Rabinovich, R., Scolaro, J. et al. Absorbable and non-absorbable cement augmentation in fixation of intertrochanteric femur fractures: systematic review of the literature. Arch Orthop Trauma Surg 133, 487–494 (2013). https://doi.org/10.1007/s00402-012-1677-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1677-2