Abstract
Mutations in the amyloid precursor protein (APP), presenilin 1 (PSEN1) and presenilin 2 (PSEN2) genes cause autosomal dominant familial Alzheimer’s disease (AD). PSEN1 and PSEN2 are essential components of the γ-secretase complex, which cleaves APP to affect Aβ processing. Disruptions in Aβ processing have been hypothesised to be the major cause of AD (the amyloid cascade hypothesis). These genetic cases exhibit all the classic hallmark pathologies of AD including neuritic plaques, neurofibrillary tangles (NFT), tissue atrophy, neuronal loss and inflammation, often in significantly enhanced quantities. In particular, these cases have average greater hippocampal atrophy and NFT, more significant cortical Aβ42 plaque deposition and more substantial inflammation. Enhanced cerebral Aβ40 angiopathy is a feature of many cases, but particularly those with APP mutations where it can be the dominant pathology. Additional frontotemporal neuronal loss in association with increased tau pathology appears unique to PSEN mutations, with mutations in exons 8 and 9 having enlarged cotton wool plaques throughout their cortex. The mechanisms driving these pathological differences in AD are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a slowly progressive degenerative dementia accounting for about one-third of the number of demented persons worldwide [222] and 6–10% of the North American population [80]. The inexorable decline in cognitive abilities usually occurs 32 months prior to diagnosis at an average age of 72 years [94]. Institutionalisation occurs on average at the age of 78 years and death intervenes approximately 8.5 years after the disease onset [94]. At autopsy, many cases with AD also have other coexisting pathologies such as Lewy bodies and Pick bodies, although these pathologies will not be considered in the current review.
Genetics of AD
Most of the AD cases are ‘sporadic’ with a disease onset after the age of 65 years (late-onset AD), although several susceptibility gene alleles confer an increased risk of late-onset AD, with the most well-established being the apolipoprotein E (ApoE) ε4 allele [163]. In addition, environmental interactions increase the risk of sporadic disease, including increased cardiovascular risk (high cholesterol, hypertension, atherosclerosis, coronary heart disease, and diabetes [18]) and obesity (both abdominal and body mass index-calculated [218–220]). These factors will not be considered in this review, but rather genetic effects shown to cause AD will be discussed.
Dominant genetic abnormalities that cause AD are largely due to fully penetrant, autosomal dominant mutations in 3 genes: the amyloid precursor protein (APP) gene on chromosome 21, presenilin 1 (PSEN1) on chromosome 14 and presenilin 2 (PSEN2) on chromosome 1. Mutations in PSEN1 account for the majority of autosomal dominant cases with 173 mutations described to date, compared to 30 and 14 mutations in APP and PSEN2, respectively (http://www.molgen.ua.ac.be/ADMutations). More recently an extra copy of the APP gene has also been identified in families with AD [170, 171]. In the majority of autosomal dominant cases, these mutations occur before the age of 65 years (early-onset AD), although rare mutations have been identified in families with late-onset AD.
Common pathogenic mechanisms
The pathological hallmarks of both sporadic and familial AD are extracellular senile plaques made up of Aβ peptides and intracellular neurofibrillary tangles (NFT) made up of hyperphosphorylated tau.
Aβ production and toxicity
Aβ peptide formation occurs through proteolysis of the amyloid precursor protein (APP) via the action of α-, β- and γ-secretases [56, 178, 187, 228]. These secretases normally process APP through two mutually exclusive pathways to produce various peptides, including Aβ [70, 177]. The non-amyloidogenic pathway occurs when membrane-associated α-secretase cleaves within the Aβ domain, thus precluding Aβ formation, and an intramembrane cleavage by the γ-secretase complex produces soluble APPα, a shortened fragment called p3 [71] and a cytoplasmic fragment identified as the APP intracellular domain (AICD) [173] (Fig. 1). In contrast, the amyloidogenic pathway initially cleaves APP at the N-terminus of the Aβ domain by β-secretase then cleaves by γ-secretase [62, 169] to generate soluble APPβ and the Aβ40 and Aβ42 peptides [70] (Fig. 1). Recently a new cleavage site for γ-secretase has been described which cleaves between the AICD (ε-cleavage) and γ-secretase site and generates longer Aβ forms, including Aβ42, Aβ45, Aβ46 and Aβ48 [231] (Fig. 1).
Proteolytic processing pathways of APP. The non-amyloidogenic pathway occurs when cleavage of APP by α-secretase yields soluble APPα, thus precluding Aβ production. Further processing by γ-secretase within its transmembrane domain leads to generation of the p3 peptide and the amyloid intracellular domain (AICD). The amyloidogenic pathway occurs via β-cleavage of APP, yielding soluble APPβ and a C terminal fragment, which undergoes further cleavage by γ-secretase leading to generation of the Aβ peptide, predominately Aβ40 and Aβ42
Aβ40 and Aβ42 exist in different conformational states anywhere from monomers to dodecamers or even higher molecular weight complexes that remain soluble after high-speed centrifugation. Anything larger than a monomer can be referred as an oligomer. Oligomers may then grow in size and form insoluble fibrils, which the Aβ42 alloform is more inclined than Aβ40 [17, 76, 215]. Due to their greater aggregation capabilities [17], longer forms of the Aβ peptides, particularly Aβ42, are considered more neurotoxic, although it is the oligomeric rather than the fibrillar non-soluble amyloid forms which appear most damaging [50, 77, 98, 151, 214, 215]. There is a robust correlation between soluble oligomeric Aβ levels and the extent of synaptic loss and severity of cognitive dysfunction in AD, with these correlations being limited for fibrillar Aβ [124, 135]. These data support the amyloid cascade hypothesis of AD [75]. Direct binding of oligomeric Aβ to synapses [103] with the resultant disruption of long-term potentiation [114, 214, 216] has been shown experimentally, although other mechanisms of oligomeric Aβ toxicity have also been described. These include Aβ’s ability to generate oxidative stress, mitochondrial damage, inflammation, and pore formation in membranes [44, 84, 121, 212]. In addition, Aβ is capable of altering tau phosphorylation, cleavage and aggregation [39, 45] providing a link between the two major pathological hallmarks of the disease.
Tau production, phosphorylation and toxicity
Tau is a microtubule-associated protein that stabilises the cytoskeleton, constantly undergoing phosphorylation and dephosphorylation to achieve this. In adult human brain, six isoforms of tau ranging from 352 to 441 amino acids are produced from a single gene by alternative splicing. These isoforms differ by the presence of one or two amino-terminal inserts and either three or four microtubule binding domains. All six isoforms can be phosphorylated through the action of several kinases, including glycogen synthase kinase-3β (GSK-3β), cyclin-dependent kinase-5 (Cdk5) and other tau kinases [6, 123].
In normal ageing, AD and other neurodegenerative diseases, natively unfolded tau becomes hyperphosphorylated and folds into a β conformation, forming abnormal filaments which become the paired helical filaments of NFT and neuritic infiltrates in plaques [27, 126]. In AD, tau neurotoxicity is, at least in part, due to an increase in the phosphorylation of all six isoforms causing hyperphosphorylation and leading to reduced microtubule binding, destabilization of the cytoskeleton, reduced axonal transport [4, 194] and insoluble intracellular fibril formation [5, 8, 104]. Classical NFT are flame-shaped and situated in cell bodies and apical dendrites while tau-positive neurites are found in distal dendrites. Once a neuron dies NFT can persist in an extracellular (or ghost) form due to their intense hyperphosphorylation and insolubility, although the precise role of tau fibrils in cellular toxicity is currently under debate [86]. NFTs are required for the clinical expression of AD, and in related tauopathies leading to dementia in the absence of amyloid plaques. In AD, neuronal loss occurs in brain regions depositing tau fibrils [227] but experimentally suppressing the mutant P301L tau transgene in a model that exhibits neurofibrillary pathology halts neuronal loss but not tau fibril formation [190]. Recent research points to a potential toxic form of soluble tau as necessary for neuronal death, as soluble tau is more toxic to neurons than aggregated, paired helical filament forms [65] and removal of soluble tau is required to achieve a therapeutic benefit with Aβ immunisation [155]. The precise molecular mechanisms of such toxicity have not been fully elucidated, as tau is modified posttranslationally by a series of complex methods, including hyperphosphorylation, glycosylation, ubiquitination, glycation, polyamination, nitration, and truncation [3]. Hyperphosphorylated tau can exist as soluble oligomeric aggregates being considered as the toxic species [86], although overexpression of an Aβ-induced, caplain-mediated cleavage of tau has also been proposed as this accelerates apoptosis and fibril formation through hyperphosphorylation [39]. Treatment of wild-type neurons with a caplain inhibitor prevents tau truncation and Aβ-induced neuronal death [159].
Common AD pathologies
Pathologies required for diagnosis
Aβ plaques and NFT are required for the diagnosis of AD. The plaque type used to diagnose AD is neuritic rather than diffuse plaques. Neuritic plaques are associated with fibrillar Aβ and dystrophic tau-positive neurites with or without a central Aβ neuritic core [15]. These plaques are smaller in size to diffuse plaques but, in contrast to diffuse plaques (which predominantly contain Aβ42), they contain both Aβ40 and Aβ42 peptides. Regions where neuritic and cored plaques are commonly found in AD include the middle frontal, superior and middle temporal, inferior parietal and entorhinal cortices and the hippocampus, which are the areas proposed for examination according to the CERAD criteria [138]. Predilection sites for tau neuritic and NFT pathology in AD are described in the Braak staging criteria. Using both the anatomical location and density of NFT formation with age, Braak and colleagues developed six stages of NFT formation with four of these stages occurring prior to the development of dementia [26]. NFT stages I/II occur in the entorhinal region, stages III/IV infiltrate into limbic regions and stages V/VI include the neocortex with these three groups corresponding to normal cognition, some cognitive impairment and frank dementia [26]. It is currently recommended that for diagnostic assessment Braak staging in conjunction with the assessment of plaque distribution, type and number from the CERAD protocol is used [138]. However, none of the neuropathological criteria set have been uniformly accepted by neuropathologists and variability and overlap in pathologies can lead to difficulties in diagnosis [92].
Atrophy and neuronal loss
Although not required for a definitive diagnosis of AD, the degeneration of brain structure is assumed to be the main substrate for the precipitation of AD dementia. While brain volume can be easily measured using MRI techniques, the identification of atrophy is more difficult due to considerable inter-individual variation in brain shape and size as well as some atrophy of white matter (less than 0.25% per year) as a normal consequence of age [57, 162]. In older individuals with mild cognitive impairment this rate of atrophy doubles in posterior cingulate, temporoparietal and medial temporal regions [57, 93]. Once clinical AD commences, progressive atrophy and neuronal loss particularly affect the hippocampus [19, 20, 91, 106] correlating with Braak staging [167, 221]. Mean brain atrophy rates for well-established clinically diagnosed AD are 2.4% per annum, with a widespread and symmetrical generalised volume loss [35, 58] with more concentrated atrophy in fusiform and inferior temporal gyri, the temporal pole, superior and middle frontal gyri, amygdala, entorhinal cortex and hippocampus. Regions unaffected by neuronal loss include orbital, inferior frontal and postcentral gyri and the posterior hippocampus [73].
In the hippocampus atrophy relates to the degree of neuronal loss [105], a concept that may be extrapolated to other brain regions. Until recently the molecular mechanism leading to neuronal loss was considered to be the deposition of fibrillar forms of hyperphosphorylated tau (see above), although evidence for other cellular mechanisms cannot be ignored. It has been suggested that apoptosis might be the primary mechanism underlying AD neurodegeneration [40] and there is substantial evidence demonstrating that at least some cells in sporadic AD die via apoptosis [29, 41, 191, 195]. Other characteristic signs of apoptosis observed in AD include mitochondrial dysfunction, caspase activity, nuclear abnormalities, DNA damage and altered activity of apoptosis-related genes, such as p53 and Bax [29, 133, 196]. Aβ can induce apoptosis by downregulating Bcl-2 and upregulating Bax [157] and by inducing oxidative stress and lipid peroxidation [44], which are the common features of AD brain [33, 144, 154, 196]. Apoptotic neuronal death has also been linked with failed attempts to reenter the cell cycle leading to abortive apoptosis [147], a theory which is supported by the presence of DNA replication in vulnerable neurons in AD [229].
Atrophy may occur because of cell shrinkage and/or synaptic loss. Decreased neuronal size (rather than neuronal loss) has been demonstrated in a recent study of AD where there was a marked decrease in the size of large neurons from layers II and III of the middle temporal cortex accompanied by an increase in the numbers of small neurons, suggesting that these supragranular layer neurons become atrophic in AD [208]. Neuronal atrophy could occur either because of reduced neurotrophic support or signalling in AD [175], or because of oligomeric Aβ induced synaptic changes [111, 140], resulting in synaptic degradation and remodelling of dendritic spines [112, 179]. Such changes are thought to occur prior to the complete loss of neurons in AD.
Inflammation
Alzheimer’s disease is also characterised by a chronic inflammatory response, possibly initiated by deposited fibrillar Aβ fragments binding to C1q receptors on microglia [55]. Increased numbers of activated microglia associate particularly with neuritic plaques [60, 165, 180, 184], even though they rarely contain phagocytosed Aβ and degrade it exceedingly slowly [59, 158]. Activated microglia directly produce toxic oxygen species and destructive enzymes that damage neurons [60, 95] and cause neurite retraction [143]. Microglial activation or the presence of Aβ deposits also cause astrocyte recruitment in order to facilitate Aβ clearance. Indeed, astrocytes in the entorhinal cortex of AD cases have been shown to contain Aβ42 in amounts proportionate to the severity of regional AD pathology [146]. However, astrocytes can also potentially act as a source of Aβ by overexpressing BACE1 when chronically stressed [168]. The degree of inflammation correlates with brain atrophy [34] and the severity of dementia [156] in early AD.
Pathogenic mechanisms of genetic forms of AD
Mutations in APP, PSEN1 and PSEN2 have all been shown to affect APP processing to alter the levels and/or length of Aβ produced, consistent with the amyloid cascade hypothesis [75]. Different APP mutations cause neuronal death via different pathogenic mechanisms [78], although all APP mutations cluster around the β- and γ-secretase cleavage sites to increase the overall production of Aβ by enhancing β-secretase cleavage [38], or modifying γ-secretase processing [193]. Some APP mutations also increase production of the AICD and other C-terminal APP fragments [102]. These fragments have been shown to play a direct role in modulating gene expression, cytoskeletal dynamics and apoptosis [61, 99, 142, 148]. Other APP mutations affect alternate intracellular mechanisms to increase cellular vulnerability to oxidative stress and death [54].
PSEN1 and PSEN2 are alternate subunits of the γ-secretase protein complex with mutations directly affecting Aβ peptide metabolism through γ-secretase cleavage to increase Aβ42 production [22, 32, 37, 139, 176]. However, experimental loss of PSEN1 and PSEN2 results in an age-related, progressive neurodegeneration characterised by synaptic loss, neuronal death, astrogliosis and tau hyperphosphorylation [13, 174] but virtually no Aβ production [47, 81]. In fact some PSEN1 mutations cause severe neurodegeneration in the absence of Aβ pathology as evidenced by the identification of a number of families with mutations in PSEN1 and frontotemporal dementia [49, 164], although further evidence for mutation segregation in these families is necessary. This has lead to the hypothesis that PSEN mutations give rise to AD through an additional partial, or in some instances a complete, loss of function [224]. The γ-secretase protein complex interacts with a large number of substrates [205] and mutations in PSEN have been shown to reduce its proteolytic activity towards several substrates [14] while enhancing APP metabolism to increase Aβ42 production [22, 32, 37, 139, 176]. Given that the γ-secretase protein complex has a large number of substrates, either a shift in substrate specificity or a partial loss of function may result in a diverse spectrum of toxicity.
The increase in Aβ peptide production of these mutations is thought to produce quantitative differences in the diagnostic pathologies (namely plaques and NFT) between genetic and sporadic forms of AD. Many studies have reported an increase in overall Aβ plaque pathology in APP, PSEN1 and PSEN2 cases compared to sporadic AD (Table 1) [63, 64, 88, 89, 108, 128, 130, 131]. However, most studies show considerable overlap with a recent report showing no statistical difference between plaque loads in PSEN1 and sporadic AD [226], similar to reports in PSEN2 Volga German families [127] and in other studies of PSEN1 and APP AD cases [122, 131, 153]. In contrast, all studies appear to agree on the fact that the majority of plaques contain Aβ42 in genetic forms of AD, often with no increase in Aβ40 compared to sporadic AD cases (Table 1) [63, 90, 127, 128, 131]. However, an increase in the mean area of cortex occupied by Aβ40 positive plaques has been reported in one of the largest studies of PSEN1 AD [89]. The reason for the discrepancy between studies is unclear, although mutation position is likely to account for some of the variations reported, at least in the PSEN1 cases [128]. It should also be noted that dramatic quantitative variations in neuropathology can exist in subjects with identical PSEN1 mutations, even when they are members of the same family [63].
Unfortunately, there are only limited studies describing the effect of PSEN or APP mutations on oligomeric Aβ concentrations, with most studies including very small numbers of cases [83, 108, 136, 149, 200–202, 210] and no studies on PSEN2 AD. These studies have largely shown increases in both soluble, and to a greater extent, insoluble Aβ42 in genetic compared to sporadic AD brain tissue (Table 2). This is consistent with the increased Aβ42 plaque burden described above. The data concerning Aβ40 appear more variable with some studies showing no change or a decrease compared to sporadic AD [136, 149, 200, 201] while others have shown increases [83, 108, 136, 200, 202], consistent with some immunohistochemical findings [89]. While these data support a growing body of literature demonstrating an increase in Aβ42 in genetic forms of AD, it is not easy to reconcile the variable reports concerning Aβ40, especially in light of in vitro and in vivo studies demonstrating mutation-specific decreases in Aβ40 [22, 51, 85, 108, 201, 213, 224]. However, there is also variability among these studies, with some mutations failing to demonstrate any change in Aβ [12, 185], while others report a decrease in Aβ42/Aβ40 ratio, suggesting a relative increase in Aβ40 [2], although additional studies to determine the pathological relevance of this mutation is required. Indeed, discrepancies between in vitro and human brain measurements of Aβ40 have also been observed in a single study using the same gene mutation [108]. Some of these studies have also found decreased levels of Aβ40 and Aβ42 in controls compared to sporadic AD cases, indicating that enhanced Aβ42 production driven by γ-secretase activity is not a feature of sporadic AD [200, 201].
Vascular Aβ
Amyloid precursor protein mutations are often associated with severe cerebral amyloid angiopathy (CAA) (Fig. 2v) and consequent cerebral haemorrhage or stroke, in addition to the conventional neuritic pathology (neuritic plaques, neuropil threads, NFT) [42, 107]. The type of Aβ deposited in vessels in CAA is Aβ40 (Fig. 2v), while plaques contain both Aβ40 and Aβ42 [166]. In some APP mutation cases, CAA dominates and there is little to no coexisting AD pathology or progressive dementia [107]. This is particularly observed in Dutch APP mutation carriers where the cognitive impairment is mostly due to recurrent vascular events, as AD pathology is rarely present [23, 150]. CAA is also found in some PSEN1 and PSEN2 mutations. There is evidence that mutations occurring in the PSEN1 gene after codon 200 have a higher incidence of severe CAA and more plaque formation [128]. Assessment of a single case with a novel L282V PSEN1 mutation agrees with this observation, finding significant Aβ40 in the vessels and plaque cores and N-truncated Aβ42 in diffuse plaques [48]. Neuropathological examination of a family carrying a PSEN2 mutation identified five of six demented members fulfilling the pathological criteria for AD and four of these had mild to severe CAA with evidence of a vascular event in one [152].
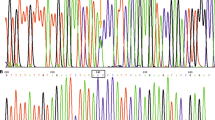
Representative micrographs of variant pathologies in the inferior temporal cortex of genetic forms of AD. i Haematoxylin and eosin stained section of a PSEN1 AD case demonstrating a cotton wool plaque (CWP). Note the lack of cellular infiltrate as indicated by an absence of glial nuclei. ii Section of a PSEN1 AD case immunohistochemically stained with an antibody against tau protein (tau-2). Tau-2 immunohistochemistry reveals globular staining in CWP. iii Immunohistochemical labelling of an inflammatory plaque (IP) stained with an antibody against Aβ42 and glial fibrillary acidic protein (GFAP) and counterstained with cresyl violet (purple) to reveal the unstained core. Abundant GFAP-positive astrocytes surround the Aβ-negative core of IPs. iv Immunohistochemical labelling of a classic cored plaque stained with an antibody against Aβ42 in a sporadic AD case. Unlike IPs, these plaques have a dense Aβ-positive core. v Immunohistochemical labelling with an antibody against Aβ40 in an APP AD case demonstrating severe Aβ40 cerebral amyloid angiopathy and unusual parenchymal Aβ40 plaques
In addition to fibrillar CAA deposition in vessel walls (sometimes extending into the lumen and out into the parenchyma), patients with APP mutations often have abnormal Aβ deposits associated with the CAA. Patients with the Flemish APP mutation often form plaques with unusually large, dense and sometimes multiple cores around or adjacent to vessels [30, 42, 107] (Fig. 2v). The Arctic APP mutation causes a more typical CAA of subarachnoid and parenchymal vessels, but has an unusual ring-like plaque lacking a central core but staining strongly with Aβ42 [11]. The Iowa APP mutation has a late age of onset compared with the Italian APP mutation with both exhibiting severe CAA with vessel thickening, calcification and occlusion in addition to vessel-associated dystrophic neurites [67, 209].
Aβ cotton wool plaques
Aβ cotton wool plaques (CWP) are most often observed in PSEN1 mutations affecting exons 8 and 9 [31, 43, 52, 83, 97, 110, 128, 129, 182, 188, 198, 211] but are also reported in PSEN1 mutations in exons 4 [192], 5, 6 [182], 12 [186] and intron 8 [52]. They occur in addition to the diffuse, neuritic and cored AD plaque types, and have been noted infrequently in sporadic AD [118, 230]. To date, 30 PSEN1 families with 25 defined mutations have been identified with CWP pathology [52, 72, 97, 186].
Cotton wool plaques have several characteristic features, notably that they are larger than most diffuse or neuritic plaques (up to 150 μm in diameter), have eosinophilic properties, clearly defined margins and little neuritic or inflammatory infiltrate [43] (Fig. 2i, ii). Staining with thioflavin S to detect fibrillar Aβ shows only very weak reactivity [43, 192, 198, 211]. When immunostained, CWP display strong positivity for Aβ42 and weak or little Aβ40 [129, 137, 186, 192, 198, 207, 211]. Immunohistochemistry also indicates the presence of non-hyperphosphorylated tau-2 [182] (Fig. 2ii) and shows variable positivity for AT8 phospho-tau within [198, 211] and around the margins of the plaques [129, 207]. Very little complement (C1q, C3d and C9) or glial activity [43, 129] is seen around CWP with immunostaining. More recently, the synaptic proteins synapsin-1 and synaptophysin have been found in CWP in the C410Y PSEN1 mutation [72]. The typical distribution pattern of CWP follows that of neuritic and diffuse plaques in AD, which are mainly found in the neocortex, particularly the frontal, cingulate and temporal cortices as well as limbic regions and striatum [192, 198, 211]. They extend through all cortical layers, often encroaching into the superficial white matter [186].
Atrophy and neuronal loss
A recent study has demonstrated greater rates and amounts of atrophy in PSEN1 and APP cases, particularly in the medial temporal lobes, despite similar disease durations [68, 69]. Greater amount and rate of neuronal loss in PSEN1 AD has also been observed in frontal and temporal regions compared to APP and sporadic AD (Table 3) [63, 69, 144, 181]. This effect may be due to the influence of PSEN1 on other substrates of the γ-secretase complex, such as β-catenin, N-Cadherin, GSK-3β, tau, calsenilin, Bcl2 proteins, metalloproteases and Notch to name just a few [205]. All of these substrates have been implicated in AD-related pathologies, such as disturbed calcium homeostasis (calsenilin), apoptosis (Bcl2), abnormal protein aggregation (tau, GSK-3β) and alterations in the cell cycle (β-catenin). Both in vitro and in vivo studies have demonstrated detrimental effects of PSEN mutations on apoptosis [10, 53], cell cycle events [1, 125], oxidative stress [21], mitochondrial dysfunction [99] and calcium dysregulation [134]. Enhanced levels of cyclin D1 indicative of abortive β-catenin regulation of cell cycle re-entry are found in some PSEN1 cases [125] and mutant PSEN can alter calcium signalling [36] and inactivate neuroprotective signalling pathways [9] to enhance neuronal degeneration.
Tau pathology
In spite of an increase in neuronal loss in genetic forms of AD (see above), it is not clear whether this is related to a general increase in NFT. Some studies show an increase in NFT compared to sporadic cases [79, 197] while others report no change [63, 64, 116, 122, 153, 226] (Table 4). This variability may be partly due to variation in the ApoE gene, which appears to affect tau and Aβ40 load [203]. Sudo and colleagues [197] report that the effects of ApoE on tau pathology is region specific with the entorhinal cortex being the initial site of NFT formation in sporadic AD compared to the CA regions of the hippocampus in APP and PSEN1 AD [197].
A significant increase in plaque-associated tau deposition has been reported in PSEN1 AD with this difference being markedly greater than the difference in Aβ deposition (6.6-fold versus 2-fold increase, respectively) [182]. A significant increase in phosphorylated tau protein within the neuropil has also been shown in PSEN1 cases [118] with PSEN1 gene mutations increasing total tau protein levels in Aβ treated neurons [161]. Deposition of additional non-fibrillar, non-hyperphosphorylated tau has also been reported in CWP in PSEN1 AD [182] consistent with an accelerated rate of cytoskeletal pathology in these cases [226]. However, a mutational deletion in exon 8 (L271V) of PSEN1 results in a complete absence of neuritic plaque pathology and a decrease in PSEN1 function [110]. Furthermore, in cases with mutations in PSEN1 giving rise to frontotemporal dementia [49, 164] and transgenic mice with common PSEN1 mutations [117] there is significant tau pathology without Aβ deposition indicative of alterations in tau processing and tau kinases [10, 199].
To date several studies have investigated the concentrations of tau in the soluble and PHF protein fractions in sporadic AD cases using biochemical techniques [7, 24, 28, 74, 82, 87, 100, 113, 119, 141, 204, 217, 223]. These studies show a redistribution of soluble tau to PHF consistent with increased NFT pathology in AD [25]. However, only one study has performed a quantitative analysis of the detergent-insoluble tau in PSEN1 and PSEN2 AD compared to sporadic cases and found no increase using a proteomic approach [225]. Further analysis of changes in tau expression, aggregation and phosphorylation in genetic forms of AD is now required in order to elucidate the role of APP and PSEN in tau pathology.
Inflammation
Imaging studies of sporadic AD demonstrate an association between microglial activation, brain atrophy and clinical progression [34]. However, no microglial imaging studies have been carried out in genetic forms of AD, and only a few studies have described the inflammatory response in these cases [120, 183, 189]. While CWP have consistently been reported as being devoid of cellular infiltrate, PSEN1 cases display a potent inflammatory response around other plaques [183] and have greater levels of inflammatory mediators in soluble brain tissue extracts [189], possibly due to a loss of PSEN regulation of inflammation [13]. These plaques with increased inflammation have been called inflammatory plaques (IP) and are found in cortical regions of both PSEN1 and APP mutation cases [181, 183].
Inflammatory plaques are small (around 25 μm diameter), dense and well-circumscribed with a distinct core and accumulations of surrounding reactive microglia and astrocytes (Fig. 2iii). The plaque core has a particularly curious staining profile, showing positivity with simple histological stains such as silver, haematoxylin and eosin, cresyl violet and thioflavin S (Fig. 2iii), but negativity for many of the components of conventional neuritic plaque cores (Fig. 2iv) such as Aβ, tau, ApoE, ubiquitin, PSEN1, IgG, α-synuclein, filipin and glial fibrillary acidic protein. HLA-DR, ferritin and glial fibrillary acidic protein immunohistochemistry demonstrate the presence of significant numbers of activated microglia and astrocytes in the areas immediately surrounding IP [183] (Fig. 2iii). While the presence of IP per se are not associated with greater neuronal loss [181], increases in specific inflammatory mediators may play an important role in the disease process and contribute to the greater neurodegeneration observed in genetic forms of AD [189] and in PSEN1/APP transgenic models of AD [66, 109, 160].
Conclusions
Most PSEN1 and PSEN2 mutations and many APP mutations enhance Aβ42 production over that observed in sporadic AD via changes in γ-secretase processing of APP, thereby supporting the amyloid cascade hypothesis [75]. This is reflected in greater hippocampal atrophy and NFT, and more significant cortical deposition of insoluble fibrillar Aβ42 plaques, which in PSEN1 cases with mutations in exons 8 and 9 forms enlarged CWP structures. More substantial inflammation is associated with a proportion of plaques (IP) in these cases. Aβ40-enhanced CAA is a feature of many cases with AD mutations, but particularly those with APP mutations where CAA can be the dominant pathology. Additional frontotemporal neuronal loss in association with tau increases appears unique to PSEN mutations, possibly due to an additional loss of PSEN function. These data indicate that APP and PSEN mutations have widespread effects on a broader range of cellular functions [16, 46, 96, 101, 115, 132, 145, 172, 206] compared to sporadic AD. These important differences need to be carefully considered when using these mutations to model AD. In particular, the enhanced γ-secretase production of Aβ42 is not a feature of sporadic AD.
References
Ahn KW, Joo Y, Choi Y et al (2008) Swedish amyloid precursor protein mutation increases cell cycle-related proteins in vitro and in vivo. J Neurosci Res 86(11):2476–2487
Albani D, Roiter I, Artuso V et al (2007) Presenilin-1 mutation E318G familial Alzheimer’s disease in the Italian population. Neurobiol Aging 28:1682–1688
Alonso AC, Li B, Grundke-Iqbal I, Iqbal K (2008) Mechanism of tau-induced neurodegeneration in Alzheimer disease and related tauopathies. Curr Alzheimer Res 5(4):375–384
Alonso AC, Zaidi T, Grundke-Iqbal I, Iqbal K (1994) Role of abnormally phosphorylated tau in the breakdown of microtubules in Alzheimer disease. Proc Natl Acad Sci USA 91(12):5562–5566
Alvarez A, Munoz JP, Maccioni RB (2001) A Cdk5–p35 stable complex is involved in the beta-amyloid-induced deregulation of cdk5 activity in hippocampal neurons. Exp Cell Res 264(2):266–274
Alvarez A, Toro R, Caceres A, Maccioni RB (1999) Inhibition of tau phosphorylating protein kinase cdk5 prevents beta-amyloid-induced neuronal death. FEBS Lett 459(3):421–426
Arendt T, Holzer M, Gertz HJ, Bruckner MK (1999) Cortical load of PHF-tau in Alzheimer’s disease is correlated to cholinergic dysfunction. J Neural Transm 106(5–6):513–523
Augustinack JC, Schneider A, Mandelkow EM, Hyman BT (2002) Specific tau phosphorylation sites correlate with severity of neuronal cytopathology in Alzheimer’s disease. Acta Neuropathol 103(1):26–35
Baki L, Neve R, Shao Z et al (2008) Wild-type but not FAD mutant presenilin-1 prevents neuronal degeneration by promoting phosphatidylinositol 3-kinase neuroprotective signaling. J Neurosci 28(2):483–490
Baki L, Shioi J, Wen P et al (2004) PS1 activates PI3 K thus inhibiting GSK-3 activity and tau overphosphorylation: effects of FAD mutations. EMBO J 23(13):2586–2596
Basun H, Bogdanovic N, Ingelsson M et al (2008) Clinical and neuropathological features of the arctic APP gene mutation causing early-onset Alzheimer disease. Arch Neurol 65(4):499–505
Batelli S, Albani D, Prato F et al (2008) Early-onset Alzheimer disease in an Italian family with presenilin-1 double mutation E318G and G394 V. Alzheimer Dis Assoc Disord 22(2):184–187
Beglopoulos V, Sun X, Saura C et al (2004) Reduced B-amyloid production and increased inflammatory responses in presenilin conditional knock-out mice. J Biol Chem 279(45):46907–46914
Bentahir M, Nyabi O, Verhamme J et al (2006) Presenilin clinical mutations can affect gamma-secretase activity by different mechanisms. J Neurochem 96(3):732–742
Benzing WC, Ikonomovic MD, Brady DR, Mufson EJ, Armstrong DM (1993) Evidence that transmitter-containing dystrophic neurites precede paired helical filament and Alz-50 formation within senile plaques in the amygdala of nondemented elderly and patients with Alzheimer’s disease. J Comp Neurol 334(2):176–191
Bergman ALH, Winblad B, Lundkvist J, Näslund J (2004) The extreme C terminus of presenilin 1 is essential for gamma-secretase complex assembly and activity. J Biol Chem 279(44):45564–45572
Bitan G, Kirkitadze MD, Lomakin A et al (2003) Amyloid beta-protein (Abeta) assembly: Abeta 40 and Abeta 42 oligomerize through distinct pathways. Proc Natl Acad Sci USA 100(1):330–335
Blennow K, de Leon MJ, Zetterberg H (2006) Alzheimer’s disease. Lancet 368(9533):387–403
Bobinski M, Wegiel J, Tarnawski M et al (1997) Relationships between regional neuronal loss and neurofibrillary changes in the hippocampal formation and duration and severity of Alzheimer disease. J Neuropathol Exp Neurol 56(4):414–420
Bobinski M, Wegiel J, Wisniewski HM et al (1995) Atrophy of hippocampal formation subdivisions with stage and duration of Alzheimer’s disease. Dementia 6:205–210
Bogdanovic N, Zilmer M, Zilmer K, Rehema A, Karelson E (2001) The Swedish APP670/671 Alzheimer’s disease mutation: the first evidence for strikingly increased oxidative injury in the temporal inferior cortex. Dement Geriatr Cogn Disord 12(6):364–370
Borchelt D, Thinakaran G, Eckman C et al (1996) Familial Alzheimer’s disease-linked presenilin 1 variants elevate Aβ1-42/1-40 ratio in vitro and in vivo. Neuron 17:1005–1013
Bornebroek M, Haan J, Maat-Schieman ML, Van Duinen SG, Roos RA (1996) Hereditary cerebral hemorrhage with amyloidosis-Dutch type (HCHWA-D): I—a review of clinical, radiologic and genetic aspects. Brain Pathol 6(2):111–114
Boutajangout A, Boom A, Leroy K, Brion JP (2004) Expression of tau mRNA and soluble tau isoforms in affected and non-affected brain areas in Alzheimer’s disease. FEBS Lett 576(1–2):183–189
Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Del Tredici K (2006) Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol 112(4):389–404
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82:239–259
Braak H, Braak E, Grundke-Iqbal I, Iqbal K (1986) Occurrence of neuropil threads in the senile human brain and in Alzheimer’s disease: a third location of paired helical filaments outside of neurofibrillary tangles and neuritic plaques. Neurosci Lett 65(3):351–355
Bramblett GT, Trojanowski JQ, Lee VM (1992) Regions with abundant neurofibrillary pathology in human brain exhibit a selective reduction in levels of binding-competent tau and accumulation of abnormal tau-isoforms (A68 proteins). Lab Invest 66(2):212–222
Broe M, Shepherd CE, Milward EA, Halliday GM (2001) Relationship between DNA fragmentation, morphological changes and neuronal loss in Alzheimer’s disease and dementia with Lewy bodies. Acta Neuropathol 101(6):616–624
Brooks WS, Kwok JB, Halliday GM et al (2004) Hemorrhage is uncommon in new Alzheimer family with Flemish amyloid precursor protein mutation. Neurology 63(9):1613–1617
Brooks WS, Kwok JB, Kril JJ et al (2003) Alzheimer’s disease with spastic paraparesis and ‘cotton wool’ plaques: two pedigrees with PS-1 exon 9 deletions. Brain 126(Pt 4):783–791
Brunkan AL, Martinez M, Wang J et al (2005) Two domains within the first putative transmembrane domain of presenilin 1 differentially influence presenilinase and gamma-secretase activity. J Neurochem 94(5):1315–1328
Butterfield DA, Castegna A, Lauderback CM, Drake J (2002) Evidence that amyloid beta-peptide-induced lipid peroxidation and its sequelae in Alzheimer’s disease brain contribute to neuronal death. Neurobiol Aging 23(5):655–664
Cagnin A, Gerhard A, Banati R (2002) In vivo imaging of neuroinflammation. Eur Neuropsychopharmacol 12(6):581–586
Chan D, Fox NC, Scahill RI et al (2001) Patterns of temporal lobe atrophy in semantic dementia and Alzheimer’s disease. Ann Neurol 49(4):433–442
Chan S, Culmsee C, Haughey N, Klapper W, Mattson M (2002) Presenilin-1 mutations sensitize neurons to DNA damage-induced death by a mechanism involving perturbed calcium homeostasis and activation of calpains and caspase-12. Neurobiol Dis 11(1):2–19
Chen F, Gu Y, Hasegawa H et al (2002) Presenilin 1 mutations activate gamma 42-secretase but reciprocally inhibit epsilon-secretase cleavage of amyloid precursor protein (APP) and S3-cleavage of notch. J Biol Chem 277(39):36521–36526
Citron M, Oltersdorf T, Haas C (1992) Mutation of the β-Amyloid precursor protein in familial Alzheimer’s disease increases β-protein production. Nature 360:672–674
Cotman CW, Poon WW, Rissman RA, Blurton-Jones M (2005) The role of caspase cleavage of tau in Alzheimer disease neuropathology. J Neuropathol Exp Neurol 64(2):104–112
Cotman CW, Su JH (1996) Mechanisms of neuronal death in Alzheimer’s disease. Brain Pathol 6:493–506
Cotman CW, Whittemore ER, Watt JA, Anderson AJ, Loo DT (1994) Possible role of apoptosis in Alzheimer’s disease. Ann N Y Acad Sci 747:36–49
Cras P, van Harskamp F, Hendriks L et al (1998) Presenile Alzheimer dementia characterized by amyloid angiopathy and large amyloid core type senile plaques in the APP 692Ala→Gly mutation. Acta Neuropathol 96(3):253–260
Crook R, Verkkoniemi A, Perez-Tur J et al (1998) A variant of Alzheimer’s disease with spastic paraparesis and unusual plaques due to deletion of exon 9 of presenilin 1. Nat Med 4(4):452–455
Crouch PJ, Harding SM, White AR et al (2008) Mechanisms of A beta mediated neurodegeneration in Alzheimer’s disease. Int J Biochem Cell Biol 40(2):181–198
De Felice FG, Wu D, Lambert MP et al (2008) Alzheimer’s disease-type neuronal tau hyperphosphorylation induced by A-beta oligomers. Neurobiol Aging 29(9):1334–1347
De Strooper B, Annaert W, Cupers P et al (1999) A presenilin-1-dependent gamma-secretase-like protease mediates release of Notch intracellular domain. Nature 398(6727):518–522
De Strooper B, Saftig P, Craessaerts K et al (1998) Deficiency of presenilin-1 inhibits the normal cleavage of amyloid precursor protein. Nature 391(6665):387–390
Dermaut B, Kumar-Singh S, De Jonghe C et al (2001) Cerebral amyloid angiopathy is a pathogenic lesion in Alzheimer’s disease due to a novel presenilin 1 mutation. Brain 124(Pt 12):2383–2392
Dermaut B, Kumar-Singh S, Engelborghs S et al (2004) A novel presenilin 1 mutation associated with Pick’s disease but not β-amyloid plaques. Ann Neurol 55(5):617–626
Deshpande A, Mina E, Glabe C, Busciglio J (2006) Different conformations of amyloid beta induce neurotoxicity by distinct mechanisms in human cortical neurons. J Neurosci 26(22):6011–6018
Dowjat W, Kuchna I, Wisniewski T, Weigel J (2004) A novel highly pathogenic Alzheimer presenilin 1 mutation in codon 117 (Pro117Ser): comparison of clinical, neuropathological and cell culture phenotypes of Pro117Leu and Pro117Ser mutations. J Alzheimer’s Dis 6(1):31–43
Dumanchin C, Tournier I, Martin C et al (2006) Biological effects of four PSEN1 gene mutations causing Alzheimer disease with spastic paraparesis and cotton wool plaques. Hum Mutat 27(10):1063–1071
Eckert A, Marques CA, Keil U, Schussel K, Muller WE (2003) Increased apoptotic cell death in sporadic and genetic Alzheimer’s disease. Ann N Y Acad Sci 1010:604–609
Eckert A, Steiner B, Marques C et al (2001) Elevated vulnerability to oxidative stress-induced cell death and activation of caspase-3 by the Swedish amyloid precursor protein mutation. J Neurosci Res 64(2):183–192
Eikelenboom P, Veerhuis R (1996) The role of complement and activated microglia in the pathogenesis of Alzheimer’s disease. Neurobiol Aging 17:673–680
Esch FS, Keim PS, Beattie EC et al (1990) Cleavage of amyloid beta peptide during constitutive processing of its precursor. Science 248(4959):1122–1124
Fotenos AF, Snyder AZ, Girton LE, Morris JC, Buckner RL (2005) Normative estimates of cross-sectional and longitudinal brain volume decline in aging and AD. Neurology 64(6):1032–1039
Fox NC, Cousens S, Scahill R, Harvey RJ, Rossor MN (2000) Using serial registered brain magnetic resonance imaging to measure disease progression in Alzheimer disease: power calculations and estimates of sample size to detect treatment effects. Arch Neurol 57(3):339–344
Frackowiak J, Wisniewski HM, Wegiel J et al (1992) Ultrastructure of the microglia that phagocytose amyloid and the microglia that produce beta-amyloid fibrils. Acta Neuropathol 84(3):225–233
Gahtan E, Overmier JB (1999) Inflammatory pathogenesis in Alzheimer’s disease: biological mechanisms and cognitive sequeli. Neurosci Biobehav Rev 23(5):615–633
Giliberto L, Zhou D, Weldon R et al (2008) Evidence that the Amyloid beta Precursor Protein-intracellular domain lowers the stress threshold of neurons and has a “regulated” transcriptional role. Mol Neurodegen 3:12–23
Goate A, Chartierharlin MC, Mullan M et al (1991) Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s-disease. Nature 349:704–706
Gomez-Isla T, Growdon W, McNamara M et al (1999) The impact of different presenilin 1 and presenilin 2 mutations on amyloid deposition, neurofibrillary changes and neuronal loss in the familial Alzheimer’s disease brain. Evidence for other phenotype-modifying factors. Brain 122:1709–1719
Gómez-Isla T, Wasco W, Pettingell WP et al (1997) A novel presenilin-1 mutation: increased ß-amyloid and neurofibrillary changes. Ann Neurol 41:809–813
Gomez-Ramos A, Diaz-Hernandez M, Cuadros R, Hernandez R, Avila J (2006) Extracellular tau is toxic to neuronal cells. FEBS Lett 580:4842–4850
Gordon M, Holcomb L, Jantzen P et al (2002) Time course of the development of Alzheimer-like pathology in the doubly transgenic PS1+APP mouse. Exp Neurol 173(2):183–195
Grabowski TJ, Cho HS, Vonsattel JP, Rebeck GW, Greenberg SM (2001) Novel amyloid precursor protein mutation in an Iowa family with dementia and severe cerebral amyloid angiopathy. Ann Neurol 49(6):697–705
Gregory G, Macdonald V, Schofield P, Kril J, Halliday G (2006) Differences in regional brain atrophy in genetic forms of Alzheimer’s disease. Neurobiol Aging 27(3):387–393
Gregory GC, Halliday GM (2005) What is the dominant Abeta species in human brain tissue? A review. Neurotox Res 7(1–2):29–41
Haass C, Hung AY, Vigo-Pelfrey C et al (1992) Amyloid b-peptide is produced by cultured cells during normal metabolism. Nature 359:322–327
Haass C, Selkoe DJ (1993) Cellular processing of β-amyloid precursor protein and the genesis of amyloid β-peptide. Cell 75:1039–1042
Haleem K, Lippa CF, Smith TW et al (2007) Presenilin-1 C410Y Alzheimer disease plaques contain synaptic proteins. Am J Alzheimer’s Dis Other Dementias 22(2):137–144
Halliday GM, Double KL, Macdonald V, Kril JJ (2003) Identifying severely atrophic cortical subregions in Alzheimer’s disease. Neurobiol Aging 24(6):797–806
Hanger DP, Brion JP, Gallo JM et al (1991) Tau in Alzheimer’s disease and Down’s syndrome is insoluble and abnormally phosphorylated. Biochem J 275(Pt 1):99–104
Hardy J, Higgins G (1992) Alzheimer’s disease: the amyloid cascade hypothesis. Science 256:184–185
Harper JD, Wong SS, Lieber CM, Lansbury PT (1997) Observation of metastable Abeta amyloid protofibrils by atomic force microscopy. Chem Biol 4(2):119–125
Hartley DM, Walsh DM, Ye CP et al (1999) Protofibrillar intermediates of amyloid beta-protein induce acute electrophysiological changes and progressive neurotoxicity in cortical neurons. J Neurosci 19(20):8876–8884
Hashimoto Y, Niikura T, Ito Y, Nishimoto I (2000) Multiple mechanisms underlie neurotoxicity by different types of Alzheimer’s disease mutations of amyloid precursor protein. J Biol Chem 275(44):34541–34551
Heckmann J, Low W, de Villers C et al (2004) Novel presenilin 1 mutation with profound neurofibrillay pathology in an indigenous Southern African family with early-onset Alzheimer’s disease. Brain 127(1):133–142
Hendrie HC (1998) Epidemiology of dementia and Alzheimer’s disease. Am J Geriatr Psychiatry 6(2 Suppl 1):S3–S18
Herreman A, Serneels L, Annaert W et al (2000) Total inactivation of gamma-secretase activity in presenilin-deficient embryonic stem cells. Nature Cell Biol 2:461–462
Herrmann M, Golombowski S, Krauchi K et al (1999) ELISA-quantitation of phosphorylated tau protein in the Alzheimer’s disease brain. Eur Neurol 42(4):205–210
Houlden H, Baker M, McGowan E et al (2000) Variant Alzheimer’s disease with spastic paraparesis and cotton wool plaques is caused by PS-1 mutations that lead to exceptionally high amyloid-beta concentrations. Ann Neurol 48(5):806–808
Iadecola C, Zhang F, Niwa K et al (1999) SOD1 rescues cerebral endothelial dysfunction in mice overexpressing amyloid precursor protein. Nat Neurosci 2(2):157–161
Ingelsson M, Fukumoto H, Newell KL et al (2004) Early Abeta accumulation and progressive synaptic loss, gliosis, and tangle formation in AD brain. Neurology 62(6):925–931
Iqbal K, Alonso Adel C, Grundke-Iqbal I (2008) Cytosolic abnormally hyperphosphorylated tau but not paired helical filaments sequester normal MAPs and inhibit microtubule assembly. J Alzheimer’s Dis 14(4):365–370
Iqbal K, Grundke-Iqbal I (1997) Elevated levels of tau and ubiquitin in brain and cerebrospinal fluid in Alzheimer’s disease. Int Psychogeriatr 9(1):289–296
Ishii K, Ii K, Hasegawa T et al (1997) Increased Aβ 42(43)-plaque deposition in early-onset familial Alzheimer’s disease brains with the deletion of exon 9 and the missense point mutation (H163R) in the PS-1 gene. Neurosci Lett 228:17–20
Ishii K, Lippa C, Tomiyama T et al (2001) Distinguishable effects of presenilin-1 and APP717 mutations on amyloid plaque deposition. Neurobiol Aging 22:367–376
Iwatsubo T, Odaka A, Suzuki N et al (1994) Visualization of A beta 42(43) and A beta 40 in senile plaques with end-specific A beta monoclonals: evidence that an initially deposited species is A beta 42(43). Neuron 13(1):45–53
Jack CR Jr, Petersen RC, Xu Y et al (2000) Rates of hippocampal atrophy correlate with change in clinical status in aging and AD. Neurology 55(4):484–489
Jellinger KA (2009) Criteria for the neuropathological diagnosis of dementing disorders: routes out of the swamp? Acta Neuropathol 117(2):101–110
Jobst KA, Smith AD, Szatmari M et al (1994) Rapidly progressing atrophy of medial temporal lobe in Alzheimer’s disease. Lancet 343(8901):829–830
Jost BC, Grossberg GT (1995) The natural history of Alzheimer’s disease: a brain bank study. J Am Geriatr Soc 43(11):1248–1255
Kalaria DL, Cohen DL, Premkumar DRD (1996) Cellular aspects of the inflammatory response in Alzheimer’s disease. Neurodegeneration 5:497–503
Kamal A, Almenar-Queralt A, LeBlanc JF, Roberts EA, Goldstein LS (2001) Kinesin-mediated axonal transport of a membrane compartment containing beta-secretase and presenilin-1 requires APP. Nature 414(6864):643–648
Karlstrom H, Brooks WS, Kwok JB et al (2008) Variable phenotype of Alzheimer’s disease with spastic paraparesis. J Neurochem 104(3):573–583
Kayed R, Sokolov Y, Edmonds B et al (2004) Permeabilization of lipid bilayers is a common conformation-dependent activity of soluble amyloid oligomers in protein misfolding diseases. J Biol Chem 279(45):46363–46366
Keil U, Hauptmann S, Bonert A et al (2006) Mitochondrial dysfunction induced by disease relevant AbetaPP and tau protein mutations. J Alzheimers Dis 9(2):139–146
Khatoon S, Grundke-Iqbal I, Iqbal K (1994) Levels of normal and abnormally phosphorylated tau in different cellular and regional compartments of Alzheimer disease and control brains. FEBS Lett 351(1):80–84
Kim DY, Ingano LA, Kovacs DM (2002) Nectin-1alpha, an immunoglobulin-like receptor involved in the formation of synapses, is a substrate for presenilin/gamma-secretase-like cleavage. J Biol Chem 277(51):49976–49981
Kim HS, Kim EM, Lee JP et al (2003) C-terminal fragments of amyloid precursor protein exert neurotoxicity by inducing glycogen synthase kinase-3beta expression. FASEB J 17(13):1951–1953
Klein WL, Stine WB Jr, Teplow DB (2004) Small assemblies of unmodified amyloid beta-protein are the proximate neurotoxin in Alzheimer’s disease. Neurobiol Aging 25(5):569–580
Kobayashi K, Nakano H, Hayashi M et al (2003) Association of phosphorylation site of tau protein with neuronal apoptosis in Alzheimer’s disease. J Neurol Sci 208(1–2):17–24
Kril J, Hodges J, Halliday G (2004) Relationship between hippocampal volume and CA1 neuron loss in brains of humans with and without Alzheimer’s disease. Neurosci Lett 361(1–3):9–12
Kril J, Patel S, Harding A, Halliday G (2002) Neuron loss from the hippocampus of Alzheimer’s disease exceeds extracellular neurofibrillary tangle formation. Acta Neuropathol 103(4):370–376
Kumar-Singh S, Cras P, Wang R et al (2002) Dense-core senile plaques in the Flemish variant of Alzheimer’s disease are vasocentric. Am J Pathol 161(2):507–520
Kumar-Singh S, Theuns J, Van Broeck B et al (2006) Mean age of onset of familial Alzheimer’s disease caused by presenilin mutations correlates with both increased Abeta42 and decreased Abeta40. Hum Mutat 27(7):686–695
Kurt M, Davies D, Kidd M et al (2001) Neurodegenerative changes associated with beta-amyloid deposition in the brains of mice carrying mutant amyloid precursor protein and mutant presenilin-1 transgenes. Exp Neurol 171:59–71
Kwok JB, Halliday GM, Brooks WS et al (2003) Presenilin-1 mutation L271 V results in altered exon 8 splicing and Alzheimer’s disease with non-cored plaques and no neuritic dystrophy. J Biol Chem 278(9):6748–6754
Lacor PN, Buniel MC, Chang L et al (2004) Synaptic targeting by Alzheimer’s-related amyloid beta oligomers. J Neurosci 24(45):10191–10200
Lacor PN, Buniel MC, Furlow PW et al (2007) Abeta oligomer-induced aberrations in synapse composition, shape, and density provide a molecular basis for loss of connectivity in Alzheimer’s disease. J Neurosci 27(4):796–807
Lai RY, Gertz HN, Wischik DJ et al (1995) Examination of phosphorylated tau protein as a PHF-precursor at early stage Alzheimer’s disease. Neurobiol Aging 16(3):433–445
Lambert MP, Barlow AK, Chromy BA et al (1998) Diffusible, nonfibrillar ligands derived from Abeta1-42 are potent central nervous system neurotoxins. Proc Natl Acad Sci USA 95(11):6448–6453
Lammich S, Okochi M, Takeda M et al (2002) Presenilin-dependent intramembrane proteolysis of CD44 leads to the liberation of its intracellular domain and the secretion of an Abeta-like peptide. J Biol Chem 277(47):44754–44759
Lantos PL, Luthert PJ, Hanger D et al (1992) Familial Alzheimer’s disease with the amyloid precursor protein position 717 mutation and sporadic Alzheimer’s disease have the same cytoskeletal pathology. Neurosci Lett 137(2):221–224
Lazarov O, Morfini GA, Pigino G et al (2007) Impairments in fast axonal transport and motor neuron deficits in transgenic mice expressing familial Alzheimer’s disease-linked mutant presenilin 1. J Neurosci 27(26):7011–7020
Le T, Crook R, Hardy J, Dickson D (2001) Cotton wool plaques in non-familial late-onset Alzheimer’s disease. J Neuropathol Exp Neurol 60(11):1051–1061
Ledesma MD, Avila J, Correas I (1995) Isolation of a phosphorylated soluble tau fraction from Alzheimer’s disease brain. Neurobiol Aging 16(4):515–522
Lewandowska E, Bertrand E, Kulczycki J et al (1999) Microglia and neuritic plaques in familial Alzheimer’s disease induced by a new mutation of presenilin-1 gene. An ultrastructural study. Folia Neuropathol 37(4):243–246
Lin H, Bhatia R, Lal R (2001) Amyloid beta protein forms ion channels: implications for Alzheimer’s disease pathophysiology. FASEB J 15(13):2433–2444
Lippa CF, Saunders AM, Smith TW et al (1996) Familial and sporadic Alzheimer’s disease: neuropathology cannot exclude a final common pathway. Neurology 46:406–412
Lucas JJ, Hernandez F, Gomez-Ramos P et al (2001) Decreased nuclear beta-catenin, tau hyperphosphorylation and neurodegeneration in GSK-3beta conditional transgenic mice. EMBO J 20(1–2):27–39
Lue LF, Kuo YM, Roher AE et al (1999) Soluble amyloid beta peptide concentration as a predictor of synaptic change in Alzheimer’s disease. Am J Pathol 155(3):853–862
Malik B, Currais A, Andres A et al (2008) Loss of neuronal cell cycle control as a mechanism of neurodegeneration in the presenilin-1 Alzheimer’s disease brain. Cell cycle 7(5):637–646
Mandelkow E, von Bergen M, Biernat J, Mandelkow EM (2007) Structural principles of tau and the paired helical filaments of Alzheimer’s disease. Brain Pathol 17(1):83–90
Mann D, Iwatsubo T, Nochlin D et al (1997) Amyloid (Abeta) deposition in chromosome 1-linked Alzheimer’s disease: the Volga German families. Ann Neurol 41(1):52–57
Mann D, Pickering-Brown S, Takeuchi A, Iwatsubo T, F.A.s.D.P.S. Group (2001) Amyloid angiopathy and variability in amyloid B deposition is determined by mutation position in presenilin-1-linked Alzheimer’s disease. Am J Pathol 158(6):2165–2175
Mann D, Takeuchi A, Sato S et al (2001) Cases of Alzheimer’s disease due to deletion of exon 9 of the presenilin-1 gene show an unusual but characteristic B-amyloid pathology known as ‘cotton wool’ plaques. Neuropathol Appl Neurobiol 27:189–196
Mann DM, Iwatsubo T, Cairns NJ et al (1996) Amyloid beta protein (Abeta) deposition in chromosome 14-linked Alzheimer’s disease: predominance of Abeta42(43). Ann Neurol 40:149–156
Mann DMA, Iwatsubo T, Ihara Y et al (1996) Predominant deposition of amyloid-beta(42(43)) in plaques in cases of Alzheimer’s-disease and hereditary cerebral-haemorrhage associated with mutations in the amyloid precursor protein gene. Am J Pathol 148:1257–1266
Marambaud P, Shioi J, Serban G et al (2002) A presenilin-1/gamma-secretase cleavage releases the E-cadherin intracellular domain and regulates disassembly of adherens junctions. EMBO J 21(8):1948–1956
Masliah E, Mallory M, Alford M, Tanaka S, Hansen LA (1998) Caspase dependent DNA fragmentation might be associated with excitotoxicity in Alzheimer disease. J Neuropathol Exp Neurol 57(11):1041–1052
Mattson M, Chan S, Camandola S (2001) Presenilin mutations and calcium signaling defects in the nervous and immune systems. Bioessays 23:733–744
McLean CA, Cherny RA, Fraser FW et al (1999) Soluble pool of Abeta amyloid as a determinant of severity of neurodegeneration in Alzheimer’s disease. Ann Neurol 46(6):860–866
Miklossy J, Taddei K, Suva D et al (2003) Two novel presenilin-1 mutations (Y256S and Q222H) are associated with early-onset Alzheimer’s disease. Neurobiol Aging 24(5):655–662
Miravalle L, Calero M, Takao M et al (2005) Amino-terminally truncated Abeta peptide species are the main component of cotton wool plaques. Biochemistry 44(32):10810–10821
Mirra SS, Heyman A, McKeel D et al (1991) The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41(4):479–486
Moehlmann T, Winkler E, Xia X et al (2002) Presenilin-1 mutations of leucine 166 equally affect the generation of the Notch and APP intracellular domains independent of their effect on Abeta 42 production. Proc Natl Acad Sci USA 99(12):8025–8030
Mukaetova-Ladinska EB, Garcia-Siera F, Hurt J et al (2000) Staging of cytoskeletal and beta-amyloid changes in human isocortex reveals biphasic synaptic protein response during progression of Alzheimer’s disease. Am J Pathol 157(2):623–636
Mukaetova-Ladinska EB, Harrington CR, Roth M, Wischik CM (1993) Biochemical and anatomical redistribution of tau protein in Alzheimer’s disease. Am J Pathol 143:565–578
Muller T, Meyer HE, Egensperger R, Marcus K (2008) The amyloid precursor protein intracellular domain (AICD) as modulator of gene expression, apoptosis, and cytoskeletal dynamics-relevance for Alzheimer’s disease. Prog Neurobiol 85(4):393–406
Munch G, Gasic-Milenkovic J, Dukic-Stefanovic S et al (2003) Microglial activation induces cell death, inhibits neurite outgrowth and causes neurite retraction of differentiated neuroblastoma cells. Exp Brain Res 150(1):1–8
Munch G, Shepherd C, McCann H et al (2002) Intraneuronal advanced glycation endproducts in presenilin-1 Alzheimer’s disease. Neuroreport 13(5):601–604
Murakami D, Okamoto I, Nagano O et al (2003) Presenilin-dependent gamma-secretase activity mediates the intramembranous cleavage of CD44. Oncogene 22(10):1511–1516
Nagele RG, D’Andrea MR, Lee H, Venkataraman V, Wang HY (2003) Astrocytes accumulate A beta 42 and give rise to astrocytic amyloid plaques in Alzheimer disease brains. Brain Res 971(2):197–209
Nagy Z (2000) Cell cycle regulatory failure in neurones: causes and consequences. Neurobiol Aging 21(6):761–769
Nakayama K, Ohkawara T, Hiratochi M, Koh CS, Nagase H (2008) The intracellular domain of amyloid precursor protein induces neuron-specific apoptosis. Neurosci Lett 444(2):127–131
Naslund J, Schierhorn A, Hellman U et al (1994) Relative abundance of Alzheimer A beta amyloid peptide variants in Alzheimer disease and normal aging. Proc Natl Acad Sci USA 91(18):8378–8382
Natte R, Maat-Schieman ML, Haan J et al (2001) Dementia in hereditary cerebral hemorrhage with amyloidosis-Dutch type is associated with cerebral amyloid angiopathy but is independent of plaques and neurofibrillary tangles. Ann Neurol 50(6):765–772
Nilsberth C, Westlind-Danielsson A, Eckman CB et al (2001) The ‘Arctic’ APP mutation (E693G) causes Alzheimer’s disease by enhanced Abeta protofibril formation. Nature Neurosci 4(9):887–893
Nochlin D, Bird TD, Nemens EJ, Ball MJ, Sumi SM (1998) Amyloid angiopathy in a Volga German family with Alzheimer’s disease and a presenilin-2 mutation (N141I). Ann Neurol 43(1):131–135
Nochlin D, van Belle G, Bird TD, Sumi SM (1993) Comparison of the severity of neuropathologic changes in familial and sporadic Alzheimer’s disease. Alzheimer Dis Assoc Disord 7(4):212–222
Nunomura A, Chiba S, Lippa CF et al (2004) Neuronal RNA oxidation is a prominent feature of familial Alzheimer’s disease. Neurobiol Dis 17(1):108–113
Oddo S, Vasilevko V, Caccamo A et al (2006) Reduction of soluble Abeta and tau, but not soluble Abeta alone, ameliorates cognitive decline in transgenic mice with plaques and tangles. J Biol Chem 281(51):39413–39423
Parachikova A, Agadjanyan M, Cribbs D et al (2006) Inflammatory changes parallel the early stages of Alzheimer disease. Neurobiol Aging 28(12):1821–1833
Paradis E, Douillard H, Koutroumanis M, Goodyer C, LeBlanc A (1996) Amyloid beta peptide of Alzheimer’s disease downregulates Bcl-2 and upregulates bax expression in human neurons. J Neurosci 16(23):7533–7539
Paresce D, Chung H, Maxfield F (1997) Slow degradation of aggregates of the Alzheimer’s disease amyloidB-protein by microglial cells. J Biol Chem 272:29390–29397
Park S, Ferriera A (2005) The generation of a 17 kDa neurotoxic fragment: and alternative mechanism by which tau mediates beta-amyloid induced neurodegeneration. J Neurosci 25:5365–5375
Patel N, Paris D, Mathurs V et al (2005) Inflammatory cytokine levels correlate with amyloid load in transgenic mouse models of Alzheimer’s disease. J Neuroinflamm 2(1):9–18
Pigino G, Pelsman A, Mori H, Busciglio J (2001) Presenilin-1 mutations reduce cytoskeletal association, deregulate neurite growth, and potentiate neuronal dystrophy and tau phosphorylation. J Neurosci 21(3):834–842
Piguet O, Double KL, Kril JJ et al (2007) White matter loss in healthy aging: a postmortem analysis. Neurobiol Aging. doi:10.1016/j.neurobiolaging.2007.10.015 [Epub ahead of print]
Raber J, Huang Y, Ashford JW (2004) ApoE genotype accounts for the vast majority of AD risk and AD pathology. Neurobiol Aging 25(5):641–650
Raux G, Gantier R, Thomas-Anterion C et al (2000) Dementia with prominent frontotemporal features associated with L113P presenilin 1 mutation. Neurology 55(10):1577–1578
Rogers J, Luber-Narod J, Styren SD, Civin WH (1988) Expression of immune system-associated antigens by cells of the human central nervous system: relationship to the pathology of Alzheimer’s disease. Neurobiol Aging 9:339–349
Rossi G, Giaccone G, Maletta R et al (2004) A family with Alzheimer disease and strokes associated with A713T mutation of the APP gene. Neurology 63(5):910–912
Rossler M, Zarski R, Bohl J, Ohm TG (2002) Stage-dependent and sector-specific neuronal loss in hippocampus during Alzheimer’s disease. Acta Neuropathol 103(4):363–369
Rossner S, Lange-Dohna C, Zeitschel U, Perez-Polo JR (2005) Alzheimer’s disease beta-secretase BACE1 is not a neuron-specific enzyme. J Neurochem 92(2):226–234
Rossner S, Sastre M, Bourne K, Lichtenthaler SF (2006) Transcriptional and translational regulation of BACE1 expression—implications for Alzheimer’s disease. Prog Neurobiol 79(2):95–111
Rovelet-Lecrux A, Frebourg T, Tuominen H et al (2007) APP locus duplication in a Finnish family with dementia and intracerebral haemorrhage. J Neurol Neurosurg Psychiatry 78(10):1158–1159
Rovelet-Lecrux AHD, Raux G, Le Meur N, Laquerrière A, Vital A, Dumanchin C, Feuillette S, Brice A, Vercelletto M, Dubas F, Frebourg T, Campion D (2006) APP locus duplication causes autosomal dominant early-onset Alzheimer disease with cerebral amyloid angiopathy. Nat Genet 38(1):24–26
Saitoh T, Sundsmo M, Roch JM et al (1989) Secreted form of amyloid beta protein precursor is involved in the growth regulation of fibroblasts. Cell 58(4):615–622
Sastre M, Steiner H, Fuchs K et al (2001) Presenilin-dependent gamma-secretase processing of beta-amyloid precursor protein at a site corresponding to the S3 cleavage of Notch. EMBO Rep 2(9):835–841
Saura CA, Choi SY, Beglopoulos V et al (2004) Loss of presenilin function causes impairments of memory and synaptic plasticity followed by age-dependent neurodegeneration. Neuron 42(1):23–36
Schindowski K, Belarbi K, Buee L (2008) Neurotrophic factors in Alzheimer’s disease: role of axonal transport. Genes Brain Behav 7(1):43–56
Schroeter EH, Ilagan MX, Brunkan AL et al (2003) A presenilin dimer at the core of the gamma-secretase enzyme: insights from parallel analysis of Notch 1 and APP proteolysis. Proc Natl Acad Sci USA 100(22):13075–13080
Selkoe D, Kopan R (2003) Notch and Presenilin: regulated intramembrane proteolysis links development and degeneration. Ann Rev Neurosci 26:565–597
Seubert P, Oltersdorf T, Lee MG et al (1993) Secretion of beta-amyloid precursor protein cleaved at the amino terminus of the beta-amyloid peptide. Nature 361(6409):260–263
Shankar GM, Bloodgood BL, Townsend M et al (2007) Natural oligomers of the Alzheimer amyloid-beta protein induce reversible synapse loss by modulating an NMDA-type glutamate receptor-dependent signaling pathway. J Neurosci 27(11):2866–2875
Sheng JG, Mrak RE, Griffin WS (1997) Neuritic plaque evolution in Alzheimer’s disease is accompanied by transition of activated microglia from primed to enlarged to phagocytic forms. Acta Neuropathol 94(1):1–5
Shepherd C, Grace E, Mann D, Halliday G (2007) Relationship between neuronal loss and ‘inflammatory plaques’ in early onset Alzheimer’s disease. Neuropathol Appl Neurobiol 33(3):328–333
Shepherd C, Gregory G, Vickers J et al (2004) Positional effects of presenilin-1 mutations on tau phosphorylation in cortical plaques. Neurobiol Dis 15(1):115–119
Shepherd CE, Gregory GC, Vickers JC, Halliday GM (2005) Novel ‘inflammatory plaque’ pathology in presenilin-1 Alzheimer’s disease. Neuropathol Appl Neurobiol 31(5):503–511
Shepherd CE, Thiel E, McCann H, Harding TJ, Halliday GM (2000) Cortical Inflammation in Alzheimer’s disease but not dementia with Lewy bodies. Arch Neurol 57:817–822
Shioi J, Georgakopoulos A, Mehta P et al (2007) FAD mutants unable to increase neurotoxic Abeta 42 suggest that mutation effects on neurodegeneration may be independent of effects on Abeta. J Neurochem 101(3):674–681
Shrimpton AE, Schelper RL, Linke RP et al (2007) A presenilin 1 mutation (L420R) in a family with early onset Alzheimer disease, seizures and cotton wool plaques, but not spastic paraparesis. Neuropathology 27(3):228–232
Sisodia SS, Koo EH, Beyreuther K, Unterbeck A, Price DL (1990) Evidence that beta-amyloid protein in Alzheimer’s disease is not derived by normal processing. Science 248(4954):492–495
Smith M, Kwok J, McLean C et al (2001) Variable phenotype of Alzheimer’s disease with spastic paraparesis. Ann Neurol 49(1):125–129
Sokolova A, Hill MD, Rahimi F et al (2008) Monocyte chemoattractant protein-1 plays a dominant role in the chronic inflammation observed in Alzheimer’s disease. Brain Pathol. doi:10.1111/j.1750-3639.2008.00188.x [Epub ahead of print]
Spires T, Orne J, SantaCruz K et al (2006) Region-specific dissociation of neuronal loss and neurofibrillary pathology in a mouse model of tauopathy. Am J Pathol 168(5):1598–1607
Stadelmann C, Deckwerth TL, Srinivasan A et al (1999) Activation of caspase-3 in single neurons and autophagic granules of granulovacuolar degeneration in Alzheimer’s disease. Evidence for apoptotic cell death. Am J Pathol 155(5):1459–1466
Steiner H, Revesz T, Neumann M et al (2001) A pathogenic presenilin-1 deletion causes abberant AB42 production in the absence of congiophilic amyloid plaques. J Biol Chem 276(10):7233–7239
Stenh C, Nilsberth C, Hammarback J et al (2002) The Arctic mutation interferes with processing of the amyloid precursor protein. Neuroreport 13(15):1857–1860
Stoothoff WH, Johnson GV (2005) Tau phosphorylation: physiological and pathological consequences. Biochem Biophys Acta 1739(2–3):280–297
Su JH, Anderson AJ, Cummings BJ, Cotman CW (1994) Immunohistochemical evidence for apoptosis in Alzheimer’s disease. Neuroreport 5(18):2529–2533
Su JH, Deng G, Cotman CW (1997) Bax protein expression is increased in Alzheimer’s brain: correlations with DNA damage, Bcl-2 expression, and brain pathology. J Neuropathol Exp Neurol 56(1):86–93
Sudo S, Shiozawa M, Cairns N, Wada Y (2005) Aberrant accentuation of neurofibrillary degeneration in the hippocampus of Alzheimer’s disease with amyloid precursor protein 717 and presenilin-1 gene mutations. J Neurol Sci 234(1–2):55–65
Takao M, Ghetti B, Hayakawa I et al (2002) A novel mutation (G217D) in the Presenilin 1 gene (PSEN1) in a Japanese family: presenile dementia and parkinsonism are associated with cotton wool plaques in the cortex and striatum. Acta Neuropathol 104(2):155–170
Takashima A, Murayama M, Murayama O et al (1998) Presenilin 1 associates with glycogen synthase kinase-3beta and its substrate tau. Proc Natl Acad Sci USA 95(16):9637–9641
Tamaoka A, Fraser PE, Ishii K et al (1998) Amyloid-beta-protein isoforms in brain of subjects with PS1-linked, beta APP-linked and sporadic Alzheimer disease. Brain Res Mol Brain Res 56(1–2):178–185
Tamaoka A, Odaka A, Ishibashi Y et al (1994) APP717 missense mutation affects the ratio of amyloid beta protein species (A beta 1-42/43 and a beta 1-40) in familial Alzheimer’s disease brain. J Biol Chem 269(52):32721–32724
Tamaoka A, Sawamura N, Odaka A et al (1995) Amyloid beta protein 1-42/43 (A beta 1-42/43) in cerebellar diffuse plaques: enzyme-linked immunosorbent assay and immunocytochemical study. Brain Res 679(1):151–156
Thaker U, McDonagh A, Iwatsubo T et al (2003) Tau load is associated with apolipoprotein E genotype and the amount of amyloid B protein, AB40, in sporadic and familial Alzheimer’s disease. Neuropathol Appl Neurobiol 29:35–44
Thal DR, Arendt T, Waldmann G et al (1998) Progression of neurofibrillary changes and PHF-tau in end-stage Alzheimer’s disease is different from plaque and cortical microglial pathology. Neurobiol Aging 19(6):517–525
Thinakaran G, Parent AT (2004) Identification of the role of presenilins beyond Alzheimer’s disease. Pharmacol Res 50(4):411–418
Turner PR, O’Connor K, Tate WP, Abraham WC (2003) Roles of amyloid precursor protein and its fragments in regulating neural activity, plasticity and memory. Prog Neurobiol 70(1):1–32
Uchihara T, Nakamura A, Nakayama H et al (2003) Triple immunofluorolabeling with two rabbit polyclonal antibodies and a mouse monoclonal antibody allowing three-dimensional analysis of cotton wool plaques in Alzheimer disease. J Histochem Cytochem 51(9):1201–1206
van de Nes JA, Nafe R, Schlote W (2008) Non-tau based neuronal degeneration in Alzheimer’s disease—an immunocytochemical and quantitative study in the supragranular layers of the middle temporal neocortex. Brain Res 1213:152–165
Van Nostrand WE, Melchor JP, Cho HS, Greenberg SM, Rebeck GW (2001) Pathogenic effects of D23 N Iowa mutant amyloid beta-protein. J Biol Chem 276(35):32860–32866
Verdile G, Gnjec A, Miklossy J et al (2004) Protein markers for Alzheimer disease in the frontal cortex and cerebellum. Neurology 63(8):1385–1392
Verkkoniemi A, Kalimo H, Paetau A et al (2001) Variant Alzheimer disease with spastic paraparesis: neuropathological phenotype. J Neuropathol Exp Neurol 60(5):483–492
von Bernhardi R (2007) Glial cell dysregulation: a new perspective on Alzheimer disease. Neurotox Res 12(4):215–232
Walker ES, Martinez M, Brunkan AL, Goate A (2005) Presenilin 2 familial Alzheimer’s disease mutations result in partial loss of function and dramatic changes in Abeta 42/40 ratios. J Neurochem 92(2):294–301
Walsh DM, Klyubin I, Fadeeva JV et al (2002) Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature 416(6880):535–539
Walsh DM, Lomakin A, Benedek GB, Condron MM, Teplow DB (1997) Amyloid beta-protein fibrillogenesis. Detection of a protofibrillar intermediate. J Biol Chem 272(35):22364–22372
Wang H, Pasternak J, Kuo H et al (2002) Soluble oligomers of beta amyloid (1-42) inhibit long-term potentiation but not long-term depression in rat dentate gyrus. Brain Res 924(2):133–140
Weaver CL, Espinoza M, Kress Y, Davies P (2000) Conformational change as one of the earliest alterations of tau in Alzheimer’s disease. Neurobiol Aging 21(5):719–727
Whitmer RA, Gunderson EP, Barrett-Connor E, Quesenberry CP Jr, Yaffe K (2005) Obesity in middle age and future risk of dementia: a 27 year longitudinal population based study. Br Med J 330(7504):1360
Whitmer RA, Gunderson EP, Quesenberry CP Jr, Zhou J, Yaffe K (2007) Body mass index in midlife and risk of Alzheimer disease and vascular dementia. Curr Alzheimer Res 4(2):103–109
Whitmer RA, Gustafson DR, Barrett-Connor E et al (2008) Central obesity and increased risk of dementia more than three decades later. Neurology 71(14):1057–1064
Whitwell JL, Shiung MM, Przybelski SA et al (2008) MRI patterns of atrophy associated with progression to AD in amnestic mild cognitive impairment. Neurology 70(7):512–520
Wimo A, Jonsson L, Winblad B (2006) An estimate of the worldwide prevalence, direct costs of dementia in 2003. Dement Geriatr Cogn Disord 21(3):175–181
Wischik CM, Edwards PC, Lai RY et al (1995) Quantitative analysis of tau protein in paired helical filament preparations: implications for the role of tau protein phosphorylation in PHF assembly in Alzheimer’s disease. Neurobiol Aging 16(3):409–417
Wolfe MS (2007) When loss is gain: reduced presenilin proteolytic function leads to increased Abeta42/Abeta40. Talking point on the role of presenilin mutations in Alzheimer disease. EMBO Rep 8(2):136–140
Woltjer RL, Cimino PJ, Boutte AM et al (2005) Proteomic determination of widespread detergent-insolubility including Abeta but not tau early in the pathogenesis of Alzheimer’s disease. FASEB J 19(13):1923–1925
Woodhouse A, Shepherd C, Sokolova A et al (2008) Cytoskeletal alterations differentiate presenilin-1 and sporadic Alzheimer’s disease. Acta Neuropathol 117(1):19–29
Wyss-Coray T (2006) Inflammation in Alzheimer disease: driving force, bystander or beneficial response. Nat Med 12(9):1005–1015
Xu M, Lai MT, Huang Q et al (2002) Gamma-secretase: characterization and implication for Alzheimer disease therapy. Neurobiol Aging 23(6):1023–1030
Yang Y, Geldmacher DS, Herrup K (2001) DNA replication precedes neuronal cell death in Alzheimer’s disease. J Neurosci 21(8):2661–2668
Yokota O, Terada S, Ishizu H et al (2003) Variability and heterogeneity in Alzheimer’s disease with cotton wool plaques: a clinicopathological study of four autopsy cases. Acta Neuropathol 106(4):348–356
Zhao G, Mao G, Tan J et al (2004) Identification of a new presenilin-dependent zeta-cleavage site within the transmembrane domain of amyloid precursor protein. J Biol Chem 279(49):50647–50650
Acknowledgments
We wish to thank Heidi Cartwright for the figure work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shepherd, C., McCann, H. & Halliday, G.M. Variations in the neuropathology of familial Alzheimer’s disease. Acta Neuropathol 118, 37–52 (2009). https://doi.org/10.1007/s00401-009-0521-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-009-0521-4