Abstract
Medulloblastoma is heterogeneous, being characterized by molecular subgroups that demonstrate distinct gene expression profiles. Activation of the WNT or SHH signaling pathway characterizes two of these molecular subgroups, the former associated with low-risk disease and the latter potentially targeted by novel SHH pathway inhibitors. This manuscript reports the validation of a novel diagnostic immunohistochemical method to distinguish SHH, WNT, and non-SHH/WNT tumors and details their associations with clinical, pathological and cytogenetic variables. A cohort (n = 235) of medulloblastomas from patients aged 0.4–52 years was studied for expression of four immunohistochemical markers: GAB1, β-catenin, filamin A, and YAP1. Immunoreactivity (IR) for GAB1 characterizes only SHH tumors and nuclear IR for β-catenin only WNT tumors. IRs for filamin A and YAP1 identify SHH and WNT tumors. SHH, WNT, and non-SHH/WNT tumors contributed 31, 14, and 55% to the series. All desmoplastic/nodular (D/N) medulloblastomas were SHH tumors, while most WNT tumors (94%) had a classic phenotype. Monosomy 6 was strongly associated with WNT tumors, while PTCH1 loss occurred almost exclusively among SHH tumors. MYC or MYCN amplification and chromosome 17 imbalance occurred predominantly among non-SHH/WNT tumors. Among patients aged 3–16 years and entered onto the SIOP PNET3 trial, outcome was significantly better for children with WNT tumors, when compared to SHH or non-SHH/WNT tumors, which showed similar survival curves. However, high-risk factors (M+ disease, LC/A pathology, MYC amplification) significantly influenced survival in both SHH and non-SHH/WNT groups. We describe a robust method for detecting SHH, WNT, and non-SHH/WNT molecular subgroups in formalin-fixed medulloblastoma samples. In corroborating other studies that indicate the value of combining clinical, pathological, and molecular variables in therapeutic stratification schemes for medulloblastoma, we also provide the first outcome data based on a clinical trial cohort and novel data on how molecular subgroups are distributed across the range of disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While therapeutic advances have improved survival rates for medulloblastoma over the last three decades, resulting in cures for approximately three quarters of standard-risk childhood patients, this improvement has been achieved at the cost of significant adverse effects among survivors. Additionally, high-risk patients with evidence of metastatic tumor (M+) or significant residual disease present a considerable therapeutic challenge and generally have a poor outcome. Recent data on distinct biological properties among molecular subgroups of disease could provide a more tailored approach to therapeutic stratification, by indicating when a targeted therapeutic would be effective, when it is feasible to reduce adjuvant therapy and thus adverse effects for low-risk disease, or when to use maximal therapy for aggressive high-risk disease [8, 33, 36].
Data generated by gene expression profiling indicate that medulloblastoma comprises distinct molecular subgroups that are likely to have different cellular origins and driving mutations [2, 27, 32, 44]. Molecular subgroups characterized by activation of the Sonic Hedgehog (SHH) and Wingless (WNT) pathways are common to all studies generating these data. Non-SHH/WNT subgroups number between two and four, are less readily separated on principal components analysis, and are not obviously associated with abnormalities of any cell signaling pathway. While less is known about non-SHH/WNT tumors, evidence suggests that at least one subgroup may be driven by amplification and/or overexpression of MYC [2].
Initially, the rare occurrence of medulloblastoma in Gorlin syndrome (nevoid basal cell carcinoma syndrome), which is caused by germline mutations in PTCH1, focused attention on abnormalities of the SHH pathway [11]. This work led to the discovery of PTCH1, SUFU, and SMOH mutations in approximately 25% of sporadic medulloblastomas [35, 38, 49]. Activation of the SHH pathway, which stimulates proliferation of granule cell neurons during cerebellar development, has been used to create mouse models of medulloblastoma [21, 46].
Similarly, the rare occurrence of medulloblastoma among families with Turcot syndrome led investigators to uncover mutations within the WNT pathway, including CTNNB1, APC, and AXINI1/2, in approximately 15% of sporadic medulloblastomas [4, 22, 25, 26, 50]. We have recently reported that WNT pathway medulloblastomas arise outside the cerebellum from cells of the lower rhombic lip, demonstrating for the first time that subtypes of medulloblastoma are likely to be intrinsically distinct diseases [17].
The identification of molecular subgroups is not only important for understanding the origins of medulloblastoma, but has the potential for immediate clinical relevance [18]. WNT tumors clearly have a good clinical outcome with standard therapies, and small molecule inhibitors of the SHH pathway, with the potential to treat this subgroup of patients, have been successfully developed [6, 10, 14, 39]. These findings suggest that detecting WNT and SHH tumors will soon become an important element of the diagnostic process for medulloblastoma patients, guiding therapeutic stratification and the use of targeted therapies [8].
While expression profiling is the ‘gold standard’ for defining molecular subgroups of medulloblastoma, it is not reliable when applied to formalin-fixed paraffin wax-embedded (FFPE) tissue, as used routinely for pathological evaluation. This manuscript reports the development of a novel immunohistochemical method that identifies SHH, WNT and non-SHH/WNT tumors and works well with FFPE tissue in the setting of a diagnostic laboratory. The method, which was first validated on a set of tumors previously subtyped by gene expression profiling, was then applied to 235 medulloblastomas, selected to represent the full range of disease. In addition to providing a valuable tool with which to study cohorts of tumors retrospectively, the assay will allow the routine prospective assignment of medulloblastomas to molecular subgroups as part of the diagnostic process.
Methods
Study tumor cohort
Study materials consisted of FFPE tissues from 235 medulloblastomas, representing primary surgical resections from children treated on the SIOP/UKCCSG CNS9102 (PNET3) and CNS9204 trials and from other infants (aged <3 years) and adults (aged >16 years) treated at Washington University, St. Louis, UCLA, and Emory University, Atlanta [43]. Atypical teratoid/rhabdoid tumors had been excluded from the series on the basis of immunoreactivity for the SMARCB1 gene product (INI1). There was no overlap between this tumor cohort and that used for validating the immunohistochemical method above. Detailed clinical data, including outcome data, were available for children aged 3–16 years (PNET3 trial patients), and basic clinical data, including status (alive/dead) were retrieved for other patients. The cohort’s demographics match those of other previously reported medulloblastoma patient populations (Table 1).
Histology and immunohistochemistry
Standard histological preparations (hematoxylin and eosin) were used to assess general architectural and cytological features, including nodule formation, differentiation along neuronal (neurocytic/ganglionic) and astrocytic lines, and large cell or anaplastic phenotypes.
Reticulin preparations were used to evaluate desmoplasia. Internodular desmoplasia was required for a diagnosis of desmoplastic/nodular (D/N) medulloblastoma, including the paucinodular D/N variant, and medulloblastoma with extensive nodularity (MBEN). The paucinodular D/N medulloblastoma displays scattered small nodules amid widespread desmoplasia [8, 30]. Intranodular cells in this variant uncommonly demonstrate the differentiated neurocytic morphology of the conventional D/N tumor or MBEN, but do express neuronal proteins and show low Ki-67 immunolabeling. The MBEN is defined by its large irregularly shaped nodules, pronounced internodular neurocytic differentiation, and sparse internodular desmoplastic regions [15, 30].
As defined by the WHO classification of CNS tumors and restated in criteria adopted for COG trials in North America, the anaplastic medulloblastoma shows marked cytological pleomorphism across most of its area, in association with high mitotic and apoptotic counts [8, 29]. The large cell medulloblastoma is defined by its groups of uniform large round cells with a single nucleolus, in most cases admixed with groups of anaplastic cells [16]. Large cell and anaplastic tumors were combined in study datasets as LC/A tumors.
Immunohistochemistry was undertaken according to established protocols with antibodies to GFAP (DAKO #M0761; 1:250), synaptophysin (Leica Microsystems #NCL-L-Synap-299; 1:400), NEU-N (Chemicon #MAB377; 1:10,000), p27Kip1 (DAKO #M7203; 1:50), and Ki-67 (DAKO #M7240; 1:200). Molecular subgroups of disease—SHH tumors, WNT tumors, and non-SHH/WNT tumors—were disclosed by immunohistochemistry using a combination of four antibodies (Table 2): β-catenin (BD #610154; 1:800; antigen retrieval, citrate buffer 20 min Bond), GAB1 (Abcam #ab27439; 1:50; antigen retrieval, citrate buffer 20 min Bond), filamin A (Fitzgerald #10R-F113A; 1:100; antigen retrieval, TRIS buffer 30 min Benchmark XT), and YAP1 (Santa Cruz #sc-101199; 1:50; antigen retrieval, citrate buffer 20 min Bond). Positive control tissues for these antibodies were: β-catenin, tissue micro-array containing samples of normal colon and colonic carcinoma; GAB1, tonsil; filamin A, appendix; YAP1, placenta.
Interphase fluorescence in situ hybridization (iFISH)
iFISH was undertaken as previously described on cases for which sufficient material was available [9, 28]. The following BACs were used to assess copy number abnormalities by iFISH: MYCN, RP11-355H10/RP11-348M12 (2q control, RP11-296A19/RP11-384O8); chromosome 6p22, DCDC2, RP11-72O5; chromosome 6q23, SGK1, RP11-692B5; MYC, CTD-3056O22/2267H22 (8p control, RP11-1077A8/RP11-867P15); chromosome 9q22, PTCH1, RP11-150G22 (9p control, RP11-643P16/RP11-45J11); chromosome 17p, HIC1, RP11-357O7/RP11-806J5 (17q control, RP11-368A16/RP11-661H23). Double minute patterns or homogeneously staining regions defined MYC and MYCN amplification, as previously described [28].
Statistical analysis
Progression-free survival (PFS) was defined as the interval between start of therapy and date of progression or death on study. Overall survival (OS) was defined as the interval between start of therapy and date of death on study. Patients not experiencing an event for PFS or OS were censored at the date of last follow-up. Survival distributions were estimated using the Kaplan–Meier method and compared between two or more groups of patients using the log-rank test. Hazard ratios were estimated using Cox proportional hazards models. Associations between any two clinicopathological or molecular variables of interest were tested using Fisher’s exact test or Exact χ 2 test. P values reported in this manuscript were not adjusted for multiplicity.
Results
Development and validation of immunohistochemical assay to define molecular subgroups
Antibodies to β-catenin for identifying WNT tumors and effective on FFPE tissue are well established in the diagnostic laboratory [10, 12]. YAP1 has recently been identified as a marker of SHH and WNT tumors in a study of interactions between the SHH and Hippo pathways in medulloblastoma [13]. GAB1 and filamin A were chosen as potential SHH tumor markers for use alongside β-catenin and YAP1 through an iterative process that started with a list of all overexpressed (P < 0.01 level) genes (n = 528) in SHH tumors from an established dataset of 46 medulloblastomas separated into five molecular subgroups [44]. A second step involved a search for commercial antibodies to protein products of listed genes and yielded a subset (n = 81) of antibodies with claimed effectiveness on FFPE tissue. Antibodies from the subset were then ranked according to reports in the scientific literature of their effectiveness and utility on FFPE tissue and then optimized, in rank order, for use with diagnostic material. Some antibodies were to elements of the SHH pathway, such as GLI proteins, but most were to surrogate markers of the molecular subgroup.
It was not possible to optimize antibodies targeting downstream elements of the SHH pathway for use with FFPE tissue (e.g., anti-GLI1/2), but antibodies to several surrogate markers gave good results. Some of these (e.g., anti-decorin antibody) clearly targeted histological features of desmoplastic/nodular medulloblastomas, which are enriched in the SHH subgroup, but did not stain non-desmoplastic SHH tumors. A final validation step employed FFPE tissue from a subset (n = 26) of the 46 medulloblastomas that contributed primary gene expression data, which were generated using Affymetrix U133Av2 arrays [44]. The anti-GAB1 antibody identified only tumors with a SHH profile or PTCH1 mutation, but the anti-filamin A antibody identified WNT and SHH tumors, but not non-SHH/WNT tumors (Supplementary Table 1).
Pathological variants
Classic medulloblastomas dominated the study cohort (Supplementary Figure 1), contributing 72% of all tumors. Most classic tumors (86%) appeared as sheets of uniform small cells with a high nuclear:cytoplasmic ratio and round hyperchromatic nuclei, while the remainder (14%) had an oval-cell morphology. Focal neuronal differentiation was evident in a minority of classic tumors, manifesting either as nodules of uniform neurocytic cells without surrounding reticulin-positive collagen (non-desmoplastic nodular phenotype; 7%), or as dense clusters of tiny round neurocytes (4%), or as regions of neuropil-like matrix with an irregular border, variable area, and scattered ganglion or neurocytic cells (ganglioneuroblastoma phenotype; n = 1). In all of these tumors, foci of neuronal differentiation demonstrated: (1) moderate to strong immunoreactivities for synaptophysin and NEU-N, (2) up-regulation of p27, and (3) a reduced growth fraction, as assessed by Ki-67 immunolabeling. Small foci of tumor cells showing astrocytic differentiation were present in three tumors. Among childhood medulloblastomas, immunoreactivity for GFAP was generally present in reactive astrocytes, but some GFAP-positive tumor cells were found in adult cases, occurring in classic and D/N (internodular regions), but not LC/A, tumors.
Desmoplastic medulloblastomas (Supplementary Figure 2), which contributed 17% of all tumors, were classified as conventional D/N medulloblastoma (67%), paucinodular D/N medulloblastoma (13%), and MBEN (20%). Intranodular cells in these desmoplastic tumors showed the expected neuronal immunophenotype and low growth fraction described above for nodular non-desmoplastic tumors. Foci of internodular cells in a few D/N tumors showed marked cytological pleomorphism amounting to anaplasia, and this cytology was occasionally associated with invasion by such cells of peripheral areas within nodules.
Anaplastic and large cell tumors contributed 10 and 1% of the cohort, respectively (Supplementary Figure 3). Several non-desmoplastic tumors from infants consisted of a densely packed monomorphic population of round cells with one or more prominent nucleoli and abundant mitotic activity. Their cytological features were distinct from the conventional classic medulloblastoma, bearing some similarities to the large cell phenotype, but without cytomegaly. Tumors with this phenotype made up approximately one sixth of non-desmoplastic tumors from children less than 3 years old and were invariably associated with a fatal outcome.
A single classic tumor in the cohort demonstrated an idiosyncratic morphology characterized by the perivascular accumulation of pleomorphic cells with an anaplastic phenotype (Supplementary Figure 4). Away from blood vessels, tumor cells had round nuclei, a neurocytic morphology, and a much lower nuclear:cytoplasmic ratio than perivascular cells. Ki-67 immunolabeling was higher among perivascular cells than among the neurocytic cells. The tumor did not contain ependymoblastic rosettes.
Medulloblastoma molecular subgroups: immunophenotypes and histopathological associations
SHH pathway medulloblastomas
Combined immunoreactivities for GAB1, filamin A, and YAP1, indicating a SHH profile, were found in 72 (31%) of medulloblastomas, including all desmoplastic tumors (n = 39). Desmoplastic medulloblastomas constituted 54% of SHH-pathway tumors, classic and LC/A tumors contributing 29 and 17% respectively. While non-desmoplastic SHH tumors generally showed widespread and strong immunoreactivities for GAB1, YAP1, and filamin A, all three types of desmoplastic tumor displayed stronger staining for these proteins within internodular regions (Figs. 1, 2, 3, 4). Immunoreacitivities for filamin A and YAP1 in SHH tumors were always strong and generally widespread. This was not always the situation for GAB1 immunoreactivity; no more than weak cytoplasmic staining for GAB1 was seen in a few non-desmoplastic SHH tumors (n = 6). These tumors were all strongly immunopositive for filamin A and YAP1, which acted to confirm the SHH phenotype. The single idiosyncratic classic tumor with perivascular anaplasia showed regional variation for filamin A, YAP, and GAB1 immunoreactivities, which tended to align with the anaplastic phenotype.
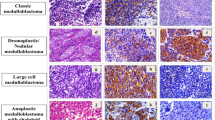
GAB1 immunoreactivity. Internodular regions of this D/N medulloblastoma show strong cytoplasmic staining for GAB1, but negligible reactivity within nodules (a). In contrast, this paucinodular tumor shows GAB1 reactivity in both anatomic compartments (b). Some anaplastic tumors are also GAB1-positive (c). Non-SHH tumors are GAB1-negative (d)
β-Catenin immunoreactivity. Most WNT pathway medulloblastomas show combined cytoplasmic and nuclear immunoreactivity (a), though some genuine WNT tumors show variable nuclear staining (b, c). Medulloblastomas that contain scattered nucleopositive cells amounting to less than 2% of cells are not WNT tumors (d). Lack of cytoplasmic β-catenin immunoreactivity is exceptional in medulloblastomas, but clusters of dense neurocytic cells in classic tumors are notably immunonegative (e). Desmoplastic medulloblastomas characteristically show enhanced cytoplasmic β-catenin immunoreactivity within nodules (f)
Filamin A immunoreactivity. Cytoplasmic immunoreactivity for filamin A is present across this classic medulloblastoma (a). As for GAB1, filamin A staining in desmoplastic SHH tumors tends to be internodular in MBENs (b), but in both nodules and internodular regions in paucinodular tumors (c). Non-SHH/WNT tumors are immunonegative for filamin A, apart from blood vessels and rare reactive astrocytes, which provide an internal control for the method (d)
YAP1 immunoreactivity. Nuclear (predominantly) and cytoplasmic YAP1 immunoreactivity are evident in the SHH anaplastic medulloblastoma (a). This D/N medulloblastoma shows strong YAP1 staining in internodular tumor cells and scattered intranodular cells (b). This MBEN shows only internodular YAP1 immunoreactivity (c). Paucinodular tumors show only weak nodular staining for YAP1 (d). The sole classic WNT medulloblastoma that contained dense foci of neurocytic cells (the rest were non-SHH/WNT) showed no YAP1 reactivity in these foci, but staining in surrounding tumor cells (e). Non-SHH/WNT tumors are YAP1-immunonegative, but the vasculature is immunopositive, providing an internal control for the method (f)
WNT pathway medulloblastomas
Widespread intermediate or strong cytoplasmic β-catenin immunoreactivity was a feature of nearly all medulloblastomas in the series; very few showed only patchy weak cytoplasmic staining for this antigen. However, lack of β-catenin immunoreactivity did characterize the clusters of tiny neurocytic cells that were a focal feature of rare classic tumors. WNT pathway medulloblastomas were identified by nuclear, as well as cytoplasmic, immunoreactivity for β-catenin (Figs. 1, 2, 3, 4). In many cases, nuclear and cytoplasmic β-catenin staining combined to blanket almost all tumor cells, but in some WNT tumors strong nuclear β-catenin immunoreactivity was present in groups of cells alongside those with weak or negligible nuclear staining. WNT pathway medulloblastomas defined by these types of nuclear β-catenin immunoreactivity also expressed filamin A. Typically, this was patchy staining and less intense than that seen in SHH tumors. Strong and widespread nuclear immunoreactivity for YAP1 was also a feature of WNT pathway tumors. This distinctive combination of β-catenin, filamin A, and YAP1 immunoreactivities robustly confirmed the status of medulloblastomas in this molecular subgroup. WNT tumors contributed 32 (14%) of all medulloblastomas in this study. Nearly all WNT pathway medulloblastomas were classic tumors. LC/A tumors (n = 2) were exceptional (6%) among WNT tumors, while desmoplastic medulloblastomas were not represented.
Non-SHH/WNT medulloblastomas
Medulloblastomas (n = 130; 55%) falling outside the SHH and WNT categories displayed cytoplasmic, but not nuclear, immunoreactivity for β-catenin (Figs. 1, 2, 3, 4). Tumor cells were immunonegative for GAB1 and YAP1. In general, tumors in this category were also immunonegative for filamin A, though very weak patchy immunoreactivity for this antigen was evident in rare non-SHH/WNT medulloblastomas (n = 9), which were classified as such on the basis of the panel of immunoreactivities. Intrinsic vascular elements were immunopositive for YAP1 and filamin A, providing an internal control. This subgroup of medulloblastomas was dominated by classic tumors (92%), including all non-desmoplastic nodular tumors and all but one medulloblastoma that contained small clusters of densely packed neurocytic cells, the exception being a WNT tumor. LC/A tumors made up the remainder (n = 11).
Medulloblastoma molecular subgroups: cytogenetic associations
Molecular cytogenetic data were generated on a large proportion of cases using iFISH and probes to loci known to harbor copy number abnormalities (CNAs) in medulloblastoma: chromosome 6 (including SGK1), chromosome 17 (including HIC1), PTCH1, MYC, and MYCN (Supplementary Fig. 5). Monosomy 6 was detected in 27 tumors (13%). All but one of these were classic tumors, and all but two belonged to the WNT subgroup (Table 3). Monosomy 6 was detected in 86% of WNT pathway tumors, which showed few CNAs at other targeted loci (Fig. 5).
Clinical, pathological, and cytogenetic features of tumor cohort by molecular subgroup. Pathological variant: brown LC/A, light yellow D/N, white classic. Age group: brown adult, dark yellow infant, white child. Chromosome 6: light yellow monosomy, white not monosomy. PTCH1 locus: brown 9q22 loss, white no 9q22 loss. Chromosome 17: Dark yellow i(17q), light yellow other chromosomal imbalance, white no chromosomal imbalance. MYCN: brown amplified, white not amplified. MYC: dark yellow amplified, white not amplified. Metastatic disease at presentation: brown yes, white no. Sex: dark yellow female, white male. Green result not available
Deletion at the PTCH1 locus, manifesting as either heterozygous deletion, or monosomy 9, or relative imbalance in the setting of hyperploidy was present in 25 tumors (14%), all but one of which were SHH pathway medulloblastomas. The one exception, which demonstrated imbalance at the PTCH1 locus on a background of hyperploidy, was a classic tumor categorized as non-SHH/WNT. PTCH1 loss was detected in 38% of SHH tumors. Most PTCH1 deletions in the series were present in desmoplastic tumors (60%); LC/A and classic tumors contributed 32 and 8%, respectively. However, the proportion of desmoplastic medulloblastomas with PTCH1 deletions (43%) was not significantly different from that of LC/A tumors with PTCH1 deletions (42%). Among SHH pathway medulloblastomas alone (Table 4), there was a significant difference in the proportions of pathological variants with and without PTCH1 deletion (P = 0.001).
Most examples of MYC amplification were present in classic tumors of the non-SHH/WNT subgroup (Table 3), though the proportion of LC/A tumors with MYC amplification (12.5%) was greater than that (3.8%) for classic tumors. All eight non-SHH/WNT medulloblastomas with MYCN amplification showed a classic morphology, while the four MYCN-amplified SHH tumors divided equally between desmoplastic and LC/A categories. A much higher proportion of medulloblastomas with chromosome 17 CNAs (including balanced copy number change) was evident among non-SHH/WNT tumors versus SHH and WNT tumors; non-SHH/WNT = 83%, SHH = 24%, WNT = 29% (P < 0.0001). Similar findings applied to imbalance of chromosome 17; non-SHH/WNT = 66%, SHH = 16%, WNT = 11% (P < 0.0001).
Medulloblastoma molecular subgroups: clinical associations
The three molecular subgroups of medulloblastoma demonstrated distinct clinical associations (Fig. 5). SHH tumors dominated medulloblastomas from infants and adults, in part reflecting the association between these age groups and desmoplastic tumors (Fig. 6). In contrast, WNT tumors nearly all presented between the ages of 6 and 12 years. Only one child with a WNT pathway medulloblastoma presented before the age of 6 years, with 5 cases after the age of 12 years, including one adult (aged 42 years). The ratio of male:female patients also varied among molecular subgroups; SHH 1.4:1, WNT 1.1:1, non-SHH/WNT 2:1.
Medulloblastoma pathological variants and molecular subgroups: age at diagnosis. The cumulative proportion of five histopathological medulloblastoma variants is plotted against age at diagnosis: blue classic, black MBEN, red LC/A, green D/N, orange non-desmoplastic nodular (a). The frequency (%) of three histopathological variants of medulloblastoma (blue classic, red LC/A, green desmoplastic) is plotted against ten age groups from birth to adulthood (b). The cumulative proportion of three molecular subgroups is plotted against age at diagnosis: blue SHH, green WNT, red non-SHH/WNT (c). The frequency (%) of three molecular subgroups of medulloblastoma (blue SHH, green WNT, red non-SHH/WNT) is plotted against ten age groups from birth to adulthood (d)
Clinical data on metastatic disease and outcome were available for children aged 3–16 years and entered onto the SIOP PNET3 trial. The frequency of metastatic disease at presentation was higher in the non-SHH/WNT subgroup (21%) than in the other two (SHH 11%, WNT 10%). Survival analyses revealed that WNT pathway medulloblastomas had significantly (P = 0.02) better progression-free (and overall) survivals than SHH pathway or non-SHH/WNT tumors (Fig. 7). When patients with SHH or non-SHH/WNT tumors were divided into standard-risk and high-risk categories according to M status, pathological variant, and MYC status (standard-risk = M0 and non-LC/A and MYC non-amplified; high-risk = M+ or LC/A or MYC-amplified), standard-risk and high-risk patients within both molecular subtypes had significantly (P < 0.0001) different outcomes (Fig. 7). No significant difference in outcome was shown for LC/A tumors belonging to the SHH-pathway or non-WNT/SHH subgroups of medulloblastoma, and the trend towards a better outcome for non-LC/A SHH pathway tumors is likely to relate to desmoplastic tumors in this category (Fig. 7).
Outcome analyses among patients aged 3–16 years on the CNS9102/PNET3 trial. Progression-free survival curves split by three histopathological variants of medulloblastoma: green D/N, blue classic, red LC/A (a P = 0.009). PFS curves split by three molecular subgroups of medulloblastoma: green WNT, blue SHH, red non-SHH/WNT (b P = 0.02). PFS curves split into five groups on the basis of molecular subgroup and pathological variant: green WNT, blue SHH classic or D/N, orange non-SHH/WNT classic or D/N, black SHH LC/A, red non-SHH/WNT LC/A (c P = 0.0003). PFS curves split into five groups on the basis of molecular subgroup and clinicopathological risk (standard-risk: tumors without metastasis, LC/A phenotype, or MYC amplification, high-risk: tumors with metastatic disease, LC/A phenotype, or MYC amplification): green WNT, blue SHH standard-risk, orange non-SHH/WNT standard-risk, black SHH high-risk, red non-SHH/WNT high-risk (d P < 0.0001)
Among all patients across the series with medulloblastomas that demonstrated amplification of MYCN (5.5%), outcome differed according to molecular subgroup; 87% (7 of 8) of patients with non-SHH/WNT tumors were alive at the time of data acquisition, which compared to 25% of patients (1 of 4) with SHH tumors. The sole surviving patient with a MYCN-amplified SHH tumor had a D/N medulloblastoma. All patients with MYC-amplified tumors across the series have died of disease.
Discussion
The potential for enhancing the clinical utility of tumor classifications by concurrent evaluation of prognostic or predictive molecular markers remains to be realized for medulloblastoma. However, recent progress in our understanding of medulloblastoma biology has provided real scope for the creation of such schemes [8, 18, 36]. Of particular value would be the identification of WNT tumors, which have a relatively good outcome with standard therapies and may benefit from a reduction in the intensity of adjuvant therapy, and of SHH tumors, which represent potential targets for novel pathway inhibitors. Despite these developments, burgeoning molecular datasets present a challenge to those involved in treating medulloblastoma: how to develop an optimal therapeutic stratification, involving clinical, pathological, and molecular variables, with improved cure rate and reduced long-term adverse effects as end-points. Rising to this challenge involves determining (1) which molecular markers are independent indicators of outcome when tested alongside clinical and pathological variables in trial cohorts of patients and (2) how best to assay selected molecular markers in diagnostic material, which is submitted in the form of FFPE tissue. Our study describes an immunohistochemical method for distinguishing three molecular subgroups of medulloblastomas, which accurately matched SHH, WNT, and non-SHH/WNT subgroups in a validation set of profiled tumors, and provides data on associations between clinical, pathological, and molecular variables.
WNT medulloblastomas are characterized by up-regulation of the canonical WNT signaling pathway, which results in translocation of β-catenin to the nucleus. About two thirds harbor a CTNNB1 mutation. Mutations in other pathway elements, such as APC and AXIN1, have been recorded in the absence of a CTNNB1 mutation, but are much less frequent [4, 9, 12, 22, 25]. A robust immunohistochemical method, suitable for use with FFPE tissue samples, exists for identifying β-catenin nucleopositive WNT pathway medulloblastomas. However, we have demonstrated previously that the WNT tumor immunophenotype is variable [9, 10]. Most WNT tumors demonstrate widespread nuclear immunoreactivity for β-catenin, present in practically all tumor cells, while some examples show patchy staining. The extent of β-catenin nuclear immunoreactivity in these WNT pathway medulloblastomas always amounts to more than a third of the total tumor area and is clearly different from the situation where very few scattered β-catenin nucleopositive cells, representing less than 2% of tumor cells, are evident. Assays for CTNNB1 mutation and monosomy 6, which occurs in nearly all WNT pathway medulloblastomas, have helped to establish the status of tumors in these immunohistochemical categories [3, 9].
In this study, we have extended our earlier clinicopathological and cytogenetic data on WNT pathway medulloblastomas, corroborating data from other researchers. WNT pathway medulloblastomas are almost all classic tumors, and most (81% in this study) present between the ages of 6 and 12 years. Our previous studies have demonstrated a good outcome for WNT tumors with standard adjuvant therapy, and recent data from patients on the CNS9102 trial have been included in the present study [9]. There is a close association between a WNT pathway immunophenotype and CTNNB1 mutation or monosomy 6, predicating a good outcome for medulloblastomas with these genetic abnormalities [3, 9, 27, 32, 34]. Assaying chromosome 6 CNAs could prove to be a useful ancillary test alongside immunohistochemistry for β-catenin, but the latter remains the optimal method for determining WNT pathway status. While monosomy 6 is frequently encountered in WNT pathway medulloblastomas, other cytogenetic abnormalities, such as MYC amplification or copy number changes on chromosome 17, are rare [3, 9, 27, 32, 34]. The idiosyncratic nature of the WNT tumor, as evinced by its restricted range of age at presentation, its pathological and cytogenetic associations, and its relatively good outcome, all align with recent evidence from our group that its histogenesis is distinct from that of other medulloblastomas [17].
While nuclear immunoreactivity for β-catenin is established as a robust marker of WNT pathway activation in diagnostic (FFPE) biopsies, finding a reliable immunohistochemical marker of SHH pathway activation for the clinical laboratory has been more challenging. Antibodies to up-regulated components of the SHH pathway that work well enough in animal models tend to perform erratically on FFPE tissue sections of human tumors, and none is established in diagnostic practice. Faced with such difficulties, we have resorted to surrogate markers of this molecular subgroup of medulloblastomas, utilizing expression profiling data to select antibodies that work well on FFPE tissue and target the protein products of genes overexpressed in SHH pathway medulloblastomas. Validating potential antibodies on medulloblastomas from a series used to generate the expression data, we selected GAB1 as a specific marker of SHH pathway medulloblastomas, and filamin A as a marker of WNT and SHH tumors. In a separate study, YAP1 nuclear immunoreactivity had already been shown to identify WNT and SHH pathway medulloblastomas [13].
GAB1 (GRB2-associated binding protein 1) is a member of the Gab/DOS (Daughter of Sevenless) family of adapter proteins and is involved in multiple cell processes, including morphogenesis, proliferation, and cell adhesion and motility [19, 24, 31]. GAB1 is tyrosine-phosphorylated upon stimulation of receptors by various growth factors, e.g. PDGF, HGF, and by cytokines, e.g. IL-6, IL-3, and interacts with multiple signaling molecules, e.g. SHP-2, PI3K, in several cell systems. Its role in the SHH pathway has yet to be clarified; dysregulation of GAB1 metabolism in other tumors that involve abnormalities of the SHH pathway has not been reported. On the basis of its biology, its specificity in classifying medulloblastomas might appear surprising. However, we have further validated the use of an anti-GAB1 antibody in this setting on over 80 tumors from the SJMB03 cohort, for which expression data are available (Dr. Amar Gajjar, personal communication). Filamin A is a large actin-binding protein involved in cell motility [48]. Nonsense mutations in the gene encoding filamin A (FLNA) cause an X-linked brain malformation, periventricular nodular heterotopia [5]. In neoplasia, filamin A plays a role in both angiogenesis and metastasis [47]. YAP1 is a transcriptional co-activator and can promote proliferation and transformation. It is a downstream target of the Hippo pathway, which upon activation inhibits YAP1 through phosphorylation and cytoplasmic sequestration. Overexpression of YAP1 is a feature of several neoplastic processes, including medulloblastoma, in which it is also amplified in a small proportion of cases [13].
SHH pathway medulloblastomas encompass all desmoplastic tumors, including the conventional D/N medulloblastoma, MBEN, and paucinodular medulloblastoma. All of these variants are characterized by reticulin-positive internodular desmoplasia and are distinct from the less common (7% in the present series) non-desmoplastic medulloblastoma that contains a variable number of nodules with an identical cytology and immunophenotype to those in desmoplastic tumors. Previously, we have demonstrated that desmoplastic medulloblastomas, when compared with non-desmoplastic nodular tumors, present at a younger age and have distinct cytogenetic associations [30]. Data from this study show that all non-desmoplastic nodular tumors fall into the non-SHH/WNT subgroup. Just over half (54%) of SHH pathway medulloblastomas are desmoplastic tumors. Among remaining non-desmoplastic SHH tumors, the LC/A variant is relatively overrepresented; the LC/A:classic ratio among the three subgroups was: SHH = 0.57; WNT = 0.06; non-SHH/WNT = 0.09. Data from this study confirm that desmoplastic variants contribute most medulloblastomas in infancy and adulthood [1, 20]. In addition, nearly all tumors in these age groups belong to the SHH pathway subgroup, LC/A and classic tumors as well as desmoplastic; only 15% of medulloblastomas in infancy and adulthood are non-SHH/WNT tumors or WNT tumors (single adult case).
Our molecular cytogenetic data link loss at 9q22, encompassing the PTCH1 locus, with SHH pathway medulloblastomas and are consistent with previous reports of 9q22 loss or PTCH1 mutations in a proportion of SHH tumors that ranges from one quarter to two thirds [7, 27, 35, 37, 42, 45, 49]. While we did not have sufficient data to complete a survival analysis of molecular subgroups among infants, the high frequency of SHH tumors in this age group (83%) suggests that molecular subgroup testing would not augment or refine the role already identified for pathological variant as the major determinant of outcome among this subset of patients [40, 41].
Data derived from the CNS9102 cohort of children aged 3–16 years show that SHH and non-SHH/WNT tumors do not have significantly different outcomes. However, PFS and OS curves generated for all patients in these two molecular subgroups may hide divergent outcomes influenced by other risk factors, particularly pathology in the case of SHH pathway medulloblastomas, with their relatively high frequency of LC/A tumors. To explore this further, we compared survival curves for children split according to established risk factors in this cohort (M status, pathological variant, and presence or absence of MYC amplification), clearly demonstrating their importance for patients with both SHH and non-SHH/WNT tumors.
Non-SHH/WNT tumors dominated our series of medulloblastomas. Gene expression profiling has split this molecular subgroup into 2–4 further categories [2, 27, 32, 44]. In a recent study by Northcott et al. [32], two non-SHH/WNT molecular subgroups were designated ‘C’ and ‘D’ alongside groups of SHH and WNT tumors. Group ‘C’ patients tended to present at a younger age and to have a worse outcome than group ‘D’ patients. The highest frequency of metastatic disease at presentation was observed in group ‘C’. MYC amplification was also most common in group ‘C’, while isochromosome (isodicentric) 17q was most common in group ‘D’. This study demonstrated a higher male:female ratio in the non-SHH/WNT category, when compared to that in the SHH and WNT subgroups, a result supported by our data. Another concordant result was that most tumors with CNAs on chromosome 17 in our series occurred in the non-SHH/WNT category.
Reflecting an increased understanding of the heterogeneity of medulloblastomas, our data contribute to a developing consensus on the prognostic or predictive utility of molecular markers in the therapeutic stratification of childhood medulloblastoma. In combination with accepted clinical and pathological outcome indicators, molecular markers would be expected to refine stratification of current therapies and to facilitate the use of targeted therapies, such as GDC-0449, a novel SHH pathway inhibitor. GDC-0449 could have particular utility in infant and adult disease, where SHH tumors predominate, although the drug’s adverse effects on bone growth could be a limiting factor for infant disease [23].
WNT tumors have a good outcome with standard therapies and, in the absence of high-risk factors, could be regarded as low-risk disease, amenable to strategies that reduce adjuvant therapy without compromising cure rate (Table 5). High-risk disease can now be defined by clinical (M+ disease), pathological (LC/A variant), and molecular (MYC amplification) factors [8, 9]. However, further refinements to such a scheme might be expected as the biological behaviors of small disease subgroups are increasingly understood. Medulloblastomas with chromosome 17 CNAs or MYCN amplification fall into this category. Various types of chromosome 17 CNA, such as isodicentric 17q or loss of 17p, have been proposed as outcome indicators in medulloblastoma [28, 34]. Data from our recent study of patients from the CNS9102 trial indicate that, once good-outcome WNT tumors (rarely showing chromosome 17 CNAs) have been removed from survival analyses, chromosome 17 CNAs of any type are not significantly associated with outcome [9]. The status of MYCN amplification as an outcome indicator is controversial, but its biological relevance could depend on cellular context; although numbers are small, our data suggest that MYCN-amplified SHH tumors have a poorer outcome than MYCN-amplified non-SHH/WNT tumors.
In summary, our studies provide details on (1) a novel immunohistochemical method based on gene expression profiling for identifying SHH, WNT, and non-SHH/WNT molecular subgroups of medulloblastoma and (2) clinicopathological data relating to these molecular subgroups from a large cohort of patients representing the entire spectrum of disease.
References
Al-Halabi H, Nantel A, Klekner A, Guiot MC, Albrecht S, Hauser P, Garami M, Bognar L, Kavan P, Gerges N, Shirinian M, Roberge D, Muanza T, Jabado N (2010) Preponderance of sonic hedgehog pathway activation characterizes adult medulloblastoma. Acta Neuropathol. doi:10.1007/s00401-010-0780-0 (on line, early release)
Cho YJ, Tsherniak A, Tamayo P, Santagata S, Ligon A, Greulich H, Berhoukim R, Amani V, Goumnerova L, Eberhart CG, Lau CC, Olson JM, Gilbertson RJ, Gajjar A, Delattre O, Kool M, Ligon K, Meyerson M, Mesirov JP, Pomeroy SL (2010) Integrative genomic analysis of medulloblastoma identifies a molecular subgroup that drives poor clinical outcome. J Clin Oncol. doi:10.1200/JCO.2010.28.5148 (on line, early release)
Clifford SC, Lusher ME, Lindsey JC, Langdon JA, Gilbertson RJ, Straughton D, Ellison DW (2006) Wnt/Wingless pathway activation and chromosome 6 loss characterize a distinct molecular sub-group of medulloblastomas associated with a favorable prognosis. Cell Cycle 5:2666–2670
Dahmen RP, Koch A, Denkhaus D, Tonn JC, Sorensen N, Berthold F, Behrens J, Birchmeier W, Wiestler OD, Pietsch T (2001) Deletions of AXIN1, a component of the WNT/wingless pathway, in sporadic medulloblastomas. Cancer Res 61:7039–7043
de Wit MC, Kros JM, Halley DJ, de Coo IF, Verdijk R, Jacobs BC, Mancini GM (2009) Filamin A mutation, a common cause for periventricular heterotopia, aneurysms and cardiac defects. J Neurol Neurosurg Psychiatry 80:426–428
Doggrell SA (2010) The hedgehog pathway inhibitor GDC-0449 shows potential in skin and other cancers. Expert Opin Investig Drugs 19:451–454
Dong J, Gailani MR, Pomeroy SL, Reardon D, Bale AE (2000) Identification of PATCHED mutations in medulloblastomas by direct sequencing. Hum Mutat 16:89–90
Ellison DW (2010) Childhood medulloblastoma: novel approaches to the classification of a heterogeneous disease. Acta Neuropathol 120:305–316
Ellison DW, Kocak M, Dalton J, Megahed H, Lusher ME, Ryan SL, Zhao W, Nicholson SL, Taylor RE, Bailey S, Clifford SC (2010) Definition of disease-risk stratification groups in childhood medulloblastoma using combined clinical, pathologic, and molecular variables. J Clin Oncol. doi:10.1200/JCO.2010.30.2810 (on line, early release)
Ellison DW, Onilude OE, Lindsey JC, Lusher ME, Weston CL, Taylor RE, Pearson AD, Clifford SC (2005) Beta-Catenin status predicts a favorable outcome in childhood medulloblastoma. J Clin Oncol 23:7951–7957
Evans DG, Farndon PA, Burnell LD, Gattamaneni HR, Birch JM (1991) The incidence of Gorlin syndrome in 173 consecutive cases of medulloblastoma. Br J Cancer 64:959–961
Fattet S, Haberler C, Legoix P, Varlet P, Lellouch-Tubiana A, Lair S, Manie E, Raquin MA, Bours D, Carpentier S, Barillot E, Grill J, Doz F, Puget S, Janoueix-Lerosey I, Delattre O (2009) Beta-catenin status in paediatric medulloblastomas: correlation of immunohistochemical expression with mutational status, genetic profiles, and clinical characteristics. J Pathol 218:86–94
Fernandez LA, Northcott PA, Dalton J, Fraga C, Ellison D, Angers S, Taylor MD, Kenney AM (2009) YAP1 is amplified and up-regulated in hedgehog-associated medulloblastomas and mediates sonic hedgehog-driven neural precursor proliferation. Genes Dev 23:2729–2741
Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE, Woo S, Wheeler G, Ahern V, Krasin MJ, Fouladi M, Broniscer A, Krance R, Hale GA, Stewart CF, Dauser R, Sanford RA, Fuller C, Lau C, Boyett JM, Wallace D, Gilbertson RJ (2006) Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol 7:813–820
Giangaspero F, Perilongo G, Fondelli MP, Brisigotti M, Carollo C, Burnelli R, Burger PC, Garre ML (1999) Medulloblastoma with extensive nodularity: a variant with favorable prognosis. J Neurosurg 91:971–977
Giangaspero F, Rigobello L, Badiali M, Loda M, Andreini L, Basso G, Zorzi F, Montaldi A (1992) Large-cell medulloblastomas. A distinct variant with highly aggressive behavior. Am J Surg Pathol 16:687–693
Gibson P, Tong Y, Robinson G, Thompson MC, Currle DS, Eden C, Kranenburg TA, Hogg T, Poppleton H, Martin J, Finkelstein D, Pounds S, Weiss A, Patay Z, Scoggins M, Ogg R, Pei Y, Yang ZJ, Brun S, Lee Y, Zindy F, Lindsey JC, Taketo MM, Boop FA, Sanford RA, Gajjar A, Clifford SC, Roussel MF, McKinnon PJ, Gutmann DH, Ellison DW, Wechsler-Reya R, Gilbertson RJ (2010) Subtypes of medulloblastoma have distinct developmental origins. Nature. doi:10.1038/nature09587 (on line, early release)
Gilbertson RJ, Ellison DW (2008) The origins of medulloblastoma subtypes. Annu Rev Pathol 3:341–365
Gillgrass A, Cardiff RD, Sharan N, Kannan S, Muller WJ (2003) Epidermal growth factor receptor-dependent activation of Gab1 is involved in ErbB-2-mediated mammary tumor progression. Oncogene 22:9151–9155
Giordana MT, Schiffer P, Lanotte M, Girardi P, Chio A (1999) Epidemiology of adult medulloblastoma. Int J Cancer 80:689–692
Goodrich LV, Milenkovic L, Higgins KM, Scott MP (1997) Altered neural cell fates and medulloblastoma in mouse patched mutants. Science 277:1109–1113
Huang H, Mahler-Araujo BM, Sankila A, Chimelli L, Yonekawa Y, Kleihues P, Ohgaki H (2000) APC mutations in sporadic medulloblastomas. Am J Pathol 156:433–437
Kimura H, Ng JM, Curran T (2008) Transient inhibition of the hedgehog pathway in young mice causes permanent defects in bone structure. Cancer Cell 13:249–260
Kiyatkin A, Aksamitiene E, Markevich NI, Borisov NM, Hoek JB, Kholodenko BN (2006) Scaffolding protein Grb2-associated binder 1 sustains epidermal growth factor-induced mitogenic and survival signaling by multiple positive feedback loops. J Biol Chem 281:19925–19938
Koch A, Hrychyk A, Hartmann W, Waha A, Mikeska T, Schuller U, Sorensen N, Berthold F, Goodyer CG, Wiestler OD, Birchmeier W, Behrens J, Pietsch T (2007) Mutations of the Wnt antagonist AXIN2 (Conductin) result in TCF-dependent transcription in medulloblastomas. Int J Cancer 121:284–291
Koch A, Waha A, Tonn JC, Sorensen N, Berthold F, Wolter M, Reifenberger J, Hartmann W, Friedl W, Reifenberger G, Wiestler OD, Pietsch T (2001) Somatic mutations of WNT/wingless signaling pathway components in primitive neuroectodermal tumors. Int J Cancer 93:445–449
Kool M, Koster J, Bunt J, Hasselt NE, Lakeman A, van Sluis P, Troost D, Meeteren NS, Caron HN, Cloos J, Mrsic A, Ylstra B, Grajkowska W, Hartmann W, Pietsch T, Ellison D, Clifford SC, Versteeg R (2008) Integrated genomics identifies five medulloblastoma subtypes with distinct genetic profiles, pathway signatures and clinicopathological features. PLoS One 3:e3088
Lamont JM, McManamy CS, Pearson AD, Clifford SC, Ellison DW (2004) Combined histopathological and molecular cytogenetic stratification of medulloblastoma patients. Clin Cancer Res 10:5482–5493
Louis DN (2007) WHO classification of tumours of the central nervous system. International Agency for Research on Cancer
McManamy CS, Pears J, Weston CL, Hanzely Z, Ironside JW, Taylor RE, Grundy RG, Clifford SC, Ellison DW (2007) Nodule formation and desmoplasia in medulloblastomas—defining the nodular/desmoplastic variant and its biological behavior. Brain Pathol 17:151–164
Nishida K, Yoshida Y, Itoh M, Fukada T, Ohtani T, Shirogane T, Atsumi T, Takahashi-Tezuka M, Ishihara K, Hibi M, Hirano T (1999) Gab-family adapter proteins act downstream of cytokine and growth factor receptors and T- and B-cell antigen receptors. Blood 93:1809–1816
Northcott PA, Korshunov A, Witt H, Hielscher T, Eberhart CG, Mack S, Bouffet E, Clifford SC, Hawkins CE, French P, Rutka JT, Pfister S, Taylor MD (2010) Medulloblastoma comprises four distinct molecular variants. J Clin. doi:10.1200/JCO.2009.27.4324 (on line, early release)
Packer RJ (2010) Risk stratification of medulloblastoma: a paradigm for future childhood brain tumor management strategies. Curr Neurol Neurosci Rep. doi:10.1007/s11910-010-0168-5 (on line, early release)
Pfister S, Remke M, Benner A, Mendrzyk F, Toedt G, Felsberg J, Wittmann A, Devens F, Gerber NU, Joos S, Kulozik A, Reifenberger G, Rutkowski S, Wiestler OD, Radlwimmer B, Scheurlen W, Lichter P, Korshunov A (2009) Outcome prediction in pediatric medulloblastoma based on DNA copy-number aberrations of chromosomes 6q and 17q and the MYC and MYCN loci. J Clin Oncol 27:1627–1636
Pietsch T, Waha A, Koch A, Kraus J, Albrecht S, Tonn J, Sorensen N, Berthold F, Henk B, Schmandt N, Wolf HK, von Deimling A, Wainwright B, Chenevix-Trench G, Wiestler OD, Wicking C (1997) Medulloblastomas of the desmoplastic variant carry mutations of the human homologue of Drosophila patched. Cancer Res 57:2085–2088
Pizer BL, Clifford SC (2009) The potential impact of tumour biology on improved clinical practice for medulloblastoma: progress towards biologically driven clinical trials. Br J Neurosurg 23:364–375
Raffel C, Jenkins RB, Frederick L, Hebrink D, Alderete B, Fults DW, James CD (1997) Sporadic medulloblastomas contain PTCH mutations. Cancer Res 57:842–845
Reifenberger J, Wolter M, Weber RG, Megahed M, Ruzicka T, Lichter P, Reifenberger G (1998) Missense mutations in SMOH in sporadic basal cell carcinomas of the skin and primitive neuroectodermal tumors of the central nervous system. Cancer Res 58:1798–1803
Rudin CM, Hann CL, Laterra J, Yauch RL, Callahan CA, Fu L, Holcomb T, Stinson J, Gould SE, Coleman B, LoRusso PM, Von Hoff DD, de Sauvage FJ, Low JA (2009) Treatment of medulloblastoma with hedgehog pathway inhibitor GDC-0449. N Engl J Med 361:1173–1178
Rutkowski S, Bode U, Deinlein F, Ottensmeier H, Warmuth-Metz M, Soerensen N, Graf N, Emser A, Pietsch T, Wolff JE, Kortmann RD, Kuehl J (2005) Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. N Engl J Med 352:978–986
Rutkowski S, von Hoff K, Emser A, Zwiener I, Pietsch T, Figarella-Branger D, Giangaspero F, Ellison DW, Garre ML, Biassoni V, Grundy RG, Finlay JL, Dhall G, Raquin MA, Grill J (2010) Survival and prognostic factors of early childhood medulloblastoma: an international meta-analysis. J Clin Oncol 28:4961–4968
Taylor MD, Liu L, Raffel C, Hui CC, Mainprize TG, Zhang X, Agatep R, Chiappa S, Gao L, Lowrance A, Hao A, Goldstein AM, Stavrou T, Scherer SW, Dura WT, Wainwright B, Squire JA, Rutka JT, Hogg D (2002) Mutations in SUFU predispose to medulloblastoma. Nat Genet 31:306–310
Taylor RE, Bailey CC, Robinson K, Weston CL, Ellison D, Ironside J, Lucraft H, Gilbertson R, Tait DM, Walker DA, Pizer BL, Imeson J, Lashford LS (2003) Results of a randomized study of preradiation chemotherapy versus radiotherapy alone for nonmetastatic medulloblastoma: The International Society of Paediatric Oncology/United Kingdom Children’s Cancer Study Group PNET-3 Study. J Clin Oncol 21:1581–1591
Thompson MC, Fuller C, Hogg TL, Dalton J, Finkelstein D, Lau CC, Chintagumpala M, Adesina A, Ashley DM, Kellie SJ, Taylor MD, Curran T, Gajjar A, Gilbertson RJ (2006) Genomics identifies medulloblastoma subgroups that are enriched for specific genetic alterations. J Clin Oncol 24:1924–1931
Vorechovsky I, Tingby O, Hartman M, Stromberg B, Nister M, Collins VP, Toftgard R (1997) Somatic mutations in the human homologue of Drosophila patched in primitive neuroectodermal tumours. Oncogene 15:361–366
Wetmore C, Eberhart DE, Curran T (2001) Loss of p53 but not ARF accelerates medulloblastoma in mice heterozygous for patched. Cancer Res 61:513–516
Zhong Z, Yeow WS, Zou C, Wassell R, Wang C, Pestell RG, Quong JN, Quong AA (2010) Cyclin D1/cyclin-dependent kinase 4 interacts with filamin A and affects the migration and invasion potential of breast cancer cells. Cancer Res 70:2105–2114
Zhou AX, Hartwig JH, Akyurek LM (2010) Filamins in cell signaling, transcription and organ development. Trends Cell Biol 20:113–123
Zurawel RH, Allen C, Chiappa S, Cato W, Biegel J, Cogen P, de Sauvage F, Raffel C (2000) Analysis of PTCH/SMO/SHH pathway genes in medulloblastoma. Genes Chromosomes Cancer 27:44–51
Zurawel RH, Chiappa SA, Allen C, Raffel C (1998) Sporadic medulloblastomas contain oncogenic beta-catenin mutations. Cancer Res 58:896–899
Acknowledgments
The authors gratefully acknowledge support from the American Lebanese Syrian Associated Charities. This study was conducted with appropriate ethics committee approval: St. Jude Children’s Research Hospital XPD07-107/IRB and Newcastle/North Tyneside REC 07/Q0905/71.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
401_2011_800_MOESM1_ESM.docx
Supplementary Figure 1: Classic medulloblastoma. Most tumors demonstrate sheets of small densely packed round cells with a high nuclear:cytoplasmic ratio (a), although 14% of classic medulloblastomas in this series contained elongated cells arranged in a vague fascicular pattern (b). A small proportion (7%) of classic tumors showed nodules of differentiated neurocytic cells (c), without surrounding desmoplasia (d; reticulin stain). Other manifestations of focal neuronal differentiation included dense aggregates of tiny neurocytes (e) or irregular regions of neurocytes and ganglion cells against a neuropil-like matrix (f). Non-desmoplastic nodular regions (g) and dense neurocytic clusters (h) express neuronal proteins, such as synaptophysin (illustrated). All foci of neuronal differentiation had a low growth fraction, as estimated by Ki-67 immunolabeling in illustrated for this neurocytic cluster (i). Foci of astrocytic differentiation are exceptional (j). (DOCX 4811 kb)
401_2011_800_MOESM2_ESM.docx
Supplementary Figure 2: Desmoplastic medulloblastoma. The archetypal desmoplastic/nodular medulloblastoma contains scattered nodules of neurocytes against a neuropil-like matrix (a). Nodules are separated by reticulin-rich desmoplastic regions (b; reticulin stain). The MBEN is characterized by large irregular nodules that dominate the tumor’s architecture (c). In the MBEN, strikingly monomorphic neurocytes may form ribbons in elongated nodules and are often separated from a nodule’s periphery by an anuclear zone (d). Strong expression of NEU-N characterizes intranodular neurocytes (e), while there is a marked disparity in growth fraction between nodular and internodular regions (f; Ki-67 immunoreactivity). Paucinodular medulloblastomas show widespread desmoplasia, among which small nodules can be detected (g). The nodules do not have the low cell density of the MBEN, and a neurocytic morphology is subtle, but expression of neuronal proteins can be demonstrated (h; NEU-N immunoreactivity). Intranodular anaplasia may be a feature of some D/N medulloblastomas (i), as may invasion of nodules by embryonal cells (j). (DOCX 3133 kb)
401_2011_800_MOESM3_ESM.docx
Supplementary Figure 3: Large cell/anaplastic medulloblastoma. Anaplastic medulloblastomas show marked cytological pleomorphism, with molding of polyhedral nuclei against one another, cell wrapping, and high mitotic and apoptotic counts (a, b, c). Despite no obvious morphological differentiation, anaplastic tumors usually express neuronal markers, including neurofilament proteins, which are rarely expressed in classic tumors (d; NFP immunoreactivity). The large cell phenotype is different from anaplastic morphology and demonstrates groups of uniform large cells with prominent nucleoli (e). A few tumors from infants demonstrated sheets of uniform round cells with one or two prominent nucleoli (f). (DOCX 2130 kb)
401_2011_800_MOESM4_ESM.docx
Supplementary Figure 4: Idiosyncratic perivascular niche phenotype. A perivascular arrangement of anaplastic embryonal cells gives way to a more differentiated phenotype, with neurocytic cells against a neuropil-like matrix, away from blood vessels (a, b). (DOCX 748 kb)
401_2011_800_MOESM5_ESM.doc
Supplementary Figure 5: Interphase FISH. Monosomy 6 (a). PTCH1 (green signal) loss (b). Isodicentric 17q (c). MYC amplification (d). (DOC 211 kb)
Rights and permissions
About this article
Cite this article
Ellison, D.W., Dalton, J., Kocak, M. et al. Medulloblastoma: clinicopathological correlates of SHH, WNT, and non-SHH/WNT molecular subgroups. Acta Neuropathol 121, 381–396 (2011). https://doi.org/10.1007/s00401-011-0800-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-011-0800-8