Abstract
Background
Fracture healing is affected by the type and the magnitude of movements at the fracture site. Mechanical conditions will be a function of the type of fracture management, the distance between the fracture fragments, and the loading of the fracture site. The hypothesis to be tested was that the use of a larger-diameter intramedullary nail, together with compressed interlocking, would enhance the primary stiffness and reduce fracture site movements, especially those engendered by shearing forces.
Materials and methods
Six pairs of human tibiae were used to study the influence on fracture site stability of two different diameters (9 and 11 mm) of intramedullary nails, in tension/compression, torsional, four-point bending, and shear tests. The nails were used with two interlocking modes (static interlocking vs. dynamic compression).
Results
With static interlocking, the 11-mm-diameter nail provided significantly (30–59%) greater reduction of fracture site movement, as compared with the 9-mm-diameter nail. Using an 11-mm-diameter nail, the stiffness of the bone-implant construct was enhanced by between 20 and 50%. Dynamic compression allowed the interfragmentary movements at the fracture site to be further reduced by up to 79% and the system stiffness to be increased by up to 80%.
Conclusion
On biomechanical grounds, the largest possible nail diameter should be used, with minimal reaming, so as to minimize fracture site movement. Compression after meticulous reduction should be considered in axially stable fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The course of fracture healing and the outcome of fracture management are, to a large extent, governed by the mechanical conditions at the fracture site [5, 6]. These conditions are a function of the stiffness of the construct used, the width of the fracture gap, and the nature and size of the external loads applied. In previous studies, little account was taken of shear, even though the shearing forces acting on the bones during common daily activities of walking and stair-climbing can be considerable, ranging up to 1.3 times body weight (BW) [22]. Biomechanically, some of the devices commonly used in fracture management are less than ideal because of the interfragmentary shear forces allowed by their designs. The resulting insufficient stiffness of the construct can contribute to delayed fracture healing.
Over the past years, intramedullary (IM) nailing has become an established technique for the surgical management of tibial shaft fractures. Apart from unreamed IM devices, reamed interlocked systems are becoming increasingly popular. Gradual reaming of the tibial medullary cavity allows larger-diameter devices to be inserted [12]. This should enhance the stability of the fixation, and reduce micromovements at the fracture site. Also, contemporary IM implants offer a variety of interlocking and/or compression options, which will affect the geometry and the stability of the overall system [4]. Choosing the correct implant length, diameter, and interlocking mode is particularly important in the management of unstable fractures of the tibial shaft. Previous biomechanical studies [18, 19] have concentrated on a comparison of different nail systems, with less attention being paid to a search for the optimum system parameters.
The present study was conducted to comprehensively investigate the influence of the nail diameter, in conjunction with the appropriate interlocking mode, on the primary stability of tibial shaft fractures. Therefore, the stiffness of the bone-implant construct and the resulting fracture site movements were to be studied under loading conditions chosen to reflect as closely as possible the physiological stress patterns of IM constructs.
The hypothesis to be tested was that the use of a larger-diameter IM nail, together with compressed locking, would enhance the primary stiffness and reduce fracture site movements, especially those engendered by shearing forces.
Materials and methods
The study was performed on six pairs of human tibiae (length: 362–439 mm, age range 25–54 years, mean ± SD: 46 years ± 9 years, male). The bones had been removed at autopsies, with the consent of the next of kin of the deceased and in compliance with the local legislation governing autopsies. Following removal, they were stripped of soft tissues down to the periosteum, wrapped in saline-soaked towels, and stored at −70°C. In each bone pair one site was randomly assigned to receive static interlocking (STAT) or compression locking (COMP).
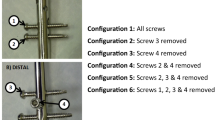
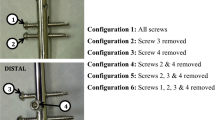
All the specimens were first fitted, under image intensifier control, with a 9-mm-diameter T2 IM nail (Stryker, Düsseldorf, Germany), following the manufacturer’s instructions [21]. Distally all nails were locked with three screws using a free-hand technique. Proximally, two different interlocking modes were used depending on the group assignment. In the STAT group, static interlocking was performed using two screws. In the COMP group, the first interlocking screw was inserted through the slot hole (dynamic interlocking) and additionally fixed with a second interlocking screw. A full-length radiograph of the bone-implant (B–I) construct was obtained to document the correct position of the nail in the medullary cavity.
All the tibiae were initially subjected to the test series described below as intact specimens (i.e., without a fracture gap). After the creation of a fracture by osteotomy all tibiae were tested sequentially first with the 9 mm and then with an 11 mm nail. In all cases, the medullary cavities were reamed to a diameter 1 mm greater than that of the IM nails to be used in the constructs.
In the compression group (COMP) the osteotomy gap was compressed using the compression feature of the intramedullary nail device. For that purpose the interlocking screw was removed, the osteotomy compressed by a compression screw 2 Nm, and the interlocking screw re-inserted. In the specimens assigned to the static interlocking group (STAT) a second osteotomy was performed distally to create an 8-mm-wide fracture gap.
To enable the specimens to be mounted in the test machines, the distal and the proximal ends of the tibiae were potted in a fast-curing methyl methacrylate-based resin (Technovit 3040, Heraeus Kulzer, Wertheim, Germany) and embedded in specially designed aluminum shells (Fig. 1).
A servohydraulic testing machine (Instron 8874, Instron Ltd, High Wycombe, UK) with a two-channel load cell was used for tension/compression and torsional testing. The distal ends of the specimens were rigidly fixed, while the proximal ends were placed in a cardanic hinge. For the bending and the shear tests, an electromechanical testing machine (Z 010, Zwick, Ulm-Einsingen, Germany) with a 10 kN load cell was used. The specimens were mounted without tension for loading in two planes (coronal and sagittal), with the anterior or the lateral aspect uppermost. The long axis of each specimen was aligned parallel to the base plate of the machine. The Zwick machine allowed distance to be directly measured (accuracy: ±0.01 mm), since the system stiffness determined prior to testing was compensated by calculating a correction curve. In the tension/compression and the torsion tests, movements of the opposing osteotomy edges were determined using an ultrasound-based 3D motion analysis system (CMS20BI, Zebris, Isny, Germany), at a scanning rate of 50 Hz and an accuracy of ±0.1 mm.
In order to eliminate the effect of running-in phenomena, the measuring cycles, in all the tests, were preceded by three conditioning cycles within the linear elastic range of the B–I constructs. The elastic range was determined in a pilot study on two different tibiae.
Axial loading in the tension/compression tests was distance-controlled, and ranged from 0 N through −100 N (compression) to 50 N (tension) and back to 0 N, at a rate of 1 mm/min and a constant torque of 0 Nm. Torsional testing was performed using a constant axial load of 30 N. Torque (applied around the long axis of the tibia at 18 deg/min) ranged from 0 Nm through −5 Nm to 5 Nm and back to 0 Nm. For the determination of shear stiffness in the coronal and the sagittal plane, distance-controlled loading was applied, ranging from 0 N through −100 N to 100 N and back to 0 N, at a rate of 20 mm/min and a distance of the mounting elements of 30 mm. The four-point bending tests (in the coronal and the sagittal plane) were performed with span widths of d = 70 mm for the inner supports and l = 200 mm for the outer supports, with the centre of the tibial shaft placed midway between the two upper supports. The bending moment applied ranged from 0 Nm through −20 Nm to 20 Nm and back to 0 Nm.
Interfragmentary movement was defined as the amplitude of the fracture-end displacements at the fracture gap in the direction of the applied load, during a complete load cycle. It was computed from the sum of the positive and the negative extreme values of the hysteresis loop in the stress-strain diagram. Construct stiffness was determined over the linear elastic range. In order to obtain results that were independent of the test setup in the bending tests, the quotient of the force (F) and the deflection (w) at the fracture site was multiplied with a factor describing the test setup \( \left(S = \frac{F}{w} \cdot \frac{{(l - d)}}{{48}} \cdot (l + 2d)\right). \) The arithmetic means of all the stiffnesses were determined over the range of positive and negative loading of the hysteresis loops. Differences between the different constructs were tested for significance with repeated measures analysis of variance with a posthoc Tukey test for paired variables (SPSS 14.0 Chicago, IL, USA); the level of significance was defined as P = 0.05.
Results
Compared with the osteotomized and nailed tibiae, the intact tibiae had overall greater system stiffnesses. In the tibiae managed without compression (STAT group), the use of a 9-mm-diameter nail produced only between 10 and 36% of the intact-specimen stiffness, while the use of an 11-mm-diameter nail achieved between 17 and 51% of the intact-specimen stiffness (Table 1).
Specimens with compressed interlocking (COMP group) consistently had greater stiffness than did the uncompressed specimens. COMP specimens had between 30 and 110% of the stiffness of the intact (non-osteotomized) specimens where a 9-mm-diameter nail had been used, and between 40 and 130% of the intact-specimen stiffness where the nail diameter was 11 mm (Table 1).
With the exception of the shear-loaded compressed constructs, the two interlocking options consistently produced greater stiffness where an 11-mm-diameter nail had been used, as compared with the constructs that had been produced using a 9-mm-diameter nail (Table 1).
Interfragmentary movement in the direction of the applied load was significantly reduced, in all loading modes, when a larger IM nail diameter was used for the uncompressed (STAT) constructs (Table 2).
With both the 9-mm and the 11-mm nail diameter, compression (COMP) resulted, in significantly reduced interfragmentary movements, as compared with the constructs that did not feature compressed interlocking (STAT). For the 9-mm-diameter nails, the interfragmentary-movement reduction in the COMP group was between 63 and 75%; for the 11-mm-diameter nail, the reduction was between 53 and 79% (Table 2).
Fracture gap shear movements are due, mainly, to torsional loading of the fragments around the tibial shaft axis and to a shear force acting at right angles to the long axis of the bone. The results of the present study showed a marked reduction of fracture gap movement during torsional and shear testing, in the different constructs. In the group with static interlocking, the use of an 11-mm-diameter nail instead of a 9-mm-diameter nail allowed interfragmentary movements to be reduced by about 40%, in both torsional and shear loading tests. Where compression was added to the construct, interfragmentary movement under torsional loading was reduced by a further 55%; under shear loading, the incremental improvement was 80% (Figs. 2, 3).
Discussion
The present study was performed in order to investigate the stability under different loading conditions of constructs used in the management of unstable tibial shaft fractures, as well as to investigate the influence of the IM nail diameter and the interlocking mechanism used.
Bone implant construct stiffness was significantly enhanced by the use of a large diameter nail under torsional loading, sagittal bending and coronal bending and the interfragmentary movement amplitude was significantly reduced under all loading conditions. In contrast, compression of the osteotomy site allowed a significant increase in construct stiffness and a significant decrease in gap movement in all constructs under all loading conditions with the exception of torsional loading.
The different movement amplitudes noted with the 9-mm-diameter and the 11-mm-diameter nails were due to different amounts of play within the systems and to different construct stiffnesses. Play predominantly occurs between the inner cortex and the nail. Play also occurs at the interfaces between the locking screws and the locking-screw holes in the nail, and between the locking screws and the bone. However, the methodology used in the present study did not allow the individual assessment of these factors.
In case of uncompressed nailing construct stiffness is made up of the respective stiffnesses of the bone, the locking screws, and the nail. With torsional loading in particular, the number and the geometry of the locking screws are of major importance [8, 15]. However, in all loading modes, what matters most in terms of construct stiffness is the stiffness of the nail itself. The B–I construct stiffness in bending was mainly determined by the bending stiffness of the intramedullary nail itself which was 63 Nm2 for the 11 mm nail and 27 Nm2 for the 9 mm nail [2]. Similarly in torsional testing most of the stiffness obtained by the B–I construct was contributed by the stiffness of the nail itself (9 mm nail: 1.0 Nm/deg, 11 mm nail: 2.1 Nm/deg) [2].
The stiffness under bending and torsional loads is determined by the second moment of inertia, which is a function of the fourth power of the nail diameter. The construct stiffnesses observed in the present study were only approximately equal to the stiffness of the nail itself. However, it should be borne in mind that the B–I construct contains components, such as the bone and the locking screws, which have much poorer stiffness than does the nail. These components weaken the system and decrease the construct stiffness to a level below the stiffness of the nail.
Compression of the nail allowed the system stiffness to be enhanced under all loading regimes tested. Efficient compression requires meticulous fracture reduction. Once the fracture fragments have been anatomically reduced, the fragment surfaces will interlock, and load transfer will be optimized. In particular, transverse (shear and torsional) forces acting at right angles to the long axis of the tibia to cause mainly shear movement can be directly resisted by the bone.
Compressed fixation produced the greatest torsional stability and, thus, very little fracture gap movement. It is a general observation that, unlike fractures fixed without compression, compressed fractures show very little movement of the fracture fragments, a fact that may be accounted for by fragment interdigitation at the fracture site. Also, by buttressing the fracture fragments on the compressed side, compression can enhance the bending stiffness of the construct. Axial (tensile and compressive) stiffness is also improved by compression, since the anatomical reduction of fragments and the tensile force in the nail will make it impossible for the two fragments to tilt into malalignment. On the other hand, the nail diameter has negligible effect on the interfragmentary movement under tension and compression (Tables 1, 2).
While a small degree of axial movement at the fracture site may promote healing [10], movements caused by shear loads will have an adverse effect [1]. These movements also tend to damage the inner cortex and may, thus, produce increased play between the nail and the surrounding bone. Shear forces constitute an important part of the bone-loading pattern. Anteroposterior shear load components amounting to 0.6–1.3 times BW may be encountered during normal gait [22]. However, the mechanical behaviour of B–I constructs under shear loading has, to date, been the subject of only a limited number of studies [18, 19]. Fracture gap movements of the order observed in the present study are very likely to occur immediately after the IM nailing of fractures. In the tests, the B–I specimens were proximally mounted in a cardanic hinge, with rigid fixation at the distal end, to simulate as closely as possible the physiological loading pattern of the tibia [2]. The frictional forces generated between the sole of the foot and the ground counteract the transverse forces produced by bending or shearing, and provide an opposing moment when the body pivots around the long axis of the tibia. In order to obtain resistance to high torsional moments in the stabilization of fractures, an interlocked IM nailing system must be used. Unlocked systems can resist only very low, if any, torsional moments. In unlocked systems the torsional stiffness of the nail itself is of lesser importance [14], since the torsional moment is produced only by friction between the inner cortex and the outer surface of the nail. For interlocked systems, there is evidence from biomechanical studies that the rotational stability of the B–I construct is greatly enhanced if the number of locking screws is increased. The stability of an IM nail fixation construct is enhanced by the use of more and larger-diameter locking screws [17].
Lack of cortical continuity is an important risk factor for reoperation [3]. Therefore, vertically unstable fractures without fracture fragment contact should be optimally fixed in such a way as to rule out gap movements. This fixation may be achieved by controlled IM reaming, to a diameter only very slightly greater than the external diameter of the selected nail [21]. While reamed IM nailing has been found to enhance the stability of the fixation [7], the relevance for fracture healing of this difference between reamed and unreamed nails has not, to date, been fully established [16, 20].
In reamed IM nailing, an insufficiently large nail diameter may lead to torsional instability and to mechanical failure [9, 14]. A larger-diameter nail will provide a more extensive interface, which will improve the pressure distribution between the external surface of the nail and the inner cortex, especially when the construct is loaded in flexion and/or in shear. Intramedullary reaming also produces reaming debris that is pressed into the fracture site. This process, which may be linked to an internal cancellous autograft, favourably affects fracture healing [11, 23]. However, the raised IM pressure produced by reaming to large diameters may cause fat embolisms and put the patient at risk of cardiopulmonary complications [13].
While the present study was carefully designed to test the hypothesis outlined above, it also has certain limitations: (1) Only 9-mm-diameter and 11-mm-diameter IM nails were used, even though, in some cases, a nail with a minimum diameter of 10 mm would have been more appropriate. In these cases, the 9-mm-diameter nail had more scope for movement, since the clearance between this nail and the inner cortex was much greater than that of an 11-mm-diameter nail in a cavity reamed to a diameter of 12 mm. This may also be one explanation for the relatively large clearance (approximately 5 mm) of the 9 mm nail in the shear test shown in Fig. 3. The fact that the smallest IM canal diameter does not necessarily coincides with the midshaft center [2] might have additionally affected the results in the uncompressed mode in particular. (2) The applied loading regimes simulated a reduced weight bearing activity as it would be typical during the first postoperative weeks after a tibia fracture. Testing therefore occurred within the linear elastic range and permanent deformation was avoided. The displacements occurring in vivo may have been underestimated; however, the determination of the stiffnesses should have been affected little, if at all. (3) No fatigue testing or alternating (cyclical) loading was performed. Therefore, the study could provide information on the primary stability of the B–I constructs in the early postoperative period only, without any information on fracture healing or possible implant loosening in the further course of events.
Conclusion
Choosing the largest possible nail diameter makes biomechanical sense, since it allows the superior stiffness offered by a larger-diameter, as compared with a smaller-diameter, nail to be exploited. Greater system stiffness will, in turn, result in less movement at the fracture gap. Also, the play of the nail inside the medullary cavity should be kept as small as possible (11-mm-diameter nail, 12-mm-diameter reamed space within the medullary cavity), since, otherwise, the nail would be excessively loose in the cavity, and shear and torsional movements would be produced at the fracture gap. Minimizing shear and torsional movements at the gap will promote fracture healing. Suitable fracture patterns like axial stable fractures (e.g. AO 42 A 3) should be meticulously reduced and then compressed. The study suggests that the stability of an IM construct may be enhanced by compression of the fracture site. However, compression is not an option with unstable fractures, and is possible only to a limited extent in stable fractures. With appropriate cases compression of the fracture is probably the most important stabilization principle. Further research will be needed in order to develop methods that will make it possible for surgeons to optimally exploit the mechanical potential of the implants within the constraints of what is feasible in the clinical environment.
References
Augat P, Burger J, Schorlemmer S, Henke T, Peraus M, Claes L (2003) Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res 21:1011–1017. doi:10.1016/S0736-0266(03)00098-6
Augat P, Penzkofer R, Nolte A, Maier M, Panzer S, Oldenburg G et al (2008) Interfragmentary movement in diaphyseal tibia fractures fixed with locked intramedullary nails. J Orthop Trauma 22:30–36
Bhandari M, Tornetta PIII, Sprague S, Najibi S, Petrisor B, Griffith L et al (2003) Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma 17:353–361. doi:10.1097/00005131-200305000-00006
Buhren V (2000) Unfallchirurg 103:708–720. Intramedullary compression nailing of long tubular bones. doi:10.1007/s001130050609
Claes LE, Heigele CA (1999) Magnitudes of local stress and strain along bony surfaces predict the course and type of fracture healing. J Biomech 32:255–266. doi:10.1016/S0021-9290(98)00153-5
Claes LE, Heigele CA, Neidlinger-Wilke C, Kaspar D, Seidl W, Margevicius KJ et al (1998) Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res S132–S147. doi:10.1097/00003086-199810001-00015
Fairbank AC, Thomas D, Cunningham B, Curtis M, Jinnah RH (1995) Stability of reamed and unreamed intramedullary tibial nails: a biomechanical study. Injury 26:483–485. doi:10.1016/0020-1383(95)00056-F
Gaebler C, Stanzl-Tschegg S, Heinze G, Holper B, Milne T, Berger G et al (1999) Fatigue strength of locking screws and prototypes used in small-diameter tibial nails: a biomechanical study. J Trauma 47:379–384. doi:10.1097/00005373-199908000-00030
Hutson JJ, Zych GA, Cole JD, Johnson KD, Ostermann P, Milne EL et al (1995) Mechanical failures of intramedullary tibial nails applied without reaming. Clin Orthop Relat Res 129–137
Kenwright J, Gardner T (1998) Mechanical influences on tibial fracture healing. Clin Orthop Relat Res S179–S190. doi:10.1097/00003086-199810001-00019
Kessler SB, Hallfeldt KK, Perren SM, Schweiberer L (1986) The effects of reaming and intramedullary nailing on fracture healing. Clin Orthop Relat Res 18–25
Krettek C (2000) Marknagelung geschlossener Femur- und Tibiafrakturen; aufgebohrt oder unaufgebohrt? Trauma Berufskrankh 2:126–128. doi:10.1007/PL00014868
Krettek C (2001) Unfallchirurg 104:639–651. Principles of intramedullary fracture stabilization. 1. doi:10.1007/s001130170095
Krettek C, Miclau T, Blauth M, Lindsey RW, Donow C, Tscherne H (1997) Recurrent rotational deformity of the femur after static locking of intramedullary nails: case reports. J Bone Joint Surg Br 79:4–8. doi:10.1302/0301-620X.79B1.6910
Krettek C, Rudolf J, Schandelmaier P, Guy P, Konemann B, Tscherne H (1996) Unreamed intramedullary nailing of femoral shaft fractures: operative technique and early clinical experience with the standard locking option. Injury 27:233–254. doi:10.1016/0020-1383(96)00008-3
Larsen LB, Madsen JE, Hoiness PR, Ovre S (2004) Should insertion of intramedullary nails for tibial fractures be with or without reaming? A prospective, randomized study with 3.8 years’ follow-up. J Orthop Trauma 18:144–149. doi:10.1097/00005131-200403000-00003
Sayana MK, Davis BJ, Kapoor B, Rahmatalla A, Maffulli N (2006) Fracture strain and stability with additional locking screws in intramedullary nailing: a biomechanical study. J Trauma 60:1053–1057. doi:10.1097/01.ta.0000197600.46577.37
Schandelmaier P, Farouk O, Krettek C, Mannss J, Tscherne H (1997). Langenbecks Arch Chir 382:167–172. Biomechanics of femoral interlocking nails at the bone-implant transition
Schandelmaier P, Krettek C, Tscherne H (1996) Biomechanical study of nine different tibia locking nails. J Orthop Trauma 10:37–44. doi:10.1097/00005131-199601000-00006
Schemitsch EH, Turchin DC, Kowalski MJ, Swiontkowski MF (1998) Quantitative assessment of bone injury and repair after reamed and unreamed locked intramedullary nailing. J Trauma 45:250–255. doi:10.1097/00005373-199808000-00008
Stryker Traumatologie, Stryker GmbH & Co KG Duisburg Germany (2005) Operation Manual T2™ Tibia Nail System. [TR-T2Tib-OT-0405: 1-36]
Taylor WR, Heller MO, Bergmann G, Duda GN (2004) Tibio-femoral loading during human gait and stair climbing. J Orthop Res 22:625–632. doi:10.1016/j.orthres.2003.09.003
Tydings JD, Martino LJ, Kircher M, Alfred RH, Lozman J (1987) Viability of intramedullary canal bone reamings for continued calcification. Am J Surg 153:306–309. doi:10.1016/0002-9610(87)90613-1
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosures: Funding for this work was received from AIOD (Association Internationale pour l’Ostéosynthèse Dynamique). Geert von Oldenburg is an employee of Stryker Trauma.
Rights and permissions
About this article
Cite this article
Penzkofer, R., Maier, M., Nolte, A. et al. Influence of intramedullary nail diameter and locking mode on the stability of tibial shaft fracture fixation. Arch Orthop Trauma Surg 129, 525–531 (2009). https://doi.org/10.1007/s00402-008-0700-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-008-0700-0