Abstract
Introduction
Moore type II Entire Condyle fractures of the tibia plateau represent a rare and highly unstable fracture pattern that usually results from high impact traumas. Specific recommendations regarding the surgical treatment of these fractures are sparse. We present a series of Moore type II fractures treated by open reduction and internal fixation through a direct dorsal approach.
Patients and methods
Five patients (3 females, 2 males) with Entire Condyle fractures were retrospectively analyzed after a mean follow-up period of 39 months (range 12–61 months). Patient mean age at the time of operation was 36 years (range 26–43 years). Follow-up included clinical and radiological examination. Furthermore, all patient finished a SF36 and Lysholm knee score questionnaire.
Results
Average range of motion was 127/0/1° with all patients reaching full extension at the time of last follow up. Patients reached a mean Lysholm score of 81.2 points (range 61–100 points) and an average SF36 of 82.36 points (range 53.75–98.88 points). One patient sustained deep wound infection after elective implant removal 1 year after the initial surgery. Overall all patients were highly satisfied with the postoperative result.
Conclusion
The direct dorsal approach to the tibial plateau represents an adequate method to enable direct fracture exposure, open reduction, and internal fixation in posterior shearing medial Entire Condyle fractures and is especially valuable when also the dorso-lateral plateau is depressed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Moore type II Entire Condyle fractures of the tibial plateau represent a rare and highly unstable fracture pattern [1] that usually results from a high impact trauma and is only insufficiently covered by the OTA/AO- or the Schatzker classification [2, 3]. The fracture line of this shearing fracture starts in the opposite compartment of the knee and runs below the eminentia intercondylaris across the tibial head at a fracture angle of approximately 45° in the sagittal plane forming a large posterior condyle fragment. The corresponding collateral ligament, as well as one or both of the cruciates, are usually avulsed or ruptured. Specific recommendations regarding the surgical treatment of this fracture type are sparse. We present a series of medial Moore type II fractures treated by open reduction and internal fixation through a direct posterior approach.
Materials and methods
The presented consecutive case–control study was performed with the approval of our institution’s human subjects review board.
Between 2003 and 2007 five patients (3 females, 2 males) with medial Entire Condyle fractures were treated in our department (Table 1) by one fellowship trained trauma surgeon. The patients were retrospectively identified by searching our local trauma-database. The mean follow-up period was 39 months (12–61) with no patient being lost to follow up. Patients mean age at the time of the operation was 36 years (26–43 years). Pre- and postoperative plain X-rays as well as preoperative CT-scans from all patients were obtained. Patient charts were then reviewed to determine demographic data and the mechanism of injury including associated injuries concerning collateral and cruciate ligaments and the soft tissue.
All injuries resulted from high-energy traumas including a fall from an elevated height (1 patient), and sport related injuries (4 patients). Compartment syndrome was not diagnosed in any of the cases.
Patients were asked to participate in the study by phone and mail. Once written consent was obtained follow-up X-rays were made. Clinical follow-up examination included range of motion, stability of the joint and range of walking. Patients were also asked about their satisfaction with the postoperative results and their ability to return to their previous employment. Finally, all patients completed two validated and reliable clinical outcome measurement scores, the SF36 general health survey [4] and the Lysholm rating score in order to evaluate the outcome after knee ligament injuries [5].
Radiological analysis
Radiological analysis of postoperative reduction was performed by two trauma surgery residents with several years of experience in radiological assessment of proximal tibia fractures and not related to the initial treatment. As recommended by several authors [6–8], a step or gap of less than 2 mm in the frontal or the sagittal plane was considered as a satisfactory articular reduction. Furthermore, a proximal medial tibial angle of 87° (±5°) and a condylar width of less than 5 mm on the frontal plane and a posterior proximal tibial angle of 81° (±5°) on the sagittal plain was considered as a satisfying alignment. Both raters were blinded towards the outcome of the clinical follow-up examination.
In cases the raters were discordant on the quality of reduction or alignment the X-rays were discussed until both raters agreed about all points of the evaluation.
Surgical technique
The patient is placed in prone position on a radiolucent table under general anaesthesia with the knee held in slight flexion. Tourniquet is on the discretion of the surgeon but has not been used in the cases presented here. A single shot application of 2 g cefazolin is performed.
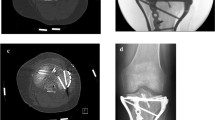
A S-shaped incision is made starting over the proximal medial head of the gastrognemic muscle and crossing the popliteal fossa as shown in Fig. 1a.
After sharp dissection of the subcutaneous tissue the popliteal fascia is incised preserving the small saphenous vein as well as the medial sural cunateous nerve. The medial head of the gastrognemic muscle is then mobilized and retracted laterally.
The oblique tendinous expansion of the semimembranosus tendon is identified and retracted medially. The superior border of the popliteal muscle is identified and the muscle is dissected subperiostally until the posterior-medial spike part of the fracture is exposed (Fig 1b). An arthrotomy is performed to assess the reduction of the articular surface at the level of the main fracture.
If a posterolateral impression zone in the remaining lateral fragment is present it can be elevated with e.g. an elevator through the fracture. To get access to the posterolateral plateau flexion has to be increased and the medial condyle fragment has to be medialized using a bone retractor. Structural support using bone graft and maintaining reduction with a k-wire are necessary before the main posteromedial fragment is reduced under full extension.
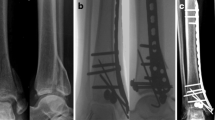
After preliminary fixation of the fragment using k-wires reduction is controlled by fluoroscopy in the frontal and lateral view. At this point a dorsal 3.5 mm anti-gliding plate as a buttress plate is placed to stabilize the fragment and compression is applied by placing compression screws in posterior–anterior direction.
Avulsion fractures of the anterior cruciate ligament are reduced in prone position under fluoroscopic control and the eminentia intercondylaris fragment is stabilized with an anterior–posterior lag screw depending on the fragment type which is inserted through an anterior stab incision with the knee in flexion. Wound closure includes repair of the capsule and the deep fascia as well as subcutaneous and skin closure.
Postoperative treatment
Postoperatively all patients were mobilized under 15 kg of weightbearing for 6 weeks. A continous passive motion device (Kinetec®) was used from the first postoperative day onwards. In addition, active-assisted range of motion exercises were started as soon as the wounds were sealed and dry and a daily injection of 5,000 IU low molecular heparin was applied to prevent deep vein thrombosis. Radiological and clinical follow-up examinations were conducted 6 and 12 weeks after surgery. After 12 weeks all patients showed a good radiological fracture healing, and as a result, were able to be mobilized under full weight bearing.
Results
The operation was performed at an average of 4.6 days (1–11 days) after the injury. Three patients had avulsion fractures of the distal anterior cruciate ligament (ACL) which were stabilized with anterior–posterior lag screws (Fig. 2). In one case an arthroscopy was performed as the articular surface could not adequately be assessed through the posterior arthrotomy.
Radiological analysis showed satisfying postoperative reduction in four cases. One patient had a step of 3 mm in the articular joint level at the anterior–posterior X-ray indicating an insufficient reduction according to our criteria.
One patient complained about chronic irritation of the soft tissue, therefore implant removal was performed 1 year after the primary surgery. Another patient sustained a deep wound infection after implant removal in an external institution 1 year postoperatively. After surgical revision the wound healed without complication. This patient had sustained a tibia shaft fracture treated by intramedullary nailing 4 years before the tibia plateau fracture. The nail had been removed 1 year later. At the time of the last follow up the patient complained about paresthesia at the area of the scar tissue as well as a limited walking range of 2 km. Clinical examination showed an instability of the ACL and a valgus instability due to an elongated MCL. The patient stated she was highly satisfied with the postoperative results and refused to undergo further reconstructive surgery.
One patient complained about a walking range limited to 2 km due to pain in the contralateral knee. At the time of the last follow up the mean range of motion was 127/0/1° with all patients reaching full extension (Table 2). Three of the five patients achieved unlimited range of walking and showed no clinical signs of joint instability during the last follow-up examination. At the time of the last follow up all patients had returned to their prior employments and were able to participate in weekly sports exercises.
The mean Lysholm score was 81.2 points (61–100 points) with the average SF36 being 82.36 points (53.75–98.88 points) (Table 3). All patients stated they were highly satisfied with the surgical result.
Discussion
Open reduction and internal fixation of tibial plateau fractures can be a challenging procedure. These fractures frequently result from high energy traumas, therefore secondary injuries, such as compartment syndromes, ruptured ligaments and soft tissue defects, are common [9–11]. In addition, infection rates between 12 and 87.5% have been reported in the literature [6, 12, 13].
Fractures of the anterior and lateral aspect of the tibial plateau and undisplaced posterior fragments can usually be stabilized through a standard anterolateral approach [1, 14, 15]. In contrast, the fracture type presented in this series represents a highly unstable injury with a large posteromedial condyle fragment prone to posterior shearing and the risk of popliteal vessel injury. Operative treatment of this type of fracture requires direct exposure and posterior stabilisation [16–18].
The surgical approach used in this study is based on a technique which was first described by Galla and Lobenhofer [19] in the German literature and which was recommended to perform reduction and stabilization of mono-condylar Moore type I “medial splint” fractures. In 2007, Fakler et al. [20]. translated this procedure into the English language. In the experience of the authors, through the presented approach even limited access to impressions in the postero-lateral tibial plateau can be addressed by medial displacement of the Entire Condyle fragment.
In fracture patterns not including impressions of the lateral plateau, the commonly used dorso-medial approach, as described by Galla and Lobenhofer [19], may be sufficient to perform open reduction and internal fixation of the Entire Condyle fragment.
Until recently only few case reports [19, 20] about postoperative results after the use of this approach have been published.
In order to enable direct exposure of the posterior part of the tibial head several other surgical approaches [16–18, 21] have been proposed. In 1968, Trickey [21] described a technique of longitudinal splitting of the medial gastrognemic muscle and the dissection of the neurovascular bundle. In the treatment of seven Moore type I “medial splint” fractures, De Boeck and Odecamp [18] described an excessive dorsal approach to the tibia head and a detachment of the proximal insertion of the medial gastrognemic and the popliteus muscles. After a mean follow-up of 6.8 years an average extension lack of 7° was observed. In 2005, Bhattacharyya et al. [16]. presented 13 cases of posterior shearing fractures treated by the same technique. The postoperatively range of motion was limited up to 10° of flexion for 2–3 weeks.
Even though satisfying anatomic reduction could be achieved in 10 of the 13 patients, a permanent lack of extension was observed in six cases.
Carlson [17] presented a series of five patients with posterior shearing bicondylar fractures of the tibial plateau. Reduction and fixation was performed through a combined dorso-medial and dorso-lateral approach. A medial splitting of the semimembranous tendon and the popliteus muscle as well as a lateral detachment of the popliteal tendon became necessary. Postoperatively an average extension deficit of 2° (range 0°–5°) was observed. One patient developed a deep vein thrombosis while another patient suffered from transient peroneal nerve palsy. Compared with these data, the direct dorsal approach as used in our series represents a soft tissue preserving technique indicating a good clinical outcome at an average follow up of 39 months.
Partenheimer et al. [22]. reported 68 cases of patients with bilateral tibial head fractures who were prospectively followed over a period of 11–13 months. The patients achieved an average Lysholm score of 87 points at the time of the last follow up. Gerich et al. [23]. evaluated the postoperative results of 168 patients younger than 60 years who were treated by antero-lateral approach and fixation for tibial plateau fractures. After a mean follow-up period of 4.2 years, the patients achieved an average Lysholm score of 78.3 points. In our series the patients achieved a mean Lysholm score of 81.2 points representing a satisfying results compared to the data published in the literature and especially in consideration of the complex fracture type.
Based upon published material to date, the SF36 health survey [4] has not been used in outcome studies dealing with fractures of the tibia plateau, therefore a direct comparison of our results with other outcome series is not possible at this time.
However, compared to the age and gender matched norm values of the SF36 as published by Bullinger and Kirchberger [4] three of the five patients achieved a better mean score than the corresponding healthy norm population. Overall, our patient collective achieved a better SF36 than the healthy German total population in 2003. In conclusion, the patient’s subjective general health status has not significantly been influenced by the prior injury. The major limitations of this study are the low number of patients and the retrospective character as well as the short follow up which does not allow us to address posttraumatic osteoarthritis.
In summary, open reduction and internal fixation was adequately possible through the direct dorsal approach and the early clinical results are promising.
The presented approach is especially valuable in cases were also the dorso-lateral plateau is depressed. In fracture patterns not including impressions of the lateral plateau, the commonly used dorso-medial approach, may be sufficient to perform open reduction and internal fixation of medial Entire Condyle fragments.
References
Moore TM (1981) Fracture-dislocation of the knee. Clin Orthop Relat Res 156:128–140
Müller M, Nazarian S, Koch P, Schatzker J (1990) The comprehensive classification of fractures of long bones. Springer, Berlin, pp 120–121
Schatzker J, McBroom R, Bruce D (1979) The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res 138:94–104
Bullinger M, Kirchberger I (1998) SF36 questionnaire concerning health status. Hogrefe, Göttingen
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154. doi:10.1177/036354658201000306
Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK (2006) Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am 88(8):1713–1721
Blokker CP, Rorabeck CH, Bourne RB (1984) Tibial plateau fractures. An analysis of the results of treatment in 60 patients. Clin Orthop Relat Res 182:193–199
Brown TD, Anderson DD, Nepola JV, Singerman RJ, Pedersen DR, Brand RA (1988) Contact stress aberrations following imprecise reduction of simple tibial plateau fractures. J Orthop Res 6(6):851–862
Colletti P, Greenberg H, Terk MR (1996) MR findings in patients with acute tibial plateau fractures. Comput Med Imaging Graph 20(5):389–394
Dirschl DR, Del Gaizo D (2007) Staged management of tibial plateau fractures. Am J Orthop 36(Suppl 4):12–17
Stallenberg B, Gevenois PA, Sintzoff SA Jr, Matos C, Andrianne Y, Struyven J (1993) Fracture of the posterior aspect of the lateral tibial plateau: radiographic sign of anterior cruciate ligament tear. Radiology 187(3):821–825
Moore TM, Patzakis MJ, Harvey JP (1987) Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma 1(2):97–119
Young MJ, Barrack RL (1994) Complications of internal fixation of tibial plateau fractures. Orthop Rev 23(2):149–154
Fernandez DL (1988) Anterior approach to the knee with osteotomy of the tibial tubercle for bicondylar tibial fractures. J Bone Joint Surg Am 70(2):208–219
Schatzker J (1988) Fractures of the tibial plateau, vol 1. Lippincott, Philadelphia, pp 421–434
Bhattacharyya T, McCarty LP 3rd, Harris MB, Morrison SM, Wixted JJ, Vrahas MS, Smith RM (2005) The posterior shearing tibial plateau fracture: treatment and results via a posterior approach. J Orthop Trauma 19(5):305–310
Carlson DA (2005) Posterior bicondylar tibial plateau fractures. J Orthop Trauma 19(2):73–78
De Boeck H, Opdecam P (1995) Posteromedial tibial plateau fractures. Operative treatment by posterior approach. Clin Orthop Relat Res 320:125–128
Galla M, Lobenhoffer P (2003) The direct, dorsal approach to the treatment of unstable tibial posteromedial fracture-dislocations. Unfallchirurg 106(3):241–247
Fakler JK, Ryzewicz M, Hartshorn C, Morgan SJ, Stahel PF, Smith WR (2007) Optimizing the management of Moore type I postero-medial split fracture dislocations of the tibial head: description of the Lobenhoffer approach. J Orthop Trauma 21(5):330–336. doi:10.1097/BOT.0b013e318055603c
Trickey EL (1968) Rupture of the posterior cruciate ligament of the knee. J Bone Joint Surg Br 50(2):334–341
Partenheimer A, Gosling T, Muller M, Schirmer C, Kaab M, Matschke S, Ryf C, Renner N, Wiebking U, Krettek C (2007) Management of bicondylar fractures of the tibial plateau with unilateral fixed-angle plate fixation. Unfallchirurg 110(8):675–683
Gerich T, Blauth M, Witte F, Krettek C (2001) Osteosynthesis of fractures of the head of the tibia in advanced age. A matched-pair analysis. Unfallchirurg 104(1):50–56
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brunner, A., Honigmann, P., Horisberger, M. et al. Open reduction and fixation of medial Moore type II fractures of the tibial plateau by a direct dorsal approach. Arch Orthop Trauma Surg 129, 1233–1238 (2009). https://doi.org/10.1007/s00402-009-0841-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-009-0841-9