Abstract
Introduction
Periprosthetic fractures after cemented hip replacement are a challenging problem to manage. Biomechanical studies have suggested the benefit of using locking screws for plate fixation, but there are concerns whether screws damage the cement mantle and promote crack propagation leading to construct failure.
Method
In this biomechanical study, different screw types were implanted into the cement mantle after pre-drilling holes of different sizes, in unicortical and bicortical configuration. The presence of cracks and the pull-out resistance of these screws were then evaluated.
Results
No unicortical screw induced cracks. Screws with a shortened tip, smaller flutes and double threads were significantly better for pull-out resistance. Bicortical screws were associated with a risk of local cement mantle damage, but also with a significantly greater holding power. By increasing the drill diameter, the onset of cracks decreased, but so does the pull-out resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic fractures are a serious complication after hip replacement and are the third most common reason for revision surgery after aseptic loosening and infection [1]. Minor trauma, such as a fall to the floor, is the most common cause after primary hip replacement [1], and the cumulative fracture risk lies between 1.0% for primary and 4% for revision total hip replacement [2, 3]. There is a rising incidence of such fractures due to the increasing lifespan of patients and continuing growth in numbers of primary and revision hip replacements being performed [4].
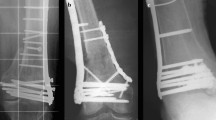
Surgical treatment can be either osteosynthesis with or without allograft bone augmentation and/or revision of the prosthesis depending on the position of fracture, implant stability and/or bone loss [3, 5–10]. There is a high rate of failure after periprosthetic fracture, due to malunion, refracture and stem loosening [11] and dislocation [12]. Biomechanical studies have shown that the internal fixation construct is more rigid if screws are used in the area of the stem for plate fixation instead of the traditional cables [13–15]. However, there are concerns that screws, penetrating the cement mantle, cause cracks which eventually lead to loosening of the construct [13–15].
The aim of this biomechanical study was to examine the effect of different screw implantation techniques on the integrity of the local cement mantle and the fixation strength of the screw. Different kinds of locking screws, LCS (Synthes, Oberdorf, Switzerland) and NCB (Zimmer, Warsaw, IN, USA), with or without a flattened tip, were implanted in unicortical and bicortical configurations and different core drill sizes were used.
Methods
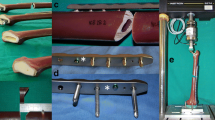
In order to simulate screw implantation in a cement mantle next to the stem of a hip arthroplasty, a 316-stainless steel rod, with an outer diameter of 12 mm, was implanted in the centre of a clear acrylic tube. The tube had an inner diameter of 24 mm and a wall thickness of 3.2 mm (Fig. 1a). The tube with a central guide screw was filled with vacuum mixed Palacos R+G bone cement (Heraeus, Wehrheim, Germany), and the steel rod was implanted over the central guide screw, leaving an equal 6 mm mantle. A lid was used to centre the top end of the rod in the acrylic cylinder and to pressurize the cement. For preventing the adherence of the cement onto the inner wall of the tube, a thin layer of high temperature silicone grease was applied. A custom made drill guide (Fig. 1b) was used to standardize the position of the drill holes (unicortical, bicortical, different drill sizes), and three drills of different diameter have been used. A 4.3 mm drill (manufacturer’s recommendation for the screw) was used as well as a 4.5 mm surgical drill (Synthes, Oberdorf, Switzerland) and a 4.8 mm standard mechanical drill. This amounted to an over drilling of the core diameter by −0.1, 0.1 and 0.4 mm. In one group, a tap was used additionally to the 4.3 mm drill. The drill was powered into the cement until its tip reached the metal tube or it penetrated the other side of the acrylic tube. Three different types of screws, all with a core diameter of 4.4 mm and an outer diameter of 5.0 mm, were used: locking head screws (LHS; Synthes, Oberdorf, Switzerland), periprosthetic locking screws (PPLS; Synthes, Oberdorf, Switzerland) and locking bolts for the non-contact bridging plate (NCB; Zimmer, Warsaw, IN, USA) (Fig. 2a). These screws were inserted unicortically and tightened with 4 nm using a torque wrench. An additional series of periprosthetic NCB screws (ppNCB) was tested with 2.5 mm off the tip removed to evaluate whether a flat tip would alter the pull-out resistance of these screws. The NCB screws were also tested bicortically (bNCB) as the NCB allows multidirectional (and hence bicortical) screw insertion.
Only new screws were used for each test. Each combination of drill and screw was tested eight times as this was the minimum number of test required regarding our power analysis.
The onset of cracks in the cement mantle was carefully monitored after drilling, tapping and screw insertion. The clear acrylic tube was then removed, and micro-cracks were quantified in numbers and length using a micrometre. Additionally, the inner cement integrity was examined using an arthroscope, following removal of the steel rod (Fig. 2).
The pull-out strength on the screws was measured using a universal testing-machine (Z020; Zwick/Roell, Ulm, Germany) and corresponding software (testXpert V10.11). The test setup was similar to the one previously described [16]. A custom made tool was created to encompass the head of the screw, while a custom designed frame, introduced into the steel tube, was used to fixate the cement tube against the axial pulling forces (Fig. 2b). The speed of the inclinator was 5 mm/min after applying 10 n of preload. The failure point was defined as the point prior to a sudden inflection in the curve of holding resistance due to loss of fixation.
Data were collected using Excel (Microsoft). The Mann–Whitney test was used to analyse differences in the pull-out strength, the Fisher exact test was used for the onset of cracks after screw implantation using SPSS 15 (SPSS, Chicago, IL, USA) with statistical significance as P < 0.05.
Results
Crack onset after screws insertion
Crack development could not be seen following the drilling of all drill diameters and configurations or after unicortical screw insertion. Cracks did occur during the implantation of bicortical screws or taps. These cracks were noted lateral to the screw in the cement mantle at the entry and at the exit hole of the screws, but in most cases (76.9%) the entry and exit hole were connected by the crack. By using a larger drill diameter (4.5 mm), the risk of crack occurrence was reduced from 62.5 to 37.5% and to 25% after drilling with a 4.8 mm drill (Fig. 3). While crack onset was reduced, the average crack length was similar; 10.82 (4.3 mm drill), 9.02 (4.5 mm drill) and 8.3 mm (4.8 mm drill).
In one tube, which could not be used for pull-out tests due to inhomogeneous cementation on the outside of the tube (air bubbles), the central metal rod was removed. Using the arthroscope, the penetration of the unicortical screws could be seen to be completely through the cement mantle. Small localized cracks were noted around the tip of the screw in some cases. Although the precise crack length could not be measured inside this hole, it never exceeded the diameter of the screw (Fig. 4a, b). In areas where a bicortical screw bypassed the stem, a white spot was noted. In some cases, the screw threads were visible, but no cracks larger than the diameter of the screw were found (Fig. 4c, d).
Arthroscopic views inside the cement mantle after removal of the inner metal tube. a Tip of the LCP screw; b tip of the PPLS; c white spot close to the area where a bicortical screw bypasses the stem; d open threads and smaller cracks in an area where a bicortical screw bypasses the stem. This was the largest damage which was seen from inside the cement mantle
Pull-out forces of different screws with standard drill sizes
A typical load/displacement curve is shown in Fig. 5. In general, the NCB screws showed a significant higher pull-out force than the LCP screws. Furthermore, the flat-tipped NCB screw (ppNCB) showed a statistically significant higher pull-out resistance than the standard NCB screw. Equally, the flat-tipped PPLS has higher resistance than the LCP. The median pull-out resistance of a bicortical implanted NCB screw (bNCB) was nearly double the median of the best unicortical screw (P = 0.002) (Fig. 6).
Pull-out forces with different drill sizes
Figure 7 summarizes pull-out resistance. Each field represents a type of screw. The special focus was on bicortical screws, as an increasing drill diameter reduces the onset of cracks. Increasing the drill size from 4.3 to 4.5 mm decreased the pull-out resistance by 23.6% (P = 0,043). Increasing the drill size to 4.8 mm reduced the resistance by 81.5% (P = 0,001). Tapping neither influenced the pull-out resistance nor reduced the likelihood of cracks forming.
The influence of cracks to the pull-out resistance was also investigated: A crack of the lateral wall had no influence on pull-out force of bicortical screws.
Discussion
Plates and intramedullary nails with and without bone grafting have been used as treatment options for osteosynthesis of periprosthetic femur fractures [17]. In early clinical studies, compression plates with screws implanted next to the femoral stem have shown promising results [18, 19], and recently biomechanical studies have demonstrated the benefits of locking plates [13–15]. Nevertheless, these studies focus on union of the fracture, and long term follow up looking at loosening of the stem has not been reported.
There are many factors such as patient age, bone quality, fracture pattern, cementing technique, stem design and type of osteosynthesis that influence the survival rate of the construct after periprosthetic fracture fixation. In this study, we investigated the cement mantel damage after screw implantation. Preliminary tests had shown a high rate of fractures in the cement, therefore we investigated whether a larger drill diameter could prevent the cement from cracking. The test cylinder was developed to simulate and standardize a cement mantle with a constant thickness around a stem (rigid metal cylinder). The outer acrylic plastic cylinder added stability and compression to the cement, while the holes were drilled and the screws implanted. Because the cylinder was transparent, the onset of cracks could be monitored.
We have shown that no cement damage occurs by inserting screws in unicortical configurations, but cement was damaged by implanting screws in a bicortical configuration. A larger drill diameter reduces this risk of cement mantle cracks but also reduces the pull-out resistance. The difference between a 4.3 and a 4.5 mm drill is not significant.
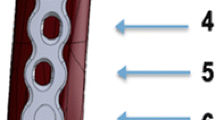
The difference in pull-out resistance differs between the screw designs. The LHS screw has single threads, three wide cutting flutes of 5.5 mm length and partial threads starting from 3.1 mm from the tip. The PPLS screw has the same core diameter of 4.4 mm, an outer diameter of 5.0 mm and single thread windings with a distance of 1.0 mm. The tip is flatted, the cutting flutes are only 3.1 mm long and first partial threads start already at 1.3 mm from the tip. Both screws are made of titanium. In a cement mantle of 6 mm, the difference in the number of full threads in the cement is 2.9 (PPLS) to 0.5 (LHS). The design of the NCB screw differs from the LHS in having smaller flutes and a double thread winding. In tests with ppNCB, the periprosthetic NCB screw was produced by filing off 2.5 mm of the tip, which we could show a significant improvement in pull-out resistance.
Other studies have focused on the tip design of self-tapping screws and could not find a reduced pull-out force or worsening of the lateral cortex by implanting screws with shorter flutes into femoral bone of human cadavers. In this study, screw tips with four flutes appear to be the ideal combination of low insertion torque and high pull-out force [16]. Following this, a screw design with a double thread, a short tip with four flutes would theoretically be a good compromise for unicortical screws, inserted next to a prosthesis stem.
The bicortical implanted bNCB had the most threads of all screws in the cement, showing by far the highest pull-out resistance, but also has a higher risk of damaging the cement mantle. Increasing the drill diameter from 4.3 to 4.5 mm reduces the onset of cracks and still leaves a 1.8 times higher pull-out strength than the unicortical screw.
There are limitations of this study. All tests were performed on cement without cortical bone surrounding it. Only direct pull-out forces were evaluated, while shear forces and rotational forces were excluded in this test setting. Further studies are planned to investigate what influence the screw damage to the mantle has on the initiation of loosening of these constructs.
In conclusion, unicortical screws can be implanted without damaging the cement. Bicortical screws have higher pull-out resistance but increase the risk of cement mantle damage. There is no benefit in tapping into cement. For implantation of bicortical screws, a 4.5 mm drill should be considered.
References
Lindahl H et al (2006) Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am 88(6):1215–1222
Berry DJ (1999) Epidemiology: hip and knee. Orthop Clin North Am 30(2):183–190
Learmonth ID (2004) The management of periprosthetic fractures around the femoral stem. J Bone Joint Surg Br 86(1):13–19
Lindahl H et al (2005) Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty 20(7):857–865
Bethea JSIII et al (1982) Proximal femoral fractures following total hip arthroplasty. Clin Orthop Relat Res 170:95–106
Brady OH et al (1999) Classification of the hip. Orthop Clin North Am 30(2):215–220
Brady OH et al (2000) The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty 15(1):59–62
Duncan CP, Masri BA (1995) Fractures of the femur after hip replacement. Instr Course Lect 44:293–304
Duwelius PJ et al (2004) A prospective modernized treatment protocol for periprosthetic femur fractures. Orthop Clin North Am 35(4):485–492, vi
Van Flandern GJ (2005) Periprosthetic fractures in total hip arthroplasty. Orthopedics 28(9 Suppl):s1089–s1095
Lindahl H et al (2006) Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br 88(1):26–30
Young SW et al (2007) Periprosthetic femoral fractures after total hip arthroplasty. ANZ J Surg 77(6):424–428
Fulkerson E et al (2006) Fixation of periprosthetic femoral shaft fractures associated with cemented femoral stems: a biomechanical comparison of locked plating and conventional cable plates. J Orthop Trauma 20(2):89–93
Dennis MG et al (2000) Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty 15(4):523–528
Schmotzer H, Tchejeyan GH, Dall DM (1996) Surgical management of intra- and postoperative fractures of the femur about the tip of the stem in total hip arthroplasty. J Arthroplasty 11(6):709–717
Yerby S et al (2001) Effect of cutting flute design on cortical bone screw insertion torque and pullout strength. J Orthop Trauma 15(3):216–221
Giannoudis PV, Kanakaris NK, Tsiridis E (2007) Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury 38(6):669–687
Serocki JH, Chandler RW, Dorr LD (1992) Treatment of fractures about hip prostheses with compression plating. J Arthroplasty 7(2):129–135
Cooke PH, Newman JH (1988) Fractures of the femur in relation to cemented hip prostheses. J Bone Joint Surg Br 70(3):386–389
Acknowledgment
This study was supported by the APOS (Asia Pacific Orthopaedic Symposium) research grant. We kindly thank Zimmer and Synthes who provided screws and cement for this study. We acknowledge the assistance of Albert Hansma and Rochelle Nicholls from Fremantle Hospital for their help at performing this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kampshoff, J., Stoffel, K.K., Yates, P.J. et al. The treatment of periprosthetic fractures with locking plates: effect of drill and screw type on cement mantles: a biomechanical analysis. Arch Orthop Trauma Surg 130, 627–632 (2010). https://doi.org/10.1007/s00402-009-0952-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-009-0952-3