Abstract
Distraction osteogenesis (DO) is used to treat specific disorders associated with growth abnormalities and/or loss of bone stock secondary to trauma or disease. However, a high rate of complications and discomfort hamper its further application in clinical practice. Here, we investigated the effects of all-trans retinoic acid (ATRA) on osteogenic differentiation of rat bone marrow-derived mesenchymal stem cells (rBMSCs) and bone consolidation in a rat DO model. Different doses of ATRA were used to treat rBMSCs. Cell viability and osteogenic differentiation were assessed using CCK-8 and alkaline phosphatase staining, respectively. The mRNA expression of osteogenic differentiation-genes (including ALP, Runx2, OCN, OPN, OSX, and BMP2) and angiogenic genes (including VEGF, HIF-1, FLK-2, ANG-2, and ANG-4) were determined by quantitative real-time PCR analysis. Further, we locally injected ATRA or PBS into the gap in the rat DO model every 3 days until termination. X-rays, micro-computed tomography (Micro-CT), mechanical testing, and immunohistochemistry stains were used to evaluate the quality of the regenerates. ATRA promoted osteogenic differentiation of rBMSCs. Moreover, ATRA elevated the mRNA expression levels of osteogenic differentiation-genes and angiogenic genes. In the rat model, new bone properties of bone volume/total tissue volume and mechanical strength were significantly higher in the ATRA-treatment group. Micro-CT examination showed more mineralized bone after the ATRA-treatment, and immunohistochemistry demonstrated more new bone formation after ATRA-treatment than that in the PBS group. In conclusion, as a readily available and very cost effective bio-source, ATRA may be a novel therapeutic method to enhance bone consolidation in the clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distraction osteogenesis (DO) is a reconstructive technique that repairs bone defects and corrects osseous deformities by applying controlled gradual traction between the osteotomy cuts [1]. DO consists of three phases: the latency phase, the distraction phase, and the consolidation phase [2]. Although this technique has been used to treat orthopedic disorders [3], the main disadvantages, including a prolonged consolidation of distracted bone, secondary surgical intervention, and limitation of morphological correction, have hampered its further application in clinical practice [4, 5]. Therefore, novel and effective approaches are urgently needed to accelerate bone regeneration during the DO process.
Recently, mesenchymal stem cells (MSCs), a subset of perivascular cells that reside in particular microenvironments, have become available for enhancing angiogenesis, reducing inflammation, and promoting tissue repair by producing the secretome in damaged tissue [6,7,8]. However, poor differentiation and survival rates after MSC transplantation limit their suitability for cell therapy and tissue regeneration [9, 10]. It is well documented that the proliferation and differentiation of osteoblasts derived from MSCs in adjacent bone marrow can result in bone regeneration after DO treatment [11, 12]. Thus, a better understanding of the osteogenesis produced by MSCs may allow us to shorten the treatment periods needed for patients with DO and reduce the incidence of clinical complications.
As an active metabolite of dietary vitamin A, all-trans retinoic acid (ATRA) participates in the regulation of cell proliferation, differentiation, migration, and various biological processes [13,14,15]. Its receptors belong to the nuclear receptor superfamily, including retinoic acid receptors (RARs) and retinoid X receptors (RXRs), of which RARs have the major bioactive effects [13,14,15]. The previous studies found that ATRA could promote favorable geometric remodeling of the rat carotid artery after balloon withdrawal injury and induce tissue factor in cultured human endothelial cells exposed to tumor necrosis factor [16,17,18]. Additionally, Zhang et al. reported that ATRA played a synergistic role in MSC osteogenic differentiation, and retinoic acid signaling pathways may be therapeutic targets in bone diseases [19]. Moreover, ATRA could significantly enhance the activity of alkaline phosphatase of BMSCs [20] as well as inhibit the growth of osteosarcoma (OS) tumors by promoting osteogenic differentiation in OS cells [21]. Combining insights from all these studies, we hypothesized that ATRA could promote bone formation and thus have the potential to be an effective therapeutic agent to stimulate bone regeneration in patients with DO.
In the present study, we investigated the effects of ATRA on osteogenic differentiation of rat bone marrow-derived MSCs (rBMSCs) and bone consolidation in a rat DO model. To the best of our knowledge, this study is the first to investigate the effect of ATRA on DO. Our findings thus might provide insights for developing a new therapy for bone regeneration.
Materials and Methods
Animals
Based on the previous study [22], twenty 12-week-old Sprague–Dawley (SD) male rats (410 ± 15 g) were selected, which were provided by the Laboratory Animal Research Centre of the SLAC Laboratory Animal Corporation (Shanghai, China).
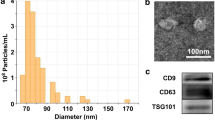
Isolation and Culture of rBMSCs
The rBMSCs were isolated from the bone marrow of 4-week-old SD male rats as previously described [23]. In brief, the rats were euthanized via intracardiac injection of 100-mg sodium pentobarbitone and it was confirmed by decapitation. To obtain mononuclear cells (MNCs), the rat bone marrow was flushed from the tibia and processed by density gradient centrifugation over Lymphoprep™ 1.077 g/mL (Axis-Shield, Alere Technologies, Oslo, Norway). Then the MNCs were cultured in complete Modified Eagle’s Medium Alpha (α-MEM) (Invitrogen, Thermo Fisher Scientific, Waltham, MA, USA), 10% fetal bovine serum, and 2 mM l-glutamine (Invitrogen) at 37 °C with 5% CO2. When the cells were confluent, they were treated with trypsin and re-plated for expansion and further examination. The rBMSCs between passages three and six were used in the experiments. The surface antigens of rBMSCs including CD31, CD34, CD45, and CD90 were detected (BD Biosciences, San Jose, CA, USA) by flow cytometry (data not shown).
Cell Viability Assay
The cell viability was determined by CCK-8 assay. Briefly, the rBMSCs at an initial density of 5000 cells per well were placed in 96-well plates and incubated for 24 h. Then ATRA (Sigma-Aldrich, St. Louis, MO, USA) was added to the medium at different doses (0, 1 µM, 10 µM, 20 µM, or 30 µM). After incubation for 12, 24, 48, or 72 h, respectively, 10 µL CCK-8 reagent was added to each 100 µL of medium (Beyotime, Jiangsu, China) and cells were incubated at 37 °C for 2 h. The absorbance at 450 nm was measured with a microplate reader. All the experiments were repeated at least three times.
Osteogenic Differentiation
After trypsinization, the rBMSCs were seeded in a 12-well plate at a concentration of 5000 cells/cm2 and incubated in the α-MEM at 37 °C. When cell density reached 80% confluence, the medium was replaced with osteogenic induction medium (OIM: α-MEM, 10% FBS, 2 mM l-glutamine, 1 nM dexamethasone, 50 µM l-ascorbic acid-2-phosphate, 20 mM β-glycerophosphate, 100 U/mL penicillin, and 100 µg/mL streptomycin) as a positive control. For in vitro experiments, ATRA at different doses (0, 1 µM, 10 µM, 20 µM, or 30 µM) was added to 3 mL of α-MEM. Finally, α-MEM was used as a negative control.
ALP Staining
After the rBMSCs were treated with OIM and ATRA (at doses of 0, 1, 10, 20, and 30 µM) for 3 days, a detection kit (Yeasen) was used to measure the ALP activity. Briefly, the cells were washed with PBS and fixed with 70% ethanol for 10 min. After equilibration in the ALP buffer for 5 min, the cells were incubated with ALP substrate solution at 37 °C in the dark for 60 min, followed by treatment with distilled water. Finally, the plate was dried and the positive rate of alkaline phosphatase was evaluated.
RNA Extraction and Quantitative Real-Time PCR (qRT-PCR)
After osteogenic induction with ATRA for 3 days, the total cellular RNA was extracted with an RNA Mini Kit (Invitrogen), and reversely transcribed into cDNA with M-MLV reverse transcriptase (Invitrogen) according to the manufacturer’s instructions. Real-time PCR amplification was performed using the Step One Plus Real-Time PCR System (Applied Biosystems, Thermo Fisher Scientific, Waltham, MA, USA) by the following procedure: first at 95 °C for 5 min, and then 40 cycles of 95 °C for 15 s and 60 °C for 60 s. The primer sequences of the osteogenic and angiogenic markers are listed in Table 1. The relative quantification of gene expression was analyzed with the values of \({2^{ - \Delta \Delta {C_{\text{t}}}}}\), and normalized by GAPDH expression level.
Animal Surgery
Twenty 12-week-old SD male rats were used for the in vivo experiments. Initially, five rats were housed in each cage, and then were placed under general anesthesia using intraperitoneal injections of sodium pentobarbital (initially 50 mg/kg, followed by maintenance doses of 0.1 mL or 9 mg/kg, i.v., as required) for the surgery. The surgical site was shaved and cleaned with a 0.5% iodophor-in-alcohol solution, and then isolated with sterile drapes. Then 1% lidocaine/epinephrine 1:105 was used for local infiltration to produce local vasoconstriction. For the duration of the experimental protocol, anesthesia was maintained, and all of the animals were subjected to a right tibial transverse osteotomy procedure with a closed fracture near the fibular–tibial junction under sterile and analgesic condition which was created by subcutaneous injection of enrofloxacin (50 mg/mL, 10 mg/kg) and buprenorphine (0.03 mg/mL, 0.05 mg/kg) 1 h before the procedure. The details of the transverse osteotomy procedure were as follows:
The right knee joint and ankle joint were fixed by hand, and the overlying skin was incised and retracted. To expose the facies medialis of the tibia, a 1–2-cm longitudinal incision was made along medial tissues overlying tibia, starting 0.5 cm below the knee joint. Then the superficial fascia was bluntly dissected, and the muscle tissues were gently separated from the intermuscular space. When the tibia was exposed, a 1.0-mm dental drill (at low rotation) was used to create four paralleled anchor wells perpendicular to medial tibia for fixation. After the screws were rotated into place, a distraction fixator (Xinzhong Company, China) was fixed with them. The tibia was cut off between the second and third screws, and finally, the wound was flushed with normal saline and the wound site was sealed in layers.
Six hours after the surgery, the rats were subcutaneously injected again with buprenorphine (0.05 mg/kg) to ensure post-operative analgesia. For the first five post-operative days, the subcutaneous buprenorphine injections (0.05 mg/kg) were performed twice a day for analgesia, and enrofloxacin (5 mg/kg) was injected once a day to prevent bacterial wound infections. The rats were randomized into two groups: a PBS group (n = 10) subjected to DO with PBS injections, and an ATRA group (n = 10) subjected to DO with ATRA injections. All rats were free to move in the cage and allowed to eat and drink ad libitum.
DO Protocol
Rat distraction was performed as previously reported [22, 24]. The distraction was performed in three phases, including latency phase of 5 days, 10-day active distraction phase (1 mm/day, in two equal increments), and a consolidation phase of 6 weeks. In the first two phases, the rats were monitored twice a day, and during the last phase, they were observed once a day, to evaluate the effectiveness of the analgesia. The procedure was modified by providing an appropriate amount of subcutaneous buprenorphine treatment according to the behavioral signs of each animal. From the beginning of the consolidation phase, the two groups received injections of PBS (100 µL) and ATRA (10 µM, 100 µL), respectively, into the distraction gap every 3 days until termination of the experiment. In order to minimize the incidence of infections, pin site care was performed including twice-daily cleaning and dressing with an external fixator for the entire length of the treatment. None of the animals became severely ill or died at any time prior to the planned endpoint of the experiments. Bilateral tibias and bone tissues were harvested from the distraction gap, and processed for further study.
Digital Radiographs
At the end of the 10-day active distraction phase, the distraction zone had been monitored by weekly X-rays until termination using a digital X-ray machine (MX-20, Faxitron X-Ray Corp., Wheeling, IL, USA) under a voltage of 32 kV and an exposure time of 6000 MS.
Micro-computer Tomography (Micro-CT/µCT) Examination
Micro-computed tomography (Micro-CT) analysis was performed after euthanasia to quantitatively assess structural changes within the distraction zone for each animal. Briefly, all the specimens were imaged with a high-solution µCT (µCT40, Scanco Medical, Bassersdorf, Switzerland) equipped with a 10-mm focal-spot microfocus X-ray tube. The entire region of the surgical defect was scanned at a 34-µ misotropic voxel size, a voltage of 70 keV, a current of 114 µA, at a 10.5-µm isotropic resolution, and an integration time of 250 ms. Three dimensional (3D) reconstructions of mineralized callus were performed using the central 150 layers in the horizontal plane of the distraction bone as the region of interest to eliminate the interference. According to different thresholds (low attenuation = 158, high attenuation = 211) based on the established protocol [25], low- and high-density mineralized tissues were reconstructed. The high-density tissues (211–1000 threshold) formed the newly highly mineralized bone, while the lower density sites (158–211 threshold) represented the newly formed callus. Bone volume (BV) and tissue volume (TV) were recorded. The percentage of BV/TV of each specimen, which was the ratio of the segmented bone volume to the total volume of the region of interest, was determined [26].
Four-Point Bending Mechanical Testing
Mechanical testing was performed 6 weeks after distraction. Specimens were harvested within 24 h after termination. A four-point bending device (H25KS; Hounsfield Test Equipment Ltd, Salfords, UK) with a 250 N load cell and a constant displacement rate of 5 mm/min was used to test the distracted tibiae to failure. The tibiae were loaded in the anterior–posterior direction with the posterior side in tension. The inner and outer span of the blades was 8 and 20 mm, respectively, with the long axis of tibia placed perpendicular to the blades during the test. The contralateral tibia was tested as an internal control. The modulus of elasticity (E-modulus), ultimate load, and energy to failure were recorded and analyzed using built-in software (QMAT Professional; Tinius Olsen, Inc., Horsham, PA, USA).
Immunohistochemistry
Immunohistochemistry staining was performed using a standard protocol as previously reported [27]. Paraffin sections were incubated with primary antibodies against OSX (1:100, ab22552, Abcam, Cambridge, MA, USA) and OCN (1:100, sc30045, Santa Cruz, USA) overnight at 4 °C, followed by incubation with horseradish peroxidase-conjugated secondary antibodies. After counterstaining with hematoxylin, the positive stained cell numbers and area in the whole distraction zone per specimen were counted and compared, which were expressed as the percentages of the bone volume. Before immunohistochemical staining, the specificity of the antibodies was confirmed through negative controls (stained with only secondary antibodies) and positive controls (stained with both primary and secondary antibodies) in bone trabecula or ossification zone of cartilage in healthy knee joint of rats.
Statistical Analysis
All quantitative data were analyzed using SPSS 18.0 software (SPSS, Chicago, IL, USA) for MS Windows. Experimental data were presented as the mean ± SD. One-way analysis of variance was used to measure the significance of comparisons between groups. The analyses were performed by the researchers who were blinded to the grouping. A p value of less than 0.05 was regarded as statistically significant.
Results
Different Doses of ATRA Had No Effect on Cell Viability but Promoted Osteogenic Differentiation of rBMSCs
To elucidate the biological effect of ATRA in bone consolidation in DO, we first compared cell viability of rBMSCs cultured in different doses of ATRA using the CCK-8 assay. As shown in Fig. 1a, compared to the untreated controls (0 µM), 48-h, and 72-h cultures with ATRA significantly decreased cell viability (p < 0.05 and < 0.01 at 48 h and 72 h, respectively), but there was no significant difference among the four ATRA-treatment groups with doses varying between 1 and 30 µM. Next, we investigated the effect of different doses of ATRA on the osteogenesis of rBMSCs in vitro by performing ALP staining. There was an apparent increase in ALP staining after exposure to 10 µM ATRA (Fig. 1b) and this effect was subsequently confirmed through quantitative analysis (Fig. 1c). More importantly, quantitative analysis revealed that the ALP activity was highest in the 10 µM group than in the groups with other doses (Fig. 1c). Thus, 10 µM ATRA was selected for the following analysis.
Effects of different doses of ATRA on cell viability and osteogenic differentiation of rBMSCs. a Cell viability was evaluated by the CCK-8 assay. b ALP staining of rBMSCs treated with different doses of ATRA for 3 days, c ALP quantitative assay of rBMSCs treated with different doses of ATRA. Data are presented as the mean value ± SD from triplicate experiments
ATRA Regulated the Expression of Osteogenic and Angiogenic Genes During Osteogenic Differentiation of rBMSCs
It has been reported that angiogenesis and osteogenesis play important roles in tissue regeneration and healing in improving DO technique [28]. Therefore, the expression of various osteogenic differentiation-related genes was detected by qRT-PCR. As shown in Fig. 2, the expression levels of ALP, BMP2, OSX, Runx2, OPN, and OCN were significantly increased after osteogenic induction (p < 0.05, p < 0.01, p < 0.001). Notably, ATRA (10 µM) treatment could further enhance these effects in osteogenic differentiation of rBMSCs (p < 0.01, p < 0.001). Furthermore, we found higher expression of VEGF, HIF-1, and FLK-2 was detected for rBMSCs cultured in ATRA, compared with α-MEM medium alone (Fig. 3, p < 0.001). Moreover, 10 µM ATRA could significantly promote the expression of ANG-2 and ANG-4 (Fig. 3, p < 0.001).
Effects of ATRA on the expression of osteogenic genes in osteogenic differentiation of rBMSCs. The genes expression of osteogenesis-related markers was assessed by quantitative real-time PCR after treatment of ATRA after osteogenic induction for 3 days. Data are presented as the mean value ± SD from triplicate experiments. *p < 0.05, **p < 0.01, ***p < 0.001, compared to the α-MEM group; ##p < 0.01, ###p < 0.001, compared to the OIM group
Radiographic Assessment of Distraction Zone
As shown in Fig. 4, a representative series of X-rays across the time-course of DO showed the progression of bone consolidation. We observed little callus formation in the distraction gap immediately after distraction was completed in the PBS and ATRA groups. As time went on, more continuous callus was expected to appear in the ATRA-treatment group compared to the PBS group, especially at the end of the consolidation. However, we could not tell the difference between them through X-ray images. But the homogeneity of the regenerated bone seemed greater and formation of a new cortex was more evident in the ATRA-treatment group than in the PBS group at the end of the protocol. Subsequently, µCT examinations were further used to look for the expected outcome after the treatment. Compared with PBS group, the results demonstrated a higher continuity (5 weeks) and homogeneity (6 weeks) in the ATRA group (Fig. 5a, shown in red dotted line). Moreover, we found the value of BV/TV was significantly increased in 158–1000 and 211–1000 three thresholds after 5 weeks of ATRA-treatment, and in 158–211, 158–1000, and 211–1000 three thresholds after 6 weeks of ATRA-treatment (Fig. 5b, c; p < 0.05), indicating more newly formed mineralized bone was present in the ATRA-treatment group compared to the PBS group.
ATRA administration improved the quality of new callus via µCT analysis and mechanical test. a 3D µCT images of the tibia distraction zone in the two groups after 5 and 6 weeks of treatment. b, c The value of BV/TV after the treatment for 5 and 6 weeks. d Mechanical properties (including E-modulus, ultimate load, and energy to failure) of distraction regenerates. Data are presented as the mean value ± SD from triplicate experiments. *p < 0.05, compared to the PBS group
Mechanical Testing
As shown in Fig. 5d, the four-point bending mechanical testing showed a significant improvement in the E-modulus (p < 0.05), ultimate load (p < 0.05), and energy to failure (p < 0.05), compared to those of the PBS group after they were normalized with respect to the contralateral intact tibiae at the end of the protocol.
Immunohistochemical Analysis
Immunohistochemical staining was performed to further confirm the effects of ATRA on osteogenic differentiation of the rBMSCs. As expected, examination for the osteogenic genes Osx and OCN revealed a significant increase in the amounts of positive osteogenic cells in the distraction gap in the ATRA-treatment group compared to the PBS group (Fig. 6a, b; p < 0.05).
Discussion
Until now, DO has been an effective tool for repair of defects and correction of osseous deformities in the treatment of orthopedic disorders. However, a high rate of complications, including a prolonged consolidation of distracted bone, as well as the need for secondary surgical interventions and limitations in the degree of morphological correction has restricted its application in clinical practice. In the present study, we demonstrated that ATRA may have novel potential in augmenting osteogenic differentiation of rBMSCs and consolidation in DO.
As an anti-proliferative and pro-differentiation factor, the ATRA has been shown to participate in various cellular functions such as differentiation, proliferation, migration, apoptosis, and inflammation [29]. Here, we found that ATRA-treatment promoted osteogenic differentiation of rBMSCs, with increased ALP activity. A related study indicated that MSCs have the ability to differentiate into various specific cell types and promote tissue regeneration [30]. But the poor differentiation and poor survival rate observed following rBMSC transplantation limited their regenerative potential [31]. Thus, ATRA-treatment might be an important new approach to the maintenance of healthy bone tissue by promoting osteogenic differentiation of MSCs. Moreover, we found osteogenesis-related genes, including ALP, Runx2, and BMP2 were all significantly up-regulated following ATRA-treatment. Of those genes, ALP could hydrolyze pyrophosphate and generate inorganic phosphate for the proper mineralization of cartilage and bone [32]. BMP2 further promotes osteogenic differentiation as rBMSCs progressed during osteogenic differentiation [33]. As for Runx2, it has been shown to be essential for osteoblast differentiation and is also involved in the production of bone matrix proteins [34]. In addition, angiogenesis is a basic step in the process of bone regeneration, in that it provides a blood supply and thus benefits the subsequent progress of osteogenesis [35]. As a key angiogenic factor, VEGF could induce recruitment and survival of osteoblasts [36]. Related studies reported that VEGF expression becomes notably reduced in MSCs, during aging and this decrease results in reduced osteoblast differentiation [37, 38]. Additionally, ANGs are other important angiogenic factors that can stimulate angiogenesis [39]. Consistently, our results showed that ATRA enhances the expression of angiogenic genes, including VEGF, ANG-2, and ANG-4, which may support angiogenetic capacity and facilitate bone healing in DO.
More importantly, the ability of ATRA to support bone regeneration was also examined in the rat DO model. The results from the micro-CT assay revealed that there was a significant increase in BV/TV with ATRA-treatment. Furthermore, the mechanical test used to quantify the healing by new bone formation in the distraction zone showed better results in the E-modulus, ultimate load, and energy to failure, demonstrating more callus formation and mineralization in the ATRA-treatment group. This evidence further supports the conclusion that ATRA plays an important role in promoting bone regeneration in the rat DO model.
However, the further development of ATRA for clinical treatment of DO will require considerable effort. The normal physiological level of ATRA is ≤ 10−8 mol/L (that is, on a nanomolar scale), but the effective pharmacological concentration may be also > 10−7 mol/L as in the situation with acute myelocytic leukemia [40,41,42]. Therefore, the results reported in the present study need to be taken with caution and may not reflect normal cell responses. The high doses utilized here may have led to selection or preferential proliferation of a subpopulation of BMSCs, and whether proliferation of that subpopulation in a clinical setting will do benefit or harm to the human body still needs to be elucidated. In addition, ATRA has many side effects when used clinically, such as typical retinoid toxicity, flu-like symptoms, and bleeding problems when administrated p.o. to patients with acute promyelocytic leukemia [43, 44]. As a result, the direct use of ATRA in DO may not be feasible at this time, and it may be necessary for us to conduct further studies of both the efficacy and safety of ATRA administration.
In summary, we concluded that ATRA promotes osteogenic differentiation of rBMSCs and enhances bone formation and consolidation during DO in a rat model. These findings suggest that ATRA, which is readily available and could be very cost effective, might be a potential agent for enhancing bone consolidation during DO treatment in patients with bone defects.
References
Carvalho RS, Einhorn TA, Lehmann W, Edgar C, Al-Yamani A, Apazidis A, Pacicca D, Clemens TL, Gerstenfeld LC (2004) The role of angiogenesis in a murine tibial model of distraction osteogenesis. Bone 34:849–861
Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res 239:263–285
El-Alfy B, El-Mowafi H, El-Moghazy N (2010) Distraction osteogenesis in management of composite bone and soft tissue defects. Int Orthop 34:115–118
Sugawara Y, Uda H, Sarukawa S, Sunaga A (2010) Multidirectional cranial distraction osteogenesis for the treatment of craniosynostosis. Plast Reconstr Surg 126:1691–1698
Abbaspour A, Takahashi M, Sairyo K, Takata S, Yukata K, Inui A, Yasui N (2009) Optimal increase in bone mass by continuous local infusion of alendronate during distraction osteogenesis in rabbits. Bone 44:917–923
Caplan AI, Dennis JE (2006) Mesenchymal stem cells as trophic mediators. J Cell Biochem 98:1076–1084
Timmers L, Lim SK, Arslan F, Armstrong JS, Hoefer IE, Doevendans PA, Piek JJ, El Oakley RM, Choo A, Lee CN, Pasterkamp G, de Kleijn DP (2007) Reduction of myocardial infarct size by human mesenchymal stem cell conditioned medium. Stem Cell Res 1:129–137
Yamagata M, Yamamoto A, Kako E, Kaneko N, Matsubara K, Sakai K, Sawamoto K, Ueda M (2013) Human dental pulp-derived stem cells protect against hypoxic-ischemic brain injury in neonatal mice. Stroke 44:551–554
Kotobuki N, Katsube Y, Katou Y, Tadokoro M, Hirose M, Ohgushi H (2008) In vivo survival and osteogenic differentiation of allogeneic rat bone marrow mesenchymal stem cells (MSCs). Cell Transplant 17:705–712
Kinnaird T, Stabile E, Burnett MS, Shou M, Lee CW, Barr S, Fuchs S, Epstein SE (2004) Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation 109:1543–1549
Lemaire V, Tobin FL, Greller LD, Cho CR, Suva LJ (2004) Modeling the interactions between osteoblast and osteoclast activities in bone remodeling. J Theor Biol 229:293–309
Feng X, Tuo X, Chen F, Wu W, Ding Y, Duan Y, Lin Z (2008) Ultrastructural cell response to tension stress during mandibular distraction osteogenesis. Br J Oral Maxillofac Surg 46:527–532
Shi JH, Zheng B, Chen S, Ma GY, Wen JK (2012) Retinoic acid receptor alpha mediates all-trans-retinoic acid-induced Klf4 gene expression by regulating Klf4 promoter activity in vascular smooth muscle cells. J Biol Chem 287:10799–10811
Axel DI, Frigge A, Dittmann J, Runge H, Spyridopoulos I, Riessen R, Viebahn R, Karsch KR (2001) All-trans retinoic acid regulates proliferation, migration, differentiation, and extracellular matrix turnover of human arterial smooth muscle cells. Cardiovasc Res 49:851–862
Chronopoulos A, Robinson B, Sarper M, Cortes E, Auernheimer V, Lachowski D, Attwood S, Garcia R, Ghassemi S, Fabry B, Del Rio Hernandez A (2016) ATRA mechanically reprograms pancreatic stellate cells to suppress matrix remodelling and inhibit cancer cell invasion. Nat Commun 7:12630
Miano JM, Kelly LA, Artacho CA, Nuckolls TA, Piantedosi R, Blaner WS (1998) all-Trans-retinoic acid reduces neointimal formation and promotes favorable geometric remodeling of the rat carotid artery after balloon withdrawal injury. Circulation 98:1219–1227
Lee CW, Park SJ, Park SW, Kim JJ, Hong MK, Song JK (2000) All-trans-retinoic acid attenuates neointima formation with acceleration of reendothelialization in balloon-injured rat aorta. J Korean Med Sci 15:31–36
Ishii H, Horie S, Kizaki K, Kazama M (1992) Retinoic acid counteracts both the downregulation of thrombomodulin and the induction of tissue factor in cultured human endothelial cells exposed to tumor necrosis factor. Blood 80:2556–2562
Zhang S, Chen X, Hu Y, Wu J, Cao Q, Chen S, Gao Y (2016) All-trans retinoic acid modulates Wnt3A-induced osteogenic differentiation of mesenchymal stem cells via activating the PI3K/AKT/GSK3beta signalling pathway. Mol Cell Endocrinol 422:243–253
Bi W, Gu Z, Zheng Y, Wang L, Guo J, Wu G (2013) Antagonistic and synergistic effects of bone morphogenetic protein 2/7 and all-trans retinoic acid on the osteogenic differentiation of rat bone marrow stromal cells. Dev Growth Differ 55:744–754
Yang QJ, Zhou LY, Mu YQ, Zhou QX, Luo JY, Cheng L, Deng ZL, He TC, Haydon RC, He BC (2012) All-trans retinoic acid inhibits tumor growth of human osteosarcoma by activating Smad signaling-induced osteogenic differentiation. Int J Oncol 41:153–160
Xu J, Sun Y, Wu T, Wang B, Liu Y, Zhang J, Lee WY, Kang Q, Chai Y, Li G (2017) Porcine brain extract promotes osteogenic differentiation of bone marrow derived mesenchymal stem cells and bone consolidation in a rat distraction osteogenesis model. PLoS ONE 12:e0187362
Xu L, Song C, Ni M, Meng F, Xie H, Li G (2012) Cellular retinol-binding protein 1 (CRBP-1) regulates osteogenenesis and adipogenesis of mesenchymal stem cells through inhibiting RXRα-induced beta-catenin degradation. Int J Biochem Cell Biol 44:612–619
ICenci RA, Silveira VS, Mayer L, Oliveira HW, Moraes JFDD, Oliveira MGD (2015) Analysis by means of cone-beam computed tomography, bone density and X-ray beam attenuation of rabbit mandibles subjected to low-level laser therapy during distraction osteogenesis. Revista de Ciências Médicas e Biológicas. Salvador 14:30–35
Sun Y, Xu L, Huang S, Hou Y, Liu Y, Chan KM, Pan XH, Li G (2015) mir-21 overexpressing mesenchymal stem cells accelerate fracture healing in a rat closed femur fracture model. BioMed Res Int. https://doi.org/10.1155/2015/412327
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro–computed tomography. J Bone Miner Res 25:1468–1486
Xu J, Wang B, Sun Y, Wu T, Liu Y, Zhang J, Lee WY, Pan X, Chai Y, Li G (2016) Human fetal mesenchymal stem cell secretome enhances bone consolidation in distraction osteogenesis. Stem Cell Res Ther 7:134
Fujio M, Xing Z, Sharabi N, Xue Y, Yamamoto A, Hibi H, Ueda M, Fristad I, Mustafa K (2017) Conditioned media from hypoxic-cultured human dental pulp cells promotes bone healing during distraction osteogenesis. J Tissue Eng Regener Med 11:2116–2126
Shi H, Yuan L, Yang H, Zang A (2017) The mechanism of all-trans retinoic acid in the regulation of apelin expression in vascular endothelial cells. Biosci Rep. https://doi.org/10.1042/BSR20170684
Tolar J, Le Blanc K, Keating A, Blazar BR (2010) Concise review: hitting the right spot with mesenchymal stromal cells. Stem Cells 28:1446–1455
Zimmermann CE, Gierloff M, Hedderich J, Acil Y, Wiltfang J, Terheyden H (2011) Survival of transplanted rat bone marrow-derived osteogenic stem cells in vivo. Tissue Eng A 17:1147–1156
Harrison G, Shapiro IM, Golub EE (1995) The phosphatidylinositol-glycolipid anchor on alkaline phosphatase facilitates mineralization initiation in vitro. J Bone Min Res 10:568–573
Bais MV, Wigner N, Young M, Toholka R, Graves DT, Morgan EF, Gerstenfeld LC, Einhorn TA (2009) BMP2 is essential for post natal osteogenesis but not for recruitment of osteogenic stem cells. Bone 45:254–266
Komori T (2003) Requisite roles of Runx2 and Cbfb in skeletal development. J Bone Miner Metab 21:193–197
Winet H (1996) The role of microvasculature in normal and perturbed bone healing as revealed by intravital microscopy. Bone 19:S39–S57
Saran U, Piperni SG, Chatterjee S (2014) Role of angiogenesis in bone repair. Arch Biochem Biophys 561:109–117
Wilson A, Shehadeh LA, Yu H, Webster KA (2010) Age-related molecular genetic changes of murine bone marrow mesenchymal stem cells. BMC Genomics 11:229
Liu Y, Berendsen AD, Jia S, Lotinun S, Baron R, Ferrara N, Olsen BR (2012) Intracellular VEGF regulates the balance between osteoblast and adipocyte differentiation. J Clin Investig 122:3101–3113
Fukuhara S, Sako K, Noda K, Zhang J, Minami M, Mochizuki N (2010) Angiopoietin-1/Tie2 receptor signaling in vascular quiescence and angiogenesis. Histol Histopathol 25:387–396
Wang A, Ding X, Sheng S, Yao Z (2008) Retinoic acid inhibits osteogenic differentiation of rat bone marrow stromal cells. Biochem Biophys Res Commun 375:435–439
Warrell RJ (1993) Retinoid resistance in acute promyelocytic leukemia: new mechanisms, strategies, and implications [editorial; comment]. Blood 82:1949–1953
Zhou DC, Kim SH, Ding W, Schultz C, Warrell RP, Gallagher RE (2002) Frequent mutations in the ligand-binding domain of PML-RARα after multiple relapses of acute promyelocytic leukemia: analysis for functional relationship to response to all-transretinoic acid and histone deacetylase inhibitors in vitro and in vivo. Blood 99:1356–1363
Chen ZX, Xue YQ, Zhang R, Tao RF, Xia XM, Li C, Wang W, Zu WY, Yao XZ, Ling BJ (1991) A clinical and experimental study on all-trans retinoic acid-treated acute promyelocytic leukemia patients. Blood 78:1413–1419
Hatake K, Uwai M, Ohtsuki T, Tomizuka H, Izumi T, Yoshida M, Miura Y (1997) Rare but important adverse effects of all-trans retinoic acid in acute promyelocytic leukemia and their management. Int J Hematol 66:13–19
Acknowledgements
This work was supported by National Natural Science Foundation of China (NSFC Nos. 81572122, 81772338) and the Interdisciplinary Program of Shanghai Jiao Tong University (Grant No. YG2017ZD05).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Zhenjun Weng, Chunyang Wang, Cheng Zhang, Jia Xu, Yimin Chai, Yachao Jia, Pei Han, and Gen Wen declare that they have no conflict of interest.
Ethical Approval
This study was specifically approved by the Animal Experimentation Ethics Committee of the Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, and the animal experiments were therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
About this article
Cite this article
Weng, Z., Wang, C., Zhang, C. et al. All-Trans Retinoic Acid Promotes Osteogenic Differentiation and Bone Consolidation in a Rat Distraction Osteogenesis Model. Calcif Tissue Int 104, 320–330 (2019). https://doi.org/10.1007/s00223-018-0501-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0501-6