Abstract
Introduction
The insertion of thoracic pedicle screws (T1–T10) is subject to a relevant rate of malplacement. The optimum implantation procedure is still a topic of controversial debate. Currently, a postoperative computed tomography is required to evaluate the screw positions. The present study was undertaken to clarify whether intraoperative 3D imaging is a reliable method of determining the position of thoracic pedicle screws.
Methods
This prospective study involved 40 consecutive patients with thoracic spinal injuries, with intraoperative 3D scans being performed to determine the positions of 240 pedicle screws in T1–T10. The results of the 3D scans were compared with the findings of postoperative CT scans, using a clinical classification system.
Results
The positions of 204 pedicle screws could be viewed by means of both 3D and CT scans and the results compared. The 3D scans achieved a sensitivity of 90.9 % and a specificity of 98.8 %. The rate of misclassification by the 3D scans was 2.5 %. Nine pedicle screws were classified as misplaced and their position corrected intraoperatively (3.8 %). No screws required postoperative revision.
Conclusions
Performing an intraoperative 3D scan enables the position of thoracic pedicle screws to be determined with sufficient accuracy. The rate of revision surgery was reduced to 0 %.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The implantation of pedicle screws (PS) in the T1–T10 spinal section is regarded as difficult, owing to the particular anatomical features of the thoracic vertebral column [1]. The optimum implantation procedure is still a matter of controversial debate. Recommendations include “freehand” implantation, conventional image intensifier-controlled implantation and navigation-assisted application [2–4]. Pedicle screws with a diameter equal to or larger than the pedicle itself have to be used in the thoracic area to ensure adequate stability of the instrumentation [5]. Perforations of the pedicle walls are therefore to be expected. Between 0.3 and 8.5 %, thoracic pedicle screws are malplaced and require revision [2, 6, 7]. Malpositioned screws can impair the stability of the fixateur and cause neurovascular damage [8].
Conventional X-rays do not assess the position of pedicle screws reliably. For example, plain radiographs show medial pedicle violations only with a positive predictive value of 0.43 [9]. A correct classification is only possible by means of postoperative computed tomography [10, 11]. Only few hospitals have computed tomographic equipment installed for intraoperative use [12].
The development and introduction of 3D imaging technologies in recent years have made a new diagnostic procedure available in which multi-dimensional images of bone structures, fractures and implants in all areas of the skeleton can be viewed intraoperatively [13]. In the area of the spinal column, it is possible to reliably assess the position of pedicle screws between T11 and L5 [14].
The present study is intended to clarify whether an intraoperative 3D scan is a reliable method for determining the position of thoracic pedicle screws.
Materials and methods
Between October 2008 and December 2010, a total of 40 consecutive patients (13 female, 27 male) with unstable vertebral fractures were treated. We stabilized 3 incomplete (A3.1) and 20 complete (A3.3) burst fractures, 7 burst split fractures (A3.2), 1 transverse bicolumn and 9 fractures with a posterior disruption associated with Type A fracture (B1.2). 240 pedicle screws were inserted into the T1–T10 vertebrae. The distribution of the pedicle screws among the individual vertebrae is shown in Table 1. In this prospective study, an intraoperative 3D scan was conducted after implantation of the pedicle screws, using the 3D imaging system “Ziehm Vision Vario 3D” (Ziehm Imaging GmbH, Nuremberg, Germany). The “Ziehm Vision Vario 3D” is a second-generation 3D imaging system which provides improved image quality through the use of a pulsed generator and improved software with enhanced gray-scale differentiation.
The ages of the patients ranged between 11 and 78 years (median 44, average 45.8).
The patients underwent surgery in a prone position on a radiolucent carbon table. The fixateur used was the “Universal Spine System” (USS, Synthes, Umkirch near Freiburg, Germany) with pedicle screws 4.0–6.0 mm in diameter. The thickness of the pedicle screws to be employed was determined prior to surgery in the axial planes of the CT scans performed. The pedicle screws were positioned by four surgeons using the conventional open technique by reference to the dorsal anatomical structures of the spine and under simultaneous fluoroscopic control. The “scanning procedure” was defined as the amount of time, measured in minutes, taken from the calibration of the equipment to the end of the isocentric image acquisition cycle. The isocentric image acquisition was conducted, with the patient in apnea, by means of a fully automated orbital motion of the C-arm around the patient with a maximum rotational radius of 135°. A total of 110 individual images were acquired for each patient. After completion of the isocentric scan, the device used reconstruction algorithms to calculate a 3D data set on the basis of the cineloop images, the scan volume of which is equivalent to a cube with edge lengths of ~12 cm. The data set enables reconstructions to be made in axial, sagittal and coronal planes. In the spine segment under investigation, it is normally possible to illustrate five complete vertebral bodies. For each patient, only one scan was necessary in order to produce an image of the instrumented spine segment.
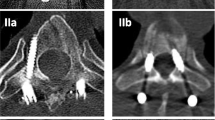
The 3D scan was evaluated intraoperatively by the operating surgeon. The basis for evaluation was the classification system developed by Zdichavsky et al. [15] (Table 2). If malpositionings requiring correction were found, the screws were repositioned. Malpositionings in absolute need of correction were classified as Types IIIa and IIIb, and malpositionings in relative need of correction were classified as Types IIa and IIb. In cases of screw correction and repeated intraoperative scan, the second 3D scan was evaluated in comparison with the CT scan.
Postoperative computed tomographies were performed of 36 patients on the instrumented spine segment to plan an additive ventral procedure. The equipment used was the “Aquilion 64” spiral CT scanner (Toshiba Computer Systems, Neuss, Germany) with a collimation of 0.5 mm and with employment of a metal artifact reduction program. The postoperative evaluation of the images was carried out by the two experienced spinal surgeons (T.M., M.B.) using a web server (Impax ES Web 1000 System, Agfa-Gevaert Group, Germany) and employing the consensual procedure. When findings differed, the “higher-grade” misplacement was assumed. The CT results were taken as the “gold standard” for the comparisons. In the axial reconstructions produced using both procedures, the positions of the pedicle screws were determined and compared using the classification systems developed by Zdichavsky et al. [15] (Table 2; Fig. 1a–e).
Scoring system of pedicle screws by Zdichavsky et al. [15]
In addition, the postoperative computed tomography scanned screws were classified into four groups “completely intrapedicular”, “penetration of cortical”, “pedicles perforation up to 2 mm” and “extension beyond the pedicle wall up to 3 mm”.
Criteria for the need of postoperative correction were medial constriction of the spinal canal by more than 3 mm and lateral malpositioning with an extracorporeal screw tip in the immediate vicinity of viscero-vascular structures, as well as pedicle screws where more than half the screw shaft was positioned outside the pedicle and corpus.
The radiation times (seconds) and radiation doses (cGy/cm2) were recorded for the conventional X-ray for the 3D scan and as a total.
Results
The average width of the pedicles, which was measured by CT preoperatively, was 4.6 mm (3–7 mm, median 4). The diameter of the implanted pedicle screws (PS) was in 32 cases larger than, in 142 cases equal to and in 66 cases smaller than the measured maximum diameter of the pedicle to be instrumented.
For each patient, one 3D scan was performed over the instrumented spine segment. Intraoperative assessment of the 3D scans resulted in nine screws in eight patients being assessed as relevant misplacements, and these were immediately repositioned (5 lateral, 4 medial misplacements) (Fig. 2a–c). Five of the corrected PS were checked in a repeat 3D scan (Fig. 3a, b).
The positions of 204 PS could, therefore, be compared using both imaging procedures.
CT scan evaluations (208 PS) showed 174 PS to be in the ideal Type I position, 34 PS were moderately malpositioned (Type Ib 10×, Type IIa 10×, Type IIb 14×), and no PS were classified as being in need of repositioning (Type IIIa, IIIb).
When the CT and 3D scans (204 PS) were compared, it was found that 169 out of 171 PS had been correctly recognized by the 3D scans as Type Ia, 9 out of 10 PS as Type Ib, 8 out of 9 PS as Type IIa and 13 out of 14 PS as Type IIb. Five PS were incorrectly classified by one classification level; there were no incorrect classifications by two classification levels. We did not find any PS requiring repositioning (Type III) or causing neurovascular complications.
The sensitivity reached 90.9 % and the specificity 98.8 %. Out of 204 PS, 199 (97.5 %) were correctly classified and 2.5 % of the PS (5 out of 204) were incorrectly classified.
In the postoperative computed tomography, 75 screws were found to be in a completely intrapedicular position, 41 screws penetrated the cortical bone to a minimal extent, 84 screws perforated the pedicles up to a width of 2 mm and 4 screws extended beyond the pedicle wall up to 3 mm. There were no malpositionings causing injury to the superior and inferior pedicle borders.
The median scan duration was 5.1 min (4–7 min). The median overall time including the 3D scan assessment required 8 min (5–11 min).
The median radiation time during the isocentric imaging was 66 s (60–72 s, average 67 s) and the median entire scanning time amounted to 317 s (average 378 s, 154–901 s). The median radiation dose applied in the 3D scan was 250 cGy/cm2 (average 247.4 cGy/cm2, 87–380 cGy/cm2) and the median total radiation dose was 1,591 cGy/cm2 (average 1,846.2 cGy/cm2, 445–4,545 cGy/cm2).
Discussion
Functionally and anatomically, the T1–T10 vertebrae form the kyphosis region of the thoracolumbar spine. This region has a number of specific anatomical features. The corpora shows a heart-shaped structure; pedicle screw length and pedicle width are significantly affected by patient sex, and the convergence angle of the pedicles varies between 7° and 28.4° with a median diameter of only 3.7 mm at T5 [16–18].
The implantation of thoracic pedicle screws is regarded as difficult, and as late as 1995 Vaccaro et al. [1] recommended giving preference to other stabilization methods owing to the high rate of complications. Medial screw perforations quickly lead to a relevant constriction of the spinal canal, and it is to be feared that injuries to the dura mater and spinal cord may occur. Anatomical investigations conducted by Lien et al. [19] have demonstrated that the distance between the medial pedicle walls of T1–T10 and the dura mater is only 1.0–1.5 mm. Most breach rates occurred at T4 and T6 using conventional freehand pedicle screw placement with intraoperative lateral radiograph [20].
The implantation methods for thoracic pedicle screws are the subject of controversial debate. The recommendations range from the freehand technique via image intensifier-controlled insertion to navigation-assisted application [2–4, 8, 20, 21]. A meta-analysis of 130 published studies has not found evidence of any advantage of navigation over conventional implantation techniques for pedicle screws in the thoracic region [22]. The problem of malpositioned screws continues to be evident.
Perforations of the thoracic pedicle walls by pedicle screws, which had a diameter of at least 4 mm in all the studies, are in many cases unavoidable and have been described for up to 70.9 % of pedicle screws [5]. Malplacements classified as acceptable are medial pedicle perforation by up to 2–3 mm and lateral “in–out–in” positions [6, 15, 23]. Misplacements considered as clinically relevant are higher-grade perforations by PS, which lead to neurovascular and visceral injuries or constitute a secondary cause of these, and laterally malpositioned PS which impair the stability of the fixateur owing to insufficient bone contact [8].
Intraoperative recognition of these relevant screw misplacements cannot prevent primary structural damage, but correction of the screw positions is necessary in order to prevent secondary complications. Intraoperative conventional image intensifier monitoring does not offer sufficient safety to detect malplaced screws, and only few centers have the facilities to perform intraoperative CT scans [12]. This results in rates of up to 8.6 % “high risk” and unacceptable PS, which have hitherto had to be repositioned in postoperative corrective surgery (Table 3).
The intraoperative use of 3D image intensifiers first became established in the treatment of intra-articular injuries to the extremities [24]. Regarding the spine, it was shown in a comparative experimental cadaver study that the sagittal cross sections of cement-augmented vertebrae could be reliably depicted and anatomically accurate measurements obtained by means of 3D scans [25]. The control of the positions of pedicle screws using 3D image intensifiers was first investigated on a cadaver model by Wang et al. [26]. All pedicle perforations by screws in excess of 2 mm in the thoracic region were recognized. A clinical study demonstrated a high overall degree of accuracy in the thoracolumbar region, but a significantly increased rate of inaccuracy in the case of 3D scans of the T1–T10 segment when using a first-generation 3D image intensifier [14].
A concurrent intraoperative imaging system that combines intraoperative fluoroscopy with the capability of multi-dimensional imaging is the “O-arm”. A human cadaveric study showed nearly the same rates of sensitivity, specificity and accuracy compared with 3D image intensifier data [26, 27]. The “O-Arm” has a few major disadvantages, firstly the higher prime costs, secondly the “O-arm” is lacking dexterity and on top of that it cannot be used as a conventional 2D image intensifier.
In thoracic scoliosis surgery, spinal cord monitoring by EMG threshold testing is another modality in which the accuracy of pedicle screw placement can be controlled. Samdani et al. [28] reported a low sensitivity and low positive predictive value of EMG to predict medial breaches from T2 to T9. Also, de Blas et al. [29] stated that t-EMG technique has low sensitivity to predict screw malpositioning and cannot discriminate between medial cortex breakages and complete invasion of the spinal canal.
In our study, the intraoperative employment of a second-generation 3D image intensifier led to the repositioning of nine pedicle screws. The postoperative CT scans did not reveal any further misplacements requiring correction among the pedicle screws implanted in our patients. The maximum anticipated correction rate was reduced from a hypothetical rate of 3.8 % (9 out of 240 PS) to a real rate of 0 %.
When using 3D image intensifiers of the current generation, scores should be used which relate to clinical criteria and take account of the overall position of the PS in the pedicle and corpus [6, 15]. This leads to a level of high sensitivity and specificity and allows the screw positions to be correctly determined in 97.5 % of cases.
The amount of time required for the complete procedure is 8 min, which is reasonable and acceptable.
Preoperative computerized tomographic scans are routinely obtained to evaluate morphology and classification of vertebra fractures [2, 7, 20, 21]. Postoperative computed tomography is the routine method in several clinics with which the accuracy of pedicle screw placement is evaluated [3, 5–7, 20, 21, 23]. The effective dose of thoracic spine CT examination has been reported to be ~17.99 mSV compared to 0.08 mSV of conventional chest radiograph [30]. Theoretical risk ratio for inducting a cancer with CT scanning of the whole thoracic spine over a lifetime is 1 in 1,800, whereas CT imaging of 3 thoracic vertebrae carries a risk of 1 in 5,800 [31]. Although no study has established an increased prevalence of malignant disease secondary to diagnostic imaging procedures yet, these theoretical data suggest that CT examinations are not benign and ratios of benefit to risk should be regarded. Postoperative low-dose spine CT is a reliable method to reduce the estimated effective dose in the assessment of pedicle screw placement [31, 32].
For the patients in our study, the mean intraoperative radiation dose increased by 16 %. Dose comparisons between 3D and CT scans were conducted by Rock et al. [13] on a phantom. A standardized spiral CT scan of the lumbar vertebrae showed significantly higher dose values than a comparable 3D scan. Hence, if the postoperative CT scan for checking the position of pedicle screws were to be replaced by the performance of an intraoperative 3D scan, the total radiation dose to which the patient is exposed would be reduced. For the operating staff, there is also no increase in radiation exposure, since the isocentric cineloop is fully automated and performed solely by the image intensifier, so that the personnel can maintain an adequate distance from the scanner.
The performance of an intraoperative 3D scan permits the position of pedicle screws in the T1–T10 region to be determined with sufficient accuracy on the basis of a clinical classification system. The 3D scan offers the advantage that screws can be repositioned immediately during the operation, and this led to immediate repositioning in the case of 3.8 % of the screws. It was possible to reduce the rate of secondary correctional surgery.
References
Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS (1995) Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am 77:1200–1206
Bransford R, Bellabarba C, Thompson JH, Henley MB, Mirza SK, Chapman JR (2006) The safety of fluoroscopically-assisted thoracic pedicle screw instrumentation for spine trauma. J Trauma 60:1047–1052
Lekovic GP, Potts EA, Karahalios DG, Hall G (2007) A comparison of two techniques in image-guided thoracic pedicle screw placement: a retrospective study of 37 patients and 277 pedicle screws. J Neurosurg Spine 7:393–398
Schizas C, Theumann N, Kosmopoulos V (2007) Inserting pedicle screws in the upper thoracic spine without the use of fluoroscopy or image guidance. Is it safe? Eur Spine J 16:625–629
Kuntz C, Maher PC, Levine NB, Kurokawa R (2004) Prospective evaluation of thoracic pedicle screw placement using fluoroscopic imaging. J Spinal Disord 17:206–214
Upendra BN, Meena D, Chowdhury B, Ahmad A, Jayaswal A (2008) Outcome-based classification for assessment of thoracic pedicular screw placement. Spine 33:384–390
Zdichavsky M, Blauth M, Knop C, Lotz J, Krettek C, Bastian L (2004) Accuracy of pedicle screw placement in thoracic spine fractures. Part II: a retrospective analysis of 278 pedicle screws using computed tomographic scans. Eur J Trauma 30:241–247
Sarlak AY, Tosun B, Atmaca H, Sarisoy HT, Buluc L (2009) Evaluation of thoracic pedicle screw placement in adolescent idiopathic scoliosis. Eur Spine J 18:1892–1897
Kim YJ, Lenke LG, Cheh G, Riew KD (2005) Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine 30:2084–2088
Berlemann U, Heini P, Müller U, Stoupis C, Schwarzenbach O (1997) Reliability of pedicle screw assessment utilizing plain radiographs versus CT reconstruction. Eur Spine J 6:406–411
Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S (1988) Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine 13:1012–1018
Zausinger S, Scheder B, Uhl E, Heigl T, Morhard D, Tonn JC (2009) Intraoperative computed tomography with integrated navigation system in spinal stabilizations. Spine 34:2919–2926
Rock C, Kotsianos D, Linsenmaier U, Fischer T, Brandl R, Vill F, Wirth S, Kaltschmidt R, Euler E, Pfeifer KJ, Reiser M (2002) Studies on image quality, high contrast resolution and dose for the axial skeleton and limbs with a new, dedicated CT system (ISO-C-3 D). Rofo 174:170–176
Beck M, Mittlmeier T, Gierer P, Harms C, Gradl G (2009) Benefit and accuracy of intraoperative 3D-imaging after pedicle screw placement: a prospective study in stabilizing thoracolumbar fractures. Eur Spine J 18:1469–1477
Zdichavsky M, Blauth M, Knop C, Graessner M, Hermann H, Krettek C, Bastian L (2004) Accuracy of pedicle screw placement in thoracic spine fractures. Part I: inter- and intraobserver reliability of the scoring system. Eur J Trauma 30:234–240
Berlet GC, Boubez G, Gurr KR, Bailey SI (1999) The USS pedicle hook system: a morphometric analysis of its safety in the thoracic spine. J Spinal Disord 12:234–239
Kretzer RM, Chaput C, Sciubba DM, Garonzik IM, Jallo GI, McAfee PC, Cunningham BW, Tortolani PJ (2011) A computed tomography-based morphometric study of thoracic pedicle anatomy in a random United States trauma population. J Neurosurg Spine 14:235–243
Vaccaro AR, Rizzolo SJ, Allardyce TJ, Ramsey M, Salvo J, Balderston RA, Cotler JM (1995) Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am 77:1193–1199
Lien SB, Liou NH, Wu SS (2007) Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J 16:1215–1222
Parker SL, McGirt MJ, Farber SH, Amin AG, Rick AM, Suk I, Bydon A, Sciubba DM, Wolinsky JP, Gokaslan ZL, Witham TF (2011) Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery 68:170–178
Fisher CG, Sahajpal V, Keynan O, Boyd M, Graeb D, Bailey C, Panagiotopoulos K, Dvorak F (2006) Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine 5:520–526
Kosmopoulos V, Schizas C (2007) Pedicle screw placement accuracy. A meta-analysis. Spine 32:E111–E120
Belmont JB, Klemme WR, Dhawan A, Polly DW (2001) In vivo accuracy of thoracic pedicle screws. Spine 26:2340–2346
Atesok K, Finkelstein J, Khoury A, Peyser A, Weil Y, Liebergall M, Mosheiff R (2007) The use of intraoperative three-dimensional imaging (ISO-C-3D) in fixation of intraarticular fractures. Injury 38:1163–1169
Verlaan JJ, van de Kraats EB, van Walsum T, Dhert WJA, Oner FC, Niessen WJ (2005) Three-dimensional rotational X-ray imaging for spine surgery. Spine 30:556–561
Wang MY, Kim KA, Liu CY, Kim P, Apuzzo ML (2004) Reliability of three-dimensional fluoroscopy for detecting pedicle screw violations in the thoracic and lumbar spine. Neurosurgery 54:1138–1142
Santos ER, Ledonio CG, Castro CA, Truong WH, Sembrano JN (2012) The accuracy of intraoperative O-arm images for the assessment of pedicle screw position. Spine 37:E119–E125
Samdani AF, Tantorski M, Cahill PJ, Ranade A, Koch S, Clements DH, Betz RR, Asghar J (2011) Triggered electromyography for placement of thoracic pedicle screws: is it reliable? Eur Spine J 20:869–874
de Blas G, Barrios C, Regidor I, Montes E, Burgos J, Pizá-Vallespir G, Hevia E (2012) Safe pedicle screw placement in thoracic scoliotic curves using t-EMG stimulation threshold variability at concavity and convexity in apex segments. Spine 37:E387–E395
Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN (2009) Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am 91:1882–1889
Richards PJ, George J, Metelko M, Brown M (2010) Spine computed tomography doses and cancer induction. Spine 35:430–433
Abul-Kasim K, Ohlin A, Strömbeck A, Maly P, Sundgren PC (2010) Radiological and clinical outcome of screw placement in adolescent idiopathic scoliosis: evaluation with low-dose computed tomography. Eur Spine J 19:96–104
Acknowledgments
The authors thank T. Wodetzki (University of Rostock) for designing the medical illustrations.
Conflict of interest
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of the manuscript including National Institutes of Health (NIH), Wellcome Trust, Howard Hughes Medical Institute (HHMI), and others.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beck, M., Rotter, R., Gradl, G. et al. Reliability and consequences of intraoperative 3D imaging to control positions of thoracic pedicle screws. Arch Orthop Trauma Surg 132, 1371–1377 (2012). https://doi.org/10.1007/s00402-012-1555-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1555-y