Abstract
Purpose
To evaluate the efficacy and safety of a new type of titanium mesh cage (NTMC) in hybrid anterior decompression and fusion method (HDF) in treating continuously three-level cervical spondylotic myelopathy (TCSM).
Methods
Ninety-four cases who had TCSM and accepted the HDF from Jan 2007 to Jan 2010 were included. Clinical and radiological outcomes were compared between cases who had the NTMC (Group A, n = 45) and traditional titanium mesh cage (TTMC, Group B, n = 49) after corpectomies. Each case accepted one polyetheretherketone cage (PEEK) after discectomy.
Results
Mean follow-up were 74.4 and 77.3 months in Group A and B, respectively (p > 0.05). Differences in cervical lordosis (CL), segmental lordosis (SL), anterior segmental height (ASH) and posterior segmental height (PSH) between two groups were not significant preoperatively, 3-days postoperatively or at final visit. However, losses of the CL, SL, ASH and PSH were all significantly larger in Group B at the final visit, so did incidences of segmental subsidence and severe subsidence. Difference in preoperative Japanese Orthopedic Association (JOA), visual analog scale (VAS), neck disability index (NDI) or SF-36 between two groups was not significant. At the final visit, fusion rate, JOA, and SF-36 were all comparable between two groups, but the VAS and NDI were both significantly greater in Group B.
Conclusions
For cases with TCSM, HDF with the NTMC and TTMC can provide comparable radiological and clinical improvements. But application of the NTMC in HDF is of advantages in decreasing the subsidence incidence, losses of lordosis correction, VAS and NDI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For cases with multilevel cervical spondylotic myelopathy (CSM), anterior approach can provide direct decompression and construction, and it has been proven to be an effective and safe technique [1]. Anterior cervical corpectomy and fusion (ACCF) offers sufficient operating space and decompression extents, but increased blood loss and high rates of graft-related complications have limited its application [2, 3]. Anterior cervical discectomy and fusion (ACDF) is reported to be of less complications when compared with the ACCF, but it will be of difficulty and challenge for complete decompression through intervertebral space in some cases [4]. Taking all these into consideration, hybrid anterior decompression and fusion technique (HDF) that combined one-vertebrae corpectomy and one-level discectomy is developed. And it is especially suitable for cases who had simple disc herniation or small osteophyte at one level, and huge herniated disc, large osteophyte, or ossification of posterior longitudinal ligament (OPLL) at adjacent level [3, 5]. Researches of Guo et al. and Liu et al. had proven the effectiveness and safety of the HDF [6, 7]. However, improvement of cervical lordosis after the HDF is inferior to the ACDF at the final visit, and subsidence of the titanium mesh cage (TMC) may play an important role in loss of lordosis correction [6, 8]. The reported incidence of traditional TMC (TTMC) subsidence was as high as 96%, and severe subsidence was reported to be associated with neurological deterioration, neck pain and instrument failures [9–11]. To eliminate these complications of the TTMC, we designed a new type of TMC (NTMC, Fig. 1) and found that it could decrease the incidence of severe subsidence after one-level ACCF [12]. In this study, we compared clinical and radiological outcomes between cases who had continuously three-level CSM (TCSM) and underwent the HDF with the application of NTMC and TTMC, to assess the efficiency and safety of the NTMC.
The lateral view of the NTMC (a). The superior endcap is curved to fit the inferior endplate, and has a tuber ventrally and paralleled grooves to prevent shifting backward (b). A 10-degree angle that tilts backward and upward and paralleled grooves are designed at the inferior endcap to fit the superior endplate (a, c)
Materials and methods
Patient population
From Jan 2007 to Jan 2010, a total of 113 cases had taken the HDF for TCSM by one senior surgeon consecutively. Nineteen cases who had injury history, previous cervical spine history, infection and tumor were excluded. Each case had either NTMC (Designed by ourselves) or TTMC (DePuy, USA) been implanted alternatively according to the sequence of admission, and had polyetheretherketone cage (PEEK, DePuy, USA) being implanted at adjacent intervertebral space. The included 94 cases were divided into Group A (NTMC/PEEK, n = 45, Fig. 2) and Group B (TTMC/PEEK, n = 49, Fig. 3) according to the TMC type.
A 65-year-old female case. She complained of weakness and numbness of limbs, and chest zonesthesia for 3 months. Preoperative MRI and lateral radiograph showed huge slipped disc locating at dorsal part of C4 vertebrae body and significant disc degeneration at C5/6 level (A–C). She accepted the HDF with NTMC/PEEK. Lateral radiograph postoperatively showed significant improvement in the CL and SL (D). The lateral radiograph 61-months postoperatively showed segmental subsidence (White arrow a, b, c and d in E)
A 61-year-old male case. He complained of degenerative hands weakness and gait instability for 1 year. Preoperative MRI, CT and lateral radiograph showed disc degeneration and calcification at C3/4 level, intervertebral instability at C4/5 and C5/6 levels (A–C). Lateral radiograph postoperatively showed increases in cervical lordosis and segmental lordosis after the HDF with TTMC/PEEK (D). E showed segmental subsidence 67 months postoperatively (White arrow a and b)
Surgical techniques
After general endotracheal anesthesia, a right-sided Smith-Robinson approach was carried out to expose cervical vertebral bodies and discs. Discectomy was performed first. After adequate removal of disc, posterior osteophyte and posterior longitudinal ligament, a proper-size PEEK cage packed with autogenous bone was implanted into intervertebral space. After necessary adjacent discectomies, three-fifths vertebral body was excised centrally to make a bone groove. Then the posterior longitudinal ligament was resected in each case to ensure complete decompression. For cases in Group A, the intervertebral spaces were decompressed bilaterally larger to accommodate the larger endcaps of the NTMC. After being packed with autogenous bone, the TMC was inserted into the bone groove. A semi-constrained cervical plate (Coddman or Slimlock, DePuy, USA) was used to bridge the fusion segments. All cases wear a Philadelphia neck collar for at least 2 months.
Radiological and clinical assessments
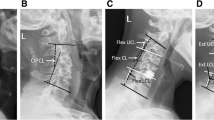
All cases took lateral radiographs before the operation and 3 days postoperatively. Additional flexion–extension lateral radiographs were also obtained at 2, 6, 12 months and then each year postoperatively. Bone graft fusion was defined as no motion across the fusion segment on the flexion–extension radiograph and presence of bridging bony trabeculae between endplates and grafts on the lateral radiograph. Cobb angles at C2–C3, C2–C7 and fusion segment were measured as local lordosis (LL), cervical lordosis (CL) and segmental lordosis (SL), respectively (Fig. 4). Anterior segment height (ASH) and posterior segment height (PSH) were also collected (Fig. 4). Time point of 3 days postoperatively was defined as post-operation. Loss of the CL, LL, SL, ASH or PSH was calculated as = Final index − Postoperative index. Occurrence of segmental subsidence and severe subsidence was validated when loss value of the ASH or PSH was >0 and >3 mm, respectively.
1 The anterior segment height, measured as distance between anterior margins of the endplates at the fusion segment. 2 The posterior segment height, measured as distance between posterior margins of the endplates at the fusion segment. 3 Local lordosis, Cobb angle between C2 and C3. 4 Cervical lordosis, Cobb angle between C2 and C7. 5 Segmental lordosis, Cobb angle at fusion segment
Neurological function was evaluated by Japanese Orthopedic Association (JOA) scoring system, and neurological recovery rate (RR) was calculated as = (Final JOA − preoperative JOA)/(17-preoperative JOA) × 100%. Preoperative and final visual analog scale (VAS), neck disability index (NDI score) and 36-item short-form health survey score (SF-36) in two groups were also compared.
Analysis methods
Statistical analyses were performed using SPSS (Version 18.0, SPSS Inc., Chicago, IL, USA). Comparisons of quantitative data were evaluated by the Independent-Samples T Test or Paired-Samples T Test, and categorical data by Pearson’s Chi squared test. Difference was defined as significant when the p value was less than 0.05.
Results
There weren’t significant differences in demographic data between two groups (Table 1). All cases obtained bone fusion within 12 months. As shown in Table 2, differences in the ASH, PSH, LL, CL and SL weren’t significant between two groups preoperatively, postoperatively and at the finial visit (p > 0.05). All the ASH, PSH, CL and SL increased significantly in Group A and B after the HDF, but the LL kept unchanged in both groups. Loss values of the ASH, PSH, CL and SL were all significantly larger in Group B (p = 0.016 and 0.031, respectively), but difference in loss of the LL between two groups was not significant (p > 0.05). The PSH/ASH value in Group A and B was 0.956 ± 0.021 and 0.953 ± 0.030 postoperatively, 0.930 ± 0.093 and 0.919 ± 0.118 at the final visit. And differences in the PSH/ASH value between Group A and B postoperatively and at the final visit were not significant (p > 0.05).
Incidences of segmental subsidence and severe subsidence were 42.2 and 6.7% in Group A, 63.3 and 22.4% in Group B, and they were both significantly different between the two groups (p = 0.033 and 0.030, respectively). There were no breakage or extrusion of implants during follow-up periods in both groups. To exclude influences of the location of TMC and appearance of the OPLL on radiological outcomes, cases were divided into eight subgroups. Results in Table 3 showed that loss values of the ASH, PSH, CL and SL in Group A were all significantly less than that in Group B, in spite of the location of TMC or the appearance of OPLL.
As shown in Table 4, the JOA and SF-36 significantly increased, and the VAS and NDI significantly decreased in both groups at the final visit (p < 0.05). No case in both groups experienced early or late neurological deterioration. There weren’t significant differences in preoperative JOA, SF-36, VAS and NDI between two groups. At the final visit, differences in the JOA, RR and SF-36 were not significant, but the VAS and NDI were significantly larger in Group B (p < 0.05).
Discussion
The ACCF technique is optional for treating multilevel CSM, but high risk of hardware failure due to long lever-arm reconstruction has limited its application prospect in clinical practice, and to reduce vertebral body resection and shorten cage length seems to be the main research direction [13, 14]. Ashkenazi et al. firstly developed a hybrid decompression and fixation technique, and considered it to be a promising technique for multilevel CSM [8]. Then Xu et al. reported that the incidence of graft migration after hybrid technique with one-level ACCF and one-level cage-standalone discectomy was lower than that after standard two-level ACCF [15]. A minimum 2-year follow-up research also found that two-level ACCF and one-level stand-alone cage fixation were of advantages over three-level ACCF in greater initial stability, less postoperative incidences of reconstructive failure C5 palsy [16]. When coming to traditional screw-plate system, three researches from our institution reported that neurological outcomes after the three-level ACDF, two-level ACCF, and the HDF with one-level ACCF and one-level ACDF were comparable, and the HDF technique provided less blood loss, operation time, non-fusion rate and complication incidences than two-level ACCF [6, 7, 17]. Our results also showed significant improvements in the CL, SL, JOA, SF-36, VAS and NDI at the final visit in both groups (Tables 2, 4), and no cases experienced disastrous complications. This is consistent with previous studies, and additionally proves the effectiveness and safety of the HDF for the treatment of TCSM.
Incidence of the TMC subsidence was reported to be higher than the PEEK cage, and segmental subsidence rate would grow higher after the HDF than the ACDF [11, 18]. As all cases in our study had the PEEK cage being implanted after discectomy, to decrease the TMC subsidence was of importance for preventing segmental subsidence [19–21]. Segmental lordosis reconstruction is based on the angulation of inferior and vertebral bodies at fusion segment. However, the paralleled TTMC contact faces will result in incomplete cage-endplate contacts and improper load distribution. Furthermore, as diameter of the TTMC is smaller than the vertebral sagittal diameter and most inferior cage-endplate contact area is limited at the anterior portion of the cage, posterior rim of the TTMC has to contact with the weak and cancellous endplate [22–26]. Although a new nano-hydroxyapatite/polyamide-66 cage with wider rim was reported to provide earlier fusion and less subsidence than the TTMC after single-level ACCF, contacts between the cage and endplates did not matched fully, either [27]. What’s more, taking excellent biocompatibility and widely accepted safety of titanium material into account, to improve cage-endplate contact basing on the TTMC might be an easy and safe solution. A new type of TMC which could match well with superior and inferior endplates to eliminate the cleavage and micro-motion between TMC endcaps and endplates was designed by ourselves [28]. Advantage of the NTMC in reducing severe subsidence incidence over the TTMC had been proved by Yu, et al. [12]. In this study, although the ASH and PSH in two groups postoperatively and at final visit were both comparable, losses of them were both significantly less in Group A, in spite of the location of TMC or the appearance of OPLL. Combining with less incidences of segmental subsidence and severe subsidence, results in Tables 2 and 3 suggest that the application of NTMC could provide better postoperative stability than the TTMC after the HDF.
As shown in Table 2, we found no significant differences in LL, CL or SL between two groups at the final visit. These results indicate that the application of the NTMC provide comparable capability with the TTMC in lordosis restoration. Loss of the PSH/ASH value, rather than the segmental subsidence, might mainly contribute to the improvement of the SL, but relationship hadn’t been confirmed [20, 25]. In this study, comparable PSH/ASH values was accompanied by similar SL in two groups during the follow-up period. This is consistent with previous studies, but improvement of the SL and loss of the CL and in this study existed as a conflict, and development of adjacent segment degeneration should be considered [6, 17, 29, 30]. As degeneration at disc C7/T1 was not common and the fusion extent did not included the C2, small loss of the LL would result in a large change in CL [31, 32]. In this study, we found loss of the LL in Group A was less than that in Group B, although difference was not significant. And this may partly explain why loss of the CL was significantly less in Group A. To explore other risk factors which could influence lordosis changes in details, we divided cases into subgroups according to the location of TMC or the appearance of OPLL. Results in Table 3 showed that change of the CL and SL were both larger in Group B. We suppose that application of the NTMC in HDF could reduce less adjacent segment degeneration, but further study with follow-up computerized tomography (CT) and magnetic resonance image (MRI) is needed.
When it came to clinical outcomes, we found cases in two groups had comparable neurological improvement and SF-36 at the final visit, and none got neurological deterioration. This had indicated the effectiveness of the HDF with NTMC in treating cases with TCSM, and it was consistent with previous studies that used the TTMC [6, 15, 17]. Neck pain after anterior reconstruction was reported to be associated with larger incidences of segmental subsidence, especially the severe subsidence [9, 24]. The NDI is used to assess the influence of neck pain on activities of daily living, and it is associated with the VAS [33]. We found no significant differences in preoperative VAS and NDI scores between two groups, but both of them were significantly less in Group A at the final visit. Basing on these results, we suppose that application of the NTMC can provide comparable improvements in neurological function and the SF-36, and decrease negative influences of neck pain when compared with the application of the TTMC after the HDF, and these might be associated with comparable maintenance of the cervical sagittal alignment and less incidence of mesh cage subsidence after the application of the NTMC [12, 34, 35].
Conclusions
This study indicates that the HDF with the NTMC or TTMC being implanted provides comparable improvements in cervical lordosis, JOA scores and SF-36 scores for cases with continuously TCSM. The application of NTMC could significantly reduce losses of segmental height and cervical lordosis, and decrease subsidence incidence, VAS and NDI after the HDF when compared with the TTMC.
References
Seng C, Tow BP, Siddiqui MA, Srivastava A, Wang L, Yew AK, Yeo W, Khoo SH, Balakrishnan NM, Bin Abd Razak HR, Chen JL, Guo CM, Tan SB, Yue WM (2013) Surgically treated cervical myelopathy: a functional outcome comparison study between multilevel anterior cervical decompression fusion with instrumentation and posterior laminoplasty. Spine J Off J N Am Spine Soc 13:723–731. doi:10.1016/j.spinee.2013.02.038
Xiao SW, Jiang H, Yang LJ, Xiao ZM (2015) Anterior cervical discectomy versus corpectomy for multilevel cervical spondylotic myelopathy: a meta-analysis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 24:31–39. doi:10.1007/s00586-014-3607-1
Lau D, Chou D, Mummaneni PV (2015) Two-level corpectomy versus three-level discectomy for cervical spondylotic myelopathy: a comparison of perioperative, radiographic, and clinical outcomes. J Neurosurg Spine 23:280–289. doi:10.3171/2014.12.SPINE14545
Shamji MF, Massicotte EM, Traynelis VC, Norvell DC, Hermsmeyer JT, Fehlings MG (2013) Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Spine 38:S195–S209. doi:10.1097/BRS.0b013e3182a7eb27
Burkhardt JK, Mannion AF, Marbacher S, Dolp PA, Fekete TF, Jeszenszky D, Porchet F (2013) A comparative effectiveness study of patient-rated and radiographic outcome after 2 types of decompression with fusion for spondylotic myelopathy: anterior cervical discectomy versus corpectomy. Neurosurg Focus 35:E4. doi:10.3171/2013.3.FOCUS1396
Guo Q, Bi X, Ni B, Lu X, Chen J, Yang J, Yu Y (2011) Outcomes of three anterior decompression and fusion techniques in the treatment of three-level cervical spondylosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 20:1539–1544. doi:10.1007/s00586-011-1735-4
Liu Y, Qi M, Chen H, Yang L, Wang X, Shi G, Gao R, Wang C, Yuan W (2012) Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 21:2428–2435. doi:10.1007/s00586-012-2323-y
Ashkenazi E, Smorgick Y, Rand N, Millgram MA, Mirovsky Y, Floman Y (2005) Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine 3:205–209. doi:10.3171/spi.2005.3.3.0205
Chen Y, Chen D, Guo Y, Wang X, Lu X, He Z, Yuan W (2008) Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech 21:489–492. doi:10.1097/BSD.0b013e318158de22
Kabir SM, Alabi J, Rezajooi K, Casey AT (2010) Anterior cervical corpectomy: review and comparison of results using titanium mesh cages and carbon fibre reinforced polymer cages. Br J Neurosurg 24:542–546. doi:10.3109/02688697.2010.503819
Karikari IO, Jain D, Owens TR, Gottfried O, Hodges TR, Nimjee SM, Bagley CA (2014) Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech 27:1–10. doi:10.1097/BSD.0b013e31825bd26d
Fengbin Y, Jinhao M, Xinyuan L, Xinwei W, Yu C, Deyu C (2013) Evaluation of a new type of titanium mesh cage versus the traditional titanium mesh cage for single-level, anterior cervical corpectomy and fusion. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22:2891–2896. doi:10.1007/s00586-013-2976-1
Hartmann S, Tschugg A, Obernauer J, Neururer S, Petr O, Thome C (2016) Cervical corpectomies: results of a survey and review of the literature on diagnosis, indications, and surgical technique. Acta Neurochir (Wien) 158:1859–1867. doi:10.1007/s00701-016-2908-z
Brenke C, Fischer S, Carolus A, Schmieder K, Ening G (2016) Complications associated with cervical vertebral body replacement with expandable titanium cages. J Clin Neurosci Off J Neurosurg Soc Australas 32:35–40. doi:10.1016/j.jocn.2015.12.036
Wei-bing X, Wun-Jer S, Gang L, Yue Z, Ming-xi J, Lian-shun J (2009) Reconstructive techniques study after anterior decompression of multilevel cervical spondylotic myelopathy. J Spinal Disord Tech 22:511–515. doi:10.1097/BSD.0b013e3181a6a1fa
Odate S, Shikata J, Kimura H, Soeda T (2016) Hybrid decompression and fixation technique versus plated 3-vertebra corpectomy for 4-segment cervical myelopathy: analysis of 81 cases with a minimum 2-year follow-up. Clin Spine Surg 29:226–233. doi:10.1097/BSD.0b013e31827ada34
Liu Y, Hou Y, Yang L, Chen H, Wang X, Wu X, Gao R, Wang C, Yuan W (2012) Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine 37:E1450–E1458. doi:10.1097/BRS.0b013e31826c72b4
Park Y, Maeda T, Cho W, Riew KD (2010) Comparison of anterior cervical fusion after two-level discectomy or single-level corpectomy: sagittal alignment, cervical lordosis, graft collapse, and adjacent-level ossification. Spine J Off J N Am Spine Soc 10:193–199. doi:10.1016/j.spinee.2009.09.006
Sasso RC, Ruggiero RA Jr, Reilly TM, Hall PV (2003) Early reconstruction failures after multilevel cervical corpectomy. Spine 28:140–142. doi:10.1097/01.BRS.0000041590.90290.56
Bartels RH, Donk RD, Feuth T (2006) Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 58:502–508. doi:10.1227/01.NEU.0000197258.30821.50 discussion 502–508
Hee HT, Majd ME, Holt RT, Whitecloud TS 3rd, Pienkowski D (2003) Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. Journal of spinal disorders & techniques 16:1–8 discussion 8-9
Cheng CC, Ordway NR, Zhang X, Lu YM, Fang H, Fayyazi AH (2007) Loss of cervical endplate integrity following minimal surface preparation. Spine 32:1852–1855. doi:10.1097/BRS.0b013e31811ece5a
Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN (2003) Failure of human cervical endplates: a cadaveric experimental model. Spine 28:2204–2208. doi:10.1097/01.BRS.0000084881.11695.50
Wu J, Luo D, Ye X, Luo X, Yan L, Qian H (2015) Anatomy-related risk factors for the subsidence of titanium mesh cage in cervical reconstruction after one-level corpectomy. Int J Clin Exp Med 8:7405–7411
Jang JW, Lee JK, Lee JH, Hur H, Kim TW, Kim SH (2014) Effect of posterior subsidence on cervical alignment after anterior cervical corpectomy and reconstruction using titanium mesh cages in degenerative cervical disease. J Clin Neurosci Off J Neurosurg Soc Australas 21:1779–1785. doi:10.1016/j.jocn.2014.02.016
Dorai Z, Morgan H, Coimbra C (2003) Titanium cage reconstruction after cervical corpectomy. J Neurosurg 99:3–7
Yang X, Chen Q, Liu L, Song Y, Kong Q, Zeng J, Xue Y, Ren C (2013) Comparison of anterior cervical fusion by titanium mesh cage versus nano-hydroxyapatite/polyamide cage following single-level corpectomy. Int Orthop 37:2421–2427. doi:10.1007/s00264-013-2101-4
Chen YCD, Yang L et al (2010) Three-dimensional finite elements study of a new titanium mesh cage for bone grafting. J Spinal Surg 18:290–294 (In Chinese)
Tome-Bermejo F, Morales-Valencia JA, Moreno-Perez J, Marfil-Perez J, Diaz-Dominguez E, Pinera AR, Alvarez L (2016) Long-term changes in sagittal alignment and its clinical implications after cervical interbody fusion cage subsidence for degenerative cervical disc disease A prospective study with standalone lordotic tantalum cages. Clin Spine Sur. doi:10.1097/BSD.0000000000000293
Lee SE, Jahng TA, Kim HJ (2015) Correlation between cervical lordosis and adjacent segment pathology after anterior cervical spinal surgery. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 24:2899–2909. doi:10.1007/s00586-015-4132-6
Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD (2014) Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J Off J N Am Spine Soc 14:1228–1234. doi:10.1016/j.spinee.2013.09.043
Carrier CS, Bono CM, Lebl DR (2013) Evidence-based analysis of adjacent segment degeneration and disease after ACDF: a systematic review. Spine J Off J N Am Spine Soc 13:1370–1378. doi:10.1016/j.spinee.2013.05.050
Resnick DN (2005) Subjective outcome assessments for cervical spine pathology: a narrative review. J Chiropr Med 4:113–134. doi:10.1016/S0899-3467(07)60121-9
Lee CH, Kim KJ, Hyun SJ, Yeom JS, Jahng TA, Kim HJ (2015) Subsidence as of 12 months after single-level anterior cervical inter-body fusion. Is it related to clinical outcomes? Acta Neurochir (Wien) 157:1063–1068. doi:10.1007/s00701-015-2388-6
Sakai K, Yoshii T, Hirai T, Arai Y, Shinomiya K, Okawa A (2016) Impact of the surgical treatment for degenerative cervical myelopathy on the preoperative cervical sagittal balance: a review of prospective comparative cohort between anterior decompression with fusion and laminoplasty. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. doi:10.1007/s00586-016-4717-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Institutional Review Board approval, which was consistent with the Helsinki Declaration was approved by the Ethical Committee of Changzheng Hospital. Each case signed the informed consent before accepting the operation. No relevant financial activities outside the submitted work and no other potential conflicts.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
X. Liu and Y. Chen have made equal contribution to this article, and should be regarded as co-first author.
Bin Xu: Co-corresponding Author for this submitted manuscript.
Rights and permissions
About this article
Cite this article
Liu, X., Chen, Y., Yang, H. et al. The application of a new type of titanium mesh cage in hybrid anterior decompression and fusion technique for the treatment of continuously three-level cervical spondylotic myelopathy. Eur Spine J 26, 122–130 (2017). https://doi.org/10.1007/s00586-016-4888-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4888-3