Abstract
Introduction
Traumatic heterotopic ossification (HO) is a common clinical condition associated with various orthopedic procedures that involve injury to soft tissues near bone. In this study, we tested the hypothesis that the prophylactic effects of NSAID’s in the treatment of HO are mediated via inhibition of the COX-2 enzyme. Here we describe a rat model that simulates HO in the human that was used to test the above hypothesis.
Materials and methods
Heterotopic ossification was surgically induced in the quadriceps by injury to the muscle and femoral periosteum and transplantation of donor bone marrow cells containing osteoprogenitors into the site of injury. HO was imaged and quantified by micro-CT scanning of femurs removed from sacrificed animals at 6 weeks post-injury, three-dimensional computer reconstructions of the scanned bones and computer-assisted morphometric analysis. Prostaglandin E2 (PGE2) synthesis was quantified using an enzyme immunoassay system. The effects of a nonselective COX inhibitor or specific inhibitors of COX-1 or COX-2 following oral administration on the content of ectopic bone and PGE2 were also measured.
Results
Micro-CT and histological analyses demonstrated that all of the femurs in operated limbs developed HO in the vastus lateralis muscle belly of the quadriceps close to the anterior femur. Only the COX-1,2 nonselective and COX-2 inhibitors significantly decreased HO formation (by about one-third in each case; P < 0.05). PGE2 synthesis at the site of injury was increased 50- and 100-fold (to 25 ng/g tissue) within 1 and 7 days, respectively, post-injury with the levels declining to near baseline within 2 weeks of surgery. Both the COX-1,2 nonselective and COX-2 inhibitors significantly decreased PGE2 levels to 25% of control HO levels within 24 h of the first administration, even at low dosages. The COX-1 inhibitor only produced the same effect after 1 week of administration.
Conclusion
These findings suggest that although inhibitors of COX-2 or COX-1 reduced PGE2 synthesis, only the COX-2 enzyme plays a role in the mechanism of traumatic HO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevention of heterotopic ossification (HO) is of particular clinical and scientific interest because of its prevalence and capacity to cause long-term disability [44]. HO is the extraskeletal formation of mature trabecular bone in areas in which it is not regularly present and is observed following orthopedic surgical procedures accompanied by trauma to the soft tissue.
Heterotopic ossification is observed in the clinical setting following surgery or burns resulting in the calcification of ligaments, tendons, and scars. Although its incidence varies widely, HO is typically seen in 20–30% of hip arthroplasty cases [34, 11, 15, 14]. It is also found that the severity of the HO response in these patients is related to the extent of soft tissue trauma. Functional loss appears to be associated with surgical approaches that require significant periosteal and muscle stripping, especially that of the hip abductor musculature, which result in pericapsular hematomas [25, 53, 23]. These findings suggest that trauma is an important factor in the mechanism of the HO that can result from these surgical procedures.
Traditional methods of preventing HO include either radiation [8, 36] or non-steroidal anti-inflammatory drugs (NSAIDs) [34, 36, 1, 27, 42]. While radiation can be effective as a preoperative therapy, risks still include genetic alterations, malignancy, and gonadal effects [8, 10, 33]. NSAIDs have prominent adverse side effects that include gastrointestinal (GI) problems, renal toxicity and platelet deficiency [53, 13, 20, 28, 35]. Previous studies indicate that the main side effects of traditional NSAID’s are due to the inhibition of COX-1-dependent prostaglandins synthesis since constitutive levels of this isoenzyme are involved in the regulation of some of the physiological functions described above. As a result, there is current interest in exploring the effects of specific inhibitors of COX-2 enzymes, which are not expressed in platelets or the GI tract to the same degree as COX-1 [28, 35, 22, 6, 37, 55].
In order to better understand the cause of traumatic HO, our laboratory developed a rodent model that mimics the physiological changes that are theoretically induced by various orthopedic procedures to predispose the patient to ectopic bone formation. Experimental HO induction can be accomplished in one (or a combination) of three ways: (a) trauma to soft tissue [40], (b) transplantation of certain cell types that possess the ability to form bone and (c) induction caused by interaction between undifferential mesenchymal cells and transplanted epithelial cells [2, 3] or bone morphogenetic protein (BMP) [5]. The single injury traumatic HO rat model reported here has been adapted from the rabbit model reported by Schneider et al. [54]. The Schneider model has been modified in the current study by the elimination of intramedullary reaming so as to avoid the introduction of bone chips into the surrounding soft tissue.
In a previously reported study, we have found, using the Michelsson multiple injury HO model [40], that prostaglandins are up regulated within 24–48 h of the initial injury and preceded the formation of HO by several weeks [4]. An obligate role for prostaglandins in the pathophysiological mechanism of HO was also demonstrated [4]. However, the repeated injury model used in this latter investigation does not closely replicate the type of injury caused by orthopedic procedures that predispose the patient to HO. In addition, the comparative roles of COX-1 and COX-2 in the etiology of traumatic HO were not examined. Therefore, our objectives in the current study using a more clinically relevant single injury model were the following: (a) to quantitate the amount of HO in a rat HO model using a micro-CT analysis procedure; (b) to measure increases in the synthesis of prostaglandin E2 (PGE2) before HO formation occurs; and (c) to compare the various effects of prophylactically administered COX-1, COX-2, and nonspecific COX inhibitors on PGE2 formation and HO content in the rat model in vivo. The latter objective would help to define the roles of prostaglandin synthesis, COX-1 and COX-2 in HO. In this study, we have shown that prostaglandin synthesis plays a significant role in traumatic HO. Findings obtained through the use of specific inhibitors also suggest that COX-2 rather than COX-1 is more involved in the etiology of this metabolic bone disorder.
Materials and methods
Materials
The COX-1 inhibitor SC-560 and the COX-2 inhibitor celecoxib were obtained from Pharmacia, Inc. (IL, USA). Purina 1002 Rodent Chow pellets with and without coformulation with COX inhibitors were obtained from Purina (IN, USA). Ibuprofen was obtained from Sigma Chemical Co. (MA, USA). SEP-PAK cartridges were obtained from Water Associates (Milford, MA, USA). Enzyme immunoassay (EIA) kits were obtained from Cayman Chemical (Ann Arbor, MI, USA). BioRad protein dye reagent was obtained from BioRad Laboratories (Hercules, CA, USA). All other chemicals used were of reagent grade and were obtained from Fisher Scientific (NJ, USA).
Animals and surgery
A total of 250–300 g skeletally mature syngeneic (inbred) Lewis rats were utilized to induce HO. Skeletally mature Lewis rats underwent a surgical procedure in which HO forms in the vastus lateralis muscle belly of the quadriceps close to the anterolateral surface of the femur. Seven experimental animal groups (9–15 rats per group) were operated on and analyzed (see Table 1). The surgical induction of HO was performed as follows. A longitudinal incision was performed along the proximal–lateral thigh. After elevation of a skin flap to expose the quadriceps, the muscle was split longitudinally (in line with the muscle fibers) to separate the rectus femoris muscle belly from the distal vastus lateralis and these two muscle bellies were elevated to expose the femur. The rectus femoris fibers were split in line as the dissection was carried down to the femur. Four Kocher clamps were then placed across the proximal vastus lateralis for 10 min to simulate surgical iatrogenic damage to the muscle and produce myonecrosis that has been postulated to be essential for HO induction [54, 17]. Part of the periosteum of the anterior femur was surgically disrupted and left in place to release osteogenic factors. Syngeneic bone marrow cells (100 million cells in 0.075 ml) were removed from one femur and one tibia of a donor Lewis rat (not subjected to surgical intervention to induce HO). The bone marrow cells were then transplanted to muscle via placement over the proximal–anterolateral femur as a source of osteoprogenitor cells (Fig. 1a). The vastus lateralis was unclamped and restored to its normal position covering the anterolateral surface of the femur (Fig. 1b). The wound was then closed in layers with gut sutures and a sterile dressing applied. Since common orthopedic surgeries that predispose the patient to HO, such as total hip replacement, can release stem cells from bone marrow, the rat HO induction procedure utilized here provides a physiologically relevant traumatic HO model.
Schematic diagram depicting the procedure for the surgical induction of heterotopic ossification (HO) in the rat quadriceps (vastus lateralis muscle belly). The clamping of the retracted muscle and placement of donor bone marrow cells from a syngeneic rat over the anterolateral surface of the recipient rat femur near a region of surgically disrupted periosteum is shown in a. The unclamping of the muscle and restoration to its normal position covering the anterolateral surface of the femur is shown in b
Rats that underwent the surgical procedure to induce HO were subclassified into seven experimental groups (Table 1). All except the No Surgery Group were subjected to this procedure. The No Surgery and Control HO (induction of HO without COX treatment) groups were administered ad libitum Purina 1002 Rodent Chow pellets and were not administered COX inhibitors. The remaining groups were fed rodent chow coformulated as pellets (beginning on the day of surgery) containing one of two (average daily dosages) dosages of either the nonselective COX inhibitor ibuprofen (10 or 25 mg/kg), the COX-2 inhibitor celecoxib (1 or 10 mg/kg), or the COX-1 selective inhibitor SC-560 [38] (0.1 or 1 mg/kg) (Table 1) for a period of 28 days following surgery. The selective COX-1 inhibitor is a synthetic analog of celecoxib (Compound 38; C17H12ClF3N2O) in which the methyl and H2NSO2 groups of the COX-2 inhibitor are replaced by a methoxy group and a chlorine at positions X and Y, respectively, of the diarylpyrazole backbone structure [49]. The COX-2 inhibitor and the nonselective COX inhibitor were administered over a range of pharmacological doses shown to be effective in treating arthritis pain or decreasing markers of COX-2 activity in humans [39, 28]. SC-560 was administered over a range of dosages shown to block more than 90% of PGE2 production in gastric mucosa (ED50 = 0.2 mg/kg), which is COX-1 dependent, with no effect on PGE2 synthesis in a model of lipopolysaccharide-induced inflammation, a COX-2-dependent process [56]. The dosage calculations were based on an average food pellet consumption of 10 g (two 5-g pellets) per day for each rat. In another arm of the study, separate experimental groups of rats were administered COX inhibitors as described in Table 1 beginning on the day of surgical induction of HO and continuing until the time of sacrifice at 1, 7, 14, or 21 (6–8 rats per time point) days post-surgery at the end of each experimental period. Operated lower limbs of the rats were dissected, and the vastus lateralis muscle belly of the quadriceps was removed for subsequent protein and prostaglandin analyses. All of the rats administered COX inhibitors showed normal daily body mass gains following surgery until sacrifice with no showed evidence of GI bleeding. The surgical and drug administration protocols were each IACUC-approved.
CT scanning and reconstruction–quantitation of heterotopic bone
Following sacrifice, each operated hind limb was dissected and the femurs were disarticulated at the hip and knee. Femoral specimens were trimmed leaving most of the vastus intermedius (anterior surface) and vastus lateralis (lateral surface) still attached to the bone. Trimmed femoral specimens were positioned in a saline-filled scan tube. Femurs with attached partial quadriceps and heterotopic bone were imaged in three dimensions by scanning in a small-animal micro-CT (MS-8, EVS, G.E. Medical Systems, ON, Canada). Isotropic voxel resolution for each scan was 17 μm. Scans of a phantom gave Hounsfield Unit (HU) calibration values for air, saline and bone mineral (1.18 g/cc, SB3). In conventional CT the X-ray source and detector rotate around the patient. In contrast, in micro-CT the sample rotates and translates longitudinally while the X-rays in a fan beam peaked at 25 keV pass through a fluorescent X-ray-to-light conversion crystal and are imaged onto a charge-coupled detector (CCD) array. For multiple X-ray projections spanning 360° around the longitudinal axis of the specimen, the illumination pattern generated by the crystal for each projection is detected and converted into a discrete pattern of stored charge in the CCD array. Charge is digitized and stored until 400 projections, at small increments of specimen rotation around 360°, are acquired to image cross-sectional “slices” of the specimen. Since the size of a detector element is 25 × 25 μm, the slice thickness is 25 μm [32]. The two-dimensional (2D) distribution of X-ray density in each slice is then calculated from the data acquired for the 400 projections. This procedure is repeated for successive slices and a 3-D distribution of X-ray absorption is then built up by applying a modified Parker reconstruction algorithm to the recorded images obtained for all of the slices [21]. Reconstructed grayscale volumes for each femur were extracted and segmented with a global threshold of 300 HU to separate mineralized tissue from the marrow and soft tissues [24].
For each femur, the combined cross-sectional area of ectopic bone in 15 slices was quantified using a Bioquant computer program to obtain a measure of HO content. Slices were saved as tagged image format files (tiff) at 1 mm intervals (along the longitudinal axis of the bone) beginning with a point immediately distal to the lesser trochanter and proceeding distally. The saved slices were then viewed and the ectopic bone cross-sectional area was traced and quantified in number of pixels (1 pixel = 25 μm2) using the Bioquant program.
Histological analysis of heterotopic bone
Femurs were fixed in 10% formalin overnight, dehydrated through a graded series of ethanol solutions, decalcified in 10% EDTA at 4°C for 1 week and dehydrated. The dehydrated specimens were embedded in polymethylmethacrylate (PMMA) and 10 μm sections were prepared. These sections were stained with trichrome to label collagen fibrils in the matrix of femoral and ectopic lamellar bone and examined by light microscopy.
Prostaglandin analysis
Prostaglandins were extracted from the vastus lateralis muscle belly of the quadriceps following the method of Powell [50]. The muscle tissue was frozen in liquid nitrogen followed by manual grinding by mortar and pestle. Ground muscle homogenate was mixed with 15% ethanol. After vortexing and centrifugation, the supernatants were acidified with 1 N HCL. Prostaglandins were separated from other lipids by column chromatography utilizing SEP-PAK cartridges (Water Associates, Milford, MA, USA). In a stepwise fashion, the fatty acids, leukotrienes and polar lipids were eluted with ethanol and neutral lipids were eluted with petroleum ether. Methyl formate was then used to elute prostaglandins. Methyl formate eluants were evaporated under a stream of liquid nitrogen at a bath temperature of 60°C. After re-suspension in EIA buffer, EIA kits (Cayman Chemical, Ann Arbor, MI, USA) were used to determine the levels of PGE2 in the muscle tissue extracts. Protein assays were also performed using BioRad protein dye reagent (BioRad Laboratories, Hercules, CA, USA) to express prostaglandin concentrations per milligram of muscle protein.
Statistical analysis
All of the data was analyzed by one-way analysis of variance (ANOVA) and Tukey–Kramer multiple comparisons test to identify statistically significant differences between individual experimental groups. The threshold for a statistically significant difference was set at P < 0.05.
Results
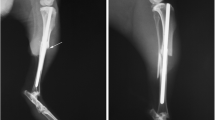
All of the animals studied developed HO in operated limbs. None of the rats that were subjected to surgical induction of HO manifested any level of disability in operated hind limbs and all showed normal daily body mass gains following surgery until sacrifice. Femurs were removed after sacrifice at 6 weeks post-surgery and scanned by micro-CT. A 3-D computer reconstruction of the proximal segment of one of these scanned femurs is shown in Fig. 2. An island of extraskeletal bone can be seen in the muscle over the anterolateral surface of the femur (Fig. 2; small arrow). An anterior proximal view of this femur shows a layer of heterotopic bone over the anterolateral surface (Figs. 2, 3a; small arrow). This band of ectopic bone was observed over the anterolateral surface of the femur in all of the operated limbs (92 limbs). In several femurs, a column of heterotopic bone that appears to unite with the anteromedial surface of the femur was observed at 6 weeks following surgical induction of HO (Figs. 2, 3b; large arrow). A micro-CT cross-section shows that this newly formed column of bone shows a marrow cavity containing a trabecular bony structure (Fig. 3c; arrow), resembling the HO that is observed clinically. In contrast, the normal structure of the femur (no surgery to induce HO) shows no ectopic bone near the anterolateral or anteromedial surfaces (Fig. 3a).
Micro-CT three-dimensional (3-D) reconstruction of the right proximal femur from a rat in which HO was surgically induced in the quadriceps. At 6 weeks following surgical induction of HO, the rat was sacrificed and the femur was removed from the right operated limb and scanned in a small animal micro-CT as described in “Materials and methods”. A 3-D computer reconstruction of the scanned bone was performed as described in “Materials and methods”; a proximal segment of the reconstructed femur is shown in the figure. The figure shows a column of heterotopic bone, identified by the large arrow, in union with the anteromedial surface of the femur. An island of extraskeletal bone, identified by the small arrow, can also be seen in the muscle over the anterolateral surface of the femur. The femoral head and the lesser trochanter are identified by one and two stars, respectively
Close-up anterior proximal view of the femur shown in Fig. 2 in comparison with that of a control femur from a rat which did not undergo surgical induction of HO. The two bones were scanned by micro-CT at different times. a Left control (No Surgery) femur. b Right HO (surgical induction of HO) femur that was also shown in Fig. 2. b A layer of heterotopic bone covering the anterolateral surface (shown by small arrow; see Fig. 5 for 2-D view) and also the column of heterotopic bone described above in Fig. 2 on the anteromedial surface (large arrow). The image under a shows normal femoral structure with no ectopic bone on either the anterolateral or anteromedial surfaces. c Micro-CT cross-section of the column of heterotopic bone described above showing marrow cavity with trabecular structure (arrow)
Two-dimensional micro-CT cross-sectional slices and histological analyses were obtained for femurs from rats subjected to surgical induction of HO. Micro-CT and histology reveal a band of heterotopic bone close to the anterolateral surfaces of the femurs (Figs. 4, 5, 6; large white arrows mark HO on the anterior surface; small white arrows mark HO on the lateral surface). This newly formed bone appears to be separated from the femur by a marrow-like space, although it also appears to unite with the femoral cortex at its anterior and lateral surfaces (Figs. 4, 5). The space separating the heterotopic bone from the femur appears to contain trabecular bone (Fig. 4; control bone) and newly formed bone marrow (Fig. 5; shown by black arrow) with fat cells (small white spaces). Micro-CT analysis showed that the bone and tissue mineral densities of the band of putative heterotopic bone observed over the femoral anterolateral surface are significantly less than those of femoral cortical bone (Table 2). Histological analysis shows areas of genuine extraskeletal bone cleanly separated from the femur (Figs. 5, 6; indicated by the cross-hatched arrows).
Effects of celecoxib administration on ectopic bone formation imaged by micro-CT scanning and computer reconstruction. Rats either underwent the surgical procedure to induce HO (Control Group), underwent surgical HO induction and then were orally administered celecoxib at 10 mg/kg for 28 days following surgery (COX-2 Group), or were not operated on (No Surgery). All of the rats in these groups were sacrificed 42 days later. Femurs were removed, scanned by micro-CT and 2-D cross-sectional slices of the scanned femurs were obtained as described in “Materials and methods”. The figure shows micro-CT cross-sectional slices of one representative femur from each of these three experimental groups taken approximately at midshaft level. A band of heterotopic bone in the control and COX-2 groups is observed to form a union with the anterior and lateral surfaces of the femur (as shown by the large and small arrows, respectively). This band was also shown in 3-D in Fig. 3
Ultrastructural analysis of heterotopic bone. At 6 weeks following surgical induction of HO, rats were sacrificed and the femurs were removed from the operated limbs. Femurs were fixed in 10% formalin, dehydrated, decalcified, embedded in PMMA, and 10 μm sections were prepared, stained and examined by light microscopy as described in “Materials and methods”. The figure shows a cross-section of a femur taken approximately at mid-shaft. An area of genuine extraskeletal bone cleanly separated from the femur is indicated by the cross-hatched arrow. A band of heterotopic bone (stained green) can be seen to form a union with the anterior and lateral surfaces as identified by the large and small white arrows, respectively. The heterotopic bone is separated from the femur by newly formed bone marrow (black arrow). Magnification 1 × 20
Ultrastructural analysis of the effects of celecoxib administration on heterotopic bone formation. At 6 weeks following surgical induction of HO, rats in the COX-2 Group were sacrificed and femurs were removed from operated limbs. Femurs were prepared for histological analysis as described in Fig. 5 and “Materials and methods”. The figure shows a cross-section of a femur taken approximately at mid-shaft. An area of genuine extraskeletal bone cleanly separated from the femur is indicated by the cross-hatched arrow. Two bands of heterotopic bone (stained green) can be seen to form a union with the anterior and lateral surfaces as identified by the large and small white arrows, respectively. The heterotopic bone is separated from the femur by newly formed bone marrow (black arrow). Magnification 1 × 20
When the COX-2 inhibitor celecoxib was orally administered at 10 mg/kg for 28 days following surgery (COX-2 Group), the band of heterotopic bone can still be viewed in micro-CT cross-sections of femurs removed after sacrifice at 6 weeks post-surgery (Fig. 4). Ultrastructural analysis of femurs from the COX-2 Group revealed bands of heterotopic bone separated from the cortical bone by newly formed bone marrow. However, each band of HO in the COX-2 Group was narrower and shorter in the anterior-to-posterior dimension compared to the Control Group (Figs. 5, 6; large white arrows mark HO on the anterior surface; small white arrows mark HO on the lateral surface; black arrows mark newly formed bone marrow). In contrast, no heterotopic bone could be seen in any of the cross-sections of femurs in the No Surgery (no surgical induction of HO) group (Fig. 4).
A selective COX-2 inhibitor (celecoxib), selective COX-1 inhibitor (SC-560), or a nonselective COX-1,2 inhibitor (ibuprofen) were each orally administered in pellet form at two different dosages to rats for 4 weeks following surgery to induce HO. The quantitative effects of these experimental treatments on both heterotopic bone content in the vastus lateralis muscle belly of the quadriceps were measured after sacrifice at 42 days post-surgery. Treatment effects on PGE2 levels at various times (1, 7, 14 or 21 days) after surgical induction of HO were also measured.
The content of ectopic bone was quantified directly by micro-CT and computer-assisted analysis as described in “Materials and methods”. HO content differed significantly between the various experimental groups (P < 0.0048). It was also demonstrated that Control HO formation was significantly reduced by 32 and 34% following prophylactic treatment with either a COX-2 (1 mg/kg; P < 0.05) or a nonselective COX-1,2 (10 mg/kg; P < 0.05) inhibitor, respectively (Fig. 7). Treatment with two different dosages of a COX-1 inhibitor (0.1 or 1 mg/kg) failed to produce a statistically significant effect on the content of HO (Fig. 7).
Effects of COX-1, COX-2 and COX-1,2 inhibitors on the amount of ectopic bone formation. The treatment groups were described in Table 1. Animals in the COX treatment groups were orally administered COX inhibitors for 28 days following surgery and thereafter were fed normal rat chow as described in “Materials and methods”. Animals underwent the surgical procedure to induce HO and were sacrificed 42 days later. Femurs were removed, scanned by micro-CT, 2-D cross-sectional slices of the scanned femurs were obtained and ectopic bone content was quantified as described in “Materials and methods”. HO content in the COX treatment groups is expressed as a percentage of HO content in the control HO (surgical induction of HO without COX inhibitor) group and is presented as means ± SE (N = 9–15 femurs). Control HO content = 9.027 ± 0.88 mm2 (mean ± SE). ANOVA indicated that the mean HO content differed significantly between experimental groups (P < 0.0048). * Significantly less than control HO (P < 0.05) based on ANOVA and Tukey–Kramer multiple comparisons test
When the quadriceps content of PGE2 was measured by ELISA, it was shown that baseline (No Surgery Group) levels of 500 ng PGE2/g quadriceps muscle were increased almost 50-fold in the HO Group within 24 h of injury. These peak levels were maintained for 7 days post-surgery and then declined dramatically to near baseline by day 14. Data indicates that even at a low dosage, the COX-2 inhibitor reduced PGE2 to 25% of control HO levels during the first day alone.
When the data were expressed as ng PGE2/mg protein, the same general trends were observed. Within 24 hrs of surgery, prostaglandin synthesis had increased 45- to 50-fold from the baseline (No Surgery) level of 6 ng/mg protein to almost 300 ng/mg protein. At 7 days following surgery, PGE2 levels had increased dramatically and decreased to almost baseline by day 14 (100-fold) compared to the ng PGE2/g wet weight measurement (Fig. 8). The difference observed between the 1- and 7-day experimental groups in PGE2 levels demonstrates that prostaglandin synthesis was continuing to increase up to 1 week post-surgery. The levels of PGE2 synthesis measured in the presence of the COX-1 inhibitor at a dosage of 0.1 mg/kg after 1 day of treatment were very similar to those in the Control HO Group. This dosage has shown to block more than 90% of gastric mucosa COX-1 activity [56]. Our finding supports the view that the COX-1 inhibitor was less potent than the COX-2 inhibitor in its effects on prostaglandin synthesis in the rat HO model. Nevertheless, PGE2 levels were significantly decreased by all three COX inhibitors, at the higher of the two dosage levels, to 5–10% of the Control HO Group level at 1 or 7 days post-surgery (Fig. 8).
Time-dependent changes in the levels of PGE2 in the vastus lateralis muscle belly of the quadriceps during the development of HO and effects of COX inhibitor administration. PGE2 levels are expressed as picograms of prostaglandin per milligram protein of muscle tissue and presented as means ± SE (N = 6–8). PGE2 content was analyzed at 21 days post-surgery only for the Control HO group. ANOVA indicated that the mean HO content differed significantly between experimental groups for the 1-day (P < 0.0006) and 7-day (P < 0.0001) time points. * Significantly greater than No Surgery Group (P < 0.05); ** significantly less than Control HO, day 1 (P < 0.05); *** less than Control HO, day 1 (P < 0.01); + less than Control HO, day 7 (P < 0.001); ++ greater than No Surgery, day 7 (P < 0.001) based on ANOVA and Tukey–Kramer multiple comparisons test. Control PGE2 content = 6.01 ± 0.21 pg/mg protein (mean ± SE)
Discussion
We have demonstrated that this rat HO model reproducibly forms heterotopic bone in all 92 operated limbs. The bone that was observed ectopically contained bone marrow and exhibited a BMD and TMD substantially less than that of femoral cortical bone. This latter finding further supports the induction of HO in this model, since it is more consistent with newly formed (immature) heterotopic bone than with orthotopic bone already formed at the time of surgery. Micro-CT imaging and histology demonstrated the presence of genuine extraskeletal bone cleanly separated from the femur (Figs. 2, 5, 6) or a column of heterotopic bone that most likely first developed in soft tissue and then united with the anteromedial femur. Importantly, we have previously shown that even after the periosteum was covered with bone wax to prevent elevation of the membrane from the cortex and the release of osteoprogenitors, the amount of ectopic bone formed in this model and its distance from the femur were unchanged [7]. The covering of the periosteum also had no impact on the decrement in HO produced by prophylactic treatment with a COX-2 inhibitor [7]. Consequently, although disrupted periosteal cells probably release osteogenic substances such as BMP’s [9] into the surrounding soft tissues, the ossification promoted by our surgical procedure is likely to have developed ectopically and not from periosteal tissue or osteoprogenitors.
Another trauma HO model in rabbits, which also involved periosteal disruption, showed that heterotopic bone formed at a quadriceps site separate from the femur even when the muscle was isolated from the periosteum by a silicon membrane barrier [40]. Also, like our previous study [7], ectopic bone failed to develop in the region of the periosteum between the barrier and the femur, suggesting that periosteal elevation per se did not account for the observed HO when no barrier was employed [40]. In the absence of membrane, the HO in this rabbit model resembled the anterolateral band of ectopic bone observed in the current study since it also coalesced with the femur [40]. These studies [7, 40] and our current results suggest that, following our HO induction procedure, as transplanted bone marrow or muscle-derived stem cells [47] differentiate into osteoblasts, bone initially forms at an ectopic site in muscle and then later grows toward the femur. Therefore, the rat model employed in the current study is likely to stimulate osteoprogenitors in soft tissue close to a site of injury, causing them to differentiate into osteoblasts and form genuine extraskeletal bone, thereby reproducing the basic mechanism of traumatic HO observed following orthopedic surgery.
Of interest is our finding that only the COX-2 inhibitor decreased HO content whereas a COX-1 inhibitor had no effect. The COX-2 inhibitor was also more potent than a COX-1 inhibitor in reducing PGE2 synthesis. We focused on PGE2 because it is the major prostanoid secreted by osteoblastic cells [60]. A number of reports have established that the administration of type E prostaglandins has an overall anabolic effect in bone when applied systemically [31, 41]. We also found that, although PGE2 levels were sharply increased within 1–7 days of HO induction, the levels declined dramatically between 7 and 14 days. This is because there was only a single episode of trauma occurring on day 0. We believe that the transient increase in prostaglandin levels can play an important role in the mechanism of ectopic osteogenesis in our model for a number of reasons. First, PGE2 can increase the expression of osteoblast transcription factors in mesenchymal stem cells after less than 2 weeks of exposure [62]. Second, since PGE2 increases the expression of BMP-2 [63] and BMP-7 [64] in mesenchymal stem cells and osteoblast precursors, respectively, PGE2 may also regulate ectopic osteogenesis via the induction of BMP’s. This induction of BMP’s may occur very early in our model, since we have preliminary results showing that BMP-2 and BMP-7 expression increases dramatically in the injured tissue in our model from 2 to 7 days following HO induction and persists through 14 days (unpublished data). Therefore, the early up regulation of prostaglandins may exert a more longterm regulatory effect on HO that extends well beyond the initial phase of enhanced prostaglandin synthesis. Therefore, our study revealed that surgical induction of HO dramatically increased the tissue levels of a prostaglandin that is likely to regulate bone formation and that the inhibition of COX-2-dependent prostaglandin synthesis was associated with a decrease in the content of HO. Our overall results from the micro-CT and prostaglandin analyses also suggest that prophylactic treatment of HO with a COX-2 or COX-1,2 inhibitor is likely to be effective when given within 1–7 days after surgery and that the clinical usefulness of a more extended treatment period is questionable.
In our HO model, an inflammatory repair process is triggered by surgical injury to soft tissues near bone. Therefore, we hypothesized that the COX-2 isoenzyme, which is up regulated in the process of inflammation [19, 29], is more likely than the COX-1 enzyme to play an important role in this traumatic HO model. This theory is supported by our results, since inhibitors of COX-2 reduced heterotopic bone formation in our model. These results are consistent with other previous reports showing that COX-2 −/− knockout mice have decreased bone density [45], suggesting that COX-2 is required for intramembranous and endochondral bone repair [62]. In the latter study, measures of new bone growth in several inflammatory and non-inflammatory in vivo models of skeletal remodeling showed a 60–80% decline in the COX-2 knockout mouse compared to wild type [62]. A more recent report showed that in a model of BMP-2-induced bone formation, mineralization was decreased almost 80% in COX-2 knockout mice compared to the wild type [16]. Another recent study showed that the selective blockade of COX-2 inhibited HO induced by the implantation of demineralized bone matrix in a rat muscle pouch in 40% of the treated rats, although the results were not statistically significant [43]. We showed here that COX-2 inhibition decreased HO content by only 32–34%. However, it is important to note that PGE2 levels remained two to tenfold that of baseline (No Surgery) levels after administration of a COX-2 inhibitor or COX-1,2 inhibitor (Figs. 7, 8). Our results suggest that if higher dosages had been employed, COX-2 activity and HO content may have been further reduced. Therefore, all of these findings strongly suggest that COX-2 is required to a significant degree for normal as well as heterotopic bone formation.
Despite our findings that inhibitors of COX-2 or COX-1 reduced prostaglandin levels, it is not clear whether PGE2 can be synthesized directly via the COX-2 or COX-1 (or both) pathways in the surgically injured muscle. It is also unclear why a COX-1-selective inhibitor decreased prostaglandin synthesis to the same degree as COX-2 inhibitors in our HO model. One report has demonstrated that the expression of both COX-1 and COX-2 mRNA is increased in the affected muscles of patients with inflammatory myopathies [57]. These findings [57] suggest that in the current study, COX-1 and COX-2 each contribute to the synthesis of prostaglandins in the injured muscle during its repair. It is also possible that, in this trauma model, one COX isoenzyme can regulate prostaglandin levels by altering the activity of the other isoenzyme. This could explain why inhibitors of COX-1 and COX-2 were each capable of reducing PGE2 content by 80–90% in our study. It has been demonstrated that traditional NSAID’s that inhibit COX-1 and COX-2 suppress inflammatory cytokine-induced COX-2 mRNA and protein expression [49, 59] and phospholipase-mediated production of arachidonic acid substrate for the COX-2 enzyme [61]. Therefore, COX-1 may even stimulate prostaglandin synthesis indirectly by up regulating COX-2 activity. Nevertheless, even if COX-1 directly regulated PGE2 synthesis or acted indirectly through COX-2, our results suggest that COX-1 is not involved in the mechanism of traumatic HO.
The mechanism by which COX-2 inhibitors reduce HO in our model remains to be elucidated. A recent study showed that bone formation was decreased substantially in the COX-2 knockout mouse but remained unimpaired in the COX-1 knockout mouse compared to the wild type. Furthermore, exogenous PGE2 restored the expression of the key osteoblast transcription factors cbfa1 and osterix in stem cells from the COX-2 knockout mouse to wild type levels, suggesting an obligate role for PGE2 in the regulation of bone formation by COX-2 [62]. In contrast, we report here that inhibiting nearly 90% of PGE2 synthesis with a COX-1 inhibitor is not sufficient to reduce the formation of ectopic bone in a trauma model. This suggests that COX-2 inhibitors decrease HO through effects on other osteogenic factors in addition to PGE2. The role of COX-2 or COX-1-dependent synthesis of PGE2 in traumatic HO will be further explored using genetic knockout mice in a future investigation.
The lack of a direct relationship between PGE2 and HO content may be explained by the complex functional role of COX-2. It was originally believed that COX-2 was exclusively a source of inflammatory and pathologic prostaglandins associated with tumor angiogenesis, tumorigenesis and Alzheimer’s disease [19]. More recently, this inducible isoenzyme has been found to regulate a number of normal physiological functions [29, 30] in the brain, kidney, pancreas, intestine and blood vessels [58] under conditions in which COX-1 may be poorly expressed. For example, COX-2 catalyzes the synthesis of prostacyclin [39, 46] in vascular endothelial cells, which promotes vasodilatation. It has also been suggested that COX-2 may resolve the pathology of inflammation and wound/gastric ulcer healing perhaps by generating alternative series of prostaglandins such as the cyclopentenone prostaglandins [18]. Therefore, COX-2 might regulate HO through prostaglandins other than PGE2. Moreover, other recent studies have demonstrated that NSAID’s and selective COX-2 inhibitors act independently of COX activity [30, 26]. Some of the COX-independent actions of COX-1 and COX-2 inhibitors include the regulation of cellular signaling molecules such as protein kinase G, NF-kappa B and the antiapoptotic protein Bcl-XL [26]. Some of these COX-independent actions may actually decrease ectopic osteogenesis which could explain why the COX-1,2 inhibitor had a weaker effect at the higher dosage compared to the lower dosage. Therefore, the effects of the COX-2 inhibitors celecoxib and ibuprofen on HO in the rat model studied here may involve the inhibition of prostaglandins other than PGE2 or other COX-independent effects. These effects could explain the poor relationship between HO and PGE2 levels or COX-1,2 inhibitor dosage.
Our findings that inhibitors of COX-1 and COX-2 have different effects on traumatic HO might also be explained by their levels of tissue and cellular expression. It has been shown that when three distinct cell types were examined in muscle, endothelial cells and inflammatory cells in normal muscle tissue were found to synthesize higher levels of COX-1 and COX-2 mRNA compared to muscle cells [57]. However, when dystrophic muscle was analyzed, only COX-2 expression was increased in muscle cells with no changes observed in COX-2 levels in the other two cell types studied compared to normal muscle [57]. Therefore, it is possible in our HO model that muscle cells of the traumatized quadriceps produce significant amounts of COX-2 but not COX-1. It is also possible that COX-2-dependent PGE2 produced by injured or necrotic myocytes induces HO through paracrine effects on nearby osteogenic stem cells. Conversely, the significant constitutive activity of COX-1 demonstrated by vascular endothelial cells or inflammatory cells in muscle [57] may be unrelated to the mechanism of HO yet contribute greatly to the whole muscle concentrations of PGE2 measured in this study. This may explain why only the COX-2 inhibitors reduced HO content even though the COX-1 inhibitor also decreased PGE2 synthesis.
It has recently been reported that the COX-2 inhibitor, celecoxib demonstrated the same efficacy as indomethacin in the prevention of HO after total hip arthroplasty with significantly fewer side effects [51]. However, COX-2 inhibitors have been demonstrated to have adverse effects on the cardiovascular system [52, 12]. These studies and others discussed above have demonstrated that the biological effects of inhibitors of COX, especially COX-2, are highly complex and deserving of further study to improve their clinical safety and effectiveness. We have utilized a rat model of traumatic HO to investigate the function of COX-2 in bone remodeling and found that a COX-2 inhibitor showed a greater prophylactic efficacy toward HO compared to a COX-1 inhibitor. Our findings strongly suggest that COX-2 inhibitors would be as effective or more effective in the prevention of severe forms of HO than non-selective COX inhibitors that have a wider range of side effects. However, the elucidation of basic mechanisms of HO is especially important given that no treatment strategy has yet to be developed which is completely effective and safe in preventing all forms of traumatic HO. Future studies will identify the cell types and molecular regulatory molecules that are necessary for the development of traumatic HO.
References
Ahrengart L, Blomgren G, Tornkvist H (1994) Short-term ibuprofen to prevent ossification after hip arthroplasty. No effects in a prospective randomized study of 47 arthrosis cases. Acta Orthop Scand 65:139–141
Anderson HC (1976) Osteogenetic epithelial–esenchymal cell interactions. Clin Orthop 119:211–223
Anderson HC, Merker PC, Foch J (1964) Formation of tumors containing bone after intramuscular injection of transformed human amnion cells (Fl) into cortisone-treated mice. Am J Pathol 44:507–519
Bartlett CS, Rapuano BE, Lorich DG Wu T, Hsu JF, Lane JM, Helfet DL (2006) Early changes in prostaglandins precede bone formation in a rabbit model of heterotopic ossification. Bone 38:322–332
Bauer FC, Nilsson OS, Tornkvist H (1984) Formation and resorption of bone induced by demineralized bone matrix implants in rats. Clin Orthop 191:139–143
Bensen WG, Fiechtner JJ, McMillen JI, Zhao WW, Yu SS, Woods EM, Hubbard RC, Isakson PC, Verburg KM, Geis GS (1999) Treatment of osteoarthritis with celecoxib, a cyclooxygenase-2 inhibitor: a randomized controlled trial. Mayo Clin Proc 74:1095–1105
Borens O, Rapuano BE, Tomin A, Lane JM, Helfet DL (2004) The effect of COX-2 inhibitors on the formation of heterotopic bone in a new rat model. J Bone Joint Surg 86-B(suppl III):259. (Privileged communication)
Bosse MJ, Poka A, Reinert CM, Ellwanger F, Slawson R, McDevitt ER (1988) Heterotopic ossification as a complication of acetabular fracture. Prophylaxis with low-dose irradiation. J Bone Joint Surg Am 70:1231–1237
Bostrom MP, Lane JM, Berberian WS, Missri AA, Tomin E, Weiland A, Doty SB, Glaser D, Rosen VM (1995) Immunolocalization and expression of bone morphogenetic proteins 2 and 4 in fracture healing. J Orthop Res 13:357–367
Brady LW (1979) Radiation-induced sarcomas of bone. Skeletal Radiol 4:72–78
Brophy JM (2005) Celecoxib and cardiovascular risks. Expert Opin Drug Saf 4:1005–1015
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement: Incidence and a method of classification. J Bone Joint Surg 55-A:1629–1632
Cella JP, Salvati EA, Sculco TP (1988) Indomethacin for the prevention of heterotopic ossification following total hip arthroplasty. Effectiveness, contraindications, and adverse effects. J Arthroplasty 3:229–234
Chantraine A, Minaire P (1981) Para-osteo-arthropathies: a new theory and mode of treatment. Scand J Rehabil Med 13:31–37
Charnley J (1972) The long term results of low-friction arthroplasty of the hip performed as primary intervention. J Bone Joint Surg [Br] 54:61–76
Chikazu D, Li X, Kawaguchi H, Sakuma Y, Voznesensky OS, Adams DJ, Xu M, Hoshi K, Katavic V, Herschman HR, Raisz LG, Pilbeam CC (2002) Bone morphogenetic protein 2 induces cyclo-oxygenase 2 in osteoblasts via a cbfa1 binding site: role in effects of bone morphogenetic protein 2 in vitro and in vivo. J Bone Miner Res 17:1430–1440
Collins M, Stone M, Harkess JW, Bliven FE (1965) Experimental myositis ossificans in dogs. J Bone Joint Surg Am 47:1277
Colville-Nash PR, Gilroy DW (2001) Potential adverse effects of cyclooxygenase inhibition: evidence from animal models of inflammation. BioDrugs 15:1–9
Dannhardt G, Kiefer W (2001) Cyclooxygenase inhibitors—current status and future prospects. Eur J Med Chem 36:109–126
Daum WJ, Scarborough MT, Gordon W Jr, Uchida T (1992) Heterotopic ossification and other perioperative complications of acetabular fractures. J Orthop Trauma 6:427–432
Feldkamp LA, Goldstein SA, Parfitt AM, Jesion G, Kleerekoper M (1989) The direct examination of three-dimensional bone architecture in vitro by computed tomography. J Bone Miner Res 4:3–11
Fort J (1999) Celecoxib, a COX-2-specific inhibitor: the clinical data. Am J Orthop 28:13–18
Foster DE, Hunter JR (1987) The direct lateral approach to the hip for arthroplasty. Advantages and complications. Orthopedics 10:274
Fritton JC, Myers ER, Wright TM, van der Meulen MCH (2005) Loading induces site-specific increases in mineral content assessed by microcomputed tomography of the mouse tibia. Bone 36:1030–1038
Garland DE (1991) A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop 263:13–29
Gately S, Kerbel R (2003) Therapeutic potential of selective cyclooxygenase-2 inhibitors in the management of tumor angiogenesis. Prog Exp Tumor Res 37:179–192
Gebuhr P, Soelberg M, Orsnes T, Wilbek H (1991) Naproxen prevention of heterotopic ossification after hip arthroplasty. A prospective control study of 55 patients. Acta Orthop Scand 62:226–229
Geis GS (1999) Update on clinical developments with celecoxib, a new specific COX-2 inhibitor: what can we expect? J Rheumatol 26(suppl 56):31–36
Hinz B, Brune K (2002) Cyclooxygenase-2—10 years later. J Pharmacol Exp Ther 300:367–375
Jacquemin C (2000) Biological functions of cyclooxygenase 2: control of its expression and activity. J Soc Biol 194:189–193
Jee WSS, Ma YF, Li M et al (1994) Sex steroids and prostaglandins in bone metabolism. In: Sex steroids and bone. Ernst Schering Research Foundation Workshop 9. Springer, Heidelberg, p 119
Jorgensen SM, Demirkaya O, Ritman EL (1998) Three-dimensional imaging of vasculature and parenchyma in intact rodent organs with X-ray micro-CT. Am J Physiol 275:H1103–H1114
Kim JH, Chu FC, Woodard HQ, Melamed MR, Huvos A, Cantin J (1978) Radiation-induced soft-tissue and bone sarcoma. Radiology 129:501–508
Kjaersgaard-Andersen P, Ritter MA (1992) Short-term treatment with nonsteroidal antiinflammatory medications to prevent heterotopic bone formation after total hip arthroplasty. A preliminary report Clin Orthop 279:157–162
Lane NE (1997) Pain management in osteoarthritis: the role of COX-2 inhibitors. J Rheumatol 24(suppl 49):20–24
Lipsky PE, Isakson PC (1997) Outcome of specific COX-2 inhibition in rheumatoid arthritis. J Rheumatol 24(suppl 49):9–14
Martinez RV, Reval M, Campos MD, Terron JA, Dominguez R, Lopez-Munoz FJ (2002) Involvement of peripheral cyclooxygenase-1 and cyclooxygenase-2 in inflammatory pain. J Pharm Pharmacol 54:405–412
McAdam BF, Catella-Lawson F, Mardini IA, Kapoor S, Lawson JA, Fitzgerald GA (1999) Systemic biosynthesis of prostacyclin by cyclooxygenase (COX)-2: the human pharmacology of a selective inhibitor of COX-2. Proc Natl Acad Sci USA 96:272–277
Michelsson J-E, Pettila M, Valtakari T, Leivo I, Aho HJ (1994) Isolation of bone from muscles prevents the development of experimental callus-like heterotopic bone. Clin Orthop Relat Res 302:266–272
Miller SC, Marks SC Jr (1993) Local stimulation of new bone formation by prostaglandin E1: quantitative histomorphometry and comparison of delivery by minipumps and controlled release pellets. Bone 14:143
Moed BR, Karges DE (1994a) Prophylactic indomethacin for the prevention of heterotopic ossification after acetabular fracture surgery in high-risk patients. J Orthop Trauma 8:34–39
Moed BR, Letournel E (1994b) Low dose irradiation and indomethacin prevent heterotopic ossification after acetabular fracture surgery. J Bone J Surg Br. 76:895–900
Murat N, Hocaoglu N, Karatosun V, Yorukoglu K, Gidener S, Gunal I (2005) The effects of non-selective and cyclooxygenase-2-selective non-steroidal anti-inflammatory drugs on heterotopic ossification in rats. Med Sci Monit 11:BR449–BR451
O’Connor JP (1998) Animal models of heterotopic ossification. Clin Orthop Rel Res 346:71–80
Okada Y et al (2000) Effects of cyclooxygenase-2 gene disruption on osteoblastic function. J Bone Miner Res 15(suppl):217
Oviedo JA, Wolfe MM (2001) Clinical potential of cyclo-oxygenase-2 inhibitors. BioDrugs 15:563–572
Ozeki N, Lim M, Yao CC, Tolar M, Kramer RH (2006) Alpha7 integrin expressing human fetal myogenic progenitors have stem cell-like properties and are capable of osteogenic differentiation. Exp Cell Res 312:4162–4180
Paik JH, Ju JH, Lee JY, Boudreau MD, Hwang DH (2000) Two opposing effects of non-steroidal anti-inflammatory drugs on the expression of the inducible cyclooxygenase: mediation through different signaling pathways. J Biol Chem 275:28173–28179
Penning TD, Talley JJ, Bertenshaw SR et al (1997) Synthesis and biological evaluation of the 1,5-diarylpyrazole class of cyclooxygenase inhibitors: identification of 4-[-5-(4-methylphenyl)-3-(trifluoromethyl)-1H-pyrazole-1-yl]benzenesulfonamide (SC-58635, Celecoxib). J Med Chem 40:1347–1365
Powell WS (1980) Rapid extraction of oxygenated metabolites of arachidonic acid from biological samples using octadecylsilyl silica. Prostaglandins 20:947–957
Romano CL, Duci D, Romano D, Mazza M, Meani E (2004) Celecoxib versus indomethacin in the prevention of heterotopic ossification after total hip arthroplasty. J Arthroplasty 19:14–18
Sanghi S, MacLaughlin EJ, Jewell CW, Chaffer S, Naus PJ, Watson LE, Dostal DE (2006) Cyclooxygenase-2 inhibitors: a painful lesson. Cardiovasc Hematol Disord Drug Targets 6:85–100
Schmidt SA, Kjaersgaard-Andersen P, Pedersen NW, Kristensen SS, Pedersen P, Nielsen JB (1988) The use of indomethacin to prevent the formation of heterotopic bone after total hip replacement. A randomized, double-blind clinical trial. J Bone Joint Surg Am 77:834–838
Schneider DJ, Moulton MJ, Singapuri K, Chinchilli V, Deol GS, Krenitsky G, Pellegrini VD Jr (1998) The Frank Stinchfield Award. Inhibition of heterotopic ossification with radiation therapy in an animal model. Clin Orthop 355:35–46
Simon LS, Lanza FL, Lipsky PE, Hubbard RC, Talwalker S, Schwartz BD, Isakson PC, Geis GS (1998) Preliminary study of the safety and efficacy of SC-58635, a novel cyclooxygenase 2 inhibitor: efficacy and safety in two placebo-controlled trials in osteoarthritis and rheumatoid arthritis, and studies of gastrointestinal and platelet effects. Arthritis Rheum 41:1591–1602
Smith CJ, Zhang Y, Koboldt CM, Muhammad J, Zweifel BS, Shaffer A, Talley JJ, Masferrer JL, Seibert K, Isakson PC (1998) Pharmacological analysis of cyclooxygenase-1 in inflammation. Proc Natl Acad Sci USA 95:13313–13318
Studynkova JT, Kuchen S, Jeisy F, Schedel J, Charvat F, Jarosova K, Sprott H, Matucci-Cerinic M, Michel BA, Pavelka K, Vencovsky J, Gay S (2004) The expression of cyclooxygenase-1, cyclooxygenase-2 and 5-lipoxygenase in inflammatory muscle tissue of patients with polymyositis and dermatomyositis. Clin Exp Rheumatol 22:395–402
Warner TD, Mitchell JA (2004) Cyclooxygenases: new forms, new inhibitors, and lessons from the clinic. FASEB J 18:790–804
Xu XM, Sansores-Garcia L, Chen XM, Matijevic-Aleksic N, Du M, Wu KK (1999) Suppression of inducible cyclooxygenase 2 gene transcription by aspirin and sodium salicylate. Proc Natl Acad Sci USA 96:5292–5297
Yokota K, Kusaka M, Oshima T, Yamamoto S, Kurihara N, Yoshino T, Kumegawa M (1986) Stimulation of prostaglandin E2 synthesis in cloned osteoblastic cells of mouse (MC3T3-E1) by epidermal growth factor. J Biol Chem 261:15410–15415
Yuan CJ, Mandal AK, Zhang Z, Mukherjee AB (2000) Transcriptional regulation of cyclooxygenase-2 gene expression: novel effects of non-steroidal anti-inflammatory drugs. Cancer Res 60:1084–1091
Zhang X, Schwarz EM, Young DA, Puzas JE, Rosier RN, O’Keefe RJ (2002) Cyclooxygenase-2 regulates mesenchymal cell differentiation into the osteoblast lineage and is critically involved in bone repair. J Clin Invest 109:1405–1415
Arikawa T, Omura K, Morita I (2004) Regulation of bone morphogenetic protein-2 expression by endogenous prostaglandin E2 in human mesenchymal stem cells. J Cell Physiol 200:400–406
Paralkar VM et al (2002) Regulation of BMP-7 expression by retinolic acid and prostaglandin E(2). J Cell Physiol 190:207–217
Acknowledgments
We thank Dillenia Reyes, Roy Chen, Ceshea Wooten, William Chuang and Simon Morr for their excellent assistance with prostaglandin extraction, protein assays, micro-CT scanning or reconstruction. We also thank Lyuda Lukashova for her assistance with the micro-CT analysis. All of the experiments performed for this study were in full compliance with the laws of the United States of America. This investigation was supported by a grant from Pharmacia, Inc. to (Rapuano BE, Lane JM and Helfet DL) and by VA Merit Grant No. 2894-005 (PI—MacDonald DE).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rapuano, B.E., Boursiquot, R., Tomin, E. et al. The effects of COX-1 and COX-2 inhibitors on prostaglandin synthesis and the formation of heterotopic bone in a rat model. Arch Orthop Trauma Surg 128, 333–344 (2008). https://doi.org/10.1007/s00402-007-0436-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0436-2