Abstract
Tau is the pathological protein in several neurodegenerative disorders classified as frontotemporal lobar degeneration (FTLD), including corticobasal degeneration (CBD) and progressive supranuclear palsy (PSP). We report an unusual tauopathy in three Japanese patients presenting with Parkinsonism and motor neuron disease (neuroimaging revealed frontotemporal cerebral atrophy in two patients who were examined). At autopsy, all cases showed FTLD with the most severe neuronal loss and gliosis evident in the premotor and precentral gyri. Although less severe, such changes were also observed in other brain regions, including the basal ganglia and substantia nigra. In the spinal cord, loss of anterior horn cells and degeneration of the corticospinal tract were evident. In addition, the affected regions exhibited neuronal cytoplasmic inclusions resembling neurofibrillary tangles. Immunostaining using antibodies against hyperphosphorylated tau and 4-repeat tau revealed widespread occurrence of neuronal and glial cytoplasmic inclusions in the central nervous system; the astrocytic tau lesions were unique, and different in morphology from astrocytic plaques in CBD, or tufted astrocytes in PSP. However, immunoblotting of frozen brain samples available in two cases revealed predominantly 4R tau, with the approximately 37-kDa and 33-kDa low-molecular mass tau fragments characteristic of CBD and PSP, respectively. No mutations were found in the tau gene in either of the two cases. Based on these clinicopathological, biochemical, and genetic findings, we consider that the present three patients form a distinct 4R tauopathy associated with sporadic FTLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abnormalities of the microtubule-associated protein tau (MAPT) are associated with several neurodegenerative disorders classified as frontotemporal lobar degeneration (FTLD), including Pick’s disease (PiD), corticobasal degeneration (CBD), progressive supranuclear palsy (PSP), and FTLD with MAPT mutation [7, 23, 24]. FTLD is an umbrella term that groups several different neurodegenerative diseases in which the neurodegeneration is predominant in the frontal and temporal lobes, and affected patients often present with a type of dementia (frontotemporal dementia: FTD) clinically different from Alzheimer’s disease (AD) [7, 23, 24].
Biochemically, there are six isoforms of tau; three isoforms contain three microtubule-binding repeats (3R tau) and three other isoforms contain four such repeats (4R tau); PiD is associated predominantly with insoluble 3R tau (rarely, the disease may be associated only with insoluble 4R tau [43]), and CBD and PSP with insoluble 4R tau [1, 6, 35]. In FTLD with MAPT mutation, cases with different mutations do not have a consistent pattern of pathology or biochemistry [6, 14, 35, 40]. At present, the accumulation of pathological 3R and 4R tau can also be detected by immunohistochemistry using specific antibodies against 3R and 4R tau, respectively. For example, neurofibrillary tangles in AD are 3R tau-positive and 4R tau-positive; Pick bodies in PiD are 3R tau-positive and 4R tau-negative, and tufted astrocytes in PSP are 3R tau-negative and 4R tau-positive [8].
From a clinical viewpoint, it is noteworthy that apart from the presence or absence of FTD, Parkinsonism is the cardinal feature of both CBD [4, 22] and PSP [21], as well as in some cases of FTLD with MAPT mutation [6, 14, 35, 40]. However, features resembling those seen in motor neuron disease (MND) or amyotrophic lateral sclerosis (ALS) are unusual in FTLD associated with abnormalities of tau, including CBD, PSP, and FTLD with MAPT mutation.
In 2005, we reported a sporadic tauopathy in a Japanese patient presenting with frontotemporal degeneration, Parkinsonism, and motor neuron disease, in whom neurodegeneration with widespread neuronal and glial 4R tau lesions was observed in the central nervous system (CNS), including the upper- and lower-motor neuron systems (case 2 in this study) [30]. At that time, we had noted that before the tau era, Kuroda et al. [20] had already reported very similar neuropathological findings revealed by silver impregnation (Bodian stain) and electron microscopy in another Japanese patient (case 3 in this study).
Recently, we encountered a new Japanese patient (case 1 in this study), in whom the entire clinicopathological picture was very similar to that seen in the other two patients [20, 30]. The aim of this study was to establish the clinical syndromes observed in these three patients, including the patient reported by Kuroda et al [20], as a distinct disease entity involving 4R tauopathy that belongs to the category of sporadic FTLD.
Materials and methods
Patients
None of the affected patients had a family history of dementia or other neurological disease.
Case 1
A 58-year-old Japanese man developed stiffness in the right leg and this symptom progressed gradually, and when fatigued with work, he also developed tremor in the bilateral arms and right leg. After 4 months, he visited a hospital. On examination, he showed spasticity in the right arm, and mild muscle weakness, with positive Babinski sign, in the right leg. Increased deep tendon reflexes were also present in the upper and lower extremities. About 6 months after onset, he was admitted to our hospital for neurological evaluation. There was no evidence of dementia: the patient’s score on the revised version of the Hasegawa dementia scale (HDS-R; a mental examination method commonly used in Japan that utilizes a scale of 0 to 30, where <21 represents dementia) was 28. He showed mild muscle weakness in the bilateral upper and lower extremities, and instability in the Mann test. When walking, spasticity was evident in the right leg, and tandem gait was impossible. EMG showed neurogenic changes in the tongue. Brain and spinal cord MRI revealed no apparent abnormalities. A tentative clinical diagnosis of MND was made.
At the age of 60, he became unable to walk, and for daily life he was confined to a wheelchair. EMG further revealed neurogenic changes in the sternocleidomastoid, femoral rectus, and anterior tibial muscles. At the age of 61, dysphagia appeared and progressed, necessitating the introduction of tube feeding. He developed symptoms of cognitive decline, including spatial and temporal disorientation, poor memory recall, and dyscalculia, with a HDS-R score of 13. No symptoms indicative of FTD, such as personality change, inappropriate behavior, and impaired executive dysfunction were noted. Atrophy and fasciculation were evident in the tongue, and rigospasticity was present in the neck, with retrocollis, and in the upper and lower extremities. Vertical (both upper and lower) eye movement was mildly limited. 123I-IMP single-photon emission computed tomography (IMP-SPECT) demonstrated widespread hypoperfusion in the cerebrum except for the occipital lobe, being most severe in the left motor cortex. He was treated with L-dopa without noticeable effect. At this point, an alternative clinical diagnosis of PSP was considered. At the age of 62, he exhibited severe dementia with a HDS-R score of 4, and brain MRI revealed frontotemporal cerebral atrophy (Fig. 1). The patient died of pneumonia (pathologically, aspiration pneumonia of both lungs), about 4 years after onset of the disease. A general autopsy was performed about 2 h after death, at which time the brain weighed 1,090 g (brainstem and cerebellum, 140 g).
Fluid-attenuated inversion recovery (FLAIR) images obtained from case 1 about 4 months before death. Asymmetric atrophy (left > right) of the frontal and temporal lobes (frontal > temporal) is evident, with dilatation of the lateral ventricle and enlargement of the sylvian fissure. Dilatation of the third ventricle is also evident. The midbrain tegmentum also appears atrophic. Arrows indicate the bilateral precentral gyri
Cases 2 and 3
The clinicopathology of these two cases has been reported previously (case 2 in 2005 [30] and case 3 in 1979 [20]). In both cases, asymmetrical extrapyramidal (Parkinsonism) and pyramidal signs were the presenting manifestations in the early stage. At autopsy, the brains weighed 1,290 g (brainstem and cerebellum, 170 g) and 1,310 g in cases 1 and 2, respectively.
The clinical presentations in the three studied patients are summarized in Table 1.
Neuropathological examination
In all cases, multiple formalin-fixed, paraffin-embedded tissue blocks were available for the present study. In addition, in case 2, multiple histological and immunohistochemical specimens from various regions of the brain and spinal cord, as well as light micrographs of double-labeling immunofluorescence for glial fibrillary acidic protein (GFAP) and tau, and tau immunoelectron micrographs showing neuronal and glial cytoplasmic inclusions in the precentral cortex and spinal anterior horn were available [30]. For the present study, additional immunohistochemical examinations for p62, TDP-43, and FUS were performed on newly prepared sections, as described below. In case 3, conventional electron micrographs showing neuronal cytoplasmic inclusions in the precentral cortex and spinal anterior horn were available [20]. A variety of histological and immunohistochemical examinations were performed on newly prepared sections, as described below. Moreover, we reviewed Gallyas–Braak stained and tau (AT8)-immunostained sections from cases of typical CBD and PSP (two each).
In cases 1 and 3, histological examinations were performed on 4-μm thick sections using two stains: hematoxylin–eosin and Klüver-Barrera. Bodian, Gallyas–Braak, and Holzer stains were also applied to selected sections. All the prepared sections were immunostained by the avidin–biotin-peroxidase complex (ABC) method using a Vectastain ABC kit (Vector, Burlingame, CA, USA) with a mouse monoclonal antibody against hyperphosphorylated tau (AT8; Innogenetics, Ghent, Belgium; 1:200). Diaminobenzidine was used as the chromogen. The immunostained sections were counterstained with hematoxylin. Selected sections were also immunostained similarly using rabbit polyclonal antibodies against GFAP (Dako, Glostrup, Denmark; 1:2,000) and ubiquitin (Dako; 1:800), and mouse monoclonal antibodies against 3R and 4R tau (RD3 and RD4; Upstate, Charlottesville, VA, USA; 1:5,000 and 1:100, respectively), p62 (BD Bioscience, San Jose, CA, USA; 1:200), and CD68 (Dako; 1:400). A double-labeling immunofluorescence study was also performed on sections obtained from the precentral gyrus with rabbit polyclonal GFAP (1:2,000) and mouse monoclonal AT8 (1:100). The second antibodies used were Alexa Fluor 568 goat anti-rabbit IgG (Molecular Probes, Eugene, OR, USA; 1:1,000) and Alexa Fluor 488 goat anti-mouse IgG (Molecular Probes; 1:1,000).
Moreover, selected sections were immunostained with mouse monoclonal antibodies against β-amyloid (Dako; 1:100), phosphorylated α-synuclein (no. 64; Wako, Osaka, Japan; 1:10,000), and phosphoserines 409 and 410 of TDP-43 (pS409/410; Cosmo Bio Co., Ltd., Tokyo, Japan; 1:5,000), and a rabbit polyclonal antibody against FUS (Novus, Littleton, CO, USA; 1:200).
In case 1, conventional electron microscopic examination was also carried out. Formalin-fixed small tissue blocks of the precentral cortex and spinal anterior horn were postfixed with 1% osmium tetroxide, dehydrated through a graded ethanol series, and embedded in Epon 812. Ultrathin sections were cut and stained with uranyl acetate and lead citrate, and examined with a Hitachi H-7100 electron microscope at 75 kV.
Biochemical analysis of tau
Biochemical analysis of tau was performed using postmortem frozen tissues from the frontal and precentral (motor) cortices of case 1 and the frontal cortex of case 2, as well as from the frontal cortex of typical PiD, PSP, and CBD cases (one each). The samples were fractioned by resolubilization in buffers containing different detergents (Tris–buffer saline, 1% Triton X-100, 1% sarkosyl, and 5 M guanidine). The sarkosyl-insoluble, guanidine-soluble fraction was dialyzed against 50 mM Tris–HCl (pH7.4). Dephosphorylation of tau was performed with λ protein phosphatase. Equal amounts of protein (approximately 15 μg in each lane) before and after dephosphorylation and a mixture of recombinant human tau containing the six isoforms were run on sodium dodecyl sulfate-polyacrylamide gel, and transferred to a polyvinylidene difluoride membrane. Full-length and cleaved fragments of tau were visualized using a phosphorylation-independent anti-tau antibody, T46 (Zymed, South San Francisco, CA, USA; 1:10,000), which recognizes the C-terminal regions (amino acid residues 404-441) of human tau.
Sequencing of the tau gene
Genomic DNAs were prepared from frozen samples of cerebellar cortex from cases 1 and 2, using a QIAamp DNA Maxi Kit (Qiagen, Hilden, Germany). The concentration of these DNAs was measured fluorometrically using a PicoGreen® dsDNA quantification kit (Invitrogen, Carlsbad, CA, USA). Exons, predominantly expressed in the human central nervous system, with the flanking intronic sequences of the tau gene (exons 1, 2, 3, 4, 5, 7, 9, 10, 11, 12, and 13), were sequenced with a BigDye® Terminator v3.1 cycle sequencing kit (Applied Biosystems, Foster City, CA, USA) and an ABI PRISM® 3100 Genetic Analyzer (Applied Biosystems), as described previously [33]. Sequence information for all the PCR primers used in this study is available on request.
Results
Neuropathology
Atrophy of the frontal lobe was a feature in all cases (Fig. 2a); although apparently milder in degree, atrophy was also noted in the anteromedial part of the temporal lobe in cases 1 and 2. In all cases, the cerebellum and spinal cord, with the anterior and posterior nerve roots, were unremarkable. In sections, atrophy was also evident in the midbrain and pontine tegmentum; pigmentation of the substantia nigra and locus ceruleus appeared to be relatively preserved (Fig. 2b).
The findings of microscopy described below were observed in all cases (the description was made using figures selected only from those obtained in cases 1 and 3, because case 2 had already been well described with many figures in our previous communication [30]). Neuronal loss and gliosis of various degrees were observed in many brain regions, including the precentral cortex (Fig. 3a, left panel; b, left panel; c, upper panel), basal ganglia (Fig. 3d, left panel), amygdala (Fig. 3e, left panel), and substantia nigra (Fig. 3f, left panel). In the spinal cord, the picture obtained from Klüver–Barrera stained sections was distinctive, being very similar to that seen in ALS (Fig. 4a); the most severe degeneration with macrophage infiltration was evident in the corticospinal tracts (Fig. 4b). Neuronal loss and gliosis were also evident in the gray matter, including the anterior horns (Fig. 4c). In cases 1 and 2, the presence of mild neurogenic muscular atrophy was confirmed in the iliopsoas muscle.
a, b, c The precentral cortex, showing marked neuronal loss and gliosis, with microvacuolation in layer II (a, b: left). Numerous tau-positive neuronal and glial lesions are evident in the precentral cortex (a, b: right). Higher magnification of the precentral cortex layer V, showing two remaining Betz cells with somewhat basophilic cytoplasmic inclusions, as well as scattered astrocytes with prominent eosinophilic processes (c, upper). Tau-positive cytoplasmic inclusions are evident in a Betz cell; in addition, many tau-positive astrocytic lesions are present (c, lower). d, e, f Neuronal loss and gliosis (left), as well as tau-positive neuronal and glial lesions (right) are evident in the putamen (d), amygdaloid nucleus (e), and substantia nigra (f). g Double-labeling immunofluorescence of GFAP (red) and tau (green) in the precentral gyrus indicates that their co-localization (yellow) is rare in the affected astrocytes. h Many tau-positive oligodendrocytes resembling coiled bodies as well as so-called threads are evident in the subcortical white matter of the precentral gyrus. a, c, e case 1; b, d, f–h case 3. a (left), b (left), c (upper), d-f (left) hematoxylin-eosin; a (right), b (right), e, f (right), h (right) AT8 immunostaining; g double-labeling immunofluorescence with GFAP and AT8; c (lower), d (right) RD4 immunostaining. Barsa, b 200 μm; c, d, e, h 50 μm; f, g 100 μm
a The spinal cord at the cervical level, showing myelin pallor in the antero-lateral columns, especially the lateral corticospinal tracts. The dorsal columns appear intact. b Infiltration of numerous macrophages is evident, being more accentuated in the lateral corticospinal tract. c The anterior horn at the lumbar level, showing mild-to-moderate loss of the lower-motor neurons. d High power view of the area indicated by the asterisk in c, showing cytoplasmic inclusions in a remaining lower-motor neuron (arrow). e Tau-positive cytoplasmic inclusions are evident in a sensory neuron in the lumbar dorsal root ganglion. f The anterior horn at the lumbar level, showing tau-positive cytoplasmic inclusions in the lower-motor neurons. a–e case 1; f case 3. a Klüver–Barrera; b CD68 immunostaining; c, d hematoxylin–eosin; e AT8 immunostaining; f RD4 immunostaining. Barsa 2 mm; b 0.5 mm; c 100 μm; d–f 50 μm
In addition, slightly basophilic, filamentous (neurofibrillary tangle-like) inclusions were found in the cytoplasm of the remaining neurons in the affected regions, including the precentral cortex (Fig. 3c, upper panel) and spinal anterior horn (Fig. 4d). AT8 immunostaining revealed neuronal and glial tau lesions in many regions of the CNS (Fig. 3a, right panel; b, right panel; e, right panel; f, right panel). AT8-positive cytoplasmic inclusions were also encountered in a few sensory neurons in the dorsal root ganglia in all cases (Fig. 4e). In the affected gray matter, predominant occurrence of morphologically unique astrocytic tau lesions was a characteristic feature (Fig. 3c, lower panel). Double-labeling immunofluorescence indicated that co-localization of tau and GFAP was rare (Fig. 3g); in this connection, the separate presence of bundles of intermediate filaments (glial filaments) and aggregates of AT8-positive abnormal tubular structures was demonstrated ultrastructurally in astrocytes in case 2 reported previously [30]. On the other hand, in the white matter, including the subcortical white matter of the precentral cortex, oligodendrocytic tau lesions (coiled body-like lesions and threads) were a notable feature (Fig. 3h). The distribution and severity of neuronal loss and AT8-positive tau lesions in the CNS are shown in Table 2 (the data sheet used was based on that introduced by Dickson et al. [10]).
Immunohistochemically, accumulated tau in these neurons and glial cells was purely 4R tau (Fig. 3c, lower panel; d, right panel; 4f) with p62 decoration (Fig. 5a). Ubiquitin immunoreactivity was often evident in the astrocytic lesions. However, it was very weak or absent in the neuronal and oligodendrocytic lesions (Fig. 5b). Of interest was that the overall neuronal and glial tau lesions were well recognized by Bodian staining (Fig. 5c), but were hardly or only faintly visible by Gallyas–Braak staining (Fig. 5d). With regard to the astrocytic lesions in particular, the pictures obtained from AT8-immunostained and Gallyas–Braak stained sections were distinct from those of astrocytic plaques in CBD, or tufted astrocytes in PSP (Fig. 6a–c).
a, b Both neuronal and astrocytic cytoplasmic inclusions are shown to be clearly positive for p62 (a). However, such neuronal cytoplasmic inclusions are not evident by ubiquitin immunostaining (b). c, d A section stained with Bodian’s method shows argyrophilic inclusions both in astrocytes (arrows) and a Betz cell (c). However, such inclusions are hardly recognizable in a section stained with the Gallyas–Braak method (d). a–d case 1, precentral cortex. Barsa–d 50 μm
a–c Astrocytic tau pathology in the precentral cortex. In the present three cases, accumulation of tau (AOT) occurs mainly in the perikarya and the proximal portion of the processes (a, upper), and argyrophilic structures corresponding to the tau lesions are not evident (a, lower). In CBD, AOT appears to occur mainly in the distal portion of the processes, showing an annular array of short stubby or nodular tau positivity (astrocytic plaque; b, upper). In PSP, AOT appears to occur throughout almost the entire length of the processes, showing a radiating curvilinear pattern of tau positivity (tufted astrocyte; c, upper). Both of these tau-positive lesions show evident argyrophilia (b, c: lower). a case 1, b CBD, c PSP; a–c (upper) AT8 immunostaining; a–c (lower) Gallyas–Braak staining. Bar 20 μm for a–c
In all cases, no histological or immunohistochemical features suggestive of complications arising from AD, Parkinson’s disease (or dementia with Lewy bodies), or ALS were evident. No senile plaques, Lewy bodies, or Bunina bodies were found, and no β-amyloid, α-synuclein, TDP-43, or FUS pathology was observed.
Conventional electron microscopy carried out in case 1 revealed cytoplasmic aggregates of abnormal tubular structures both in neurons and in glial cells in the precentral cortex and spinal anterior horn (Fig. 7a–d); the ultrastructural profiles were indistinguishable from those observed in cases 2 [30] and 3 [20].
Case 1. a–d Electron micrographs, showing cytoplasmic aggregates of abnormal tubular structures, about ~20 nm in diameter, in an astrocyte (a), a small pyramidal neuron (b), and an oligodendrocyte (c) in the precentral cortex, as well as in a lower-motor neuron (d) in the spinal anterior horn. Interestingly, the occurrence of tubular structures showing wavy bundle formation was a feature of the precentral cortex pyramidal neurons in all cases [20, 30]. Bars a–d 200 nm
Sarkosyl-insoluble tau
Representative results of immunoblot analysis of sarkosyl-insoluble fractions are shown in Fig. 8. The findings were essentially the same in cases 1 and 2. Immunoblot analysis using dephosphorylated samples revealed two major bands that aligned with the recombinant 4R tau isoforms of 412 (4R, 1N) and 383 (4R, 0N) amino acids in both cases (Fig. 8a). Immunoblot analysis using non-dephosphorylated samples revealed cleaved low-molecular mass tau fragments of approximately 33 kDa in a PSP case, and of approximately 37 kDa in a CBD case (Fig. 8b, upper panel), as reported previously [2]. In cases 1 and 2, it is noteworthy that both the 37-kDa and 33-kDa tau fragments were also visualized after long exposure (Fig. 8b, lower panel).
a Immunoblot analysis of the sarkosyl-insoluble fraction after dephosphorylation from the frontal cortex (FC, lane 4) and precentral (motor) cortex (MC, lane 5) of case 1 and the frontal cortex of case 2 (FC, lane 6), as well as from the frontal cortex of typical PiD (lane 1), PSP (lane 2), and CBD cases (lane 3). Sarkosyl-insoluble tau in cases 1 and 2 consists predominantly of 4R tau isoforms (4R0N and 4R1N), similarly to that in PSP and CBD cases. A PiD case exhibits predominantly 3R tau isoforms. Six recombinant human tau isoforms are indicated on the right (Tau ladder). b Immunoblot analysis of the sarkosyl-insoluble fraction before dephosphorylation. The pattern of low-molecular mass tau fragments (upper panel) in a PSP case shows a prominent band of 33 kDa (lane 1, arrow), while that in a CBD case shows a prominent band of 37 kDa (lane 2, arrowhead). In cases 1 and 2, although the amount of cleaved tau fragments is very small, especially in the latter, in comparison with PSP and CBD cases (upper panel, lanes 3–5), both the 37-kDa and 33-kDa tau fragments become more recognizable after long exposure (lower panel, lanes 3–5). An additional band at approximately 50 kDa is present in the frontal cortex of case 2 (upper panel, lane 5). Also note that case 1 shows a CBD-predominant fragment pattern in the frontal cortex (lower panel, lane 3), but a PSP-predominant fragment pattern in the motor cortex (lower panel, lane 4). In case 1, tau lesions are mild in degree and occur predominantly in the glial (astrocytic) cells of the frontal cortex, while tau lesions are severe and occur equally in the neurons and glial (astrocytic) cells of the motor cortex (Table 1)
Tau gene
In case 1, there were no mutations in the tau gene; in case 2, the previous negative result [30] was also confirmed in the present study (data not shown).
Discussion
In the three cases examined in the present study, asymmetric extrapyramidal and pyramidal syndromes were the presenting manifestations, namely, involuntary movements and muscle weakness with spasticity, increased deep tendon reflexes, and so-called pathological reflexes. It is noteworthy that in all cases, muscle weakness was evident, and obvious muscle wasting was not noted in the upper and lower extremities throughout the entire clinical course. Neuroimaging revealed frontotemporal cerebral atrophy in cases 1 and 2 (with regard to case 3, CT or MRI examination was not available at that time); in the former, dementia was evident in the late stage of the illness. In cases 1 and 2 [30], PSP and CBD were considered as the possible clinical diagnosis during life, respectively. However, in general, MND shown in the present three cases is not a feature in patients with CBD [4, 22] or PSP [21].
It was evident that neuropathologically, the present three cases had a common tauopathy involving cytoplasmic accumulation of phosphorylated 4R tau in neurons and glial cells in a considerably wider area of the CNS; the disease process also involved sensory neurons in the dorsal root ganglia. The ultrastructural profiles of the cytoplasmic inclusions were also essentially the same in these three cases.
Clinicopathologically, the upper-motor predominant form of MND observed in the present three patients appeared to well correspond to the neuropathology obtained: like primary lateral sclerosis [37], neuronal loss, and gliosis of the upper-motor neuron system was obviously more severe than that of the lower-motor neuron system. However, it was not certain whether the extrapyramidal syndromes observed in these patients were explainable only by degeneration affecting the basal ganglia and substantia nigra: neuronal loss and gliosis in these regions were at most mild to moderate in degree. It is noteworthy that extrapyramidal syndromes (Parkinsonism) can be produced in the absence of neuronal loss in the basal ganglia and substantia nigra in patients with certain disease conditions affecting the fronto-parietal neocortical areas [5, 29].
The astrocytic tau lesions observed in the present three cases were unique, and apparently different in morphology from astrocytic plaques and tufted astrocytes, which are characteristic of CBD and PSP, respectively [9–12, 15, 18]. In cases 1 and 3 in the present study, like case 2 reported previously [30], it was also confirmed that the staining properties of the tau-positive neuronal and glial inclusions with silver impregnation were quite unusual, namely, roughly Bodian-positive and Gallyas–Braak negative; they were distinct from those of the tau-positive neuronal and glial inclusions observed in CBD [10, 11] and PSP [12, 15], two representative sporadic 4-repeat tauopathies, and were rather similar to those of the tau-positive neuronal inclusions (Pick bodies) observed in Pick’s disease, a representative sporadic 3-repeat tauopathy [38, 39].
Recently, focal involvement of the motor cortex, with degeneration of the corticospinal tracts, has been reported in PSP; in 11 out of 12 cases showing such a feature, the upper-motor predominant form of MND and extrapyramidal signs were present [16]. However, even in such cases of atypical PSP, the lower-motor neurons examined were spared and free of tau-positive inclusions. In addition, there have been a few previous reports of cases showing a combination of FTD, MND, and tau pathology [25, 41], in which the neuropathology of MND was that of typical ALS [31]. In the present three cases, no histological or immunohistochemical features suggestive of an association of ALS with the tau pathology were evident [28, 31]. Moreover, there have been several previous reports of unusual cases showing a combination of FTD and tau pathology [3, 13, 19, 32, 34, 36]. Of interest was that two sporadic cases described as having “multiple system 4R tauopathy” (one by Bigio et al. [3] and the other by Ferrer et al. [13]) demonstrated widespread neuronal and glial tau lesions in the CNS. However, in addition to the clinical features, the morphology, distribution and density of the neuronal and glial tau lesions appeared to be fundamentally different from those observed in the present three cases. The remaining cases can be considered to represent primarily white matter 4R tauopathies [19, 32] or unusual variants of CBD [34, 36].
Additionally, in the present three cases, no FUS pathology was observed in the CNS: FUS immunohistochemistry revealed no abnormal immunostaining corresponding to the tau-positive neuronal and astrocytic lesions, indicating that the disease condition affecting these patients was distinct from FTLD associated with FUS abnormalities [26, 27].
In the present study, in two patients (cases 1 and 2) who showed no mutations in the tau gene, immunoblotting of insoluble tau after dephosphorylation revealed predominantly 4R tau [1, 6]. Of great interest was that long exposure immunoblotting of insoluble tau before dephosphorylation revealed a shared feature of CBD (a prominent 37-kDa fragment) and PSP (a prominent 33-kDa fragment) [2]. To our knowledge, such a biochemical feature has so far been reported in only one previous case showing pathological features of both CBD and PSP [17]. It remains unclear why the neuronal and glial tau lesions in this apparent 4R tauopathy were not revealed by Gallyas–Braak staining.
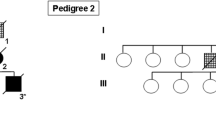
All of the three patients studied were Japanese. However, it seems very unlikely that the clinicopathological and biochemical features were attributable simply to unusual presentations of CBD or PSP within the Japanese population. In conclusion, our findings in the present three patients indicate that the sporadic 4R tauopathy widely affecting both neurons and glial cells in the CNS is a distinct disease entity associated with sporadic FTLD. However, as mentioned previously [30], it is still of interest that a similar clinicopathology may be encountered in patients with FTLD showing MAPT mutation: in two pedigrees with a K317M mutation, widespread 4R tau pathology affecting both neurons and glial cells has been described in association with FTD—Parkinsonism and MND [42].
References
Arai T, Ikeda K, Akiyama H et al (2001) Distinct isoforms of tau aggregated in neurons and glial cells in brains of patients with Pick’s disease, corticobasal degeneration and progressive supranuclear palsy. Acta Neuropathol 101:167–173
Arai T, Ikeda K, Akiyama H et al (2004) Identification of amino-terminally cleaved tau fragments that distinguish progressive supranuclear palsy from corticobasal degeneration. Ann Neurol 55:72–79
Bigio EH, Lipton AM, Yen S-H et al (2001) Frontal lobe dementia with novel tauopathy: sporadic multiple system tauopathy with dementia. J Neuropathol Exp Neurol 60:328–341
Boeve BF, Lang AE, Litvan I (2003) Corticobasal degeneration and its relationship to progressive supranuclear palsy and frontotemporal dementia. Ann Neurol 54(Suppl 5):S15–S19
Boeve BF, Maraganore DM, Parisi JE et al (1999) Pathologic heterogeneity in clinically diagnosed corticobasal degeneration. Neurology 53:795–800
Buée L, Delacourte A (1999) Comparative biochemistry of tau in progressive supranuclear palsy, corticobasal degeneration, FTDP-17 and Pick’s disease. Brain Pathol 9:681–693
Cairns NJ, Bigio EH, Mackenzie IRA et al (2007) Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the consortium for frontotemporal lobar degeneration. Acta Neuropathol 114:5–22
de Silva R, Lashley T, Gibb G et al (2003) Pathological inclusion bodies in tauopathies contain distinct complements of tau with three or four microtubule-binding repeat domains as demonstrated by new specific monoclonal antibodies. Neuropathol Appl Neurobiol 29:288–302
Dickson DW (1999) Neuropathologic differentiation of progressive supranuclear palsy and corticobasal degeneration. J Neurol 246(Suppl 2):II6–II15
Dickson DW, Bergeron C, Chin SS et al (2002) Office of rare diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol 61:935–946
Dickson D, Litvan I (2003) Corticobasal degeneration. In: Dickson DW (ed) Neurodegeneration: the molecular pathology of dementia and movement disorders. ISN Neuropath Press, Basel, pp 115–123
Dickson DW, Rademarkers R, Hutton ML (2007) Progressive supranuclear palsy: pathology and genetics. Brain Pathol 17:74–82
Ferrer I, Hernández I, Boada M et al (2003) Primary progressive aphasia as the initial manifestation of corticobasal degeneration and unusual tauopathies. Acta Neuropathol 106:419–435
Ghetti B, Hutton ML, Wszolek ZK (2003) Frontotemporal dementia and Parkinsonism linked to chromosome 17 associated with tau gene mutation (FTDP-17T). In: Dickson DW (ed) Neurodegeneration: the molecular pathology of dementia and movement disorders. ISN Neuropath Press, Basel, pp 86–102
Hauw J-J, Agid Y (2003) Progressive supranuclear palsy (PSP) or Steele-Richardson-Olszewski disease. In: Dickson DW (ed) Neurodegeneration: the molecular pathology of dementia and movement disorders. ISN Neuropath Press, Basel, pp 103–114
Josephs KA, Katsuse O, Beccano-Kelly DA et al (2006) Atypical progressive supranuclear palsy with corticospinal tract degeneration. J Neuropathol Exp Neurol 65:396–405
Katsuse O, Iseki E, Arai T et al (2003) 4-Repeat tauopathy sharing pathological and biochemical features of corticobasal degeneration and progressive supranuclear palsy. Acta Neuropathol 106:251–260
Komori T, Arai N, Oda M, Nakayama H et al (1998) Astrocytic plaques and tufts of abnormal fibers do not coexist in corticobasal degeneration and progressive supranuclear palsy. Acta Neuropathol 96:401–408
Kovacs GG, Majtenyi K, Spina S et al (2008) White matter tauopathy with globular glial inclusions: a distinct sporadic frontotemporal lobar degeneration. J Neuropathol Exp Neurol 67:963–975
Kuroda S, Otsuki S, Tateishi J, Hirano A (1979) Neurofibrillary degeneration in a case of quadriplegia and myoclonic movement. Acta Neuropathol 45:105–109
Litvan I, Agid Y, Calne D et al (1996) Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 47:1–9
Litvan I, Grimes DA, Lang AE (2000) Phenotypes and prognosis: clinicopathologic studies of corticobasal degeneration. Adv Neurol 82:183–196
Mackenzie IRA, Neumann M, Bigio EH et al (2009) Nomenclature for neuropathologic subtypes of frontotemporal lobar degeneration: consensus recommendations. Acta Neuropathol 117:15–18
Mackenzie IRA, Neumann M, Bigio EH et al (2010) Nomenclature and nosology for neuropathologic subtypes of frontotemporal lobar degeneration: an update. Acta Neuropathol 119:1–4
Martinaud O, Laquerrière A, Guyant-Maréchal L et al (2005) Frontotemporal dementia, motor neuron disease and tauopathy: clinical and neuropathological study in a family. Acta Neuropathol 110:84–92
Munoz DG, Neumann M, Kusaka H, Yokota O, Ishihara K, Terada S, Kuroda S, Mackenzie IR (2009) FUS pathology in basophilic inclusion body disease. Acta Neuropathol 118:617–627
Neumann M, Rademakers R, Roeber S, Baker M, Kretzschmar HA, Mackenzie IRA (2009) A new subtype of frontotemporal lobar degeneration with FUS pathology. Brain 132:2922–2931
Nishihira Y, Tan CF, Onodera O et al (2008) Sporadic amyotrophic lateral sclerosis: two pathological patterns shown by analysis of distribution of TDP-43-immunoreactive neuronal and glial cytoplasmic inclusions. Acta Neuropathol 116:169–182
Okazaki K, Fu Y-J, Nishihira Y et al (2009) Alzheimer’s disease: report of tow autopsy cases with a clinical diagnosis of corticobasal degeneration. Neuropathology doi:10.1111/j.1440-1789.2009.01062.x
Piao Y-S, Tan C-F, Iwanaga K et al (2005) Sporadic four-repeat tauopathy with frontotemporal degeneration, Parkinsonism and motor neuron disease. Acta Neuropathol 110:600–609
Piao Y-S, Wakabayashi K, Kakita A et al (2003) Neuropathology with clinical correlations of sporadic amyotrophic lateral sclerosis: 102 autopsy cases examined between 1962 and 2000. Brain Pathol 12:10–22
Powers JM, Bryne NP, Ito M et al (2003) A novel leukoencephalopathy associated with tau deposits primarily in white matter glia. Acta Neuropathol 106:181–187
Rizzu P, Van Swieten JC, Joosse M et al (1999) High prevalence of mutations in the microtubule-associated protein tau in a population study of frontotemporal dementia in the Netherlands. Am J Hum Genet 64:414–421
Sakai K, Piao Y-S, Kikugawa K et al (2006) Corticobasal degeneration with focal, massive tau accumulation in the subcortical white matter astrocytes. Acta Neuropathol 112:341–348
Spillantini MG, Bird TD, Ghetti B (1998) Frontotemporal dementia and Parkinsonism linked to chromosome 17: a new group of tauopathies. Brain Pathol 8:387–402
Tan C-F, Kakita A, Piao Y-S et al (2003) Primary lateral sclerosis: a rare upper-motor-predominant form of amyotrophic lateral sclerosis often accompanied by frontotemporal lobar degeneration with ubiquitinated neuronal inclusions? Report of an autopsy case and a review of the literature. Acta Neuropathol 105:615–620
Tan C-F, Piao Y-S, Kakita A et al (2005) Frontotemporal dementia with co-occurrence of astrocytic plaques and tufted astrocytes, and severe degeneration of the cerebral white matter: a variant of corticobasal degeneration? Acta Neuropathol 109:329–338
Uchihara T (2007) Silver diagnosis in neuropathology: principles, practice and revised interpretation. Acta Neuropathol 113:483–499
Uchihara T, Ikeda K, Tsuchiya K (2003) Pick body disease and Pick syndrome. Neuropathology 23:318–326
van Swieten J, Spillantini MG (2007) Hereditary frontotemporal dementia caused by tau gene mutations. Brain Pathol 17:63–73
Yokota O, Tsuchiya K, Oda T et al (2006) Amyotrophic lateral sclerosis with dementia: an autopsy case showing many Bunina bodies, tau-positive neuronal and astrocytic plaque-like pathologies, and pallido-nigral degeneration. Acta Neuropathol 112:633–645
Zarranz JJ, Ferrer I, Lezcano E et al (2005) A novel mutation (K317M) in the MAPT gene causes FTDP and motor neuron disease. Neurology 64:1578–1585
Zhukareva V, Mann D, Pickering-Brown S et al (2002) Sporadic Pick’s disease: a tauopathy characterized by a spectrum of pathological τ isoforms in gray and white matter. Ann Neurol 51:730–739
Acknowledgments
We thank C. Tanda, J. Takasaki, H. Saito, T. Fujita and S. Egawa for their technical assistance. This work was supported by a grant from the Research Committee for CNS Degenerative Diseases, the Ministry of Health, Labour and Welfare, Japan (H. T.), Grants-in-Aid 20240037 (to H. T.) and 21200041 (to T. I.) for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology, Japan, and a Project Research Promotion Grant from the University of Niigata (to H. T.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fu, YJ., Nishihira, Y., Kuroda, S. et al. Sporadic four-repeat tauopathy with frontotemporal lobar degeneration, Parkinsonism, and motor neuron disease: a distinct clinicopathological and biochemical disease entity. Acta Neuropathol 120, 21–32 (2010). https://doi.org/10.1007/s00401-010-0649-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-010-0649-2