Abstract
Objective
This retrospective study was to evaluate the relationship between osteoporosis and dynamic cervical plates in screw–plate or screw–bone interface of elderly cervical spondylotic myelopathy (CSM) patients.
Methods
Retrospective study was conducted on elderly CSM patients, treated by anterior corpectomy and reconstruction with titanium mesh cages (TMC) and dynamic cervical plate between July 2004 and June 2007. All patients underwent bone mineral density (BMD) assessment in preoperation, and according to the osteoporosis degree they have been divided into two groups: moderate osteoporosis degree group and severe osteoporosis degree group. The clinical outcome [Japanese Orthopaedic Association score (JOA) and Visual Analogue Scale (VAS)], bone fusion assessment (CT mielogram), the change of titanium mesh cages and plate of cephalic screw-plate-angle (SPA) and cephalic endplate-plate-angle (EPA) of plain X-ray films were measured.
Results
The mean JOA score and recovery rate were not different between the two groups (P > 0.05). There was no loss of sagittal alignment after surgery in any patient, and no significant difference between both groups on lordosis measurements (P > 0.05). Although there was a significant difference of the cage subsidence rate between the two groups (P < 0.001), all patients had favorable bone union and none required additional treatment. The average changes of SPA were greater in A group patients than in B group patients, while the variation of EPA was higher in B group patients than in A group patients (P < 0.001).
Conclusions
Despite the fact that there is a significant difference of the cage subsidence rate between the two groups no clinical outcome, nor sagittal alignment or fusion rate differences among groups was observed in elderly CSM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical spondylotic myelopathy (CSM) is a neurological disorder caused by the narrowing of the spinal canal as a result of degenerative changes in the cervical spine with the advancing age in the population [18, 26, 30]. Various pathologic processes in the cervical spine may cause mechanical compression of the spinal cord and yield to degenerative cervical myelopathy [21, 23]. When the clinical symptoms are severe and progressive, or when conservative treatment is not effective, surgical intervention is indicated [28]. Anterior corpectomy may be the most appropriate procedure to decompress the spinal cord in patients with severe canal stenosis and anterior pathologies [7, 15]. Stabilization after corpectomy is achieved with instrumentation using tricortical autogenous iliac bone graft, autogenous or allogenous fibular graft, and recently titanium mesh cage (TMC) [1, 4, 11, 20, 32].
Cervical corpectomy removes almost all pathology causing spinal cord compressions such as osteophytes, discs, and ossified posterior longitudinal ligament (PLL) [7, 19], and the anterior column support after corpectomy may be restored using structural auto- or allografts and titanium mesh cage [10]. However, Fernyhough et al. [6] reported that autogenous or allogeneous fibular strut grafts may show subsidence into the vertebral bodies, especially in osteoporosis patients, and this increases stress concentration on the implants and sometimes failure of anterior plate or instrumentation. The spinal cord may be compressed for the strut grafts subsidence into the vertebral bodies [30, 32]. Kanayama et al. [13] showed that the anterior plate fixation provides a more rigid construct and results in rapid solid fusion with less risk of graft-related complications. Anterior plates provide stability following decompression and fusion of the cervical spine, and the locking plate includes an integrated lock mechanism, which is designed to prevent migration of the bone screws. Dynamic cervical plate allows for better load sharing while providing overall resistance to motion, address perceived biomechanical deficiencies of rigid cervical plate.
Several clinical studies showed that advanced age, prolonged symptoms prior to surgery, severe preoperative neurologic dysfunction, and a greater degree of cord compression adversely impact the results of anterior surgery [22, 24, 29, 30]. Not only the autogenous or allogeneous fibular strut grafts, but also the TMC may show subsidence into the vertebral bodies, especially in osteoporosis patients, and this causes stress concentration on the implants and sometimes failure of anterior plate or instrumentation [6, 10]. Few data exist on the outcome of dynamic cervical plate in elderly CSM patients of osteoporosis. This retrospective study was to evaluate the relationship between the osteoporosis and dynamic cervical plates in screw–plate or screw–bone interface of elderly CSM patients.
Patients and methods
A retrospective study was conducted on elderly patients, surgically treated for CSM between July 2004 and June 2007. The inclusion criteria were elderly CSM patients in whom only one level needs corpectomy have clinical symptoms and no improvement for at least 6 weeks of conservative therapy (i.e., physical therapy together with use of anti-inflammatory medications and muscle relaxants at the manufacturer’s recommended therapeutic dose). The defined “elderly” patients were older than 65 years, and the patients had osteoporosis. Exclusion criteria included posterior longitudinal ligament (PLL) ossification in addition to spondyloarthritis, patients less than 65 years, and patients without osteoporosis. Preoperative radiologic evaluation in each patient consisted of anteroposterior, lateral, and bilateral oblique radiographs and also flexion–extension films for detecting instability. Magnetic resonance imaging (MRI) was routinely performed. Indications for surgical treatment were progressive myelopathy and spinal cord compression documented by MRI studies, persistent and progressive pain, and impaired neurologic functions.
All patients underwent bone mineral density (BMD) assessment using the peripheral dual-energy X-ray absorptiometry scanner (FR DMS Corp, Challenger) before operation. The bone mineral density of the lumbar spine (L2–L4, in g/cm2) was assessed, T score to justify whether osteoporosis and T ≤ −2.5 SD is osteoporosis. According the osteoporosis degree [14], they were divided into two groups: moderate osteoporosis (A group,T ≤ −2.5 SD, 41 cases) and severe osteoporosis (B group, T ≤ −2.5 SD and had one or more fragility fractures in medical history before operation, 45 cases). Eighty-six patients initially fulfilled the study criteria, and 11 patients were lost to follow-up. Of the remaining 75 patients available for analysis, 36 belong to group A (included 19 men and 17 women with an average age of 72.73 ± 5.61 years), and 39 belong to group B (included 20 men and 19 women with an average age of 73.51 ± 6.32 years). Two groups had similar age and sex distribution, level of pain, and the pain history (Table 1).
Surgical procedures
Anterior corpectomy and decompression procedure was similar to the procedure described by Saunders et al. [28]. TMC was given in proper length and contour according to the angle of proximal and distal endplates before filling with cancellous auto grafts. Bone obtained after corpectomy was used as the autogenous bone graft to fill the mesh cages. Anterior cervical locking plate system (Zephir plate) was used in all patients for further stabilization. All patients were mobilized immediately after the surgery with a hard cervical collar that the patients wore continuously the first 6 weeks after surgery.
Critical of clinical outcome
Before surgery and at the 2-year follow-up, neck pain (Visual Analogue Scale, VAS) and neurologic function (Japanese Orthopaedic Association score, JOA) were quantified. Surgical outcome was represented by the recovery ratio, calculated using the formula: Recovery ratio = (postoperative JOA score−preoperative JOA score)/(17 points−preoperative JOA score)×100%.
Plain X-rays of the cervical spine were obtained, as well as lateral views in flexion and extension. Should any segment show 5° or more angulation and 2 mm or more displacement at lateral flexion and extension radiographs, the segment was considered unstable. The Canvas 9.01 software (Deneba Systems, Scientific Imagine Edition, Miami, FL, USA) was used to measure the cephalic screw-plate-angle (SPA) and cephalic endplate-plate-angle (EPA) of plain X-ray films on personal computer. The SPA was defined as the angle between the axis shaft line of screw and plate, and the EPA as the angle between the line of cephalic endplate posterior marginal to the joint of screw contact plate and the line of plate axis. Take the plate as the point of reference under gravity and linear motion, the SPA response the change of screw, and the EPA response the adjustment of the vertebrae.
CT myelograms were also obtained for all patients. The focus was to evaluate three radiographic characteristics at follow-up: the cervical alignment of C2–C7 curvature, cage position, and fusion rate. The criteria for fusion were continuity of trabecular pattern, and the fusion rate assessed using Computed tomography (CT) scan. Criteria described by Bridwell et al. [3] were used to evaluate fusion through the mesh cages.
Statistical analysis
Statistical analyses were performed independently by a non-clinical research assistant and an outside party to ensure objectivity, using SPSS Version 16.0 software. Student’s t test was used and results were considered statistically significant if the P value was equal to or less than 0.05 for continuous variables.
Results
There was no intraoperative death in our study. Eighty-six patients were included in this study at initially and 75 cases had follow-up at least 24 months. Eleven patients were lost for the follow up time was less than 24 months, and the follow-up rate was 87.8% (36/41) in the A group and 86.7% (39/45) in the B group. The followed time was from 24 to 32 months (average 28 month), and average 28.15 ± 3.24 months on A group and 27.86 ± 2.68 months on B group (P > 0.05). There was no patient with neurologic deterioration after the surgical treatment. All patients had neurologic recovery compared with their preoperative neurologic status, and at the last follow up, they were all able to walk and perform daily activities without any assistance.
There were four patients (11.1%) in A group and five patients (12.8%) in B group noted sometimes with slight neck pain, but none reported mild or severe axial neck pain. The pain index improved from 7.25 ± 2.59 to 2.84 ± 1.16 (P < 0.001) in A group patients and improved from 7.18 ± 2.46 to 2.78 ± 1.35 (P < 0.001) in B group patients (Table 2). At the final follow-up, the pain index of VAS was 1.53 ± 0.62 in A group patients and 1.48 ± 0.71 in B group patients, and there was no significant difference (P > 0.05).
The mean JOA score was 8.9 ± 2.3 preoperatively, 15.6 ± 1.1 on the initial postoperatively, and 15.24 ± 1.2 on the final follow-up in A group patients. Compared to A group, the average JOA score was 8.3 ± 2.4 preoperatively, 15.4 ± 1.3 on the initial postoperatively, and 15.3 ± 1.4 on the final follow-up in B group patients (Table 2). The recovery rates of JOA score were 82.3 ± 10.2 in A group and 81.8 ± 11.6 in B group (P > 0.05).
Postoperative sagittal cervical alignment was within the normal range in all patients. There was no loss of sagittal alignment after surgery in any patients. The average of lordosis between C2 and C7 was 14.5 ± 6.9 degrees at preoperatively, 12.4 ± 5.6° at post-3 months and 12.7 ± 4.1° at last follow up in A group. Compared to A group, the mean lordosis was 14.7 ± 6.3° at preoperatively, 13.1 ± 6.2° at post-3 months and 12.2 ± 5.6° at last follow up in B group. The difference in lordosis measurements at preoperative, at post-3 months and at last follow up was not significant (P > 0.05). There was also no significant difference between both groups (P > 0.05).
There was no anterior implant failure. Spinal fusion was noted in all patients between the mesh cage and adjacent upper and lower endplates on dynamic X-rays of the cervical spine at 11 months. None of the patients had evidence of pseudarthrosis. There were no cases of cage extrusion, migration, or collapse. Three cases (8.3%) of loss of corpectomy level height between the initial and final postoperative X-rays suggestive of cage subsidence (average 2.8 ± 1.1 mm; range 2–4 mm) over time in A group (Table 3). However, an average cage subsidence of 4.2 ± 2.1 mm (range 3–6 mm) was seen on the postoperative radiograph in 12 patients (30.8%) in B group. Although there was significant difference of the cage subsidence rate between two groups (P < 0.001), all patients had favorable bone union and none required additional treatment.
The fact of osteoporosis in patients should be taken into account when the dynamic cervical plate was put to use in elderly CSM patients, for the movement at the screw–plate or screw–bone interface was different on the degree of osteoporosis (Table 3, Figs. 1, 2). The average change of SPA was greater in A group patients than B group patients (10.27 ± 4.59 deg versus 2.69 ± 1.75 deg, P < 0.001), and the variation of EPA were higher in B group patients than A group patients (4.81 ± 2.73 deg versus 2.93 ± 1.86 deg, P < 0.001).
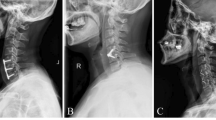
Moderate osteoporotic of CSM patient. a Preoperative lateral radiographs of 73-year-old man with cervical spondylotic myelopathy. b Postoperative lateral cervical radiograph reveals anterior corpectomy and fusion of C5–6–7 with titanium curve mesh cage packed with autogenous bone graft and anterior cervical plate fixation. c Lateral radiography obtained 12 months after surgery
Severe osteoporosis of CSM patient. a Lateral roentgenogram of 72-year-old man with cervical spondylotic myelopathy. b Postoperative lateral cervical radiograph reveals anterior corpectomy and fusion of C5–6–7 with a mesh cage packed with autogenous bone graft and anterior cervical plate. c lateral radiography obtained 12 months after surgery
Discussion
Cervical spondylotic myelopathy is the most common reason of spinal cord dysfunction in patients over 50 years of age [15, 23]. Their history usually involves an indolent course, and neurologic status is usually good in the early period. However, there is no sign or method to understand when neurologic deterioration will occur. Several clinical studies show that advanced age, prolonged symptoms prior to surgery, severe preoperative neurologic dysfunction, and a greater degree of cord compression adversely impact the results of surgery [2, 8, 18, 28, 31]. Major neurologic recovery occurs in the first 6 months in these cases. The mean JOA score was better than preoperational and maintained to final follow up. Postoperative sagittal cervical alignment was within the normal range in all patients. A period of neurologic recovery after anterior corpectomy varies in the literature. Majd et al. [20] reported a surgical treatment for cervical spondylotic myelopathy patients, most of neurologic recovery occurs gradually in the first 6 months. Kirkpatrick [16] and Orr [25] studies suggested that it may take up to 2 years. Fessler et al. [7] reported 92% improved neurologic status in their series. In the current study, four patients (11.1%) in moderate osteoporosis group and five patients (12.8%) in severe osteoporosis group were sometimes noted with slight neck pain post operation, but none reported mild or severe axial neck pain. The pain index got better than preoperational and maintained to final follow up, and there were no significant differences between the two groups.
Cervical corpectomy removes almost all pathology which causing spinal cord compression [7, 19], and the anterior column support may be restored using TMC after corpectomy. TMC, used with variable diameter and height and can be filled with autogeneous cancellous bone graft, has many advantages when used for anterior column support [10, 12]. Primary stability is improved with the spikes, which penetrate into the adjacent upper and lower endplates. Also, precontoured cages help to achieve better sagittal alignment, especially when more than 2-level corpectomy is performed. TMC filled with autogenous iliac cancellous bone graft helps in early fusion [4]. There were no cases of cage extrusion, migration, or collapse in this study. The difference in lordosis measurements at preoperative, at post three month and at last follow up was not significant. There was no loss of sagittal alignment after surgery in any patient. Thus, stability is improved and sagittal alignment is preserved. However, the cage subsidences were not only in moderate osteoporosis group patients, but also in the severe osteoporosis group patients. There was no anterior implant failure in this series. Spinal fusion was noted in all patients between the mesh cage and adjacent upper and lower end plates on dynamic X-rays of the cervical spine.
Cervical plates offer the advantages of improved initial stability in the post-operative period, which decreases the need for wearing a cervical collar and results in a faster return to normal activities [9, 17]. Anterior cervical plate has become widely accepted when single and multi-level anterior cervical fusion surgery is performed, and several important features have been added to the newer generation of plates for increasing the rate of graft fusion. Dynamic cervical plate, which was designed in a way to increase the load on the graft and allow for better load sharing allows axial translation and rotation at the plate–screw interface so that, theoretically, fusion rates would increase and time to fusion would diminish [5, 27]. The movement at the screw–plate interface was different on the degree of osteoporosis in this study (Figs. 1, 2). For the elderly patients, frequently having a variety of osteoporosis, the movements at the screw–plate interface were bigger in moderate than severe osteoporotic patients. On the contrary, there were more movements at the screw–bone interface in severe osteoporotic patients than moderate. For this reason, the facts osteoporosis in patients should be take into account when the dynamic cervical plates was put to use in elderly cervical spondylotic myelopathy patients.
The major shortcoming of this study is that the results are not compared with a control series of non osteoporotic patients and the limitations of this study are the nature of this analysis was retrospective which may be associated with biases. Further studies are required to avoid selection bias, and long-term prospective and randomized studies will be necessary to provide optimal clinical data to determine the associations between the osteoporosis and dynamic cervical plates in elderly CSM patients.
Conclusion
Despite the fact that there is a significant difference of the cage subsidence rate between the two groups no clinical outcome, nor sagittal alignment or fusion rate differences among groups was observed in elderly CSM patients.
References
Acosta FL, Aryan HE, Chou D, Ames CP (2008) Long-term biomechanical stability and clinical improvement after extended multilevel corpectomy and circumferential reconstruction of the cervical spine using titanium mesh cages. J Spinal Disord Tech 21(3):165–174
Barnes MP, Saunders M (1984) The effect of cervical mobility on the natural history of cervical spondylotic myelopathy. J Neurol Neurosurg Psychiatry 47(1):17–20
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K (1995) Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 20(12):1410–1418
Eck KR, Bridwell KH, Ungacta FF, Lapp MA, Lenke LG, Riew KD (2000) Analysis of titanium mesh cages in adults with minimum two-year follow-up. Spine (Phila Pa 1976) 25(18):2407–2415
Fassett DR, Apfelbaum R, Clark R, Bachus KN, Brodke DS (2005) Biomechanical analysis of a new concept: an add-on dynamic extension plate for adjacent-level anterior cervical fusion. Spine (Phila Pa 1976) 30(22):2523–2529
Fernyhough JC, White JI, LaRocca H (1991) Fusion rates in multilevel cervical spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976) 16(10 Suppl):S561–S564
Fessler RG, Steck JC, Giovanini MA (1998) Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery 43(2):257–265 (Discussion 265–257)
Herkowitz HN (1989) The surgical management of cervical spondylotic radiculopathy and myelopathy. Clin Orthop Relat Res 239:94–108
Hussain M, Natarajan RN, Fayyazi AH, Braaksma BR, Andersson GB, An HS (2009) Screw angulation affects bone-screw stresses and bone graft load sharing in anterior cervical corpectomy fusion with a rigid screw-plate construct: a finite element model study. Spine J 9(12):1016–1023
Hwang S-L, Lee K-S, Su Y-F et al (2007) Anterior corpectomy with iliac bone fusion or discectomy with interbody titanium cage fusion for multilevel cervical degenerated disc disease. J Spinal Disord Tech 20(8):565–570
Ikenaga M, Shikata J, Tanaka C (2005) Anterior corpectomy and fusion with fibular strut grafts for multilevel cervical myelopathy. J Neurosurg Spine 3(2):79–85
Ikenaga M, Shikata J, Tanaka C (2006) Long-term results over 10 years of anterior corpectomy and fusion for multilevel cervical myelopathy. Spine (Phila Pa 1976) 31(14):1568–1574 discussion 1575
Kanayama M, Cunningham BW, Weis JC, Parker LM, Kaneda K, McAfee PC (1998) The effects of rigid spinal instrumentation and solid bony fusion on spinal kinematics:a posterolateral spinal arthrodesis model. Spine (Phila Pa 1976) 23(7):767–773
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9(8):1137–1141
Kawakami M, Tamaki T, Iwasaki H, Yoshida M, Ando M, Yamada H (2000) A comparative study of surgical approaches for cervical compressive myelopathy. Clin Orthop Relat Res 381:129–136
Kirkpatrick JS, Levy JA, Carillo J, Moeini SR (1999) Reconstruction after multilevel corpectomy in the cervical spine A sagittal plane biomechanical study. Spine (Phila Pa 1976) 24(12):1186–1190 discussion 1191
Kristof RA, Kiefer T, Thudium M et al (2009) Comparison of ventral corpectomy and plate-screw-instrumented fusion with dorsal laminectomy and rod-screw-instrumented fusion for treatment of at least two vertebral-level spondylotic cervical myelopathy. Eur Spine J 18(12):1951–1956
LaRocca H (1988) Cervical spondylotic myelopathy: natural history. Spine (Phila Pa 1976) 13(7):854–855
Macdonald RL, Fehlings MG, Tator CH et al (1997) Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg 86(6):990–997
Majd ME, Vadhva M, Holt RT (1999) Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 24(15):1604–1610
Matz PG, Anderson PA, Holly LT et al (2009) The natural history of cervical spondylotic myelopathy. J Neurosurg Spine 11(2):104–111
Min J-H, Jung B-J, Jang J-S, Kim S-K, Jung D-J, Lee S-H (2009) Spinal cord herniation after multilevel anterior cervical corpectomy and fusion for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 10(3):240–243
Montgomery DM, Brower RS (1992) Cervical spondylotic myelopathy Clinical syndrome and natural history. Orthop Clin North Am 23(3):487–493
Oh MC, Zhang HY, Park JY, Kim KS (2009) Two-level anterior cervical discectomy versus one-level corpectomy in cervical spondylotic myelopathy. Spine (Phila Pa 1976) 34(7):692–696
Orr RD, Zdeblick TA (1999) Cervical spondylotic myelopathy. Approaches to surgical treatment. Clin Orthop Relat Res 359:58–66
Rafael H (2003) Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery 53(3):787 author reply 787–788
Reidy D, Finkelstein J, Nagpurkar A, Mousavi P, Whyne C (2004) Cervical spine loading characteristics in a cadaveric C5 corpectomy model using a static and dynamic plate. J Spinal Disord Tech 17(2):117–122
Saunders RL, Bernini PM, Shirreffs TG, Reeves AG (1991) Central corpectomy for cervical spondylotic myelopathy: a consecutive series with long-term follow-up evaluation. J Neurosurg 74(2):163–170
Vaccaro AR, Falatyn SP, Scuderi GJ et al (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11(5):410–415
Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T (2003) Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery 52(1):122–126 discussion 126
Zdeblick TA, Bohlman HH (1989) Cervical kyphosis and myelopathy Treatment by anterior corpectomy and strut-grafting. J Bone Joint Surg Am 71(2):170–182
Zdeblick TA, Ducker TB (1991) The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976) 16(7):726–729
Conflict of interest
There are no competing interests in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yan, D., Wang, Z., Deng, S. et al. Anterior corpectomy and reconstruction with titanium mesh cage and dynamic cervical plate for cervical spondylotic myelopathy in elderly osteoporosis patients. Arch Orthop Trauma Surg 131, 1369–1374 (2011). https://doi.org/10.1007/s00402-011-1317-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-011-1317-2