Abstract
Introduction
The long treatment duration of distraction osteogenesis (DO) usually causes some complications such as re-fracture, non-union. We have previously demonstrated that the combined use of biomaterial with distraction osteogenesis technique can enhance bone formation and consolidation. This study further tested whether the use of biological agents such as rhBMP-2 or alendronate together with biomaterials in DO will further promote bone formation.
Methods
A 1.0-cm tibial shaft was removed in the left tibia of 30 rabbits. The 1.0-cm defect gap was reduced to 0.5 cm and the remaining 0.5-cm defect gap was filled with 0.5-cm restorable hydroxyapatite/tri-calcium phosphates (HA/TCP) cylindrical block. The animals were divided into three groups with the following added on the HA/TCP block: Group A 50 μl of saline, Group B 75 μg rhBMP-2 in 50 μl of saline, Group C 250 μg alendronate in 50 μl saline. The tibia was then fixed with unilateral lengthener and lengthening started 7 days after at a rate of 1.0 mm/day for 5 days. All animals were terminated at day 37 following surgery. The excised bone specimens were subject to micro-CT, mechanical testing and histological examinations.
Results
Bone mineral density and content were significantly higher in Groups A and B compared to Group C and the mechanical properties of the regenerates in Group B were highest. Micro-CT and histological examinations also confirmed that the regenerates in Group B had the most advanced bone formation, consolidation and remodeling comparing to other groups.
Conclusion
The combined use of rhBMP-2 with HA-TCP biomaterial in DO has significantly enhanced bone formation and consolidation than using the HA-TCP biomaterials alone, whereas the use of alendronate has inhibitory effects on bone formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Induction of osteogenesis through distraction osteogenesis (DO) technique has been widely used in the management of bone defects [1]. However, the time for bone formation and consolidation phase is usually long during DO treatments, complications such as re-fracture, non-union, infection of pin holes may result [2, 3]. It is desirable to significantly reduce the treatment duration of distraction osteogenesis by enhancing bone formation and consolidation. One solution is to use bone substitutes to reduce the bone defect and then apply the DO treatment, taken the advantage of bone conductive prosperities of the biomaterials and the biological enhancement of bone formation and angiogenesis of DO technique. We have previously demonstrated that the use of restorable porous hydroxyapatite and tri-calcium phosphates cylindrical block (HA/TCP block) together with DO can significantly enhance bone formation, consolidation and biomaterial remodeling for the management of bone defect [4].
The other possible solution is to use biological agent to promote bone formation during DO. Since Urist [5] made the key discovery that demineralized bone matrices contain bone morphogenetic proteins (BMPs), it revolutionized skeletal tissue engineering. Among the BMPs, BMP-2 has been found to have pleiotropic functions that range from extraskeletal osteogenesis to bone regeneration [6]. BMP-2 acts primarily as a differentiation factor for bone and cartilage precursor cells, and has been shown to induce bone formation and heal bony defects in a variety of preclinical models [7, 8]. We have also previously demonstrated that administration of rhBMP-2 during distraction osteogenesis can significantly improve bone formation, consolidation and remodeling [9].
Anti-resportive agent such as alendronate (ALN) has been widely used for the treatment of osteoporosis. Some studies also demonstrated that the use of ALN before or during fracture healing, or both, resulted in no adverse effects on the rate of fracture healing, union or strength [9, 10]. The use of ALN during DO may have the advantage of enhance bone consolidation. Further to our previous findings, this study tested the hypothesis that the use of biological agents such as rhBMP-2 or ALN together with HA-TCP biomaterials in distraction osteogenesis (DO) may further promote bone formation and consolidation than using HA-TCP biomaterials alone.
Materials and methods
Animal model of distraction osteogenesis and experimental groups
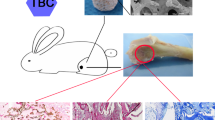
All animal experimental procedures were performed under the guidelines for animal scientific procedures approved by the host institution’s ethical committee. Mid-tibial osteotomies were performed in 30 adult male NZW rabbits (age 20–24 weeks, body weight 2.3–2.8 kg), with the tibiae stabilized by external fixators as previously described [11–13]. In brief, under general anesthesia osteotomy was made by a hand saw in the left tibia below the tibiofibular junction, and a 1.0-cm tibial shaft was removed through a second osteotomy. The 1.0-cm defect gap was immediately reduced to 0.5 cm, with tibia shortened for 0.5 cm and the remaining 0.5-cm defect gap was filled with 0.5 cm (length) × 0.5 cm (diameter) restorable porous hydroxyapatite/tri-calcium phosphates (HA/TCP) cylindrical block (OsteoStim™, Millenium Biologix Inc, Kingston, ON, Canada) and the bone was stabilized by an unilateral fixator (Orthofix M-100, Orthofix, UK). The OsteoStim™ biomaterials consist of approximately 70% Silicon-TCP and 30% HA/TCP, with more than 70% porosity.
The animals were divided into three groups (N = 10 in each group), with the following agents added on the HA-TCP block: Group A 50 μl saline, Group B 75 μg rhBMP-2 (Wyeth Pharmaceuticals, USA) in 50 μl of saline, Group C 250 μg Alendronate (Merck, Rahway, NJ, USA) in 50 μl saline. All the HA-TCP blocks were placed in a sterilized plastic tube, and allowed to soak with the added solutions for 30 min prior to use.
Lengthening started 7 days after the osteotomy, at a rate of 1.0 mm/day, in two steps, for 5 days. Once the lengthening (0.5 cm) was achieved, the regenerate was allowed to consolidate for further 25 days. All animals were terminated at day 37 following initial surgery, and all animal experimental group details were summarized in Table 1.
Radiographic examination
Serial radiographs were taken at the day of surgery (day 0), day 12, day 17, day 27, day 37 (termination point), using a C-arm fluoroscopic machine. The exposure condition was 32 KV, 10 ms at 1× magnifications.
Micro-CT imaging
Specimens of the experimental tibiae including the bone defect gap containing HA-TCP block and 0.5 cm adjacent intact bone at both ends were subject to micro-CT examinations using a micro-CT system (GE Healthcare Explore Locus; MicroView v2.1 software ABA, UK) before processing for mechanical testing. For CT scanning, samples were placed in a sample holder with specimen’s flat anterior surface facing downward. This sample orientation allows for longitudinal scanning of the single specimen. A control file, or measurement protocol was created to define scanning parameters such as source energy, sample size, and image resolution. Parameters selected for this study included a source voltage of 80 kV and 450 mA. Sample measurements (scans) were performed on the samples using high resolution settings. The regenerate bone in the 1-cm distraction gap was chosen as the region of interest (Voxel size: 0.041 × 0.041 × 0.041, ROI type: box). The 3D reconstruction of the distraction gap was performed by 45 mm-resolution using the software provided. For data analysis, the following parameters were used to generate reports: mean volumetric bone mineral density (BMD), bone mineral content (BMC), tissue mineral content (TMC), bone volume (BV), tissue volume (TV), trabeculae thickness (Calib.Tb.Th.3D), and trabeculae space (Calib.Tb.Sp.3D).
Mechanical testing
Mechanical testing was performed on eight samples from each group after the micro-CT examination. Torsional test was performed on a MTS 858 Mini BionixRll testing machine at room temperature (22°C) using a customer designed jig. The rotation angle was applied at a rate of 4.5°/s and the torque and angular displacement was measured by the in-built devices and recorded. The biomechanical properties of specimens were determined by the maximum torque, torsional stiffness, and the maximum angular displacement required to failure of specimens.
Histological examination
The samples were fixed in 10% buffered formalin for 48 hours and decalcified at 4°C over a period of 4 weeks in 14% EDTA in 0.1 M Tris–HCl buffer, pH 7.2. All samples were then processed through graded alcohols, xylene and embedded longitudinally (on their coronal plane) in paraffin wax. 7 μm sections are cut at and stained with routine hematoxylin and eosin (HE) and Alcian blue/Sirius red. Alcian blue/Sirius red staining, following de-paraffin, re-hydration, nuclear staining with Weigert’s hematoxylin, sections are stained with Alcian blue 8GX (0.1% in 1% acetic acid) and Sirius red F3B (1% in saturated picric acid). Alcian blue stains the proteoglycan-rich cartilage matrix (blue), while Sirius red stains the type I collagen fibril (red).
Statistical analysis
All quantitative data from micro-CT examination and mechanical testing were transferred to statistical spreadsheets and analyzed using a commercially available statistical program SAS (Version 9.0). Data from each age group were first tested by one-way ANOVA to identify significant difference between the groups. If a significant difference (p < 0.05) was found, multiple comparisons were performed using SNK-q (Student–Newman–keuls) test. Difference is considered significant at p < 0.05 in all tests.
Results
General observations
At the first 2 weeks post-operation, all the skin incision wounds healed with no sign of pin site infection, swelling and suppuration. During the last 3 weeks post-operation, no apparent difference was noticed in animals in all groups. There were total six animals had pin-hole fracture and they were terminated and replaced by new animals.
Radiographic evaluations of the regenerates
The average (mean ± SD) lengthening of all the animals was 9.6 ± 0.5 mm. There was no much difference on X-ray before day 12 among the three groups. The bone formation was more obvious at day 17 in group B compared to groups A and C. At day 27 and day 37 post-surgery, radiographs show that there was more bone formation in the groups A and B than that in groups C, more bone was seen in group B. Radiolucent regions representing focal defects in the distraction regenerates were frequently seen in group C at day 37. There is also a small focal defect in the conjunction of bone and regenerates of group A (Fig. 1). Among the three groups, bony union of the distraction gap was seen in group B as early as day 17; and at day 27 there were radiographic signs of cortical continuity and the HA/TCP block was less visible in group B compared to groups A and C (Fig. 1).
Representative radiographs of all experimental groups at day 0, 12, 17, 27 and 37 post-surgery. Day 0 The 1.0-cm defect gap was reduced with the tibia shortened for 0.5 cm, and the remaining 0.5 cm defect gap was filled with 0.5-cm restorable porous HA/TCP cylindrical block in the three groups. Day 12 The 0.5 cm lengthening has just completed, there was little difference on the radiographs among the three groups. Day 17 There appeared to be increase in callus formation in group B compared to the other two groups. Day 27 There was visible increase in callus formation in groups A and B compared to day 17. Group B had more callus formation than group A and callus formation in group C was very small. Day 37 All animals were terminated at this point. There was a continuous increase in callus formation in groups A and B comparing to day 27, and all distraction gaps were filled with new bone in groups A and B. The radiographic sign of cortical continuity was only seen in group B, indicating the best bone quality compared to groups A and C. In group C, large areas of bone defects were still visible
Micro-CT images and data
Micro-CT images of the distraction gap tissues demonstrated enhanced bone formation in group A and B. Group B had better bone remodeling than group A, the new cortical bones have clearly formed at day 37 (Fig. 2B1). The newly formed bone was more evenly distributed across the distraction gap in group B compared to groups A and C (Fig. 2A1–C1). In group C, the newly formed bone was scarce comparing to that in groups A and B, with focal bone defects. In group A and C, HA/TCP biomaterials were still clearly visible, whereas in group B, the HA/TCP biomaterial and new bone have been remodeled and the cortical bone modeling was almost completed (Fig. 2B1–3). However, in group C, larger focal defects were frequently seen and the new bone formation was very poor in the distraction gap (Fig. 2C1–3).
Representative micro-CT images of the entire regenerates were shown. The far left panel A–B–C shows the representative radiographs of the regenerates of the three groups at day 37 post-surgery. The panel A1–B1–C1 shows the longitudinal CT scans of the corresponding specimens boxed in the A–B–C panel. The panel A2–B2–C2 was 3D micro-CT reconstruction images of the same specimens as panel A1–B1–C1. The panel A3–B3–C3 was the corresponding cross-sectional images of the boxed areas in panel A2–B2–C2. In group A, there was still a little focal defect in the regenerate and the HA/TCP block was clearly evident in the gap (A, A1, A2, A3), there was sign of new bone formation into the HA/TCP biomaterials. In group B, the quality of newly formed bone was much superior compared to group A, the callus was evenly distributed in the distraction gap and grown into the HA/TCP biomaterials with clear signs of bone and biomaterial remodeling, new corticalization and the HA/TCP block has been almost resorbed (B, B1, B2, B3). In group C, the bone formation was rather poor at this stage, with frequent focal defects and only small amounts of bone formation was seen at the proximal end of the tibial osteotomy end, there were larger areas of HT/TCP and no sign of new bone formation into the HA/TCP biomaterials, nor HT/TCP being resorbed (C, C1, C2, and C3)
The quantitative micro-CT measurement results are summarized in Table 2. The mean volumetric BMD and the mean volumetric BMC of the regenerates was significantly higher in groups A and B compared to group C (p < 0.0001). The mean volumetric TMD and the mean volumetric TMC of the regenerates was also significantly higher in groups A and B compared to group C (p < 0.0001). There was no significant difference between groups A and B (p > 0.05). The BV/TV ratio was higher in groups A and B compared to group C (p < 0.05), and there was no difference between groups A and B.
Mechanical testing results
All mechanical testing results are also summarized in Table 2. There was no significant difference in the maximum rotation angle for failure among the groups A and B, and the maximum rotation angle in groups A and B were significantly higher than that of the group C. The maximum torque and the torsional stiffness was significantly higher in group B compared to groups A and C (p < 0.05); and the group A was higher than the group C (p < 0.05).
Histology results
At day 37 following surgery, the regenerates in groups A and B were mainly consisted of woven bone with only small areas of HA/TCP residues (Fig. 3A, B), whereas in group C the new bone only formed in the peripherals of the HA/TCP and not fully consolidated with large areas of HA/TCP in the middle of the regenerate (Fig. 3C). In groups A and B, the new bone was formed in parallel to the distraction force in the gap and grow into the HA/TCP biomaterials (Fig. 3A1, B1). In group B, the callus was evenly formed in the distraction gap and the regenerates had more signs of bone remodeling, only small areas of HA/TCP residues in the regenerates were seen comparing to group A (Fig. 3A, B). In group C, focal defects with larger areas of HA/TCP residues were frequently seen (Fig. 3C). In comparison, bone consolidation and remodeling was most advanced in group B as the regenerates were completely united with well-organized woven bone with little HA/TCP residues, whereas new callus formation was still going on with some sign of bone remodeling in group B; focal bone defects and larger areas of HA/TCP residues were still visible in group C.
Representatives of histological sections of the regenerates from the three experimental groups are shown. A In group A, the regenerate was mainly consisted of newly formed woven bone, but the bone formation was not evenly distributed among the gap, with a larger amount of HA/TCP blocks were still visible (arrows). A1 Boxed area in A, showing sign of new bone formation into the HA/TCP biomaterials. B In group B, the newly formed callus was in parallel to the distraction force and evenly distributed throughout the gap; there were signs of callus remodeling and new cortical bone formation and remodeling, only small amounts of HA/TCP residues (arrows) were seen, and it is hard to distinguish the HA/TCP residues and newly formed bone at this stage (B1, boxed area of B). C In group C, the amount of callus formed was the least among the three groups and HA/TCP block was clearly visible (arrows), there was no sign of any new bone formation into the HA/TCP biomaterials (C1, boxed area in C), only small amount of callus formed along the surfaces of HA/TCP. A–C Sirius red/Alcian blue staining; original magnification ×25; A1–C1 ×100
Discussion
We have previously shown that the combined use of HA/TCP biomaterials and DO technique could reduce the treatment time and enhance bone consolidation compared to the established treatment methods, such as using DO technique or biomaterials alone [4]. This study further tested the effects if HA/TCP block combined with rhBMP-2 or alendronate in DO. The data suggested that HA-TCP combined with a single dose of rhBMP-2 (75 μg) in DO significantly enhanced the bone formation and remodeling than the use of HA-TCP alone, whereas the use of ALN with HA-TCP in DO has significantly inhibited bone formation.
A rabbit model of 1-cm tibial bone defect was used, and the three groups (HA/TCP; HA/TCP + rhBMP-2; HA/TCP + ALN) had the same duration for consolidation following surgery and DO management. Micro-CT, mechanical testing and histological examination data indicated that overall quality of newly formed bone in the HA/TCP + rhBMP-2 group was significantly improved compared to the HA/TCP and HA/TCP + ALN groups. The torsional test is the golden standard for determining the functional quality of the regenerates in DO. HA/TCP + rhBMP-2 group had the higher maximum torque and torsional stiffness than those of HA/TCP and HA/TCP + ALN groups, suggesting that the regenerate quality was the best in the HA/TCP + rhBMP-2 group. The micro CT and histology results also demonstrated that bone remodeling was almost completed in HA/TCP + rhBMP-2 group. The finding was consistent with our previous work, that administration of a single dose of rhBMP-2 (75 μg) significantly enhanced the bone consolidation during distraction osteogenesis in rabbit [9]. Watanabe et al. [14] also reported that during bone transport, HA biomaterial loaded with rhBMP-2 was capable of promoting bone formation.
BMP-2 induced bone formation in vivo is clearly a complex multistage process and likely involves the activities of multiple locally produced growth factors and systemically available hormones. Osteoblastic or osteoprogenitor cells respond to BMP-2 by increasing cell proliferation [15]. The rhBMP-2 has chemotactic effects on mesenchymal cells, osteoblastic cells and endothelial cells [16], suggesting the enhancement of bone formation by rhBMP-2 may be related to an increase in recruitment of bone-forming cells and enhancement of neovascularization. In the setting of distraction osteogenesis, the regenerate provides a rich source of osteoprogenitor cells and good microenvironment for angiogenesis [11, 17]. The primary effect of rhBMP-2 in this setting is likely to promote differentiation of progenitor cells into osteoblasts and endothelial cells, resulting in rapid bone formation and remodeling as we have observed in the current study.
The HA/TCP + ALN group had the least bone formation and all the results showed that HA/TCP + ALN had inhibited bone formation and remodeling when compared to the HA/TCP alone group. Bisphosphonates are structurally analogous to pyrophosphate, having greater affinity to bone that can rapidly accumulate in bone tissue and induce osteoclast apoptosis during bone resorption process [18]. Alendronate (ALN) has been widely used for the management of osteoporosis. Little et al reported that systemic administration of zoledronic acid significantly increased BMC and strength in rabbit DO [19]. Based on these findings, we hypothesized that application of ALN combined with HA/TCP biomaterial might lead to a greater bone formation during DO. However, the results demonstrated that the mean volumetric BMD, BMC, TMC, TMD and BV/TV of the regenerates were significantly lower in the HA/TCP + ALN group compared to the HA/TCP and HA/TCP + rhBMP-2 groups. The Micro-CT and mechanical testing data also shown that the bone formation remodeling and quality was compromised in the HA/TCP + ALN group in contrast to the other two groups, suggesting that the local administration of ALN with HA/TCP in DO had inhibitory effects on bone formation and biomaterial remodeling. However, since the ALN in this study was administrated locally with the HA/TCP biomaterial, which was different from usual clinical oral administration, the high dose of ALN may cause local toxic effects and this may explain the difference between our study and previous report by Little et al [19]. Further investigations using ALN oral administration and dosage similar to clinical use in this experimental system are needed.
In Greiner’s study [20, 21], they used 20 μg Zoledronic acid (ZOL) in 250 g rat (average dose of 80 μg/kg). In our study, 250 μg alendronate was used in 2.5 kg rabbit (the average dose was 100 μg/kg), which was very close the reported dose. Because the alendronate was soaked into the HA-TCP blocks, and there were some loss as not all the alendronate solution was completely absorbed by the HA-TCP block. So the dosage of alendronate used should be close to 8,080 μg/kg. The ZOL and alendronate were all the third-generation nitrogen-containing bisphosphonate, so that the drug dosage used in this study was chosen accordingly to Greiner’s study, which has demonstrated positive effect on bone healing.
The negative effect seen in our study may be due to the different micro-environment between the bone defect healing model and distraction osteogenesis model. The distraction osteogenesis process can be divided to three phases: distraction phase, consolidation phase, and remodeling phase. The micro-environment of bone defect healing model is close to that of consolidation phase in distraction osteogenesis model. But the presence of bisphosphonates in the distraction phase may have inhibitory effects and cause delayed healing in the later consolidation and remodeling phases.
Recent studies [22, 23] also reported that bisphosphonates might delay repair in stress fractures. So we think that the inhibitory effects of alendronate local application in distraction osteogenesis found in this study were genuine. Of course, arguably there are many possible factors may affect the healing result in distraction osteogenesis model, such as route of administration, other (low) dose of alendronate, etc. that we did not test. Nonetheless, the reported bisphosphonates dose with positive effect on bone healing did not show beneficial effects in our distraction osteogenesis model, hence its clinical application should not be encouraged for distraction osteogensis cases.
In conclusion, we demonstrated that the use of HA/TCP block combined with small dose rhBMP-2 in DO significantly enhance new bone formation and regenerate remodeling, hence reduced treatment duration. The newly described technique may be applied clinically for the management of larger bone defects caused by trauma, bone infection, and bone tumors surgeries.
References
Moseley CF (1989) Leg lengthening. A. review of 30 years. Clin Orthop 247:38–43
Dahl MT, Gulli B, Berg T (1994) Complications of limb lengthening. A learning curve. Clin Orthop 301:10–18
Garcia CE, Olsen B, Ruiz Yague M et al (1992) Ilizarov technique: results and difficulties. Clin Orthop 283:116–123
Wang Y, Ni M, Tang PF et al (2009) Novel application of HA-TCP biomaterials in distraction osteogenesis shortened the lengthening time and promoted bone consolidation. J Orthop Res 27:477–482. doi:10.1002/jor.20782
Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899
Sakou T (1998) Bone morphogenetic proteins: from basic studies to clinical approaches. Bone 22:591–603. doi:10.1016/S8756-3282(98)00053-2
Welch RD, Jones AL, Bucholz RW et al (1998) Effect of recombinant human bone morphogenetic protein-2 on fracture healing in a goat tibial fracture model. J Bone Miner Res 13:1483–1490. doi:10.1359/jbmr.1998.13.9.1483
Yudell RM, Block MS (2000) Bone gap healing in the dog using recombinant human bone morphogenetic protein-2. J Oral Maxillofac Surg 58:761–766. doi:10.1053/joms.2000.7261
Li G, Bouxsein ML, Luppen C et al (2002) Bone consolidation is enhanced by rhBMP-2 in a rabbit model of distraction osteogenesis. J Orthop Res 20:779–788. doi:10.1016/S0736-0266(01)00166-8
Peter CP, Cook WO, Nunamaker DM et al (1996) Effect of alendronate on fracture healing and bone remodeling in dogs. J Orthop Res 14:74–79. doi:10.1002/jor.1100140113
Li G, Simpson AHRW, Kenwright J et al (1999) Effect of lengthening rate on angiogenesis during distraction osteogenesis. J Orthop Res 17:362–367. doi:10.1002/jor.1100170310
Li G, Simpson AHRW, Kenwright J et al (1997) Assessment of cell proliferation in regenerating bone during distraction osteogenesis at different distraction rates. J Orthop Res 15:765–772. doi:10.1002/jor.1100150520
Wang Y, Wan C, Szoke G et al (2008) Local injection of thrombin-related peptide (TP508) in PPF/PLGA microparticles enhanced bone formation during distraction osteogenesis. J Orthop Res 26:539–546. doi:10.1002/jor.20495
Watanabe K, Tsuchiya H, Sakurakichi K et al (2007) Bone transport using hydroxyapatite loaded with bone morphogenetic protein in rabbits. J Bone Joint Surg Br 89:1122–1129. doi:10.1302/0301-620X.89B8.19003
Yamaguchi A, Katagiri T, Ikeda T et al (1991) Recombinant human bone morphogenetic protein-2 stimulates osteoblastic maturation and inhibits myogenic differentiation in vitro. J Cell Biol 113:681–687
Li G, Cui Y, Mcllmurray L et al (2005) rhBMP-2, rhVEGF(165), rhPTN and thrombin-related peptide, TP508 induce chemotaxis of human osteoblasts and microvascular endothelial cells. J Orthop Res 23:680–685
Li G (2004) New developments and insights learned from distraction osteogenesis. Curr Opin Orthop 15:325–330
Bergstrom JD, Bostedor RG, Masarachia PJ (2000) Alendronate is a specific, nanomolar inhibitor of farnesyl diphosphate synthase. Arch Biochem Biophys 373:231–241
Little DG, Smith NC, Williams PR et al (2003) Zoledronic acid prevents osteopenia and increases bone strength in a rabbit model of distraction osteogenesis. J Bone Miner Res 18:1300–1307. doi:10.1359/jbmr.2003.18.7.1300
Greiner SH, Wildemann B, Back DA, Alidoust M, Schwabe P, Haas NP, Schmidmaier G (2008) Local application of zoledronic acid incorporated in a poly(d, l-lactide)-coated implant accelerates fracture healing in rats. Acta Orthop 79(5):717–725
Greiner S, Kadow-Romacker A, Wildemann B, Schwabe P, Schmidmaier G (2007) Bisphosphonates incorporated in a poly(d, l-lactide) implant coating inhibit osteoclast like cells in vitro. J Biomed Mater Res 83(4):1184–1191
Sloan AV, Martin JR, Li S et al (2010) Parathyroid hormone and bisphosphonate have opposite effects on stress fracture repair. Bone 47(2):235–240. doi:10.1016/j.bone.2010.05.015
Matos MA, Tannuri U, Guarniero R et al (2010) The effect of zoledronate during bone healing. J Orthop Traumatol 11(1):7–12. doi:10.1007/s10195-010-0083-1
Acknowledgments
We thank Mr. Jason Hendry, Millenium Biologix Corporation, Kingston, Canada for providing the cylindrical Skelite™ scaffolds for this study.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ni, M., Li, G., Tang, PF. et al. rhBMP-2 not alendronate combined with HA-TCP biomaterial and distraction osteogenesis enhance bone formation. Arch Orthop Trauma Surg 131, 1469–1476 (2011). https://doi.org/10.1007/s00402-011-1357-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1357-7