Abstract
Introduction
Secondary dislocation due to loss of fixation is the most common complication after plate fixation of proximal humeral fractures. A wide range of different techniques for augmentation has been described to improve the primary and secondary stability. Nevertheless, comparative analyses on the specific advantages and limitations are missing. Therefore, the aim of the present article was to systematically review and evaluate the current biomechanical and clinical studies.
Materials and methods
The databases of PubMed and EMBASE were comprehensively searched for studies on augmentation techniques for proximal humeral fractures using defined search terms. Subsequently, all articles identified were screened for eligibility and subdivided in either clinical or biomechanical studies. Furthermore, the level of evidence and study quality were assessed according the Oxford Centre for Evidence-Based Medicine and the Coleman Methodology Score, respectively.
Results
Out of 2788, 15 biomechanical and 30 clinical studies were included. The most common techniques were structural allogenic or autologous bone grafting to enhance the medial support, metaphyseal void filling utilizing synthetic bone substitutes or bone grafts, and screw-tip augmentation with bone cement. Biomechanical data were available for structural bone grafting to enhance the medial support, void filling with synthetic bone substitutes, as well as for screw-tip augmentation. Clinical evidence ranged from level II–IV and study quality was 26–70/100 points. Only one clinical study was found investigating screw-tip augmentation. All studies included revealed that any kind of augmentation positively enhances mechanical stability, reduces the rate of secondary dislocation, and improves patients’ clinical outcome. None of the studies showed relevant augmentation-associated complication rates.
Conclusions
Augmentation of plate fixation for proximal humeral fractures seems to be a reliable and safe procedure. All common techniques mechanically increase the constructs’ stability. Clinically evaluated procedures show reduced complication rates and improved patient outcomes. Augmentation techniques seem to have the highest significance in situations of reduced bone mineral density and in high-risk fractures, such as 4-part fractures. However, more high-quality and comparative clinical trials are needed to give evidence-based treatment recommendations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures are among the most common fractures in the adult with an incidence of 304/100.000 [1]. At least 70% of all fractures occur in patients older than 65 years of age [2]. Osteoporosis-associated low-energy trauma account for the majority of injury patterns in the elderly [3,4,5]. As the population at risk continuously expands a profound understanding of the optimal treatment options for these fractures becomes more important [6].
In general, treatment options include a variety of operative and non-operative strategies, but evidence-based recommendations are missing. The majority of fractures, especially with little or no displacement, is treated non-operatively with good clinical outcome [7,8,9]. Displaced and unstable fractures are often indicated for surgery according to the Neer criteria [10]. Open reduction and internal fixation with locking plates is the most widely performed procedure allowing for high primary stability in the osteoporotic bone [11]. Long-term clinical results show excellent and good results in approximately two-thirds of the patients. Unfortunately, moderate and poor results are still reported for one-third of all patients [12]. Unsatisfactory clinical outcome is often related to a significant rate of complications and subsequent revision surgery [13, 14]. Loss of fixation leading to secondary varus displacement of the humeral head and sometimes even articular screw penetration is the most common complication [15]. To prevent these particular complications, primary arthroplasty can be considered as an alternative in complex fractures. Nevertheless, arthroplasty shows inferior clinical outcomes when compared to uneventful clinical course after anatomic reconstruction [14, 16]. Therefore, many efforts have been made to improve the constructs’ stability and to minimize the risk of locking plate failure.
In this context, the augmentation of locking plate osteosynthesis is an often reported and promising approach. An increasing number of biomechanical and clinical studies have been published. These studies evaluate a large variety of augmentation techniques in different biomechanical models and fracture situations using allografts, autografts, or synthetic bone substitutes. Most of the studies are retrospective outcome studies and the number of comparative studies is limited. An assessment and a comprehensive summary of the different techniques with regard to their specific limitations and advantages are missing. Therefore, the intent of the present study was to systematically review all available biomechanical and clinical studies investigating augmentation techniques to enhance plate fixation of proximal humeral fractures.
Materials and methods
The literature research was conducted in a sequential approach according to the principles of Evidence-Based Practice (EBP). Prior to the identification of articles, guidelines of national and international standard were discovered searching the databases of the “Guidelines International Network” (and http://www.g-i-n.net/) and National Guideline Clearinghouse (https://www.guideline.gov/). According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (http://www.prisma-statement.org), a systematic review of the literature was then conducted [17]. The databases of PubMed and EMBASE have been comprehensively searched for meta-analysis, systematic or narrative reviews, and primary clinical and biomechanical studies until January 2018 using various connections of the keywords “humer*” in combination with either “augment*”, “cement*”, “graft*”, “cancell*”, “allograft*”, or “autograft*”. Journals not published in English or German language have been excluded yielding 2788 relevant studies. Subsequent primary screening included the manuscripts title and abstract. Studies without an abstract were excluded and the full text was obtained if the abstract did not allow finding the defined inclusion and exclusion criteria. Studies investigating shaft fractures, distal humeral fractures, pathological fractures, prosthetic replacement, nerve damage, rotator cuff augmentation, or arthroscopic repair were excluded. To minimize selection bias, all reviewers independently screened each abstract and close read the gathered data of all articles. A cross-reference research was also conducted to obtain every available and relevant source and maximize accuracy. Subsequently, full-text articles were assessed for eligibility and excluded, respectively. We then subdivided the final studies in two groups containing biomechanical investigations and clinical trials. To define the quality of the studies, the Coleman Methodology Score (CMS) was utilized. It assesses the scientific quality using ten criteria, giving a total score ranging between 0 and 100 points. A score of 100 indicates that the study largely avoids chance, various biases, and confounding factors. The final score can be defined as excellent (85–100 points), good (70–84 points), fair (50–69 points), and poor (< 50 points) [18].
Results
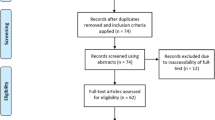
Out of 2788 studies, 15 biomechanical and 30 clinical studies have been included. 2702 studies have been excluded according to the screening process and 58 full-text articles were assessed for eligibility. Subsequently, 13 studies have been excluded after full-text analysis due to the exclusion criteria (Fig. 1). The most commonly described techniques were structural allogenic or autologous bone grafting to enhance the medial support, filling the metaphyseal void with synthetic bone substitutes or bone grafts as well as screw-tip augmentation with bone cement (Table 1).
Research protocol according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (http://www.prisma-statement.org) [17]
Biomechanical data were available for augmentation techniques enhancing the medial support by fibular strut (n = 5) or bone block grafts derived from femoral heads (n = 1) using cadaveric or synthetic bone models. Filling-the-void techniques have been described in three biomechanical studies, all using injectable calcium phosphate cements as synthetic bone substitutes. Furthermore, six studies could be identified using screw-tip augmentation with polymethyl methacrylate (PMMA) (n = 5) or strontium-containing hydroxyapatite (n = 1) (Table 2).
Nineteen clinical studies described structural bone grafting to enhance medial support. Allogenic bone grafts have been used in 15 and autologous bone grafting in four studies. Techniques for filling the metaphyseal void have been identified in 14 studies, using bone grafts, synthetic bone substitutes or metallic implants in eight, four, and two studies, respectively. One clinical study reported on 1-year clinical results after screw-tip augmentation. Clinical evidence ranged from level II–IV (LoE II: 1, LoE III: 9, LoE IV: 20 studies) according to the Oxford Centre for Evidence-Based Medicine. According to the CMS scoring system 23 studies revealed a poor, six studies a fair, and one study a good methodology (Table 3).
Biomechanical studies
Bone grafts to enhance medial support
A total of five biomechanical studies investigated on fibular strut grafts for augmenting the medial support. Mathison et al. investigated on augmented locking plates (Philos, Synthes, Switzerland) with an intramedullary fibular allograft under the stress of varus bending. Stiffness and failure load increased when using the strut graft by 3.8 and 1.7 times, respectively [19]. Osterhoff et al. used the same graft technique in single-plane abduction for unstable two-part fractures in a synthetic bone model. Fragment motion and change in gap distance were significantly less when using the strut graft [20]. Similar results were shown by Bae et al. who tested fibular allografts fixed by locking plates (Philos, Synthes, Switzerland) in axial loading for unstable three-part fractures. Displacement, stiffness and maximum load were significantly superior in augmented locking plates [21]. Chow et al. demonstrated no loss of reduction in unstable two-part fractures augmented by locking plates (LCP, Synthes, Switzerland) with an intramedullary fibula strut graft when applying varus force to the humeral shaft. No augmentation leads to an average of 75% collapse rate [22]. Lately, Hsiao et al. compared unstable two-part fractures augmented by a cortical bone allograft fixed with a locking plate (Unify, United Orthopedic Corporation, Taiwan) to no form of augmentation. The mechanical strength as measured by interfragmentary motion and maximum load to failure were doubled by the augmentation under cyclic axial loading [23]. Katthagen et al. compared non-augmented locking plates (Philos, Synthes, Switzerland) in osteoporotic specimens with and without calcar screws vs. an additional augmentation of the medial fracture gap with corticocancellous bone block grafts derived from femoral heads. The mechanical effect of additional calcar screws was non-significant when compared to no calcar screws, whereas bone block augmentation significantly increased the construct’s stiffness and failure load [24].
Filling the void
Kwon et al. compared K-wire fixation vs. cloverleaf plates vs. blade plates each augmented with calcium phosphate cement or non-augmented in unstable three-part fractures. All augmented implants showed superior results regarding interfragmentary motion and maximum load with the exception in abduction when using K-wires. The addition of calcium phosphate cement increased the stiffness of even the most osteoporotic specimens to levels that were higher than those of the most osteodense specimens that had been treated with internal fixation alone [25]. Gradl et al. tested calcium phosphate augmented locking plates (AxSOS; Stryker Trauma, Switzerland) in unstable two-part fractures under axial loading. They found higher values for stiffness and a maximum load to failure [26]. As much as 20% volume of the humeral head was replaced with calcium triphosphate by Kennedy et al. who then investigated locking plates (Arthrex Suture Plate, Arthrex, USA) in unstable three-part fractures under axial loading. With the void augmented, the mean difference in failure load changed to 300 N and interfragmentary motion was 1 mm and 6.4 mm for the augmented and non-augmented groups, respectively [27].
Screw-tip augmentation
Unger et al. tested PMMA (Traumacem V+, Synthes, Switzerland) augmented locking screws in unstable three-part fractures. The augmentation led to significantly increased cycles to failure in varus bending and axial rotation [28]. Röderer et al. presented similar results after augmenting only two locking screws aiming at the lowest bone mineral density. PMMA-augmented implants showed superior cycles to failure when compared to no augmentation [29]. The difference of screw-tip augmentation (Philos/PMMA, Synthes, Switzerland) in stable and unstable fracture models was investigated by Kathrein et al. For stable fractures, no significant difference between augmented and non-augmented implants could be found. Regarding the unstable fracture situation, augmented implants showed significantly lower values for varus dislocation per cycle motion and in total [30]. Scola et al. tested PMMA-augmented locking plates (Philos, Synthes, Switzerland) in unstable three-part fractures and found significantly delayed varus collapse and higher maximum load in the augmented group [31]. One recent biomechanical studies derived from Schliemann et al. Screw-tip augmentation of the anterior directed head screws (DiPhos-H plate, Lima Corporate, Udine, Italy /PMMA, Synthes, Switzerland) under varus bending in unstable three-part fractures showed less motion at the bone-implant interface with no difference in stiffness and mean load to failure [32]. Kuang et al. utilized strontium-containing hydroxyapatite (Sr-HA) bone cement instead of PMMA for screw augmentation in an osteoporotic three-part fracture model. In comparison to non augmented locking plates (Philos, Synthes, Switzerland) Sr-HA cement-augmented fracture fixation showed a better biomechanical performance in varus bending tests revealing significantly less displacement, higher failure points, and higher stiffness. However, no significant differences were found between augmented and non-augmented specimens in axial rotational tests [33].
Clinical studies
Bone grafts to enhance medial support
Walch et al. reported on 20 proximal humeral nonunions after failed conservative and operative therapy treated with an intramedullary bone peg augmented t plate. Autografts were obtained from the iliac crest, anterior tibial crest, or fibula shaft. After a mean follow-up of 42 months, findings included a union rate of 96% with an overall age- and sex-adjusted Constant score of 81. Three pathologic tibial fractures occurred as procedure-related complications [34]. Ring et al. found similar results after treating 25 proximal humeral nonunions with an iliac crest-augmented blade plate. The mean Constant Score was 77 after a mean follow-up of 41 months. Complications included two persisting nonunited fractures and one fracture of the iliac wing near the bone harvesting site [35]. Zhu et al. compared four-part fractures treated by iliac crest-augmented locking plates to no form of augmentation. Using the intramedullary graft led to superior results in regard to patient satisfaction measured by a mean SF-36 of 88 and 69.5, respectively. The iliac crest autografts used in comminuted four-part fractures resulted in bony union in all cases, whereas two nonunion were found with no augmentation [36]. In 2012, Gao et al. investigated seven surgical neck nonunions treated with autologous fibular grafts fixed with a locking plate. After a mean of 6.1 months, all fractures showed radiographic signs of bony union and at final follow-up patients presented with an overall Constant score of 77.7 and a 0.57 on the VAS Scale. Major complications according to the procedure were one transient peroneal nerve palsy in the donor leg and one transient radial nerve palsy [37].
Gardner et al. treated proximal humeral fractures with unstable medial column comminution using locking plates (PHP, Synthes, Switzerland) with fibular allografts as indirect medial support. All fractures healed without loss of reduction and all patients were followed to bony union [38]. Badman et al. used fibular and ulnar allografts fixed by locking or bent plates for the treatment of proximal humeral nonunion. Bony consolidation was achieved in 94% with minimal residual pain and improved functional results with an ASES score of 81 postoperatively [39]. Rollo et al. also investigated proximal humeral nonunion treated by an extramedullary humeral shaft allograft fixed by a locking plate (PHILOS, Synthes, Switzerland). No complication was noted after a mean of 63 months of follow-up and union was achieved in all the cases [40]. Neviaser et al. used locking plates (Philos, Synthes, Switzerland) and fibular allografts on 38 Patients with two-, three-, and four-part proximal humerus fractures. One loss of reduction and one partial osteonecrosis occurred with overall excellent clinical results and high subjective patient satisfaction as measured by Constant and DASH scores of 87 and 15, respectively [41]. Similar clinical results were shown by Matassi et al. who prospectively investigated three- and four-part proximal humeral fractures with metaphyseal comminution after the reduction with a fibular allograft-augmented locking plate (Philos, Synthes, Switzerland; PERI-LOC, Smith & Nephew, USA). No major complication was detected, and the mean Constant and DASH scores were 79 and 33, respectively [42]. Semitubular plates and fresh-frozen fibular allografts were used as endosteal implants by Hettrich et al. to prevent varus collapse and maintain the intraoperative head-shaft angle fixed by a locking plate. The authors reported on only one loss of reduction with an average of 2° change in head-shaft angle [43]. Little et al. reported about 72 patients after fracture reduction of displaced and unstable two-, three- and four-part proximal humeral fractures with a fibular allograft and locking plates (PHP, Synthes, Switzerland). The mean Constant Score was 89 and 85 for valgus and varus deformities, respectively. DASH and SF-36 scores did not differ between the two subgroups. One osteonecrosis was present at latest follow-up in the valgus group [44]. Tan et al. approached displaced and unstable proximal humeral fractures with an intramedullary fibular strut graft reduced by a locking plate. On radiographs after 12 weeks, all fractures showed signs of callus formation with a retained head-shaft angle. The range of motion was satisfactory allowing all patients for overhead activities [45]. To detect the influence of age related comorbidities of the aging population on structural augmented proximal humeral fractures, Hinds et al. compared geriatric to non-geriatric patients suffering from 2-, 3- and 4-part fractures. Fibular strut graft augmented locking plates were used during fracture reduction. At a mean follow-up of 34 months, geriatric patients showed a mean Constant and DASH score of 82.7 and 16.4, respectively. Clinical results of non-geriatric patients did not differ significantly from the results of younger individuals. One geriatric patient developed an osteonecrosis with secondary screw cut-out [46]. Displaced 2-, 3-, and 4-part proximal humeral fractures with medial comminution were also treated with locking plating reinforced by fibular strut grafts by Pancha et al.. At latest follow-up ASES and UCLA-scores were 80.4 and 28.8, respectively. Varus collapse, osteonecrosis, and breakage of the drill bit were noted in two patients [47]. To investigate whether graft shape has an influence on the functional outcome when treating 4-part proximal humerus fractures with augmented locking plates (PHILOS, Synthes, Switzerland), Chen et al. compared anatomic-to-non-anatomic allografts to enhance the medial support. Anatomic allografts formed from frozen cadaveric donors to additionally fill the metaphyseal void resulted in a mean Constant and DASH score of 75.4 and 9.3, respectively, and did not differ significantly when compared to a fibular strut graft [48]. A case–control study was performed by Cha et al. who compared 2-, 3-, and 4-part fractures fixed by locking plates (PHILOS, Synthes, Switzerland) to locking plates augmented by fresh-frozen allografts. Augmentation showed significant fewer complications and helped to maintain the neck-shaft angle and the humeral head height [49]. Similar results have been reported by Chen et al. analyzing the effect of fibular allograft augmentation in 3- and 4-part fractures. In comparison to a retrospective, historic cohort of non-augmented locking plate fixation (PHILOS, Synthes, Switzerland), patients treated with fibular allograft augmentation showed significantly better functional and subjective outcome values as well as a significantly lower complication rate compared to patients treated with locking plate alone [50]. Kim et al. recently confirmed these findings in a cohort of elderly patients suffering from 3- and 4-part fractures with medial comminution. The authors compared fibular allograft augmentation of locking plate fixation with non-augmented locking plate fixation featuring additional inferomedial screws. In 4-part fractures patients treated with fibular allografts had significantly superior clinical and radiological results compared to the patients treated with inferomedial screws only. However, this effect was not observed in 3-part fractures [51]. Chen et al. compared locking plating augmented by fresh-frozen fibula strut grafts to hemiarthroplasty (Link, Germany) in a prospective randomized study. Superior clinical results with a better range of motion for the osteosynthetic reconstruction with a mean Constant score of 80.1 and 75.4 were found, respectively. Complications included one case of avascular necrosis, one case of varus displacement, and one patient with screw perforation of the articular surface [52].
Filling the void
Euler et al. focused their investigation on high-risk and severely displaced varus 2-part fractures using a cancellous allograft from a frozen femoral head fixed with a locking plate (Philos, Synthes, Switzerland). After a mean follow-up of more than 2 years, the Constant score was 72 and pain decreased to an average of 1 on the VAS scale. Despite one deep infection leading to conversion to a reversed shoulder prosthesis, no major complication was noted. Bony union was achieved in 90% with further follow-up [53, 54]. Fractures with valgus deformities were investigated by Atalar et al. who used an iliac crest allograft for structural augmentation of impacted 4-part fractures fixed with locking plate (Philos, Synthes, Switzerland). All fractures healed with good functional results as measured by a Constant and DASH score of 87.7 and 7.6, respectively. Single postoperative complication was one case of early articular screw penetration [55]. Checchia et al. discovered high satisfaction rates and good fracture consolidation for the treatment of proximal humeral nonunion resulting from 2-part and minimal displaced 3-part fractures treated with a blade plate augmented by autologous cancellous chips and an iliac crest graft. Mean elevation, and lateral and medial rotation were 130°, 42°, and hand position at T10, respectively [56]. The treatment of displaced 4-part fractures using an iliac crest autograft-augmented locking plate is used by Kim et al. and resulted in good functional results with a Neer score of 92. At final follow-up, all fractures healed radiographically and imaging yielded a mean head-shaft angle of 129°. No complication was noted [57]. Robinson et al. investigated 25 consecutive patients with 3- and 4-part valgus impacted fractures who were treated with calcium phosphate cement (SRS, Norian, USA) to fill a metaphyseal defect. Fracture reduction was maintained by either a buttress plate or position screws only. After 12 months of follow-up, the mean Constant and Dash scores were 80 and 22, respectively. No major complication was detected [58]. A similar technique was used by Lee et al. who used calcium sulfate injections and locking plates (Philos, Synthes, Switzerland) to reinforce medial cortex stabilization in 14 patients with 2-, 3-, and 4-part proximal humerus factures. With overall satisfactory clinical results patients receiving augmentation showed significant higher UCLA scores of 30.2 and 28.9, respectively. The reduction failure rate was not influenced by additional augmentation [59]. Calcium sulfate injections were also used by Somasundaram et al. who treated 2-, 3-, and 4-part fractures with locking plates (Philos, Synthes, Switzerland). Final Constant and DASH scores were 64 and 16.2, respectively. No complications were noted and reduction was maintained in every case [60]. A case–control study was used by Egol et al. to compare the reduction with locking plates (Philos, Synthes, Switzerland) augmented by either cancellous chips, calcium phosphate injections, or no type of augmentation when treating 2-, 3- and 4-part proximal humerus fractures. Postoperative radiographs showed significantly less loss of reduction and fracture settling when using calcium phosphate cement augmentation compared to cancellous bone chips or no augmentation (p = 0.02) [61]. A recent complex retrospective study was performed by Russo et al. The authors compared K-wires or osteosutures and/or thin and elastic non-locked or locked plates augmented by an iliac crest or cancellous bone shaped as triangular trapezoidal block to a titanium triangular-shaped implant (Da Vinci, Arthrex, USA). Results according to Constant and DASH scores were 83.2% good and excellent, 12.8% fair, and 4% bad [62].
Screw-tip augmentation
Only one clinical study evaluated the technique of screw-tip augmentation following locking plate fixation (PHILOS, Synthes, Switzerland) in a small cohort of 24 patients with 2-, 3-, and 4-part fractures and a follow-up of 1 year. When compared to a historic control group of locking plate fixation without augmentation, an additional PMMA screw-tip augmentation showed similar clinical outcomes, but reduced the rate of early implant-related complications, such as early loss of reduction and articular screw perforation [63].
Discussion
The intent of this overview was to systematically review all available biomechanical and clinical studies investigating augmentation techniques of plate fixation for proximal humeral fractures. The different augmentation techniques were then categorized according to their operative principles, the Levels of Evidence were assessed and the studies’ quality was evaluated. The most commonly described techniques were structural allogenic or autologous bone grafting to enhance the medial support, filling the metaphyseal void with synthetic bone substitutes or bone grafts as well as screw-tip augmentation with bone cement. Although the evidence is limited and prospective or randomized clinical trials are still missing for any of the techniques described, all of the strategies appear to have a positive effect on primary and secondary stability after open reduction and plate fixation of proximal humerus fractures.
Five studies investigating fibular strut graft as enhancement of the medial support revealed biomechanically increased varus bending load, stiffness, and load to failure as well as reduced rate of loss of fixation and interfragmentary movement [19,20,21,22,23]. Since none of these biomechanical studies utilized a four-part fracture model, these findings may only be transferred to a clinical scenario of unstable two- or three-part fractures. Furthermore, all biomechanical studies utilized servohydraulic testing machine without simulating rotator cuff muscle forces. Taken together, the biomechanical models represent only a time-zero situation and do not adequately reflect the clinical reality.
Nevertheless, 19 clinical studies using structural bone grafting to enhance the medial support could be identified. The major findings within these studies were higher rates of fracture healing, superior clinical outcome scores, and higher patient satisfaction as well as reduced loss of fixation and varus malunion. While the vast majority of studies utilized fibular allografts [38, 39, 41,42,43,44,45,46,47,48,49,50,51,52], autologous and allogenic bone grafts derived from the iliac crest seem to allow for likewise promising results [34, 36]. One comparative study was conducted by Chen et al., revealing good clinical and radiological outcomes for elderly patients with four-part fractures without significant differences between anatomical precontoured vs. non-contoured fibula strut allograft [48]. A total of three comparative study on fibular allograft augmentation in 2- to 4-part fractures found significantly better functional outcome, higher subjective patient satisfaction, and reduced loss of fixation after fibular strut graft augmentation of comminuted fractures compared to non-augmented fractures [49,50,51]. Kim et al. pointed out that augmentation of 4-part fractures with medial comminution in the elderly had the strongest effect on improving outcome and minimizing complications. Interestingly, the use of allografts to enhance the medial support is equally effective in geriatric patients compared to non-geriatric patients [46]. Furthermore, the joint preserving procedure with locking plate fixation with allogenic strut graft fixation showed significantly superior clinical outcomes when prospectively compared to hemiarthroplasty [52]. Taking the current data and the low level of evidence into account, availability, donor site morbidity, patient’s or surgeon’s preferences have a significant impact on the graft choice in clinical practice.
The concept of filling the void was investigated in three biomechanical studies, which all utilized injectable synthetic bone substitutes [25,26,27]. Across the studies, significantly decreased fracture-gap deflection and interfragmentary motion as well as increased axial stiffness and maximum load to failure was observed due to the augmentation. Again, these biomechanical approaches only assess the primary stability. The clinical degradation and remodeling processes of injectable bone grafts and their influence on the constructs stability in the course of time were evaluated in four clinical studies. Three of these studies were case series without a non-augmented control group. In contrast to the biomechanical studies, they also included more complex fracture pattern, such as four-part fractures. In summary, good clinical outcome values, low rates of loss of reduction and screw perforation were described. The studies neither assessed specific complication due to the injected bone fillers, nor the resorption and remodeling processes. One study retrospectively compared void filling techniques using either calcium phosphate or cancellous bone chips. The authors revealed less loss of fixation and significantly less glenohumeral screw cut-out with calcium phosphate cement compared with no augmentation or with cancellous bone chips [61].
A total of eight studies investigated the significance of allogenic and autologous bone grafts for filling the metaphyseal void [48, 53,54,55,56,57, 61, 62]. Beside the above-mentioned study by Egol et al., all remaining studies are case series reporting good clinical outcomes and stating void filling with bone grafts as a safe-and-reliable procedure. In addition to bone grafting of the metaphyseal void, two studies introduced metallic implants as a potential alternative resulting in similar outcomes and complication rates [43, 62]. Nevertheless, these techniques are currently deemed to be of inferior significance in clinical practice.
The basic principle of screw-tip augmentation with injectable PMMA is to increase the primary stability by enhancing the screw-tip/bone interface. Another advantage of this technique is that it does not substantially change the operative standard procedure of open reduction and internal plate fixation. A total of five biomechanical studies demonstrated that screw-tip augmentation significantly decreases motion between the bone–implant interface and counteracts the varus collapse [28,29,30,31,32]. The most striking effects were detected in specimens with low bone mineral density and unstable fracture patterns, like unstable two-part fractures. On the other hand, comparative analyses in stable fracture patterns and healthy bone specimens did not reveal advantages of screw-tip augmentation. Although this technique has already been widely implemented in clinical practice, there is only one study providing clinical data of a small patient cohort with 12 month follow-up [63]. Especially, the clinical impact of potential adverse events like glenohumeral PMMA leakage, avascular necrosis, or cartilage damage due to exothermic reaction is not fully overseen.
Conclusion
Augmentation of plate fixation for proximal humeral fractures seems to be a reliable and safe procedure. All common techniques mechanically increase the constructs’ stability. Clinically evaluated procedures show reduced complication rates and improved patient outcomes. Augmentation techniques seem to have the highest significance in situations of reduced bone mineral density and in high-risk fractures, such as 4-part fractures, fractures with medial comminution, and severe valgus and varus displacement. However, more high-quality and comparative clinical trials are needed to give evidence-based treatment recommendations.
References
Kannus P, Palvanen M, Niemi S, Sievanen H, Parkkari J (2009) Rate of proximal humeral fractures in older Finnish women between 1970 and 2007. Bone 44(4):656–659. https://doi.org/10.1016/j.bone.2008.12.007
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697. https://doi.org/10.1016/j.injury.2006.04.130
Kralinger F, Blauth M, Goldhahn J, Kach K, Voigt C, Platz A, Hanson B (2014) The influence of local bone density on the outcome of one hundred and fifty proximal humeral fractures treated with a locking plate. J Bone Joint Surg Am 96(12):1026–1032. https://doi.org/10.2106/JBJS.M.00028
Maier D, Jaeger M, Izadpanah K, Strohm PC, Suedkamp NP (2014) Proximal humeral fracture treatment in adults. J Bone Joint Surg Am 96(3):251–261. https://doi.org/10.2106/JBJS.L.01293
Haasters F, Prall WC, Himmler M, Polzer H, Schieker M, Mutschler W (2015) Prevalence and management of osteoporosis in trauma surgery. Implementation of national guidelines during inpatient fracture treatment. Unfallchirurg 118(2):138–145. https://doi.org/10.1007/s00113-013-2500-4
Palvanen M, Kannus P, Niemi S, Parkkari J (2006) Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 442:87–92
Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J (2011) Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 20(7):1025–1033. https://doi.org/10.1016/j.jse.2011.04.016
Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin BC, Goodchild L, Chuang LH, Hewitt C, Torgerson D, Collaborators PT (2015) Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA 313(10):1037–1047. https://doi.org/10.1001/jama.2015.1629
Handoll HH, Brorson S (2015) Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000434.pub4
Lill H, Bewer A, Korner J, Verheyden P, Hepp P, Krautheim I, Josten C (2001) Conservative treatment of dislocated proximal humeral fractures. Zentralbl Chir 126(3):205–210. https://doi.org/10.1055/s-2001-12495
Tepass A, Blumenstock G, Weise K, Rolauffs B, Bahrs C (2013) Current strategies for the treatment of proximal humeral fractures: an analysis of a survey carried out at 348 hospitals in Germany, Austria, and Switzerland. J Shoulder Elbow Surg 22(1):e8–e14. https://doi.org/10.1016/j.jse.2012.04.002
Ockert B, Siebenburger G, Kettler M, Braunstein V, Mutschler W (2014) Long-term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 23(8):1223–1231. https://doi.org/10.1016/j.jse.2013.11.009
Jost B, Spross C, Grehn H, Gerber C (2013) Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg 22(4):542–549. https://doi.org/10.1016/j.jse.2012.06.008
Haasters F, Siebenburger G, Helfen T, Daferner M, Bocker W, Ockert B (2016) Complications of locked plating for proximal humeral fractures-are we getting any better? J Shoulder Elbow Surg 25(10):e295–e303. https://doi.org/10.1016/j.jse.2016.02.015
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42(4):408–413. https://doi.org/10.1016/j.injury.2010.11.058
Ockert B, Biermann N, Haasters F, Mutschler W, Braunstein V (2013) Reverse shoulder arthroplasty for primary fracture treatment. Displaced three and four part fractures of the proximal humerus in the elderly patient. Unfallchirurg 116(8):684–690. https://doi.org/10.1007/s00113-013-2410-5
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10(1):2–11
Mathison C, Chaudhary R, Beaupre L, Reynolds M, Adeeb S, Bouliane M (2010) Biomechanical analysis of proximal humeral fixation using locking plate fixation with an intramedullary fibular allograft. Clin Biomech (Bristol Avon) 25(7):642–646. https://doi.org/10.1016/j.clinbiomech.2010.04.006
Osterhoff G, Baumgartner D, Favre P, Wanner GA, Gerber H, Simmen HP, Werner CM (2011) Medial support by fibula bone graft in angular stable plate fixation of proximal humeral fractures: an in vitro study with synthetic bone. J Shoulder Elbow Surg 20(5):740–746. https://doi.org/10.1016/j.jse.2010.10.040
Bae JH, Oh JK, Chon CS, Oh CW, Hwang JH, Yoon YC (2011) The biomechanical performance of locking plate fixation with intramedullary fibular strut graft augmentation in the treatment of unstable fractures of the proximal humerus. J Bone Jt Surg Br 93(7):937–941. https://doi.org/10.1302/0301-620X.93B7.26125
Chow RM, Begum F, Beaupre LA, Carey JP, Adeeb S, Bouliane MJ (2012) Proximal humeral fracture fixation: locking plate construct +/- intramedullary fibular allograft. J Shoulder Elbow Surg 21(7):894–901. https://doi.org/10.1016/j.jse.2011.04.015
Hsiao CK, Tsai YJ, Yen CY, Lee CH, Yang TY, Tu YK (2017) Intramedullary cortical bone strut improves the cyclic stability of osteoporotic proximal humeral fractures. BMC Musculoskelet Disord 18(1):64. https://doi.org/10.1186/s12891-017-1421-8
Katthagen JC, Schwarze M, Meyer-Kobbe J, Voigt C, Hurschler C, Lill H (2014) Biomechanical effects of calcar screws and bone block augmentation on medial support in locked plating of proximal humeral fractures. Clin Biomech (Bristol Avon) 29(7):735–741. https://doi.org/10.1016/j.clinbiomech.2014.06.008
Kwon BK, Goertzen DJ, O’Brien PJ, Broekhuyse HM, Oxland TR (2002) Biomechanical evaluation of proximal humeral fracture fixation supplemented with calcium phosphate cement. J Bone Jt Surg Am 84-A(6):951–961
Gradl G, Knobe M, Stoffel M, Prescher A, Dirrichs T, Pape HC (2013) Biomechanical evaluation of locking plate fixation of proximal humeral fractures augmented with calcium phosphate cement. J Orthop Trauma 27(7):399–404. https://doi.org/10.1097/BOT.0b013e318278c595
Kennedy J, Molony D, Burke NG, FitzPatrick D, Mullett H (2013) Effect of calcium triphosphate cement on proximal humeral fracture osteosynthesis: a cadaveric biomechanical study. J Orthop Surg (Hong Kong) 21(2):173–177
Unger S, Erhart S, Kralinger F, Blauth M, Schmoelz W (2012) The effect of in situ augmentation on implant anchorage in proximal humeral head fractures. Injury 43(10):1759–1763. https://doi.org/10.1016/j.injury.2012.07.003
Röderer G, Scola A, Schmolz W, Gebhard F, Windolf M, Hofmann-Fliri L (2013) Biomechanical in vitro assessment of screw augmentation in locked plating of proximal humerus fractures. Injury 44(10):1327–1332. https://doi.org/10.1016/j.injury.2013.05.008
Kathrein S, Kralinger F, Blauth M, Schmoelz W (2013) Biomechanical comparison of an angular stable plate with augmented and non-augmented screws in a newly developed shoulder test bench. Clin Biomech (Bristol Avon) 28(3):273–277. https://doi.org/10.1016/j.clinbiomech.2012.12.013
Scola A, Gebhard F, Roderer G (2015) Augmentation technique on the proximal humerus. Unfallchirurg 118(9):749–754. https://doi.org/10.1007/s00113-015-0061-4
Schliemann B, Seifert R, Rosslenbroich SB, Theisen C, Wahnert D, Raschke MJ, Weimann A (2015) Screw augmentation reduces motion at the bone-implant interface: a biomechanical study of locking plate fixation of proximal humeral fractures. J Shoulder Elbow Surg 24(12):1968–1973. https://doi.org/10.1016/j.jse.2015.06.028
Kuang GM, Wong TM, Wu J, Ouyang J, Guo H, Zhou Y, Fang C, Leung FKL, Lu W (2018) Augmentation of a locking plate system using bioactive bone cement-experiment in a proximal humeral fracture model. Geriatr Orthop Surg Rehabil 9:2151459318795312. https://doi.org/10.1177/2151459318795312
Walch G, Badet R, Nove-Josserand L, Levigne C (1996) Nonunions of the surgical neck of the humerus: surgical treatment with an intramedullary bone peg, internal fixation, and cancellous bone grafting. J Shoulder Elbow Surg 5(3):161–168
Ring D, McKee MD, Perey BH, Jupiter JB (2001) The use of a blade plate and autogenous cancellous bone graft in the treatment of ununited fractures of the proximal humerus. J Shoulder Elbow Surg 10(6):501–507. https://doi.org/10.1067/mse.2001.118414
Zhu L, Liu Y, Yang Z, Li H, Wang J, Zhao C, Chen X, Zhang Y (2014) Locking plate fixation combined with iliac crest bone autologous graft for proximal humerus comminuted fracture. Chin Med J (Engl) 127(9):1672–1676
Gao K, Gao W, Huang J, Wu X, Wang CS, Wang Q (2012) Treatment of surgical neck nonunions of the humerus with locked plate and autologous fibular strut graft. Med Princ Pract 21(5):483–487. https://doi.org/10.1159/000337438
Gardner MJ, Boraiah S, Helfet DL, Lorich DG (2008) Indirect medial reduction and strut support of proximal humerus fractures using an endosteal implant. J Orthop Trauma 22(3):195–200. https://doi.org/10.1097/BOT.0b013e31815b3922
Badman BL, Mighell M, Kalandiak SP, Prasarn M (2009) Proximal humeral nonunions treated with fixed-angle locked plating and an intramedullary strut allograft. J Orthop Trauma 23(3):173–179. https://doi.org/10.1097/BOT.0b013e31819b0bdc
Rollo G, Rotini R, Pichierri P, Giaracuni M, Stasi A, Macchiarola L, Bisaccia M, Meccariello L (2017) Grafting and fixation of proximal humeral aseptic non union: a prospective case series. Clin Cases Miner Bone Metab 14(3):298–304. https://doi.org/10.11138/ccmbm/2017.14.3.298
Neviaser AS, Hettrich CM, Beamer BS, Dines JS, Lorich DG (2011) Endosteal strut augment reduces complications associated with proximal humeral locking plates. Clin Orthop Relat Res 469(12):3300–3306. https://doi.org/10.1007/s11999-011-1949-0
Matassi F, Angeloni R, Carulli C, Civinini R, Di Bella L, Redl B, Innocenti M (2012) Locking plate and fibular allograft augmentation in unstable fractures of proximal humerus. Injury 43(11):1939–1942. https://doi.org/10.1016/j.injury.2012.08.004
Hettrich CM, Neviaser A, Beamer BS, Paul O, Helfet DL, Lorich DG (2012) Locked plating of the proximal humerus using an endosteal implant. J Orthop Trauma 26(4):212–215. https://doi.org/10.1097/BOT.0b013e318243909c
Little MT, Berkes MB, Schottel PC, Lazaro LE, LaMont LE, Pardee NC, Nguyen JT, Helfet DL, Lorich DG (2014) The impact of preoperative coronal plane deformity on proximal humerus fixation with endosteal augmentation. J Orthop Trauma 28(6):338–347. https://doi.org/10.1097/BOT.0000000000000012
Tan E, Lie D, Wong MK (2014) Early outcomes of proximal humerus fracture fixation with locking plate and intramedullary fibular strut graft. Orthopedics 37(9):e822–e827. https://doi.org/10.3928/01477447-20140825-60
Hinds RM, Garner MR, Tran WH, Lazaro LE, Dines JS, Lorich DG (2015) Geriatric proximal humeral fracture patients show similar clinical outcomes to non-geriatric patients after osteosynthesis with endosteal fibular strut allograft augmentation. J Shoulder Elbow Surg 24(6):889–896. https://doi.org/10.1016/j.jse.2014.10.019
Panchal K, Jeong JJ, Park SE, Kim WY, Min HK, Kim JY, Ji JH (2016) Clinical and radiological outcomes of unstable proximal humeral fractures treated with a locking plate and fibular strut allograft. Int Orthop 40(3):569–577. https://doi.org/10.1007/s00264-015-2950-0
Chen H, Ji X, Zhang Q, Liang X, Tang P (2015) Clinical outcomes of allograft with locking compression plates for elderly four-part proximal humerus fractures. J Orthop Surg Res 10:114. https://doi.org/10.1186/s13018-015-0258-9
Cha H, Park KB, Oh S, Jeong J (2017) Treatment of comminuted proximal humeral fractures using locking plate with strut allograft. J Shoulder Elbow Surg 26(5):781–785. https://doi.org/10.1016/j.jse.2016.09.055
Chen H, Yin P, Wang S, Li J, Zhang L, Khan K, Zhang L, Tang P (2018) The Augment of the Stability in Locking Compression Plate with Intramedullary Fibular Allograft for Proximal Humerus Fractures in Elderly People. Biomed Res Int. https://doi.org/10.1155/2018/3130625
Kim DS, Lee DH, Chun YM, Shin SJ (2018) Which additional augmented fixation procedure decreases surgical failure after proximal humeral fracture with medial comminution: fibular allograft or inferomedial screws? J Shoulder Elbow Surg 27(10):1852–1858. https://doi.org/10.1016/j.jse.2018.03.020
Chen H, Ji X, Gao Y, Zhang L, Zhang Q, Liang X, Tang P (2016) Comparison of intramedullary fibular allograft with locking compression plate versus shoulder hemi-arthroplasty for repair of osteoporotic four-part proximal humerus fracture: Consecutive, prospective, controlled, and comparative study. Orthop Traumatol Surg Res 102(3):287–292. https://doi.org/10.1016/j.otsr.2015.12.021
Euler SA, Hengg C, Wambacher M, Spiegl UJ, Kralinger F (2015) Allogenic bone grafting for augmentation in two-part proximal humeral fracture fixation in a high-risk patient population. Arch Orthop Trauma Surg 135(1):79–87. https://doi.org/10.1007/s00402-014-2128-z
Euler SA, Kralinger FS, Hengg C, Wambacher M, Blauth M (2016) Allograft augmentation in proximal humerus fractures. Oper Orthop Traumatol 28(3):153–163. https://doi.org/10.1007/s00064-016-0446-8
Atalar AC, Eren I, Uludag S, Demirhan M (2014) Results of surgical management of valgus-impacted proximal humerus fractures with structural allografts. Acta Orthop Traumatol Turc 48(5):546–552. https://doi.org/10.3944/AOTT.2014.14.0115
Checchia SL, Miyazaki AN, Fregoneze M, Santos PD, da Silva LA, Nascimento LG (2009) Pseudarthrosis of the humeral neck: analysis of the results when using the technique described by walch Et Al. Rev Bras Ortop 44(3):239–246. https://doi.org/10.1016/S2255-4971(15)30074-4
Kim SH, Lee YH, Chung SW, Shin SH, Jang WY, Gong HS, Baek GH (2012) Outcomes for four-part proximal humerus fractures treated with a locking compression plate and an autologous iliac bone impaction graft. Injury 43(10):1724–1731. https://doi.org/10.1016/j.injury.2012.06.029
Robinson CM, Page RS (2003) Severely impacted valgus proximal humeral fractures. Results of operative treatment. J Bone Jt Surg Am 85-A(9):1647–1655
Lee CW, Shin SJ (2009) Prognostic factors for unstable proximal humeral fractures treated with locking-plate fixation. J Shoulder Elbow Surg 18(1):83–88. https://doi.org/10.1016/j.jse.2008.06.014
Somasundaram K, Huber CP, Babu V, Zadeh H (2013) Proximal humeral fractures: the role of calcium sulphate augmentation and extended deltoid splitting approach in internal fixation using locking plates. Injury 44(4):481–487. https://doi.org/10.1016/j.injury.2012.10.030
Egol KA, Sugi MT, Ong CC, Montero N, Davidovitch R, Zuckerman JD (2012) Fracture site augmentation with calcium phosphate cement reduces screw penetration after open reduction-internal fixation of proximal humeral fractures. J Shoulder Elbow Surg 21(6):741–748. https://doi.org/10.1016/j.jse.2011.09.017
Russo R, D’Auria D, Ciccarelli M, Della Rotonda G, D’Elia G, Siciliano B (2017) Triangular block bridge method for surgical treatment of complex proximal humeral fractures: theoretical concept, surgical technique and clinical results. Injury 48(Suppl 3):S12–S19. https://doi.org/10.1016/S0020-1383(17)30651-4
Katthagen JC, Lutz O, Voigt C, Lill H, Ellwein A (2018) Cement augmentation of humeral head screws reduces early implant-related complications after locked plating of proximal humeral fractures. Obere Extrem 13(2):123–129. https://doi.org/10.1007/s11678-018-0440-x
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biermann, N., Prall, W.C., Böcker, W. et al. Augmentation of plate osteosynthesis for proximal humeral fractures: a systematic review of current biomechanical and clinical studies. Arch Orthop Trauma Surg 139, 1075–1099 (2019). https://doi.org/10.1007/s00402-019-03162-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03162-2