Abstract
Introduction
The aim of this study was to describe early results of a new internal locking system, PHILOS, used for the treatment of proximal humeral fractures.
Materials and methods
A chart and radiographic review of 25 cases that had proximal humeral internal locking system (PHILOS) plate for the treatment of proximal humeral fractures was performed.
Results
Of the 25 cases, 20 went to union with a mean neck/shaft angle of 127.2°. Five cases required or were considered for revision surgery for non-union or implant failure. Of the 25 implants, 4 had screw protrusion into the gleno-humeral joint, 4 had screw loosening and backing out, and 1 plate broke without further trauma.
Conclusions
Our results suggest that PHILOS is an effective system for providing fracture stabilisation to bony union but awareness of potential hardware complications is essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traditional internal fixation stabilisation methods for proximal humeral fractures include semi-rigid (percutaneous k-wiring, screw fixation, tension band wiring) [3, 15] and rigid (conventional plates and screws, intramedullary nailing) [1, 2, 5, 7, 8, 11–16] means. The proximal humeral internal locking system (PHILOS, Stratec Medical) is a new implant designed for the fixation of proximal humeral fractures and is one of a new generation of locking plates [4, 10]. Its shape is anatomical, conforming to the proximal humerus. In the humeral head component of the plate, locking screws are inserted in multiple directions into the humeral head. In the shaft component of the implant combi-holes provide the option of locking or non-locking screws to be inserted. Smaller holes allow the passage of sutures or wires to help reattachment of the greater and lesser tuberosities. The implant comes in short and long sizes with three and five shaft combi-holes, respectively.
The aim of this study was to describe early results of this implant, in particular potential implant related complications.
Methods
This was a clinical and radiographic review of patients with proximal humeral fractures treated with PHILOS plate at the East Lancashire NHS trust, UK. Patients were identified by reviewing the theatre and the hospitals’ clinical coding registries. Patients’ records were reviewed with regards to demographics, operative details and post-operative outcome. Fractures were classified using Neer’s [9] classification system. Radiographic evaluation was performed to assess for union, mal-union, implant loosening and hardware related complications. The neck-shaft angle [1, 6] was measured for all fractures that united, on the best AP projection radiograph following union, using an electronic goniometer (Scale version 2.0, ©Ricardo Sgrillo, 2001, Freeware). For those fractures classified as mal-union the neck-shaft angle was also assessed in the final intra-operative or first post-operative films to determine whether mal-union was the result of poor initial reduction or post-operative fracture displacement. For the purpose of this study union was defined as the patient reporting no shoulder pain or only mild activity related pain and having no loss of the initial fracture reduction or evidence of implant loosening, breakage, along with evidence of internal or external callous formation [13]. The presence of pain due to some other obvious cause such as protruding screws or adhesive capsulitis did not exclude the diagnosis of union. Non-union was defined as failure of union for 6 months post-fixation. Mal-union was defined as healing of the fracture with a neck/shaft angle of less than 120° or more than 145° on an antero-posterior radiograph. In this study each PHILOS plate used was considered as a separate index episode. During the study period PHILOS was the main implant used for open reduction and internal fixation of proximal humeral fractures at our institution.
Results
During the study period, 25 PHILOS fixations were performed in 23 patients for proximal humeral fractures. Their demographics are shown in Table 1. The delto-pectoral approach was used in 24 and deltoid split in one. Seventeen PHILOS plates were performed for the fixation of acute fractures and eight for delayed or non-united fractures, or for previously used hardware failure. All patients were followed up at least until union or until it was decided they needed revision surgery. Follow up ranged from 3 to 18 months (median 6 months).
In 20 PHILOS fixations the fractures united, whereas 5 PHILOS fixations underwent or were decided to need revision surgery, either for non-union or implant failure. The mean neck shaft angle was 127.2° (range 103°–140°) with three mal-unions. The results are presented separately for the acute fractures and those treated for delayed/non-unions or metalwork failure.
PHILOS used for acute fractures
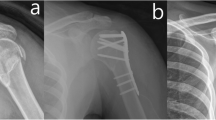
Seventeen PHILOS plates were used for the treatment of acute fractures, with surgery performed within a median of 4 days (range 1–16) from injury. Six long and 11 short plates were used, with one case having bone grafting. Fourteen of the 17 acute fractures went to union (Fig. 1) whilst 3 had to be revised.
Acute fractures: cases that united
Of those fractures that united, three mal-united. In two of these the fracture was not adequately reduced, with a neck-shaft angle of 119° and 108° in the immediate post-operative period and 113° and 103°, respectively, at final follow up. In the third patient, the immediate post-operative neck-shaft angle was 127° and the final 118°, suggesting that post-operative fracture collapse was responsible for mal-union.
In one patient, following a further injury, it was found that the humeral head screws loosened and backed out, causing persisting discomfort. In 1 of the 14 cases that united, the head screws were found post-operatively to be protruding into the gleno-humeral joint, but were asymptomatic (Fig. 2 a). The screws were not seen protruding into the joint intra-operatively. One case, a 47-year-old male with a 4-part fracture dislocation, developed radiological evidence of avascular necrosis diagnosed at 7 months post-operatively and also required manipulation under anaesthesia for post-operative adhesive capsulitis. One case developed a chronic discharging sinus.
Acute fractures: cases requiring revision
Three acute fractures developed significant complications and required revision. The first case was of an 83-year-old male with a four-part fracture, the screws loosened and backed out from the humeral head, the fracture displaced 26 days following surgery and this was revised to shoulder hemi-arthroplasty. In the second case, of a 63-year-old male with a history of alcohol abuse and a two-part fracture, the locked shaft screws loosened and backed out, and the fracture displaced about 2 months post-surgery (fig. 2b). This patient is awaiting medical investigations for black-outs before proceeding with revision surgery. In the third case, of a 57-year-old female with a two-part acute fracture, one screw required removal because of protrusion into the gleno-humeral joint that caused persistent pain (this was not recognised intra-operatively). This case eventually went on to non-union and was revised to a new PHILOS, 10 months post initial surgery.
PHILOS used for delayed/non-union or metalwork failure
Eight cases were operated for delayed/non-union or hardware failure. These were operated at a median of 4.5 months (range 28 days to 15 months). Of these, the initial fixation was PHILOS in two cases (one of which was described in the acute fracture section above, used in a two-part fracture of a 57-year-old female, whilst the other was a PHILOS used for a non-union and is described in a greater detail below), clover-leaf non-locking plate in another, whilst the rest were initially managed non-operatively. Three long and five short plates were used. All cases had bone grafting.
In six of the eight cases where PHILOS was used for delayed/non-unions or metalwork failure, the fractures united. Amongst these six cases, there were two where the humeral head screws were found post-operatively to be protruding into the gleno-humeral joint, but were asymptomatic and needed no further treatment. In none of these was the screw penetration apparent intra-operatively.
The two PHILOS, which failed were used in a 77-year-old male with a three-part fracture. He was treated initially for non-union 7 months post-injury, using a titanium PHILOS that broke about 11 weeks post-operatively without any history of further trauma. This was then revised to a new PHILOS, but 6 months post-revision the humeral head screws loosened and backed out and the fracture failed to unite. At that point it was decided not to undertake any further treatment.
The complications for all the cases of PHILOS plates in this study are summarised in Tables 2 and 3.
Discussion
PHILOS is one of a new generation of internal fixation locking plate systems [4, 10]. Locking the screws onto the plate has a similar effect to a blade-plate. As the humeral head screws are orientated in multiple directions the effect is similar to providing a blade-plate like fixation in multiple planes. In this study we examined the early results of internal fixation of PHILOS. We looked separately at acute fractures and those treated for delayed/non-union or metalwork failure, as the management of the latter tends to be more challenging.
As demonstrated by our results, the PHILOS system stabilised the fracture to union in a satisfactory position, in the majority of fractures in both groups we examined. However, a high rate of hardware related complications are evident in both acute fractures as well those treated for delayed/non-union or previous metalwork failure. Seven of 17 (41%) acute fractures and 4 of 8 (50%) delayed/non-union fractures treated with the PHILOS, developed a complication. This high complication rate may be due to the fact that proximal humeral fractures are a difficult entity to treat, or it may be a reflection of the design, operative technique or steep learning curve associated with this implant.
In four cases, the humeral head screws were found to be protruding into the gleno-humeral joint. Review of the intra-operative radiographs showed that in one case the protrusion was missed intra-operatively. In the remaining three, it became apparent only post-operatively. Although it is possible that in these three cases inadequate intra-operative screening was the cause of screw protrusion, this complication may also have been due to early post-operative fracture collapse. Both implant design and surgical technique may contribute to this. The locking of the screws onto the plate aims at preventing their backing out. Thus if fracture collapse occurs, the screws may penetrate the articular surface, protruding into the gleno-humeral joint. This may be more likely to happen if long screws are used with their tips placed very close to the articular surface, or if the articular surface is in-adversely penetrated during drilling. Furthermore, as screws are placed in multiple directions into the humeral head, excessive intra-operative screening is essential to ensure that there is no breaching of the articular surface. Fracture collapse and articular surface penetration was a major complication of a previously reported locking system, which led its authors to suggest that it was unsatisfactory for patients with osteopenic bone. In that study, Sadowski et al. [14] reported on seven patients treated with the PlantTan humerus fixator plate (Medizintechnik GmbH, Aachen, Germany), a plate system aiming at providing rotational and angular stability using two cancellous screws placed into the humeral head that are then locked onto the plate using a transverse compression screw. Of their seven patients, all four that were older than 75 years old had failed fixation, with the screws penetrating the articular surface of the head in three and secondary fracture displacement in the other. In our study, only one of three patients who showed screw protrusion post-operatively was older than 75, suggesting that this potential complication is not necessarily limited only to severely osteoporotic bone.
In four cases, locking screws loosened and backed out, in three from the humeral head, and in one from the humeral shaft. This could be explained either by inadequate locking of the screws onto the plate or by micro-motion between the screw and plate threads. PHILOS instrumentation system provides a drill sleeve which screws onto the plate to ensure that the direction of drilling and thus screw insertion is such that locking of the screws onto the plate is optimal. In addition, a torque limiter (limit of 1.5 nm) can be attached to the screwdriver to further ensure that adequate locking is performed. Failure to pay particular attention to the above may result in inadequate locking and thus backing out of the screws. However, we observed that loosening and backing out of screws occurred even in cases where meticulous attention was paid to locking, which suggests that micro-motion may be a potential cause of loosening. In one case, a PHILOS plate broke without any history of further injury. This was a titanium plate, which questions the strength of plates made of this material. Review of the radiographs of this case did not show any obvious other biomechanical factor to explain such an early failure.
The hardware complication rate observed in this study is similar to that reported previously for other commonly used implants. Bernard et al. [2] reported on 11 proximal humeral fractures treated with the Polarus nail, of which 4 (36%) required further surgery for failed fixation, and 2 (18%) had backed out proximal screws. More recently, Agel et al. [1] reported proximal screw loosening in 3 of 20 (15%) Polarus nails used for proximal humeral fracture fixation, and 2 (10%) required revision for proximal fixation failure. In a report by Hintermann et al. [5], of 42 proximal humeral fractures in elderly patients treated by blade plate fixation, 6 (14%) required implant removal, although the exact reasons for this were not stated. Similarly, 2 of 27 (7%) T-buttress plates used for severely displaced proximal humeral fractures were removed for loosening, in a report by Kristiansen [7], whereas results in 12 of 14 (86%) fractures treated with AO plating were reported unsatisfactory mainly due to fixation failure [12]. Wijgman et al. [15] reported poor results in 8 of 60 (13%) patients treated with open reduction and internal fixation using either cerlage wire or a T-plate, at an average of 10 years follow up. As stated above, hardware related complications, in terms of articular surface penetration and fixation failure, were seen in 4 of 7 (57%) patients treated with the PlantTan Humerus fixator plate [14]. The results of that initial study have been supported by two more recent studies. Burton et al. [3] looked at 16 fractures treated with PlantTan. Avascular necrosis was seen in 25% of their cases, all in patients over 70. Hence they concluded that this implant should not be used in elderly patients. Similarly, Machani et al. [8] reported on 62 cases treated with the PlantTan plate. In their series, there were 8 (13%) fixation failures, 2 (3%) cases of avascular necrosis and non-union and 5 (8%) cases where the implant had to be removed for pressure symptoms. On the basis of those results those authors stopped using the PlantTan implant.
There are certain limitations to this study. Neck shaft angle was assessed only in one plane using antero-posterior radiographs. It would have been desirable to assess retroversion/anteversion on a lateral radiograph. However, given the retrospective nature of the study standardised lateral radiographs were not available. Clinical evaluation with functional scoring would be desirable however, could not be done as many patients had been discharged from clinic by the time of the study and some were no longer living locally.
In summary, our study suggests that PHILOS can be an effective implant in providing fracture stabilisation of proximal humeral fractures. Understanding the potential hardware complications, and limitations of this system, is vital in anyone intending to use PHILOS for the treatment of such fractures.
References
Agel J, Jones CB, Sanzone AG, Camuso M, Henley MB (2004) Treatment of proximal humeral fractures with polarus nail fixation. J Shoulder Elbow Surg 13:191–195
Bernard J, Charalambides C, Aderinto J, Mok D (2000) Early failure of intramedullary nailing for proximal humeral fractures. Injury 31:789–792
Burton D, Wells G, Watters A, Schilders E, Venkateswaran B (2005) Early experience with the PlantTan fixator plate for 2 and 3 part fractures of the proximal humerus. Injury 36:1190–1196
Haidukewych GJ (2004) Innovations in locking plate technology. J Am Acad Orthop Surg 12:205–212
Hintermann B, Trouillier H, Schafer D (2000) Rigid internal fixation of fractures of the proximal humerus in older patients. J Bone Joint Surg Br 8:1107–1112
Iannotti JP, Gabriel JP, Schneck SL, Evans BG, Misra S (1992) The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am 74:491–500
Kristiansen B, Christensen SW (1986) Plate fixation of proximal humeral fractures. Acta Orthop Scand 57:320–323
Machani B, Sinopidis C, Brownson P, Papadopulos P, Gibson J, Frostick SP (2006) Mid term results of PlantTan plate in the treatment of proximal humeral fractures. Injury 37:269–276
Neer CS II (1970) Displaced proximal humeral fractures. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Perren S (2003) Backgrounds of the technology of internal fixators. Injury 34:S-B1–S-B3
Rajasekhar C, Ray P, Bhamra M (2001) Fixation of proximal humeral fractures with the polarus nail. J Shoulder Elbow Surg 10:7–10
Robinson CM, Christie J (1993) The two part-proximal humeral fracture: a review of operative treatment using two techniques. Injury 24:123–125
Robinson CM, Page R (2003) Severely impacted valgus proximal humeral fractures. J Bone Joint Surg Am 9:1647–1655
Sadowski C, Riand N, Stern R, Hoffmeyer P (2003) Fixation of fractures of the proximal humerus with the PlantTan humerus fixator plate: early experience with a new implant. J Shoulder Elbow Surg 12:148–151
Wijgman A, Roolker W, Patt T, Raaymakers E, Marti R (2002) Open reduction and internal fixation of three and four part fractures of the proximal part of the humerus. J Bone Joint Surg Am 84:1919–1924
Zyto K, Ahrengart L, Sperber A, Tornkvist H (1997) Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br 3:412–417
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Charalambous, C.P., Siddique, I., Valluripalli, K. et al. Proximal humeral internal locking system (PHILOS) for the treatment of proximal humeral fractures. Arch Orthop Trauma Surg 127, 205–210 (2007). https://doi.org/10.1007/s00402-006-0256-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-006-0256-9