Abstract
Purpose
The purpose of this study was to evaluate the outcome of Ilizarov external fixation (IE) versus dynamic compression plate (PO) in the management of extra-articular distal tibial fractures.
Methods
Between 2010 and 2011, extra-articular distal tibial fractures in 40 consecutive patients met the inclusion criteria. They were classified according to AO classification fracture type A (A1, A2, and A3). In a randomized method, two equal groups were managed using either IE or PO. PO was performed using open reduction and internal fixation (ORIF) and DCP through anterolateral approach. IE was done using Ilizarov frame. For the PO group, non-weight bearing ambulation was permitted on the second postoperative day but partial weight bearing was permitted according to the progression in union criteria clinically and radiologically. For the IE group, weight bearing started as tolerated from the first postoperative day. Physiotherapy and pin-site care was performed by the patient themselves.
Results
Modified Mazur ankle score was applied to IE (excellent 10, good 10) and in PO (excellent 2, good 8, poor 6). Data were statically analysed using (Mann–Whitney test). The rate of healing in the IE group (average 130) was higher than the PO (average 196.5); plus, there were no cases of delayed union or nonunion in the IE group (p value 0.003).
Conclusion
It was found that IE compared with PO provides provision of immediate weight bearing as tolerated following postoperative recovery, irrespective of radiological or clinical healing with no infection, deformity or non-union.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal tibial fracture remains one of the most common fractures of long bones. This fracture may be caused by bending and rotational forces. Because of thin skin and less soft tissue coverage, open fracture and liability to infection with sloughing of the skin are more common in this type of fracture. When conservative treatment is inappropriate, several methods of surgical management could be used [1, 2]. Open reduction and internal fixation (ORIF) provides stability, but it often requires extensive soft-tissue dissection, further devascularization of the bone fragments with higher rates of complications and secondary surgery. Minimally invasive percutaneous plate osteosynthesis (MIPPO) showed high rates of healing and low rate of soft-tissue complications [3]. Closed intramedullary nailing (IMN) presents itself as a treatment option that preserves the extra osseous blood supply, fracture haematoma and maintains the integrity of the soft tissue envelope [4]. Some comparative studies have been published about ORIF, MIPPO, and IMN [2–4].
In our country, generally speaking, ORIF using dynamic compression plate (DCP) remains preferable for its familiar experience and low cost management of such fractures compared to Ilizarov external fixation (IE). To our knowledge, there is no study in the English literature about the use of IE in the management of extra-articular distal tibial fractures, or a comparative study with conventional plate osteosynthesis (PO).
In this study we prospectively compared the use of PO and IE as initial and definitive management of post traumatic extra-articular distal tibia fracture in adults.
Materials and methods
The cohort consisted of 40 consecutive patients treated by the authors at Manchiet El-Bakry and El-Fayoum General Hospitals between 2010 and 2011. Their data were collected prospectively and the study was approved by the ethical committee. There were 26 men and 14 women, with a mean age of 28.6 years (range 20–40). Patients were immobilized in an above knee back slab before surgery. The right leg was affected in 28 patients and the left in 12. The injuries were caused by a motor car accident in 20 patients, a motorcycle accident in four, an automobile–pedestrian accident in 11 and fall from a height in five. All patients were prepared pre-operatively as poly-trauma patients to be sure that they were vitally stable. Examination for abrasion, bruises, contusion, laceration, neurovascular injury and radiological investigation was done and classified according to AO classification fracture type A (A1, A2, and A3). All patients were manual workers from El-Fayoum governorate (103 km south-east of Cairo). PO cases were done in El-Fayoum General Hospital while IE was done in Manchiet El-Bakry General Hospital in Cairo (non-paid). The inclusion criteria were patients between 20 and 40 years old, with extra articular distal tibial fracture which was: closed or open grade I (GI) according to Gustilo and Anderson classification (GAC), and type “A” fracture according to AO classification (Table 1).
All patients had pre-operative explanation of full details about their condition, operative details and postoperative instructions. They had been consented to be included in this study and to undergo either PO or IE in a randomized method.
Surgical technique
All surgeries were done under spinal anaesthesia. Pre-operative parental antibiotics (first generation cephalosporin) were administrated one hour pre-operatively, and tourniquet used for the group of PO. PO was performed using ORIF and DCP through an anterolateral approach. We used Ilizarov frames of stainless steel material, consisting of three rings only for all patients, with 1.8-mm k-wire and 3.5-mm Schanz. In six cases we added calcaneal 5/8-ring. Reduction was possible in PO using ORIF. In the IE group, we used manual traction or distraction techniques or olive wires of IE itself or aided by percutaneous mobilization using Steinmann pins, assisted by an image intensifier.
Postoperative instructions
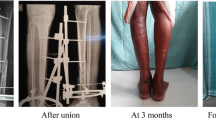
For the PO group, non-weight bearing ambulation was permitted on the second postoperative day, with hospital discharge in a below knee back slab, removed temporarily in the first two weeks to check the wound and forsuture removal, then once daily for free mobilisation during the next two weeks, finally it was removed completely if pain subsided with active knee and ankle ROM. Because of low socioeconomics, postoperative physiotherapy was done by patients themselves in the form of active range of motion for knee and ankle joints. This was done immediately in the IE group, and gradually after suture removal in the PO group. Partial weight bearing was permitted according to the progression in union criteria clinically and radiologically. For the IE group, weight bearing started as tolerated from the first postoperative day (Fig. 1). Continuous pin-site care was performed by the patient himself and checked regularly at every visit.
A 28-year-old male, presented with A1 extra-articular fracture left tibia and fibula treated with Ilizarov external fixation (IE). A AP and lateral radiographs of post traumatic fracture left leg bones. B AP and lateral radiographs of postoperative Ilizarov application C. AP radiograph after Ilizarov removal D. Lateral radiograph after Ilizarov removal E. Clinical photo during last follow up
Post hospital discharge, the follow-up visit for both groups was weekly in the first month, bimonthly in the second month, monthly up to the sixth month and every three months till the end of the follow-up period. Urgent calls and visits were available if needed. In each visit, the patients were assessed clinically, functionally, and radiographically for union, infection, deformity, leg-length discrepancy, knee and ankle ROM, return to previous job, return to previous activity, sports practice, complications, and need for secondary procedures.
By the end of follow up, all clinical, functional and radiological outcomes were compared between the immediate postoperative and final visit. Radiographic union was considered if mature callus bridging of at least three of four cortices on two orthogonal [5] views and clinically if the patient had painless full weight bearing.
Results
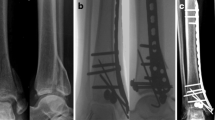
The time from trauma to surgery ranged from 45 to 71 hours (mean 58.6 hours) for PO and from 54 to 90 hours (mean 72.4 hours) for IE. The main cause for the extended period before surgery was financial support. The longer period for the IE group was related to logistics for budget and transportation from El-Fayoum to Cairo. Operative time ranged from 90 to 110 minutes (average 85 minutes) for the PO group and from 120 to 180 minutes (average 140 minutes) for the IE group. No major intra-operative complications were encountered. Hospital stay ranged from one to three days (mean 1.3 days) in IE and from two to five days (mean 3.4) in PO. The mean follow up was 26 months (18–36 months). In the PO group, two cases developed superficial infection and two hardware failures. In both groups all wounds healed smoothly without deep infection. Pin-site inflammation was recorded in all cases of the IE group. Pin-site infection was also common. It occurred in more than four sites in six patients. All cases had been controlled via oral or parental first generation cephalosporin with no deep infection. All fractures united without any secondary procedures to achieve union, except two metal failures in the PO group. Postoperative X-ray revealed acceptable reduction, and the last follow-up X-rays showed no indication for deformity correction. All patient had PO progressed union in an average healing time of 196.5 days (161–273) (Fig. 2) and 130 days for the IE (110–150) group. The clinical evaluation was performed using the modified Mazur ankle score [6], based on clinical examination of the injured extremity and rated as excellent, good, poor and fair (Table 2). Results were excellent in two cases, good in eight cases, fair in four cases and poor in six cases of the PO group, while in the IE group it was excellent in ten cases and good in ten cases (Table 3).
A 30-year-old male presented with A1 extra-articular fracture of the right tibia and fibula treated with conventional plate osteosynthesis (PO). A AP and lateral radiograph of post traumatic fracture of lower leg bones. B AP, oblique and lateral radiographs of postoperative fracture fixation using conventional plating. C AP, oblique and lateral radiographs at last follow up after 213 days and results were good
Statistical analysis
Data were statically analysed, whereby comparison of variables between the study groups was done using Mann–Whitney test. For comparing the two groups, a probability value (p value) less than 0.05 was considered statically significant. The rate of healing in the IE group (average 130) was higher than the PO (average 196.5) (Fig. 3.); plus, there were no cases of delayed union or nonunion in the IE group (p value 0.003).
Discussion
A wide range of treatment modalities are indicated for management of extra-articular distal tibial fractures either by IMN, PO or external fixation. Janssen et al. [7] compared the use of PO and IMN in extra-articular distal tibial fractures. The average hospital stay was 9.5 days for PO and 9.8 days for IMN, while in our study it was 3.5 days in PO and 1.3 days in the IE group. Janssen reported that the average time for radiological union was 133 days for PO and 147 days for IMN. In our study, it was 196.5 days in PO and 130 days in IE. Regarding time to weight bearing, it was after 3.8 and 3.3 months in PO and IMN, respectively. While in our IE group weight bearing was as tolerated from the first day postoperative, in the PO group it was after bone union (6.5 months). Patients with IE were permitted to return to work as early as possible, while those who underwent PO or IMN had to wait for six months as reported by Janssen et al. Lee et al. [8] reported a comparative study between locked and unlocked IMN and had 6.1 % mal-union and recommended that distal third fracture tibia treated with IMN showed a trend of increased mal-union rate when compared to middle third fractures (P = 0.06). He also reported four cases on nail migration in the unlocked group and two cases had broken distal locking screws in the locked group. At last follow-up there was no indication for mal-union correction in both groups but two cases of metal failure in the PO group that had been treated by IE.
Major complications following IMN include infection, compartment syndrome, venous thrombo-embolic events, fat embolism syndrome, neurovascular damage and non-union [9]. Brown et al. [10], in their study about knee pain after IMN, showed that functional impairment was in 91.8 % of patients experiencing pain on kneeling and 33.7 % having pain even at rest. Keeting et al. [11] reported in his study about IMN in tibial fracture that 80 % of patients required nail removal. Chronic knee pain after IMN remains a troublesome complication regardless of the surgical approach used, ranging from 5 to 86 %. Removal of the nail failed to eliminate the pain, which according to some persisted in as many as 69 % at an average of 1.5 years [12]. We had no case with anterior knee pain. Another operation is required for metal removal either in the IM nailing or PO groups, while in IE removal of the frame had been done as an outpatient procedure. Plate fixation is effective in stabilizing distal tibia fractures but conventional techniques involve extensive dissection and periosteal stripping, which increase the risk of soft tissue complications [13]. No study has specifically evaluated the clinical outcomes of conventional plating techniques in the management of nonarticular distal tibia fractures [13], but Vallier et al. [14] launched a retrospective comparative study between PO and IMN for 111 patients with extra-articular distal tibia fractures (76 were treated with IMN and 37 were treated with PO). Osteomyelitis developed in 5.3 % treated by IMN and 2.7 % after PO, 12 % had delayed union or nonunion after IMN and 2.7 % had a nonunion after plating (P = 0.10). Bach et al. [15] compared the use of external fixator and plate in 59 patients with distal tibia open fracture types II and III, and there were 19 % of patients complicated by severe osteomyelitis, and 11.5 % had plate fixation failure which required an external fixator, while only one case of the external fixator group reported osteomyelitis. We reported no deep infection or osteomyelitis in both groups. Pin-site infection in IE and two cases of superficial infection in the PO group was successfully treated with local dressing, oral or parental first generation cephalosporin. Ristiniemi et al. [16] reported a retrospective comparative study between IMN and external fixator in the distal tibial fracture. The healing time was 21 and 23 weeks in the IMN and external fixator groups, respectively (P = 0.53), while in our study the mean healing time was 18.5 and 28 weeks in IE and PO groups, respectively (P = 0.003). Conventional plating of distal tibial fractures has been associated with high rates of infection and soft-tissue complications requiring revision surgery [17, 18]; however these outcomes have been attributed to the extensile exposure and soft-tissue dissection required with conventional AO plating techniques [13].
Some authors reported that the fracture closed to the plafond is difficult to stabilize using IMN or PO. PO has a higher complication rate, particularly infection, hardware prominence, malalignment, and loss of alignment. Some of the complications may reflect the techniques that were used and should decrease with more experience; however, some may be inherent in the treatment of high-energy fractures using PO [19]. Bach et al. [15] recommended that external fixators should be the primary method of stabilization for Grades II and III open tibial shaft fractures. Hosny and Fadel [20] treated 34 open tibial fracture (GI, II & III) using IE. Twenty-eight patients graded as excellent and good results, one fair, and one poor. They recommended use of IE as initial and definitive treatment for such fractures (Table 4).
We found that IE provides provisions of immediate weight-bearing as tolerated following postoperative recovery, irrespective of radiological or clinical signs of healing with no need for secondary surgical interference for management of non-union, mal-union or infection. Consequently, the present study as well as that of Phisitkul [19], Bach et al. [15], Hosny and Fadel [20], we recommend further research in using IE in different grade II and III open fracture tibia. According to the results of this prospective randomized comparative study, we found that use of IE is recommended over PO in management of extra-articular distal tibial fracture.
References
Newman SD, Mauffrey CP, Krikler S (2011) Distal metadiaphyseal tibial fractures. Injury 42(10):975–984
Coles CP, Gross M (2000) Closed tibial shaft fractures: management and treatment complications. A review of the prospective literature. Can J Surg 43:256–262
Oh CW, Kyung HS, Park IH et al (2003) Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res 408:286–291
Hoenig M, Gao F, Kinder J et al (2010) Extra-articular distal tibia fractures: a mechanical evaluation of 4 different treatment methods. J Orthop Trauma 24(1):30–35
Shisha T (2010) Parameters for defining efficacy in fracture healing. Clin Cases Miner Bone Metab 7(1):15–16
Teeny SM, Wiss DA (1993) Open reduction and internal fixation of tibial plafond fractures variables contributing to poor results and complications. Clin Orthop Relat Res 292:108–117
Janssen KW, Biert J, Kampen A (2007) Treatment of distal tibial fractures: plate versus nail. Int Orthop 31(5):709–714
Lee YS, Lo TY, Huang HL (2008) Intramedullary fixation of tibial shaft fractures: a comparison of the unlocked and interlocked nail. Int Orthop 32:69–74
Mahmood A, Kumar G (2014) Review of the treatment of distal tibia metaphyseal fractures; plating versus intramedullary nailing: a systematic review of recent evidence. Foot Ankle Surg 20(2):151
Court-Brown CM, Gustilo T, Shaw AD (1997) Knee pain after intramedullary nailing: its incidence, etiology, and outcome. J Orthop Trauma 11:103–105
Keating JF, Orfaly R, O’Brien PJ (1997) Knee pain after tibial nailing. J Orthop Trauma 11:10–13
Katsoulis E, Court-Brown C, Giannoudis PV (2006) Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg (Br) 88:576–580
Bedi A, Le TT, Karunakar MA (2006) Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg 14(7):406–416
Vallier HA, Le TT, Bedi A (2008) Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma 22(5):307–311
BACH AW, Hansen ST Jr (1989) Plates versus external fixation in severe open tibial shaft fractures: a randomized trial. Clin Orthop Relat 241:89–94
Ristiniemi J, Luukinen P, Ohtonen P (2011) Surgical treatment of extra-articular or simple intra-articular distal tibial fractures: external fixation versus intramedullary nailing. J Orthop Trauma 25(2):101–105
Richard RD, Kubiak E, Horwitz DS (2014) Techniques for the surgical treatment of distal tibia fractures. Orthop Clin North Am 45(3):295–312
Schurz M, Binder H, Platzer P et al (2010) Physeal injuries of the distal tibia: long-term results in 376 patients. Int Orthop 34(4):547–552
Phisitkul P, McKinley TO, Nepola JV et al (2007) Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma 21(2):83–91
Hosny G, Fadel M (2003) Ilizarov external fixator for open fractures of the tibial shaft. Int Orthop 27(5):303–306
Acknowledgments
We would like to acknowledge the LRS.PD program. Professional Diploma in Limb Reconstructive Surgery and Correction of Deformity (LRS.PD) is organized by the Arab Institute for continuing professional development (AICPD) in association with the Pan Arab Orthopaedic Association (PAOA) and scientific support of the International Orthopedic Association (SICOT).
Conflict of interest
There are no conflicts of interest associated with this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fadel, M., Ahmed, M.A., Al-Dars, A.M. et al. Ilizarov external fixation versus plate osteosynthesis in the management of extra-articular fractures of the distal tibia. International Orthopaedics (SICOT) 39, 513–519 (2015). https://doi.org/10.1007/s00264-014-2607-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2607-4