Abstract
Background
Vascularized fibular grafting (VFG) has been initiated to treat avascular necrosis of the femoral head (ANFH) since the late 1970s. There are a number of review articles updating the use of VFG to treat the ANFH. None of them applied statistical analysis for combining results from different studies to obtain a quantitative estimate of the overall effect and potential harm of VFG in comparison to other treatment.
Methods
Several electronic databases were searched to find studies using VFG to treat ANFH. The outcomes sought included Harris Score, failure rate (conversion to total hip arthroplasty (THA) and/or femoral head collapse), and complications rate. Included studies were assessed for methodological bias and estimates of effect were calculated. Potential reasons for heterogeneity were explored.
Results
The clinical results of 69.0 % of VFG-treated patients and 25.0 % of non-VFG-treated patients were good to excellent (OR 0.13; p < 0.01). The conversion rate to THA of VFG-treated and that of other methods treated hips was 16.5 % and 42.6 % (OR 0.19; p < 0.001). Collapse rate of VFG-treated and that of non-VFG-treated hips was 16.7 % and 63.6 % (OR 0.09; p < 0.05). The complication rate of VFG-treated and that of other methods treated patients was 23.8 % and 8.9 % (OR 3.44; p = 0.09). For Steinberg stage I, II ANFH, failure rate of VFG-treated and that of non-VFG-treated hips was 9.8 % and 40.2 % (OR 0.17; p < 0.001). For Steinberg stage II, III ANFH, failure rate of VFG-treated and that of non-VFG-treated hips was 16.5 % and 42.8 %, respectively (OR 0.17; p < 0.001).
Conclusions
VFG is a justified method that can prevent the ANFH from progressing to collapse, and that can retard or avoid hip replacement, especially in the hips of Steinberg stage I, II, and III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Avascular necrosis of the femoral head (ANFH) is a debilitating disease that usually leads to destruction of the hip joint in patients who are in the third, fourth, or fifth decades of life. It has been estimated to 10,000–20,000 new patients a year in United States [1–4]. Clinicians concur that ideal treatment should focus on pain relief, preservation or restoration of the integrity of the femoral head, and ultimately prevention of deterioration of the hip [5]. Several treatment methods and procedures have been proposed to arrest this disease; these strategies include core decompression [6–9], electrical stimulation [10, 11], transtrochanteric rotational osteotomy [12], non-vascularized structural grafting [13–15], and vascularized bone graft [16, 17]. However, they all are not completely successful [18, 19], and there has not been a consensus on how to achieve the objectives of removing the painful necrotic bone while preserving the native hip geometry and restoring pain-free full hip range of motion [20].
The use of vascularized fibular grafts (VFG) was initiated in late 1970s [21–23]. Advocates of VFG believe that besides removal of the necrotic bone from the femoral head, the vascularization of the graft should enhance its incorporation to the host bed, maintain graft viability, and provide perfusion and osteoformative cells to the osteonecrotic area; these can be demonstrated in histologic sections of the femoral heads [18]. Nevertheless, there are also some results reported in the literature suggesting that the success rates are similar, whether or not the graft was vascularized [14, 15, 24] Some opponents deemed that VFG was no longer justified because of its low success rate, high complication rate or morbidity, and compromise of subsequent total hip arthroplasty (THA) [25, 26].
There have been a number of review articles updating the practice of the use of the vascularized fibular grafting to treat the ANFH [5, 27–29]. However, none of them applied statistical analysis for combining results from different studies to obtain a quantitative estimate of the overall effect and potential harm of VFG on ANFH compared with other treatment modalities. The primary aim of this systematic review and meta-analysis is to integrate the data from controlled clinical trials of VFG treatment of ANFH to demonstrate whether this method is still justified.
Methods
Literature search
A search of relevant systematic reviews on VFG in the Cochrane Library, the online MEDLINE, Embase, and Cochrane (CENTRAL) database search was conducted using the following keywords: vascularized fibula, vascularized fibular, free fibula, free fibular, vascularized bone graft, femur head, femoral head. Bibliographies from retrieved articles and relevant overview articles were checked to identify additional studies.
Inclusion criteria
It was planned to include a broad range of controlled comparison studies: randomized controlled trials (RCTs), controlled trials, and controlled before-and-after studies. As there were few such experimental studies, these observational studies have to be included as long as there is a control group to compare outcomes. The studies were included if they contained all of the following:
-
1.
The study population consisted of patients with ANFH.
-
2.
One of the treatments included vascularized fibular grafting for treating ANFH.
-
3.
A standardized outcome score was used to evaluate the outcome after surgery.
-
4.
Publication date was from January 1980 through April 2012.
Retrospective studies and studies without comparison group were excluded from the review.
Study selection and data extraction
Two investigators independently applied the inclusion criteria, reviewed titles and abstracts for potential inclusion. All articles deemed relevant to the study underwent a full review of the text. Data extraction was completed by two reviewers independently and disagreements in data extraction were resolved by discussion and consensus. Information was collected on the study population, intervention(s) performed, outcome measures and outcome. The follow-up time was also recorded. Furthermore, complication rates and failure rates (conversion to THA and/or radiographic collapse of the hip) were recorded.
Outcome measurement
All clinical outcomes were considered. A variety of outcome scores were acknowledged in this review, including the Harris Hip Score, Charnley’s modification of Merle d’ Aubigne and Postel’s Hip Function Score, survival rate, rate of conversion to THA, and the rate of collapse. Complications were analyzed as a distinct outcome subset.
Stratified failure rate was analyzed, in which the extracted follow-up data were investigated after two new stratification groups being made for analysis, including Group 1: Steinberg stage I and II (pre-collapse); Group 2: Steinberg stage II and III (pre-collapse to mild collapse). Two studies [30, 31] were excluded when analyzing Group 1, because cases of Steinberg stage I were not investigated in these two studies. To the study, in which Pittsburgh classification was applied, only Stage II was extracted because the Pittsburgh Stage II includes Stages II and III of the classification of Steinberg [32].
Validity assessment
In accordance with the recommendations of the Cochrane Collaboration [33], the Newcastle–Ottawa Quality Assessment Scale [34] was used to identify bias in the cohort studies and case-control studies. This scale was originally developed as a tool for quality assessment of non-randomized studies to be used in a systematic review. The scale uses a “star” rating system to judge the quality of studies from 0 to 9 stars using eight criteria that cover three sources of bias: selection, comparability, and outcome/exposure bias. Each criterion is worth one star except for comparability, which is worth two stars. Two authors independently assessed the methodological quality of the selected studies without blinding.
Assessment of heterogeneity and reporting bias
Heterogeneity between studies was described non-statistically and statistical heterogeneity between studies was examined visually using I 2 statistic and a Chi-squared test (a Chi-squared p value <0.1 or an I 2 value equal to or >50 % was considered indicative of possible heterogeneity). Deeks and colleagues (for the Cocharane Collaboration) [33] suggested the following as a rough guide for interpreting the I 2 statistic:
-
0–40 %: might not be important
-
30–60 %: may represent moderate heterogeneity
-
50–90 %: may represent substantial heterogeneity
-
75–100 %: considerable heterogeneity
Data synthesis and analysis
Data across the inclusion studies were pooled and summary estimates of treatment effect (odds ratio with associated 95 % confidence intervals) were calculated. Meta-analysis methods were selected based on study heterogeneity and the number of trials included in the analyses. When I 2 statistic was >50 %, substantial heterogeneity should be considered and the study results would be pooled using a random effects model. If no significant statistical heterogeneity was detected, or a small number of trials were included in the analysis, a fixed-effect model was applied [35, 36]. In the pooled analysis, studies were weighted by the Mantel–Haenszel methods for the reported outcome. The Review Manager (RevMan 5.1) software program [37] (The Nortic Cochrane Centre, Copenhagen, Denmark), provided by The Cochrane Collaboration, was used for graphical representation of the pooled data.
Results
Study selection
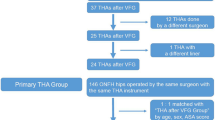
The keywords produced 203 hits and 95 duplicated studies were removed. Case reports and review articles were excluded on the basis of the abstract and title. As a result, only six comparative studies [19, 20, 30, 31, 38, 39] were included for methodological quality assessment in this review (Fig. 1). Among the six studies, three studies compared VFG with non-vascularized fibular graft [19, 30, 38], two studies set core decompression as a control group [20, 31], and the other one study described VFG versus vascularized iliac graft in the treatment of ANFH [39]. No systematic reviews and randomized clinical trials (RCTs) could be found. Details are shown in Table 1.
Validity assessment
The validity of the studies is summarized in Table 2. Of the six studies, only two studies reported their level of evidence (Therapeudic Level III) in the publication. The methodological qualities of the six included studies were independently assessed through the use of Newcastle–Ottawa Quality Assessment Scale. Two reports (Plaksechuk [19] and Kim [38]) had been scored eight stars and the other four studies had been awarded seven stars (Kane [31]), six stars (Scully [20]), five stars (Tetik [30]),and four stars (Yen [39]), respectively.
Clinical results
Three studies [19, 30, 38] were found to use Harris Hip Score [40] to evaluate the outcome. All of the three studies were comparing vascularized fibular versus non-vascularized fibular graft. The clinical result was graded as excellent when the Harris Hip Score was ≥90 points, good when it was between 80 and 89 points, fair when it was between 70 and 79 points, and poor when it was <70 points. In the study of Kim [38], the mean Harris Hip Score improved in 70 % (sixteen) of the 23 hips treated with vascularized grafting and in 35 % (eight) of the 23 hips treated with non-vascularized grafting. In the study of Plakseychuk [19], the mean Harris Hip Score improved in 70 % of the hips treated with free vascularized fibular grafting and improved in 36 % of the hips treated with non-vascularized fibular grafting. In the study of Tetik [30], when analyzing postoperative first year average Harris Hip Score, it was found that the patients treated with vascularized fibular grafting had an average postoperative Harris Hip Score of 83.09 ± 3.39. The patients treated with non-vascularized fibular grafting had an average postoperative Harris Hip Scores of 61.20 ± 4.26, and none was higher than 80. The clinical results of 58 of the 84 (69.0 %) VFG treated patients and 22 of the 88 (25.0 %) non-vascularized fibular graft treated patients were good or excellent (n = 172 total patients followed) (Fig. 2). Thus, patients treated with VFG were more likely to get good or excellent clinical result than those who were treated with non-vascularized fibular graft. When the clinical results were summated across studies, the weighted test for overall effect showed that the difference was of significance (OR 0.13; 95 % CI 0.03–0.51; p < 0.01; I 2 = 62 %).
Graph showing clinical results comparing vascularized fibular graft (VFG) versus non-vascularized fibular graft (NVFG) groups (P = 0.003). The size of each square is proportional to the weight of the study. Z p value of weighted test for overall effect, CI confidence interval, df degree of freedom, I 2 test statistic
Rate of conversion to THA
As an end-point of follow-up, all of the six included studies reported the cases that conversed to total hip arthroplasty. Meta-analyses were performed using the six studies (n = 984 total patients followed). In the 740 vascularized fibular treated patients, there were 122 conversions to THA (16.5 %). In the 244 patients treated with other methods including core decompression, non-vascularized fibular graft, and vascularized iliac graft, there were 104 conversions to THA (42.6 %). VFG can achieve lower conversion rate than the other three methods (OR 0.19; 95 % CI 0.13–0.28; p < 0.001; I 2 = 24 %) (Fig. 3).
Graph showing the rates of conversion to THA comparing vascularized fibular graft (VFG) versus other method groups (P < 0.00001). The size of each square is proportional to the weight of the study. Z p value of weighted test for overall effect, CI confidence interval, df degree of freedom, I 2 test statistic
Rate of collapse
Three of the included studies recorded the collapse rate. The literature review identified 172 patients, who all underwent vascularized or non-vascularized fibular grafting procedure. A total of 14 of 84 (16.7 %) hips treated with VFG collapsed, and a total of 56 of 88 (63.6 %) hips treated with non-vascularized fibular graft collapsed (Fig. 4). The result favored vascularized grafting more than non-vascularized grafting (OR 0.09; 95 % CI 0.01–0.57; p < 0.05; I 2 = 81 %).
Stratified failure rate
In cases of pre-collapse phase (Steinberg stage I and II) osteonecrosis, vascularized fibular grafting got a higher rate of hip joint salvage than other treatment modalities including core decompression, non-vascularized fibular grafting, and vascularized iliac grafting. Among the 270 hips, a total of 16 of 163 (9.8 %) hips treated with VFG failed, and a total of 43 of 107 (40.2 %) hips treated with non-vascularized fibular graft failed (OR 0.17; 95 % CI 0.09–0.33; p < 0.001; I 2 = 5 %) (Fig. 5).
Graph showing survival data of Steinberg stage I and II comparing vascularized fibular graft (VFG) versus other treatment groups (P < 0.00001). The size of each square is proportional to the weight of the study. Z p value of weighted test for overall effect, CI confidence interval, df degree of freedom, I 2 test statistic
In the treatment of the lesions of pre-collapse and early post-collapse (Steinberg stage II and III), vascularized fibular grafting has a higher survival rate than core decompression, non-vascularized fibular grafting, and even vascularized iliac grafting. A total of 899 hips were reported. 116 of 705 (16.5 %) hips treated with VFG failed, and a total of 83 of 194 (42.8 %) hips treated with non-vascularized fibular graft failed (OR 0.17; 95 % CI 0.11–0.26; p < 0.001; I 2 = 0 %) (Fig. 6).
Graph showing survival data of Steinberg stage II and III comparing vascularized fibular graft (VFG) versus other treatment groups (P = 0.01). The size of each square is proportional to the weight of the study. Z p value of weighted test for overall effect, CI confidence interval, df degree of freedom, I 2 test statistic
Complications
A specific set of complications being reported in all of the studies included claw toe, parethesia over lateral femoral cutaneous nerve, wound-edge necrosis, sensory peroneal neuropathy, flexor halluces longus contracture, proximal femur/subtrochanteric fracture, compartment syndrome at donor site, distal venous/graft vessel thrombosis, and inguinal protrusion.
Five studies were included in the meta-analysis, whereas, one study [20] did not mention complications. When complications are summated across studies, an un-weighted Chi-square analysis showed a lower complication rate in the methods other than VFG group. A total of 30 complications (23.8 %) were reported in 126 VFG treated patients and 13 complications (8.9 %) in 146 patients treated with core decompression, non-vascularized fibular graft, and vascularized iliac graft (n = 272 total patients followed, p < 0.01). However, in the weighted test for overall effect, this difference does not reach significance (OR 3.44; 95 % CI 0.81–14.62; p = 0.09; I 2 = 59 %) (Fig. 7).
Discussion
The literature has been systematically reviewed to evaluate the outcome and complications for patients with ANFH treated with VFG versus other treatment modalities, such as core depression [39], non-vascularized fibular graft [18, 36], and vascularized iliac graft [20, 31]. To our knowledge, this review article is the first systematic review and meta-analysis on this subject.
The cortical fibular graft not only offers structural stability, but also biologic incorporation, as the vascularized bone promotes callus formation and remodeling in the femoral head [41, 42]. In the total 984 patients described, 740 patients were treated with VFG and 244 were treated with the other method. Our meta-analysis revealed that VFG did have lower rate of conversion to THA than the other three methods. The overall clinical results could be only analyzed across the three studies that provided Harris Hip Score as outcome score. Patients with non-vascularized fibular graft were the control group in these three studies. The overall clinical results of the patients treated with VFG were better than those treated with non-vascularized fibular graft. Although the finding is in accordance with the published opinions [27–29], there are some potential biases in this result. As listed in Table 1, the maximum follow-up period of VFG group in the six included studies was only 96 months, which could not be deemed as a long-term follow-up, thus, potentially confounding the true outcomes. Despite the best efforts in using multiple search methods and content experts, it is possible that there’s still an eligible existing trial not detected, the results of which may be applicable to our meta-analysis. The conclusions drawn from a meta-analysis are only as unbiased and accurate as the data that are entered. Bias is inherent in analyses that focus on a specific population or geographic area. By including all studies available, including those from multiple countries reported in multiple languages, the conclusions of this review should be applicable to most populations.
Vascularized fibular grafts deter progression of pre-collapse lesions and can also delay the development of end stage osteonecrosis after mild collapse has occurred [43]. In the patients being classified as Steinberg stage I and II, our review demonstrated that the hips treated with VFG achieved functional joint salvage, which is higher than the rate of functional joint survival of the hips treated with other treatments. In the patients of Steinberg stage II and III, our meta-analysis revealed that the hips treated with VFG achieved functional joint, which is significantly higher than the functional joint survival of the hips treated with the other three methods.
There are several classification systems for ANFH. These classification systems include Marcus, Ficat, Steinberg, Pittsburgh, and Japanese Investigation Criteria for Avascular Necrosis of the Femoral Head [27]. When extracting the stratified survival data from the included studies, it was found that different classification systems were applied. Kane [31], Scully [20], and Tetik [30] used the Ficat classification; Kim [38] and Yen [39] used Steinberg classification; and Plakseychuk [19] used Pittsburgh classification. As is known, Ficat [44] classification system was developed using radiographic findings, consisting of four stages. Steinberg et al. [45] expanded this classification system, by dividing Ficat stage IV lesions into Steinberg stage IV, V, and VI based on whether femoral heads are with or without collapse, or hips with or without acetabular involvement. In addition, they quantified the amount of involvement of the femoral head into A (mild, <15 %), B (moderate, 15–30 %) and C (severe, >30 %), based on radiographs. Thus, these three systems are in the same series. With the data available, a conclusion could be drawn that VFG can sustain functional joint survival longer than the other methods.
Complications of VFG are divided into two types: those related to the harvesting of the fibular flap and those related to the hip reconstruction. The predominant complications in the VFG group were claw toe, sensory peroneal neuropathy, ankle pain, and distal venous/graft vessel thrombosis. Although an un-weighted Chi-square analysis shows that the overall complication rates in the VFG group were higher than those in the control groups, our meta-analysis indicates that the difference of the complication rate is of no significance, which means there is not enough evidence to ascertain that complication is more likely to happen in VFG group. On the other hand, in Kane’s [31] study, the complication rate in the VFG was 45 %, compared with the 10.2 % in the control group [31]. It might be a source of heterogeneity in assessment of complication rate.
The level of evidence of this review is debatable due to the quality of the included studies (Therapeudic Level III). Literature search could not detect any report of random controlled trials (RCTs), in which VFG was compared to the other treatment. The exact role of vascular anastomosis will not be clarified until a prospective, randomized, multicenter study is conducted by surgeons who are experts and skilled with the technique of graft placement, randomizing, patients to receive fibular graft with and without vascular anastomosis. Well-designed trials with blinded measurement of outcomes would help generate higher quality evidences, which would help in reaching more robust conclusion regarding these treatment modalities and would enable us to statistically analyze the outcomes as well.
Conclusions
In conclusion, our analysis represents the recent available evidence regarding the efficacy and potential harm of the four main treatment modalities of earlier stage of ANFH. Our review suggests that VFG is a justified method because of its better clinical result and lower conversion rate to THA than non-vascularized fibular graft, core decompression, and vascularized iliac graft. Although there is currently not a completely satisfactory method for treating osteonecrosis, VFG is an alternative that can prevent the necrotic femoral head from progressing to collapse which can retard or avoid hip replacement, especially in the patients of Steinberg stage I, II, and III.
References
Mankin HJ (1992) Nontraumatic necrosis of bone (osteonecrosis). N Engl J Med 326(22):1473–1479
Ohzono K, Saito M, Takaoka K (1991) Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br 73(1):68–72
Roshan A, Ram S (2008) The neglected femoral neck fracture in young adults: review of a challenging problem. Clin Med Res 6(1):33–39
Arlet J (1992) Nontraumatic avascular necrosis of the femoral head. Past, present, and future. Clin Orthop Relat Res 277:12–21
Aldridge JM 3rd, Urbaniak JR (2007) Avascular necrosis of the femoral head: role of vascularized bone grafts. Orthop Clin North Am 38(1):13–22
Fairbank A, Bhatia D, Jinnah R, Hungerford D (1995) Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br 77:42–49
Koo K, Kim R, Ko G, Song H, Jeong S, Cho S (1995) Preventing collapse in early osteonecrosis of the femoral head. A randomised clinical trial of core decompression. J Bone Joint Surg Br 77:870–874
Mont M, Carbone J, Fairbank A (1996) Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop 324:169–178
Helbig L, Simank HG, Kroeber M, Schmidmaier G, Grutzner PA, Guehring T (2012) Core decompression combined with implantation of a demineralised bone matrix for non-traumatic osteonecrosis of the femoral head. Arch Orthop Trauma Surg 132(8):1095–1103
Aaron R, Lennox D, Bunce G, Ebert T (1989) The conservative treatment of os- teonecrosis of the femoral head. A comparison of core decompression and pulsing electromagnetic fields. Clin Orthop 249:209–218
Bassett C, Schink-Ascani M, Lewis S (1989) Effects of pulsed electromagnetic fields on Steinberg ratings of femoral head osteonecrosis. Clin Orthop 246:172–185
Sugioka Y, Hotokebuchi T, Tsutsui H (1992) Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head. Indications and long-term results. Clin Orthop Relat Res 227:111–120
Boettcher W, Bonfiglio M, Smith K (1970) Non-traumatic necrosis of the femoral head. II. Experiences in treatment. J Bone Joint Surg Am 52:322–329
Buckley P, Gearen P, Petty R (1991) Structural bone-grafting for early atraumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 73:1357–1364
Smith K, Bonfiglio M, Montgomery WJ (1980) Non-traumatic necrosis of the femo- ral head treated with tibial bone-grafting. A follow-up note. J Bone Joint Surg Am 62:845–847
Katz R, Bourne R, Rorabeck C, McGee H (1992) Total hip arthroplasty in patients with avascular necrosis of the hip. Follow-up observations on cementless and cemented operations. Clin Orthop 281:145–151
Kirschenbaum I, Vernace J, Booth RJ, Balderston R, Rothman R (1991) Total hip arthroplasty for osteonecrosis. Semin Arthroplasty 2:234–240
Gonzalez Della Valle A, Bates J, Di Carlo E, Salvati EA (2005) Failure of free vascularized fibular graft for osteonecrosis of the femoral head: a histopathologic study of 6 cases. J Arthroplasty 20(3):331–336
Plakseychuk AY, Kim SY, Park BC, Varitimidis SE, Rubash HE, Sotereanos DG (2003) Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am 85:589–596
Scully SP, Aaron RK, Urbaniak JR (1998) Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am 80(9):1270–1275
Gilbert A, Judet H, Judet J, Ayatti A (1986) Microvascular transfer of the fibula for necrosis of the femoral head. Orthopedics 9:885–890
Urbaniak J, Coogan P, Gunneson E, Nunley J (1995) Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am 77:681–694
Sotereanos D, AY P, Rubash H (1997) Free vascularized fibula graft-ing for the treatment of osteonecrosis of the femoral head. Clin Orthop Relat Res 344:243–256
Steinberg ME, Larcom PG, Strafford B, Hosick WB, Corces A, Bands RE, Hartman KE (2001) Core decompression with bone grafting for osteonecrosis of the femoral head. Clin Orthop Relat Res 386:71–78
Hungerford DS (2007) Treatment of osteonecrosis of the femoral head: everything’s new. J Arthroplasty 22(4 Suppl 1):91–94
Aulakh TS, Rao C, Kuiper JH, Richardson JB (2010) Hip resurfacing and osteonecrosis: results from an independent hip resurfacing register. Arch Orthop Trauma Surg 130(7):841–845
Chen W, Zhang F, Chang S-M, Hui K, Lineaweaver WC (2006) Microsurgical fibular flap for treatment of avascular necrosis of the femoral head. J Am Coll Surg 202(2):324–334
Korompilias AV, Beris AE, Lykissas MG, Kostas-Agnantis IP, Soucacos PN (2011) Femoral head osteonecrosis: why choose free vascularized fibula grafting. Microsurgery 31(3):223–228
Zhang CQ, Gao YS, Zhu ZH, Yu XW (2011) Why we choose free vascularized fibular grafting for osteonecrosis of the femoral head? Microsurgery 31(5):417–418
Tetik C, Basar H, Bezer M, Erol B, Agir I, Esemenli T (2011) Comparison of early results of vascularized and non-vascularized fibular grafting in the treatment of osteonecrosis of the femoral head. Acta Orthop Traumatol Turc 45(5):326–334
Kane SM, Ward WA, Jordan LC, Guilford WB, Hanley EN Jr (1996) Vascularized fibular grafting compared with core decompression in the treatment of femoral head osteonecrosis. Orthopedics 19(10):869–872
Plakseychuk AY, Shah M, Varitimidis SE, Rubash HE, Sotereanos D (2001) Classification of osteonecrosis of the femoral head. Reliability, reproducibility, and prognostic value. Clin Orthop Relat Res 386:34–41
(2011) Cochrane handbook for systematic reviews of interventions, version 5.1.0 The Cochrane Collaboration, London, Available from: http://www.cochrane-handbook.org/
(2010) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses Ottawa. Ottawa Hospital Research Institute, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis. Wiley, Chichester
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
(2011) Review Manager (RevMan), Version 5.1. The Nortic Cochrane Centre, The Cochrane Collabration, Copenhagen
Kim SY, Kim YG, Kim PT, Ihn JC, Cho BC, Koo KH (2005) Vascularized compared with nonvascularized fibular grafts for large osteonecrotic lesions of the femoral head. J Bone Joint Surg Am 87(9):2012–2018
Yen CY, Tu YK, Ma CH, Yu SW, Kao FC, Lee MS (2006) Osteonecrosis of the femoral head: comparison of clinical results for vascularized iliac and fibula bone grafting. J Reconstr Microsurg 22(1):21–24
Harris W (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Brannon JK (2007) Influence of acetabular coverage on hip survival after free vascularized fibular grafting for femoral head osteonecrosis. J Bone Joint Surg Am. 89(2):448–449 author reply 449–450
Katz MA, Urbaniak JR (2001) Free vascularized fibular grafting of the femoral head for the treatment of osteonecrosis. Tech Orthop 16(1):44060
Kaushik AP, Das A, Cui Q (2012) Osteonecrosis of the femoral head: An update in year. World J Orthop 3(5):49–57
Ficat P, Arlet J (1977) Etiopathogenesis of arthrosis; nosological consequences. Rev Rhum Mal Osteoartic 44(11):627–631
Steinberg ME, Hayken GD, Steinberg DR (1995) A quantitative system for staging avascular necrosis. J Bone Joint Surg Br 77(1):34–41
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Fang, T., Zhang, E.W., Sailes, F.C. et al. Vascularized fibular grafts in patients with avascular necrosis of femoral head: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133, 1–10 (2013). https://doi.org/10.1007/s00402-012-1627-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1627-z