Abstract
Several studies have looked at accuracy of thoracic pedicle screw placement using fluoroscopy, image guidance, and anatomical landmarks. To our knowledge the upper thoracic spine (T1–T6) has not been specifically studied in the context of screw insertion and placement accuracy without the use of either image guidance or fluoroscopy. Our objective was to study the accuracy of upper thoracic screw placement without the use of fluoroscopy or image guidance, and report on implant related complications. A single surgeon inserted 60 screws in 13 consecutive non-scoliotic spine patients. These were the first 60 screws placed in the high thoracic spine in our institution. The most common diagnosis in our patient population was trauma. All screws were inserted using a modified Roy-Camille technique. Post-operative axial computed tomography (CT) images were obtained for each patient and analyzed by an independent senior radiologist for placement accuracy. Implant related complications were prospectively noted. No pedicle screw misplacement was found in 61.5% of the patients. In the remaining 38.5% of patients some misplacements were noted. Fifty-three screws out of the total 60 implanted were placed correctly within all the pedicle margins. The overall pedicle screw placement accuracy was 88.3% using our modified Roy-Camille technique. Five medial and two lateral violations were noted in the seven misplaced screws. One of the seven misplaced screws was considered to be questionable in terms of pedicle perforation. No implant related complications were noted. We found that inserting pedicle screws in the upper thoracic spine based solely on anatomical landmarks was safe with an accuracy comparable to that of published studies using image-guided navigation at the thoracic level.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pedicle screw use for spinal fixation was first reported in the 1970s [23]. Pedicle screw insertion in the lumbosacral region of the spine has been extensively studied and is widely performed today. The relative ease of implantation is mainly due to the larger size of both the vertebral body and the pedicle diameters, as compared to the mid and upper thoracic vertebral anatomy [20]. Interest in thoracic pedicle screw use has gained momentum recently, especially in the lower thoracic spine, as it presents an alternative to the use of hook and wire fixation [14, 15]. Safety concerns with the use of upper thoracic pedicle screws however, have led to limited use and consequently circumscribed reported clinical experience.
Safety concerns with thoracic pedicle screw placement include neurological complications with more severe consequences when compared to the lumbar spine, caused by possible violations to the spinal canal, and vascular and/or visceral injury. This is especially the case for the mid and upper thoracic spine having smaller pedicle diameters and being closer in proximity to vascular structures [27, 28]. Consequently, the surgical approach in this region presents a higher risk, especially in deformity correction, and is more intricate and limiting in regards to the use of pedicle screw instrumentation. It is therefore important to study optimal placement of thoracic pedicle screws in order to evaluate safety of their use. The goal is to improve methods for avoiding screw misplacement [9, 20].
In our institution, given the encouraging results of thoracic pedicle fixation in scoliosis [10], we recently moved away from hook and/or wire fixation for nondeformity cases. Our aim was to begin on nondeformity cases and prospectively assess the accuracy and complications related to pedicle screw placement in the upper thoracic spine, in our first consecutive series of patients requiring high thoracic fixation, using post-operative computed tomography (CT). Additionally, we aimed to examine the safety of inserting screws from T1 to T6 without the use of fluoroscopy, which we found cumbersome and offering poor visualization of the cervicothoracic junction in most of our cases. Finally we aimed to compare our findings to the limited published data on pedicle screw placement accuracy in nondeformed high thoracic spines.
Methods
Sixty upper thoracic (T1–T6) pedicle screws were implanted in 13 consecutive patients (9 males, 4 females) having an average 54 years of age (range 18–80) at the time of surgery. Pre-operative diagnosis was trauma in ten patients, tuberculosis of the spine (one patient), degenerative disc disease adjacent to a long instrumented fusion (one patient), and rheumatoid arthritis (RA) (one patient). Only the latter patient had pre-operative neurological impairment (Ranawat III B). All surgeries were performed by the same senior surgeon. Various surgical techniques have been described for inserting pedicle screws, the more widely used being those of Roy-Camille et al. [24], and Lenke et al. [13]. The surgical technique used in this study for the upper thoracic spine was based on a modification of the Roy-Camille technique [24], with the addition of mandating pre-operative planning based on CT images. In essence, the entry point and direction in the axial plane were defined based on axial CT images obtained pre-operatively (Fig. 1). On the CT images the deepest part of the junction between the transverse process (TP) and lamina was first defined (point p, later the entry point), and then a line was drawn linking this point to the middle of the pedicle (line AB). Then the mid sagittal line was drawn, linking the middle of the lamina to the middle of the vertebral body (line BC). The angle formed by these two lines (α) defined the intended screw direction on the axial plane. During surgery the entry point p was chosen at the deepest part of the junction of the TP and lamina, a landmark we found to be relatively easy to locate in the mediolateral direction. In the craniocaudal direction the entry point was chosen at the most superior border of the aforementioned junction of the TP and lamina. The entry point was opened using a high-speed drill. A curette or a drill, depending on bone quality, was subsequently used to cannulate the pedicle. The axial plane direction mimicked as much as possible the α angle drawn on the CT images. In the sagittal plane, a direction perpendicular to the posterior elements was chosen. No laminectomy or facetectomy was performed. Screw diameter tended to be 4.35 mm in the upper four thoracic vertebrae. Multiaxial titanium implants were used. No fluoroscopy, X-rays or neurophysiological studies were performed during surgery.
Pre-operative CT scan used to determine the entry point p, defined as the deepest part of the junction between the transverse process and lamina, and the direction (angle α) of the pedicle screw. Angle α is formed by a line linking point p to the middle of the pedicle (line AB), and the mid sagittal line linking the middle of the lamina to the middle of the vertebral body (line BC)
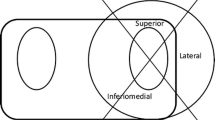
Post-operative CT scans were obtained for all 13 patients in order to assess implant position. Image acquisition was performed in helical mode using an eight-detector row Lightspeed CT unit (GE Medical Systems, Milwaukee, WS, USA) in the craniocaudal direction. The imaging series consisted of 2.5 mm thick CT sections (collimation, 8 × 2.5 mm) reconstructed at 2 mm intervals with a pitch of 0.875:1 and acquisition parameters of 120 kVp and 280 mAs. The raw data was used to reconstruct transverse 2.5 mm thick CT cross sections every 2 mm with a field of view adequate for visualization of the spine. The transverse images were read and assessed by an independent radiologist according to the “in”, “out”, or “questionable” criteria previously published in the literature [3]. To clarify our use of this technique, screws inside the pedicle were classified as “in”, screws with possible perforation but not clearly visible were classified as “questionable”, and any perforation of the pedicle was classified as “out” (Fig. 2). Screws were also screened for anterior perforations of the vertebral body.
Results
A total of 60 pedicle screws were placed in our region of interest (upper thoracic spine T1–T6) and evaluated for placement accuracy. No screw placement had to be abandoned due to intra-operative perforation. Some screws were deliberately placed unilaterally only in an effort to minimize the total number of upper thoracic implants. The average follow up was 21 months (8–40). The distribution of the pedicle screws per level and corresponding accuracy can be seen in Table 1. Fifty-three out of the 60 screws were placed correctly giving an overall accuracy of 88.3%. Four of the six screws classified as “out” had medial violations (1 at T2 and 3 at T6) and the other two screws had lateral violations (T4, T5). A single “questionable” screw at T1 was identified to be possibly perforating the medial pedicle cortex.
Eight out of the 13 patients (61.5%) had all of the inserted screws classified as “in”. One (7.7%) of the five remaining patients, having a classification other than “in”, had two screws classified as “out” (T2, T6) and one screw as “questionable” (T1), all in the medial direction. The majority of the medially misplaced screws (4/5), were located in the left-side pedicles. Four anterior perforations were noted from which three were left sided (2 at T5 and 1 at T6) without abutting the aorta.
No post-operative complications related to screw misplacement were observed. We did nevertheless have a deep infection in the RA patient and one wound dehiscence in a fracture case. Both patients required re-operation and fully recovered. The only patient with abnormal neurology, the one with RA, improved post-operatively. At latest follow up, no late neurological symptoms occurred and no implant loosening was observed in any of the other remaining patients.
Discussion
Insertion of thoracic pedicle screws is a demanding technique especially in the upper half of the thoracic spine. Even though in theory fluoroscopy can help, its practical use in this region of the spine has limitations. Visualization of the cervicothoracic junction on lateral images is a limitation, due to the humeral head projection, as is good visualization of the upper thoracic pedicles on lateral images, due to the interference generated by the lungs and rib heads. Anterio-posterior (AP) fluoroscopy is an alternative but requires an operating table or set up permitting access to the image intensifier. Another option may be obtaining an intra-operative chest film, something we did not use for practical reasons. CT or fluoroscopy based navigation could be further alternatives, however, in our experience using such technology for lumbar cases, we have observed a significant increase in operative time as already supported by the literature [18]. Furthermore, not all navigation methods are equal, with some offering an unacceptable rate of misplacement [18].
Previous studies evaluating thoracic placement have focused mostly in the lower thoracic region [1, 4, 12, 16, 17, 19, 26, 29]. Furthermore, accuracy of thoracic pedicle screw instrumentation has been reported in several cadaveric populations [5, 7, 21, 22, 25, 28, 29, 31, 32], and with the use of assisted-navigation techniques [2, 5, 6, 8, 25]. While there is data on thoracic screw placement accuracy in the literature, we found little information specifically reporting on upper thoracic screws inserted in vivo on nondeformed spines.
A search of the relevant literature on in vivo studies involving purely thoracic pedicle screws inserted between T1 and T6 with the help of navigation showed an accuracy of 88.5% [33]. It should be noted however, this placement accuracy reported does include some deformity cases in the final statistic. An in vivo study of non-deformed spines [11] reported on 27 and 109 screws placed at T1–T2 and between T3 and T9, respectively, from a total of 209 placed between T1 and T12. The use of fluoroscopy was employed which resulted in an approximate placement accuracy of 56% for the T1–T2 screws, and 14% for the T3–T9 screws. In the study, screws penetrating the lateral pedicle wall adjacent to the rib head were also considered to be accurately placed, which is currently recognized as posing no threat and giving satisfactory fixation. In our study, the overall accuracy of 88.3% compares well with the first aforementioned study reporting on pedicle screw placement using image-guided navigation.
Our study, to our knowledge, reports on the largest number of upper thoracic screws placed in vivo without the assistance of fluoroscopy or navigation, simply using anatomical landmarks. We must emphasize however, that obtaining a CT or magnetic resonance imaging (MRI) scan pre-operatively should be mandatory if no fluoroscopy or other type of imaging or navigation is used during surgery. This pre-operative imaging helps the surgeon plan entry point, screw direction, and screw diameter. A big proportion of our patients were trauma cases, and as such, CT images were already available as part of the routine procedure performed at our institution [30]. Nevertheless, to avoid the radiation dose to the patient from CT, MRI may be an acceptable alternative for determining the screw entry point and direction.
Taking into account that this study included our first patients to benefit from upper thoracic pedicle screw insertion, we found upper thoracic pedicle screw placement to be safe providing that special attention is paid to pre-operative CT images and the insertion technique. In addition, we acknowledge that the reported accuracy from this insertion technique could depend on the expertise of the surgeon and might not be reproducible by less experienced surgeons.
Every effort should be taken to improve accuracy of screw placement in the upper thoracic spine. We found that routine feedback from post-operative CT was helpful in establishing our misplacement rate and helpful in improvement of the technique. In conclusion, we feel that for experienced surgeons familiar with insertion of screws in the lumbar and/or lower thoracic spine in nondeformity cases, insertion of upper thoracic screws should constitute no major difficulty. Nevertheless, one should not underestimate the danger of inserting screws from T6 and above and every effort should be made to further develop safer and easier guidance/imaging techniques.
References
Amiot LP, Lang K, Putzier M, Zippel H, Labelle H (2000) Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine 25(5):606–614
Choi WW, Green BA, Levi AD (2000) Computer-assisted fluoroscopic targeting system for pedicle screw insertion. Neurosurgery 47(4):872–828
Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR (1995) Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine 1494–1499
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine 15:11–14
Hart RA, Hansen BL, Shea M, Hsu F, Anderson GJ (2005) Pedicle screw placement in the thoracic spine: a comparison of image-guided and manual techniques in cadavers. Spine 30(12):E326–E331
Holly LT, Foley KT (2003) Three-dimensional fluoroscopy-guided percutaneous thoracolumbar pedicle screw placement. Technical note. J Neurosurg 99(3 suppl):324–329
Jang JS, Lee WB, Yuan HA (2001) Use of a guide device to place pedicle screws in the thoracic spine: a cadaveric study. Technical note. J Neurosurg 94(2 suppl):328–333
Kim KD, Patrick JJ, Bloch BO, Masciopinto JE (2001) Computer-assisted thoracic pedicle screw placement: an in vitro feasibility study. Spine 26(4):360–364
Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29(3):333–342 (discussion 342)
Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G (2006) Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine 31:291–298
Kuntz C, Maher PC, Levine NB, Kurokawa R (2004) Prospective evaluation of thoracic pedicle screw placement using fluoroscopic imaging. J Spinal Disord Tech 17(3):206–214
Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients (see comment). Eur Spine J 9(3):235–240
Lenke LG, Rinella AS, Kim YJ (2002) Free-hand thoracic pedicle screw placement. Semin Spine Surg 14:48–57
Liljenqvist UR, Halm HF, Link TM (1997) Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine 22(19):2239–2245
Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H (2002) Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J 11:336–343
Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB (1999) Complications associated with pedicle screws (see comment). J Bone Joint Surg Am 81(11):1519–1528
Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Troccaz J, Cinquin P, Sautot P (1998) Computer-assisted spine surgery. Comput Aided Surg 3(6):297–305
Mirza SK, Wiggins GC, Kuntz C, York JE, Bellabarba C, Knonodi MA, Chapman JR, Shaffrey CI (2003) Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance: a cadaver study. Spine 28:402–413
Odgers CJ, Vaccaro AR, Pollack ME, Cotler JM (1996) Accuracy of pedicle screw placement with the assistance of lateral plain radiography. J Spinal Disord 9(4):334–338
Rampersaud YR, Pik JH, Salonen D, Farooq S (2005) Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine 30(7):E183–E190
Rao G, Brodke DS, Rondina M, Dailey AT (2002) Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg 97(2 suppl):223–226
Rao G, Brodke DS, Rondina M, Bacchus K, Dailey AT (2003) Inter- and intraobserver reliability of computed tomography in assessment of thoracic pedicle screw placement. Spine 28(22):2527–2530
Roy-Camille R, Saillant G, Berteaux D, Salgado V (1976) Osteosynthesis of thoraco-lumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol 15:2–16
Roy-Camille R, Saillant G, Mazel C (1986) Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am 17:147–159
Sagi HC, Manos R, Park SC, Von Jako R, Ordway NR, Connolly PJ (2003) Electromagnetic field-based image-guided spine surgery part two: results of a cadaveric study evaluating thoracic pedicle screw placement. Spine 28(17):E351–E354
Schulze CJ, Munzinger E, Weber U (1998) Clinical relevance of accuracy of pedicle screw placement. A computed tomographic-supported analysis. Spine 23(20):2215–2220 (discussion 2220–2221)
Sucato DJ, Duchene C (2003) The position of the aorta relative to the spine: a comparison of patients with and without idiopathic scoliosis (see comment). J Bone Joint Surg Am 85-A:1461–1469
Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS (1995) Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am 77:1200–1206
Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S (1988) Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement (see comment). Spine 13:1012–1018
Wintermark M, Mouhsine E, Theumann N, Mordasini P, van Melle G, Leyvraz PF, Schnyder P (2003) Thoracolumbar spine fractures in patients who have sustained severe trauma: depiction with multi-detector row CT. Radiology 227:681–689
Xu R, Ebraheim NA, Ou Y, Yeasting RA (1998) Anatomic considerations of pedicle screw placement in the thoracic spine. Roy-Camille technique versus open-lamina technique. Spine 23(9):1065–1068
Xu R, Ebraheim NA, Shepherd ME, Yeasting RA (1999) Thoracic pedicle screw placement guided by computed tomographic measurements. J Spinal Disord 12(3):222–226
Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM (2001) Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery 48(4):771–778 (discussion 778–779)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schizas, C., Theumann, N. & Kosmopoulos, V. Inserting pedicle screws in the upper thoracic spine without the use of fluoroscopy or image guidance. Is it safe?. Eur Spine J 16, 625–629 (2007). https://doi.org/10.1007/s00586-006-0262-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-006-0262-1