Abstract
The indications for the use of intramedullary (IM) nails have been extended to include extra-articular distal metaphyseal tibia fractures. We hypothesize that interfragmentary motion during physiologic compressive loading of distal tibia fractures is influenced by fracture obliquity and can be modulated by interlocking screw configuration. Sawbone specimens were osteotomized with frontal plane obliquities ranging from 0° to 60° and then fixed by IM nailing with six interlocking screw configurations. Interfragmentary motion was evaluated during loading in axial compression to 1000 N. Comparisons of interfragmentary motions were made (1) between configurations for the various fracture obliquities and (2) between fracture obliquities for the various screw configurations using a mixed-effects regression model. As the degree of fracture obliquity increased, significantly more interfragmentary displacement was shown in configurations with two distal interlocking screws and one proximal screw set in dynamic mode. Fracture obliquity beyond 30° causes demonstrated instability in configurations with less than two distal locking screws and one proximal locking screw. Optimizing the available screw configurations can minimize fracture site motion and shear in distal tibial fractures with larger fracture obliquities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reamed intramedullary (IM) nailing has become the preferred procedure for management of most displaced diaphyseal tibia fractures as a result of its low incidence of complications and excellent clinical outcomes [1,2,3,4,5]. Over time, implant design and screw-locking options have advanced with a longer working range for fixation due to more distal and proximal screw interlocking options. Consequently, the indications for use of IM nails have been extended to include metaphyseal tibia fractures [6,7,8,9]. Several studies have successfully demonstrated that interlocking nailing could be used in treating fractures of the distal tibia, specifically [10,11,12,13,14,15,16,17,18,19]. However, as the indications for IM fixation have been expanded to include proximal and distal extra-articular tibia fractures, secondary loss of reduction with malalignment becomes a concern [20,21,22,23,24,25,26].
Fractures in the distal metaphyseal tibia managed with IM nail fixation provide less stability as a result of the morphology of the distal tibia. The metaphyseal flare of the medullary canal lessens the contact between the nail and the endosteal surface.
Advances in nail design, most notably the presence of more distal locking options with multiplanar fixation, have improved the biomechanics of IM nailing for distal tibia fractures. In addition to the fracture site region, fracture patterns and patterns of locking screw configurations may play a role in distal fragment stabilization or lack thereof. Fracture obliquity has been shown to influence fracture stability in external fixation models, but no such work has been done with intramedullary nailing [38].
The purpose of this study was to evaluate the influence of fracture obliquity and locking screw configuration on interfragmentary motion during physiologic compressive loading of distal metaphyseal tibial fractures fixed by IM nailing. We hypothesize that interfragmentary motion increases with increasing fracture obliquity in distal tibial fractures and can be modified by interlocking screw configuration.
Materials and methods
The construct stability of six IM nail locking screw configurations used to fix distal metaphyseal tibial fractures of various obliquities were evaluated using a composite synthetic tibia bone model.
Implantation procedure
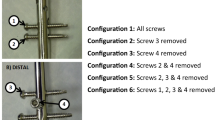
Fourth-generation composite tibias (Part Number: 3402, Pacific Research Laboratories, Inc., Vashon Island, WA) were used to maintain consistency and eliminate the variability of cadaveric bones. The sawbones were osteotomized following reaming of the medullary canal to 12 mm (or 2 mm over the IM nail diameter). Distal cuts were made at various obliquities measured from horizontal in the coronal plane: 0°, 30°, 40°, 50° and 60°. The resulting cuts traveled from proximal and lateral to distal and medial, passing through the tibial midline 7 cm proximal to the edge of the distal tibial articular surface. Osteotomies were created using a band saw with the specimens mounted in a custom fixture ensuring consistent planar alignment of the cuts between specimens. Additionally, a spiral cut pattern oriented 45° from horizontal was created in one specimen using a Dremel rotary hand tool. The sawbones were then instrumented using a stainless steel intramedullary nail measuring 10 mm × 360 mm (M/DN; Zimmer, Warsaw, IN). The nail was inserted according to standard tibial intramedullary technique. The osteotomized fracture ends were then perfectly apposed, so there was no gap in the fracture ends present. Two screws were inserted at the proximal interlocking holes, and three screws at the distal interlocking holes. This nail locking screw configuration, configuration 1, and the five other nail locking screw configurations evaluated in this study are shown in Fig. 1. All screws were inserted in static mode. To determine the effect of reaming and nail fit on stability, another group of sawbones were reamed to 10.5 mm to create a minimally reamed group to compare against the 12 mm over-reamed group (using a 50° osteotomy with same screw configurations).
Mechanical testing
Biomechanical testing was conducted on an Instron ElectroPuls E10000 (Instron Corporation, Norwood, MA) equipped with a 10 KN, 100 Nm Dynacell biaxial load cell.
The proximal and distal ends of the specimens were held in polymethylmethacrylate (PMMA) molds secured in an aluminum frame. The same PMMA molds were used for all specimens, ensuring identical loading points and specimen orientation for all tests. Loads were applied through a loading arm with a ball end attached to the machine actuator. The ball engaged a spherical depression in the proximal fixture located at the center of the tibial plateau. On the distal end, specimens were attached to the base of the test machine using a similar ball and socket joint with the loading point aligned with the center of inferior articular surface. The mechanical testing setup is shown in Fig. 2a, b.
a Experimental testing setup used for mechanical testing. Motion trackers were rigidly attached on the sawbone tibia proximal and distal to the osteotomy site. Figure 2b. 3D Creator motion tracking system (Boulder Innovation Group, Boulder CO)
Specimens were loaded in axial compression at a rate of 0.05 mm/s to 1000 N followed by a hold at 1000 N for 2 s. The maximum load of 1000 N was selected to approximate compressive loading present during ambulation. Throughout testing, custom trackers with infrared emitters rigidly attached to the proximal and distal segments were monitored with a 3D creator motion capture system (Boulder Innovation Group, Boulder CO) at 28 Hz. Preliminary testing showed the position and rotational accuracies of the trackers to be 0.1 mm and 0.2°, respectively.
A custom MATLAB program was used to analyze the motion capture data and determine interfragmentary motion of the specimens at 1000 N compressive load. The initial positions of the trackers were calculated by averaging the last 40 frames of data before loading, while the final tracker positions were determined by averaging the last 40 frames of data acquired during the two second hold period at 1000 N. Interfragmentary displacement was defined as the vector magnitude of the individual displacement components (superior–inferior, medial–lateral, anterior–posterior), while interfragmentary rotation was defined as the rotation of the distal segment about the long axis of the proximal segment. Three trials are performed for each of the six screw-locking configurations shown in Fig. 1, resulting in a total of 18 tests on each specimen. One specimen was tested for each fracture obliquity evaluated in the study.
Statistical analysis
Comparisons of interfragmentary motions were made (1) between configurations for the various fracture obliquities, and (2) between fracture obliquities for the various screw configurations. For each fracture obliquity, a mixed-effects regression model was fit to estimate the effect of the six screw configurations on the two outcome measures: interfragmentary displacement and rotation. The estimated marginal means and 95% confidence intervals were produced from these models, and pairwise comparisons between the configurations were made with a 95% family-wise confidence level assuming equal variance across the conditions. The analyses were then transposed to compare the effects of different obliquities within each configuration. In addition, minimally reamed configurations were statistically compared with matched over-reamed configurations using a paired t test. Significance was set at p < 0.05.
Due to the large number of statistically significant comparisons between the various fracture obliquities and screw configurations, thresholds were established in order to limit the presentation of significant findings to only clinically meaningful data. The authors decided that thresholds would be set to either 1 mm or 2 mm of interfragmentary displacement. Both a magnitude threshold and difference threshold were defined in order to achieve this goal. In order for a comparison between two fracture obliquities or screw configurations to be valid, the magnitude of at least one of the interfragmentary displacements compared needed to be greater than or equal to the magnitude threshold. Furthermore, the difference between the interfragmentary displacements being compared was required to be at least the value of the difference threshold.
In addition to the thresholds defined for interfragmentary displacement, rotational thresholds (magnitude and difference) were established for comparisons of interfragmentary rotation. Thresholds were calculated based on rotations involving either 1 mm or 2 mm of displacement on the outer surface of the tibia. These displacement values and the average tibial outer radius at the location of the cut were used to calculate rotation thresholds of 4° and 8° using the arc length formula for a circle (arc length = radius × angle in radians).
Results
Interfragmentary displacements organized by locking screw configuration are presented in Fig. 3. Additionally, the interfragmentary displacements are presented in tabular form as supplementary data for this article. For fracture obliquities of 0° and 30°, interfragmentary displacements were less than 0.5 mm for all locking screw configurations. For a fracture obliquity of 40°, only configuration 6 resulted in interfragmentary displacements larger than 1 mm. For fracture obliquities of 50°, 60° and a spiral fracture, configurations 4, 5, and 6 resulted in interfragmentary displacements larger than 1 mm. Compression testing resulted in no significant interfragmentary rotations, with all rotations being less than 2°.
Significant configuration comparisons for various fracture obliquities at designated interfragmentary displacement thresholds are presented in Tables 1, 2 and 3.
Differences between minimally and over-reamed groups tended to favor more stability in the minimally reamed group with respect to displacement and rotation (Table 4); however, results were not statistically significant (displacement p = 0.08; rotation p = 0.11).
Magnitude threshold: 1 mm, difference threshold: 1 mm
For a fracture obliquity of 40°, configuration 6 displayed significantly greater interfragmentary displacement compared to all other configurations. For fracture obliquities of 50° and 60°, configurations 4, 5 and 6 had significantly larger displacements than configurations 1, 2 and 3. For a spiral fracture, interfragmentary displacements for configurations 5 and 6 were significantly greater than configurations 1, 2 and 3. All comparisons noted above resulted in p values < 0.001.
Magnitude threshold: 2 mm, difference threshold: 2 mm
For a fracture obliquity of 50°, configuration 6 displayed significantly greater interfragmentary displacement compared to configuration 1. For a fracture obliquity of 60°, configurations 4, 5 and 6 showed significantly greater interfragmentary displacement compared to configurations 1, 2 and 3. All aforementioned comparisons resulted in p values < 0.001.
Significant fracture obliquity comparisons for various locking screw configurations at designated interfragmentary displacement thresholds are presented in Table 2.
Magnitude threshold: 1 mm, difference threshold: 1 mm
For configuration 4, a fracture obliquity of 60° had significantly greater interfragmentary displacement compared to all other fracture obliquities. A fracture obliquity of 50° displayed significantly more interfragmentary displacement than fracture obliquities of 0° and 30°. A spiral fracture obliquity showed significantly more interfragmentary displacement than fracture obliquities of 0° and 30°.
For configuration 5, a fracture obliquity of 60° displayed significantly greater interfragmentary displacement compared to all other fracture obliquities. A fracture obliquity of 50° showed significantly more displacement than fracture obliquities of 0°, 30° and 40°. Interfragmentary displacement for a spiral fracture obliquity was significantly greater than fracture obliquities of 0° and 30°.
For configuration 6, a fracture obliquity of 60° had significantly greater interfragmentary displacement compared to all other fracture obliquities. Interfragmentary displacement for fracture obliquities of 40°, 50° and spiral were significantly larger than that seen in fracture obliquities of 0° and 30°. All aforementioned comparisons resulted in p values < 0.02.
Magnitude threshold: 2 mm, difference threshold: 2 mm
For configurations 4 and 5, a fracture obliquity of 60° displayed significantly greater interfragmentary displacement compared to fracture obliquities of 0°, 30°, 40° and spiral. For configuration 6, a fracture obliquity of 60° exhibited significantly greater interfragmentary displacement compared to fracture obliquities of 0°, 30°, 40° and spiral. A fracture obliquity of 50° displayed significantly more interfragmentary displacement than fracture obliquities of 0° and 30°. All comparisons noted above resulted in p values < 0.002.
Discussion
Locked intramedullary nailing is a standard method for treatment of displaced tibial shaft fractures [1,2,3,4,5]. The treatment of distal metaphyseal tibial fractures remains a challenging problem in modern fracture care. To exploit the benefits of IM nailing even in distal fractures, various modifications in the implants have been introduced. These changes include the number and location of the locking holes in the nail. As a result of the ability to have distal locking in a multiplanar manner, IM nails have been successfully used for fixation of fractures in the distal metaphysis of the tibia [9, 10, 12,13,14,15,16,17,18,19]. Despite some historical evidence that plate and screws fixation leads to less malunion than IM nailing for the treatment of distal tibial fractures, newer suprapatellar, semi-extended approaches have significantly helped to mitigate this risk associated with nailing [7, 8, 27, 28]. Clinical trials have suggested that union rates and overall disability are equivalent between groups with improved patient-reported outcomes in patients treated with IM nailing [29, 30].
Modern tibial nail designs have interlocking holes that enable distal placement of screws to within 5 mm of the tip of the nail. Multiplanar patterns to a very distal extension are commonly found in these next-generation nails. Distal locking screws have less cortical purchase in metaphyseal bone, and control of the IM nail position in the distal tibial canal as well as control of the fracture fragments depends on these screws. There is hence increased stress on the screws to maintain fracture alignment [31]. The locking screws are important in increasing torsional rigidity and compressive strength of the nail–screw construct. Because the metaphyseal flare of the distal tibia causes a widening of the intramedullary canal as compared to the diaphysis, sufficient nail–bone contact is not provided, and thus the interface between nail, bone and locking screw number and configuration become important variables in overall construct stability.
Our study confirms our hypothesis that interfragmentary motion is influenced by fracture obliquity in distal metaphyseal fractures treated with IM nailing and can be modulated by interlocking screw configuration. Screw configuration significantly influenced interfragmentary displacement for fracture obliquities greater than or equal to 40°. Fracture obliquities of 30° or less are adequately stabilized under compressive loading with an IM tibial nail for all screw configurations tested in this study. These constructs are inherently stable with dynamic proximal interlocking. Fracture obliquity beyond 30° increasingly showed instability in dynamic constructs with less than two distal screws and one proximal screw.
Screw orientation (two parallel versus two perpendicular distal interlocking screws) or amount of over-reaming did not significantly influence construct stability in this metaphyseal fracture model. This result corroborates the findings shown by Chen et al. [32] which demonstrated no statistical difference in nail stability between the two screw patterns in anterior, posterior, medial or lateral directions, or torsional loading. Mohammed et al. [33] found that there was a high incidence of nonunion in distal metaphyseal tibia fractures treated with IM nailing when only one distal locking screw was used. Therefore, they recommended that two distal locking screws be utilized for these distal metaphyseal tibial fractures, which was confirmed in subsequent clinical and biomechanical studies [18, 34, 35]. Another study demonstrated that three points of fixation in the distal segment significantly improved construct stability compared to two although both configurations were stable enough to support immediate weight bearing after nailing of distal tibial fractures [36]. Unlike the present study, fracture obliquity was not accounted in the aforementioned investigations. The findings presented in this study are consistent with another study suggesting increased fracture obliquity is associated with increased interfragmentary motion, despite our more rigorous biomechanical testing conditions [37].
The successful implantation of a locked tibial nail for fixation of distal tibia fractures relies on a clear understanding of both proximal and distal interlocking screw configurations for the particular fracture pattern that is present. Lowenberg et al. [38] reported that the fracture angulation introduces two elements during axial compressive loading: incomplete opposition to the axial load and the introduction of an unopposed horizontal component of force. After the summation of the vector forces, a resultant shear force is realized. Shearing is the culprit of instability in an oblique fracture and is exacerbated with increasing fracture angulation. Blocking screws can be helpful as a reduction tool to correct malalignment in distal tibial fractures if they are placed in the concavity of the deformity. From a biomechanical perspective, however, the extra stiffness provided by the addition of a blocking screw is not significantly different than without for distal tibia fractures [36].
We recognize some limitations to our study. We used Sawbone tibias instead of cadaveric specimens to ensure consistency and reproducibility. Cadaver bones are impractical as a testing material when comparing tests with multiple variables due to the difficulty of obtaining bones of equivalent bone mineral density and strength. One limitation of using sawbones is the lack of soft tissue or muscle restraint which contributes to fracture stability. Moreover, the osteotomies evaluated in this study do not account for the additional stability conferred by fracture interdigitation. In addition to compressive loading, other loading conditions (torsion, bending) should be considered when selecting the appropriate fixation method. Finally, although numerous statistically significant differences were identified between specimens, it should be noted that only a single specimen was tested for each fracture obliquity examined in this study. We chose to use interfragmentary motion or displacement to evaluate construct stability. Alternatively, we could have evaluated significant angulation as a threshold for instability. From a practical point of view, our methods allowed us to measure a consistent threshold of displacement in any plane of motion as opposed to an angulation threshold based upon orthogonal values to assign clinical significance.
Conclusion
Our study demonstrated that optimizing the available screw configurations can minimize fracture site motion and shear in distal tibial fractures with increased obliquity. When fracture obliquity at the distal tibia exceeds 30° and even with absolute fracture fragment apposition, the number of interlocking screws becomes important to resist shear forces experienced under physiologic load.
References
Alho A, Ekeland A, Stromsoe K, Folleras G, Thoresen BO (1990) Locked intramedullary nailing for displaced tibial shaft fractures. J Bone Joint Surg Br 72:805–809
Henley MB (1989) Intramedullary devices for tibial fracture stabilization. Clin Orthop Relat Res 240:87–96
Bone LB, Johnson KD (1986) Treatment of tibia fractures by reaming and intramedullary nailing. J Bone Joint Surg Am 68:877–887
Coles CP, Gross M (2000) Closed tibial shaft fractures: management and treatment complications. A review of the prospective literature. Can J Surg 43:256–262
Collins DN, Pearce CE, McAndrew MP (1990) Successful use of reaming and intramedullary nailing of the tibia. J Orthop Trauma 4:315–322
Bedi A, Le TT, Karunakar MA (2006) Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg 14:406–416
Im GI, Tae SK (2005) Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma 59:1219–1223
Janssen KW, Biert J, van Kampen A (2007) Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop 31:709–714
Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA (2005) Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am 87(6):1213–1221
Fan CY, Chiang CC, Chuang TY, Chiu FY, Chen TH (2005) Interlocking nails for displaced metaphyseal fractures of the distal tibia. Injury 36:669–674
Dogra AS, Ruiz AL, Thompson NS, Nolan PC (2000) Dia-metaphyseal distal tibial fractures-treatment with a shortened intramedullary nail: a review of 15 cases. Injury 31:799–804
Gorczyca JT, McKale J, Pugh K, Pienkowski D (2002) Modified tibial nails for treating distal tibial fractures. J Orthop Trauma 16:18–22
Hoegel FW, Hoffmann S, Weninger P, Bühren V, Augat P (2012) Biomechanical comparison of locked plate osteosynthesis, reamed and unreamed nailing in conventional interlocking technique, and unreamed angle stable nailing in distal tibia fractures. J Trauma Acute Care Surg 73(4):933–938
Moongilpatti Sengodan M, Vaidyanathan S, Karunanandaganapathy S, Subbiah Subramanian S, Rajamani SG (2014) Distal tibial metaphyseal fractures: does blocking screw extend the indication of intramedullary nailing? ISRN Orthop 20114:542623
Tejwani N, Polonet D, Wolinsky PR (2014) Controversies in the intramedullary nailing of proximal and distal tibia fractures. J Am Acad Orthop Surg 22(10):665–673
Kruppa CG, Hoffmann MF, Sietsema DL, Mulder MB, Jones CB (2015) Outcomes after intramedullary nailing of distal tibial fractures. J Orthop Trauma 29(9):e309–e315
Kuhn S, Greenfield J, Arand C, Jarmolaew A, Appelmann P, Mehler D, Rommens PM (2015) Treatment of distal intraarticular tibial fractures: a biomechanical evaluation of intramedullary nailing vs. angle-stable plate osteosynthesis. Injury Suppl 4:S99–S103
Agathangelidis F, Petsatodis G, Kirkos J, Papadopoulos P, Karataglis D, Christodoulou A (2016) Distal locking screws for intramedullary nailing of tibial fractures. Orthopedics 39(2):e253–e258
Maredza M, Petrou S, Dritsaki M, Achten J, Griffin J, Lamb SE, Parsons NR, Costa ML (2018) A comparison of the cost-effectiveness of intramedullary nail fixation and locking plate fixation in the treatment of adult patients with an extra-articular fracture of the distal tibia. Bone Joint J 100-B(5):624–633
Koval KJ, Clapper MF, Brumback RJ, Ellison PS Jr, Poka A, Bathon GH et al (1991) Complications of reamed intramedullary nailing of the tibia. J Orthop Trauma 5:184–189
Freedman EL, Johnson EE (1995) Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res 315:25–33
Whittle A, Crates J, Wood GW et al (1997) Distal fourth tibial fractures treated with locked intramedullary nails: does fibular fracture influence mal-alignment? In: Annual meeting of the OTA, Louisville
Lang GJ, Cohen BE, Bosse MJ, Kellam JF (1995) Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res 315:64–74
Robinson CM, McLauchlan GJ, McLean IP, Court-Brown CM (1995) Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br 77:781–787
Mosheiff R, Safran O, Segal D, Liebergall M (1999) The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury 30:83–90
Tyllianakis M, Megas P, Giannikas D, Lambiris E (2000) Interlocking intramedullary nailing in distal tibial fractures. Orthopedics 23:805–808
Vallier HA, Cureton BA, Patterson BM (2011) Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 25(12):736–741
Avilucea FR, Triantafillou K, Whiting PS, Perez EA, Mir HR (2016) Suprapatellar intramedullary nail technique lowers rate of malalignment of distal tibia fractures. J Orthop Trauma 30(10):557–560. https://doi.org/10.1097/BOT.0000000000000631
Costa ML, Achten J, Griffin J, Petrou S, Pallister I, Lamb SE, Parsons NR, FixDT Trial Investigators (2017) Effect of locking plate fixation vs intramedullary nail fixation on 6-month disability among adults with displaced fracture of the distal tibia: the UK FixDT Randomized Clinical Trial. JAMA 318(18):1767–1776
Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML (2012) A randomised pilot trial of “locking plate” fixation versus intramedullary nailing forextra-articular fractures of the distal tibia. J Bone Joint Surg Br 94(5):704–708
Varsalona R, Liu GT (2006) Distal tibial metaphyseal fractures: the role of fibular fixation. Strateg Traum Limb Reconstr 1:42–50
Chen AL, Tejwani NC, Joseph TN, Kummer FJ, Koval KJ (2001–2002) The effect of distal screw orientation on the intrinsic stability of a tibial intramedullary nail. Bull Hosp Jt Dis 60(2):80–83
Mohammed A, Saravanan R, Zammit J, King R (2008) Intramedullary tibial nailing in distal third tibial fractures: distal locking screws and fracture non-union. Int Orthop 32:547–549
Sharma S, Pradhan RL, Khanal KR, Rijal KP, Lakhey S, Pandey BK, Manandhar RR, Prasai T (2015) Distal third tibia fractures treated with interlocking intramedullary nail. Nepal Med Coll J 17(1–2):78–82
Lucas BL, Chong AC, Buhr BR, Jones TL, Wooley PH (2011) Biomechanical comparison of distal locking screws for distal tibia fracture intramedullary nailing. J Biomed Sci Eng 4(4):235–241
Chan DS, Nayak AN, Blaisdell G, James CR, Denard A, Miles J, Santoni BG (2015) Effect of distal interlocking screw number and position after intramedullary nailing of distal tibial fractures: a biomechanical study simulating immediate weight-bearing. J Orthop Trauma 29(2):98–104
Chaichankul C (2017) Fracture motion in distal tibial rodding: effect of obliquity, load, and locking screw pattern. J Med Assoc Thai 100:1274
Lowenberg DW, Nork S, Abruzzo FM (2008) Correlation of shear to compression for progressive fracture obliquity. Clin Orthop Relat Res 466(12):2947–2954
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have received no benefits or funds in support of the study and no personal relationships with organizations that could inappropriately influence (bias) this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lowenberg, D.W., DeBaun, M.R., Sox-Harris, A. et al. Influence of fracture obliquity and interlocking nail screw configuration on interfragmentary motion in distal metaphyseal tibia fractures. Eur J Orthop Surg Traumatol 30, 343–350 (2020). https://doi.org/10.1007/s00590-019-02553-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02553-w