Abstract
Previously we have employed antibodies to the tight junction (TJ)-associated proteins ZO-1 and occludin to describe endothelial tight junction abnormalities, in lesional and normal appearing white matter, in primary and secondary progressive multiple sclerosis (MS). This work is extended here by use of antibodies to the independent TJ-specific proteins and junctional adhesion molecule A & B (JAM-A, JAM-B). We have also assessed the expression in MS of β-catenin, a protein specific to the TJ-associated adherens junction. Immunocytochemistry and semiquantitative confocal microscopy for JAM-A and β-catenin was performed on snap-frozen sections from MS cases (n = 11) and controls (n = 6). Data on 1,443 blood vessels was acquired from active lesions (n = 13), inactive lesions (n = 13), NAWM (n = 20) and control white matter (n = 13). In MS abnormal JAM-A expression was found in active (46%) and inactive lesions (21%), comparable to previous data using ZO-1. However, a lower level of TJ abnormality was found in MS NAWM using JAM-A (3%) compared to ZO-1 (13%). JAM-B was strongly expressed on a small number of large blood vessels in control and MS tissues but at too low a level for quantitative analysis. By comparison with the high levels of abnormality observed with the TJ proteins, the adherens junction protein β-catenin was normally expressed in all MS and control tissue categories. These results confirm, by use of the independent marker JAM-A, that TJ abnormalities are most frequent in active white matter lesions. Altered expression of JAM-A, in addition to affecting junctional tightness may also both reflect and affect leukocyte trafficking, with implications for immune status within the diseased CNS. Conversely, the adherens junction component of the TJ, as indicated by β-catenin expression is normally expressed in all MS and control tissue categories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple Sclerosis is a primary demyelinating inflammatory disease of the central nervous system [57]. The pathogenic events in MS are not fully understood and the cause is unknown; pathological hallmarks include inflammation, formation of demyelinated plaques and neurodegeneration. Lesions are often centred on blood vessels and from an early stage these become inflamed and leaky [23]. Indeed, some of the earliest cerebrovascular abnormalities in MS brain include BBB dysregulation, an increase in inflammatory mediators and transendothelial migration [1, 40]. Moreover, transient or persistent loss of blood–brain barrier (BBB) integrity, as indicated by vascular leak and disruption of tight junctions, has been clearly demonstrated in active and inactive lesions in both primary and secondary progressive MS [17, 25, 29, 47]. Finally, both MRI and confocal microscopic studies point to BBB disturbance in MS normal-appearing white matter [NAWM; 13, 37, 47, 58]. The events which lead to the initial disruption of the BBB in MS are not yet fully elucidated but appear to be intimately linked to this inflammatory cell infiltration into the CNS [12].
The link between inflammatory infiltration and BBB damage is not entirely straightforward; however, there are contradictory reports on the effects of leukocyte diapedesis on BBB tight junctions. Although many reports link inflammation to barrier damage and leak [7, 62], recent experimental studies confirm the presence and likely importance of a long-suspected transcellular route for diapedesis of leukocytes which does not involve paracellular passage [9, 60]. In a model of EAE which showed this mechanism, the ultrastructure of tight junctions remained normal during mononuclear cell diapedesis [60]. Moreover all observations of this route, including our own in an experimental viral model (unpublished observations), suggest that the passage of an individual leukocyte involves minimal disruption to endothelial integrity. These findings if confirmed by more direct assessment of the state of the key tight junctional proteins may imply that at least, where the flux of cells is not too great, the process of inflammatory cell diapedesis need not necessarily cause either detectable junctional disruption or significant leak.
However, not all CNS inflammation is so benign in effect. In some models of EAE, BBB disruption and permeability increase can be induced by T-cells [38] or monocytes [41] and occurs in the presence of increased expression of inflammatory cytokines. Similarly in experimental autoimmune uveoretinitis, transient loss of tight junction protein in retinal venules was seen to accompany leukocyte adhesion and migration in an ex vivo retinal whole-mount study [62]. The widespread occurrence of both disrupted tight junctions and leak in MS suggests that the inflammation in our long term MS autopsy cases differs from that seen in Wolburg’s recently described EAE model. Thus the BBB pathology extended far beyond the inflamed vessels which might currently have been involved in diapedesis. Two factors which may account for the difference by creating an unfavourable chemical milieu are (a) the chronic, lingering nature of inflammation in MS and (b) the effect of parenchymal and perivascular microglial activation, which in MS is a major component of the inflammatory pathology. Additionally, the sheer weight of current and past pathology in the MS brain may adversely affect barrier integrity, as for example where perivascular astrocytes have been displaced by macrophages during acute inflammation [24].
In MS, inflammatory cell infiltration at the BBB, accompanied by the local and diffuse generation of pro-inflammatory cytokines, such as TNF-α, IL-1B and interferon-γ appears to play a principal role in demyelination and lesion formation [40]. Elevations in these BBB mediators have also been found in cerebrospinal fluid taken from MS patients [55] and MRI studies show a compromised barrier prior to clinical symptoms [23, 27].
The BBB itself is composed mainly of tight (TJ) junctions present between adjacent endothelial cells that act to prevent paracellular diffusion into the brain and to maintain the important functional polarity of the barrier endothelium [50]. There are important structural distinctions in the arrangement of epithelial and endothelial tight junctions. In the epithelial junctional complex, adherens junctions (AJ) and TJs are spatially separate with the AJs located near the basolateral side, between adjacent epithelial cells. AJs consist mainly of cadherin proteins, members of a superfamily involved in cell–cell adhesion, all of which are single transmembrane domain proteins. The calcium-dependent cadherin receptors are linked to the actin cytoskeleton at the adherens junctions by alpha or β-catenin [8, 63]. β-Catenin, a 92 kDa protein, is important in both cell adhesion and transcriptional activation through the Wnt signaling pathway [20, 53, 64]. Loss of equilibrium between β-catenin and E-cadherin has been implicated in the development of tumours arising from non-intestinal epithelia [19]. In barrier endothelium, however, the ‘adherens’ junctions are not physically separated from the tight junctions. Rather its components are intermingled and more closely integrated with the molecules which comprise the tight junctions [52].
The TJs are found as parallel bands of tight apposition towards the apical side of the lateral membrane contacts (clefts) between adjacent endothelial cells. Its main functions are to restrict the paracellular passage of molecules through the BBB and to maintain endothelial polarity [25]. This enables the endothelial cells to maintain differential expression of various membrane transporter molecules which act to tightly regulate the entry and exit of materials to/from the sensitive CNS parenchyma. TJ proteins include claudins, occludin, the zonula occludens (ZO) proteins ZO-1, ZO-2 and ZO-3 and junctional adhesion molecules (JAMs). Compromised BBB tight junctions are recognised as hallmarks of neuroinflammatory and other CNS diseases. Dysfunctional tight junctions and impaired endothelial function possibly allow more cells and immunologically active molecules access to the privileged CNS, thus amplifying inflammation and parenchymal damage states [46].
JAMS are glycoproteins containing two extracellular immunoglobulin folds. Currently JAM-A, B and C have been identified and shown to be present at cell-to-cell contacts and specifically enriched at tight junctions. Studies have identified that JAM proteins are important in many cellular processes, including tight junction assembly and function, leukocyte transmigration, platelet activation, angiogenesis [2, 22, 31, 42, 59] and virus binding [4, 34]. Though closely related, the JAMs have varying functions and localisation.
JAM-A, also known as platelet adhesion molecule 1 (PAM-1), localises to intercellular junctions of polarised endothelial and epithelial cells but is also expressed on leukocytes, neutrophils, monocytes, erythrocytes and platelets [5, 32, 44, 56]. JAM-B, also known as vascular endothelial junction-associated molecule (VE-JAM), has a more restricted distribution. It is prominently expressed on high endothelial venules but is also present on the endothelial of other vessels [45]. High endothelial venules are specialised sites along vessels in the lymph tissue where lymphocytes migrate from the circulating blood system to the lymphoid organs and due to this function are generally leaky, unlike the tight junctions in the BBB [15]. JAMs expression and their ability to bind many ligands in either a homophilic or a heterophilic manner indicate a role for JAMs in tight junction stability and possibly leukocyte transmigration and cell activation [5].
We have previously completed a series of post mortem studies which revealed aspects of tight junction pathology, as revealed principally by ZO-1 immunocytochemistry, in primary and secondary progressive MS and in various control CNS tissues [25, 29, 47]. The highest frequency of disruption was present in active MS lesions but was also apparent in inactive lesions and in normal appearing white matter (NAWM). The main objective of the present study is to determine whether the independent TJ proteins JAM-A and JAM-B are also affected in MS. Furthermore, we have also examined for the first time expression of β-catenin, a prominent component of the ‘adherens’ component of blood–brain barrier junctions, in MS.
Materials and methods
Brain tissue samples and characterisation
Case selection was retrospective on the basis of a confirmed clinical and neuropathological diagnosis of MS. Snap-frozen MS and control tissue samples were available from the National MS Brain Bank at Charing Cross Hospital, London (registered charity No. 207495). Informed consent for research for all brain tissues and local ethical approval for the conduct of this study was obtained. The tissue used in the study encompasses different MS lesions (active and inactive) and MS normal appearing white matter (NAWM) and has been compared with white matter from healthy controls. In total tissue was available from 11 MS patients all of whom were diagnosed with either primary or secondary progressive MS. Tissues from six control cases contained no CNS neuropathology or inflammatory plaques. The demographic and clinical data of this MS and control case set has been previously published [29].
Cryostat sections (12 μm) from all tissue blocks were cut onto (APES)-coated slides for tissue characterisation with haematoxylin and eosin (H&E), oil-red O (ORO), HLA-Dr and MOG immunocytochemistry as previously described [29]. MS tissue blocks were characterised as containing active or inactive plaques or as normal appearing white matter as previously described [47].
Immunofluoresence
Cryostat sections were fixed in ice-cold acetone for 10 min, allowed to air dry, then incubate overnight at 4°C with polyclonal antibodies to ZO-1 (Zymed, PAD No. Z-R1; 1:200) and JAM-A (Zymed, PAD No. ZMD.275; 1:200) and monoclonal antibodies to JAM-B (R&D systems, clone number 156624; 1:100) and β-catenin (Novocastra, clone 17C2; 1:100). Immunofluoresence staining was also carried out with biotinylated Ulex (Vector, 1:500) to assess the integrity of the cerebral endothelium. After appropriate washes in PBS monoclonals were detected by incubation for 1 h at 37°C in anti-mouse -alexa 488 or -alexa 568 secondary antibodies (Molecular Probes, 1:500). Polyclonal antibodies were visualised with anti-rabbit -alexa 488 (Molecular Probes, 1:500). Sections stained with B. Ulex were detected with streptavidin-Alexa 488. Sections were counterstained with propidium iodide and mounted in citifluor. All fluorescence staining was assessed under 400× magnification on a Leica SP2 confocal microscope equipped with a krypton–argon laser.
Assessment of staining
Confocal microscopic images at 400× were acquired from samples of all tissue categories (control white matter, MS NAWM, active and inactive plaque) until approximately 25 discrete blood vessels were available from each sample. Tight junction (ZO-1, JAM-A) or adherens junction (β-catenin) status at blood vessels was scored as 0 = no disruption, 1 = more than 25% disruption. Tight junction abnormality was judged in comparison to the continuous, linear expression observed in most control brain or in many normal MS vessels. A pilot series of blood vessels was used as a training set to ensure that consensus agreement in the scoring of abnormalities was reached between two independent observers in the majority of blood vessels. Such a method of consensus learning where inter-observer reliability was high, allowed the remaining series of images to be analysed by a single observer. Any expression of the molecules in the tissue parenchyma was also noted. JAM-B expression was much less abundant and only general observations were possible. Results from analysis of JAM-A expression were tabulated, graphed and statistically analysed using Prism 4 software. The non-parametric ANOVA Kruskal–Wallis test was used to analyse significance of differences between the group means.
Results
Tissue characterisation
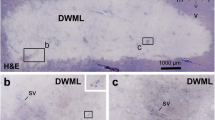
A set of snap-frozen tissue blocks from 11 MS autopsy cases from the UK multiple sclerosis tissue bank in London were screened by H&E, ORO, HLA-Dr and MOG to characterise the pathological state of individual blocks for use in the study. A typical example of a section from a cryostat block that contains an active plaque is shown in Fig. 1a. Such ORO-positive areas were present in 13 blocks examined (Fig. 1b). A further 13 ORO-negative blocks with plaque were classified as inactive (Fig. 1 c). Twenty areas of MS NAWM were examined from blocks with lesions or in blocks containing lesions, from areas greater than 1 cm from the lesion edge. Thirteen areas of control white matter were also characterised from six normal cases.
Histological, immunoperoxidase and immunofluoresence labelling of snap-frozen MS autopsy tissues in multiple sclerosis: immunofluoresence sections were counterstained with DAPI (fluorescence microscopy) or with propidium iodide (confocal microscopy). a Whole cryostat section containing ORO-positive active MS lesion. b Centre of active lesion; ORO is strongly positive. c Inactive lesion centre; ORO negative. d Active lesion edge; MOG immunoreactivity on myelin sheaths while depleted is still present in the lesion. Insert shows the entire section containing the active lesion. e Active white matter lesion; abundant HLA-Dr immunoreactivity. f Inactive white matter lesion; relatively little HLA-Dr immunoreactivity. g Edge of inactive white matter lesion; ulex demonstrates endothelial integrity. h Active white matter lesion in PPMS; ulex. i–n Projected images from confocal data sets. Single fluorescent labelling with alexa-488 (green). i NAWM in MS; multiple, continuous, linear ZO-1 reactivity marks normal tight junctions of blood–brain barrier. j–k NAWM in MS; continuous but more diffuse expression of JAM-A along the vessel walls. l–n Active white matter lesions in MS: vessels with pronounced abnormalities of JAM-A expression (arrows) are present in all fields. Note also the high density of stained vessels in m. Scale bars 2 mm in a; 50 μm in b and c; 1 mm in d; 25 μm in e–h; 17 μm in i–l
Inactive plaques were invariably negative for MOG except for occasional areas of intact myelin sheaths or MOG-positive oligodendrocytes at the plaque edge. More pronounced areas of MOG-positive myelin sheaths were present throughout the actively demyelinating lesions (Fig. 1d). High densities of HLA-Dr-positive cells were present in all active lesions examined (Fig. 1e), and at the edge of some of the inactive lesions. In control white matter and MS NAWM HLA-Dr activity was variable ranging from few (Fig. 1f) to abundant positive cells per microscopic field. All blood vessels in MS and control tissue categories showed uniform endothelial integrity as indicated by normal immunostaining for Ulex (Fig. 1g, h).
Expression of junctional adhesion molecules
As in our previous studies the tight junction associated protein ZO-1 showed high levels of abnormalities in active lesions. The present study revealed that a similar level of abnormality also affects the independent tight junction protein JAM-A. Direct comparison on serial sections of ZO-1 and JAM-A revealed that ZO-1 produces a clearly defined, intense, sharp staining of normal vessels (Fig. 1i). JAM-A staining while continuous is less intense and more diffuse in individual vessels (Fig. 1j, k). Despite the less intense immunofluoresence signals obtained using a polyclonal antibody to JAM-A it was still possible to assess normal from abnormal expression in individual blood vessels.
JAM-A expression was studied in 328 blood vessels from 13 areas of normal control white matter, 427 vessels from 20 areas of MS NAWM, 330 vessels from 13 inactive lesions and 358 vessels from 13 active lesions. Our staining protocols and method of data collection did not allow us to fully classify the vessels into arteries, capillaries and veins. As in our previous publication on TJ abnormalities in MS [25], however, we found that the abnormalities of JAM-A expression affected all calibers of vessels ranging from capillaries ≤10 μm to large vessels >50 μm to a more or less equal extent. JAM-A abnormalities were recognised as interruption or loss of staining or reduced clarity of expression with distinctive intra-parenchymal staining adjacent to blood vessels (Fig. 1l, m, n). In some such areas there was an unusually high density of stained vessels (Fig. 1m).
Statistical analysis of the incidence of TJ abnormalities in the four tissue categories as indicated by expression of JAM-A was highly significant using the Kruskal–Wallis test, indicating that there were differences in the group medians (Fig. 2). The incidence of abnormality in the active plaques (46%) was significantly higher than in either normal controls (4%; P < 0.01) or in MS NAWM (3%; P < 0.001). The difference in TJ incidence of abnormality between inactive lesions (21%) and either control white matter or MS NAWM while pronounced did not achieve statistical significance. Abnormalities in JAM-A expression were observed across a full range of vessel sizes from small capillaries of <10 μm diameter to large vessels of >50 μm diameter. Within the tissue categories variation in the incidence of JAM-A abnormalities is similar, irrespective of vessel size.
Comparison amongst MS tissue categories of the incidence of vessels showing abnormal junctional adhesion molecule-A expression. Data is the mean percentage of assessed vessels rated ‘abnormal’. Columns show mean + SEM. Significant difference of abnormality in active lesions from controls and NAWM (* P < 0.001) are indicated. bv blood vessels
Analysis of JAM-B expression was also carried out on the same series of tissue blocks. Expression was at a level too low to perform quantitative analysis. In control white matter and MS NAWM JAM-B was only expressed on a small number of large blood vessels (Fig. 3a). In three of the active plaques and two of the inactive plaques examined a slight increase in the number of blood vessels with JAM-B expression was observed (Fig. 3b). Furthermore in a small number of high power fields, in two active lesions and at the active edge of two of the inactive lesions, a high level of JAM-B expression was present on cells in the tissue parenchyma. These cells had the morphological appearance of inflammatory lymphocytes (Fig. 3c).
Immunofluoresence labelling of snap-frozen control and MS autopsy tissues in multiple sclerosis: immunofluoresence sections were counterstained with propidium iodide. a Control white matter; discontinuous JAM-B expression on large blood vessel. b Active MS lesion; JAM-B expression is observed on three blood vessels in this field. c Edge of inactive lesion; expression of JAM-B on cells in the tissue parenchyma. d–f β-Catenin is uniformly expressed along blood vessels in d control white matter. e Inactive lesion and f active lesion. In both lesion types a low level of expression of β-catenin is also present in the tissue parenchyma. Scale bars 17 μm in a–f
Expression of adherens proteins
The expression of the adherence junction molecule β-catenin was also studied in the same set of MS and control tissue blocks. Unlike the tight junction proteins, ZO1 and JAM-A, where frequent abnormalities were observed, comparatively uniform expression of β-catenin was present in cerebral vessels of all sizes from all tissue categories examined (Fig. 3d–f). Increased β-catenin was occasionally observed on cells with the morphological characteristics of astrocytes in the parenchyma surrounding cerebral vessels. This was most apparent in areas of active plaque (Fig. 3f).
Discussion
In the present study, we have confirmed, using an independent primary tight junctional molecule JAM-A, that the blood–brain barrier is persistently impaired in MS. In keeping with our previous studies [25, 29], TJ abnormalities were most common in active lesions but also occur to a lesser extent in inactive lesions. The observed expression of JAM-A in the tight junctions of human cerebral endothelium, in a localisation pattern identical with that of ZO-1, is comparative to the co-localisation of both these proteins in rabbit corneal endothelium [35]. The immunofluorescent signals of JAM-A expression were not as clearly defined as those of ZO-1. For this reason we adopted a cautious approach to assessment by only describing abnormal expression if over 25% of the blood vessel profile was disrupted.
Knowledge of the role of JAM-A in cell adhesion and TJ formation arises from evidence of JAMs homophilic interactions. During TJ formation in epithelial cell monolayers, antibodies against JAM-A significantly delay the recovery of transepithelial electrical resistance [30, 32]. In Chinese hamster ovary cells expression of JAM-A at the apical face of the tight junction complex causes reduced paracellular permeability [36]. Jam-A appears to function differently from both occludin and the claudins. When ectopically expressed in fibroblasts, claudins induce TJ strand formation and occludin is incorporated into these strands [14]. However, in the same system JAM-A, ectopically expressed does not induce the formation of TJ strands [21]. JAM-A has been shown to bind to the β2-integrin leukocyte function associated antigen-1 (LFA-1), supporting a role in T-cell and neutrophil transendothelial migration [43]. In the context of MS it is important to note that LFA-1 on leukocyte subsets also binds to endothelial intercellular adhesion molecules (ICAMs) for adhesion [18]. Elevated levels of ICAM-1 are a feature of the microvasculature adjacent to demyelinating lesions in MS [6, 10] and pro-inflammatory cytokines, present in MS lesions [61], such as TNF-α and INF-γ are involved in upregulation of ICAM-1 and VCAM-1.
It is likely that cellular infiltration and cytokine expression, especially TNF-α and INF-γ, contribute to JAM-A abnormalities in MS. Furthermore, it has been suggested that prior relocalisation is needed for interaction of JAM-A with LFA-1 [11, 43]. In the present study the highest level of JAM-A disruption was present in active lesions with pronounced expression present in the tissue parenchyma. The absence of parenchymal expression in samples from inactive lesions is probably due to the relative absence in these burnt out lesions of infiltrating leukocytes or macrophages, cell types known to express JAM-A. However, the consistently reduced TJ protein expression (both ZO-1 and JAM-A) in inactive lesions suggests a persistent low amplitude leakage BBB defect and probable leak that could hinder both vascular and neural repair mechanisms within lesions.
An additional factor complicating interpretation is the increased density of blood vessels seen in some active lesions where JAM-A expression was high but disorganised. Inflammatory mediators, present in active phases of MS include the pro-angiogenic vascular endothelial growth factor [VEGF; 49]. A higher density of vascular profiles in inactive lesions than in NAWM has previously been observed in MS [28]. Although tissue shrinkage and atrophy may contribute to this, VEGF-induced angiogenesis, occurring in active may also be involved [26, 28]. Despite these speculations there is no published pathological evidence regarding either the extent of new vessel formation in MS, or its possible contribution to junctional abnormality and vascular leak. It should be noted however that such vessels in brain diseases typically fail to establish an effective barrier phenotype [16].
The lack of expression of JAM-B in barrier blood vessels in control and non-lesional MS tissue is supported by a study of tight junction expression in frozen tissue samples from grey matter, cortex and white matter derived from fetuses and premature infants [3]. The primary endothelial TJ molecules, including claudin-5, occludin and JAM-A were expressed as early as 16 weeks gestation but JAM-B and JAM-C were not expressed at any gestation time point. Also, in a study of rodent brain sections JAM-B was not expressed on the brain–blood vessels [2].
In three active MS lesions JAM-B was expressed on a greater number of blood vessels suggesting up-regulation at the most immunologically active sites. However, expression of JAM-B was also occasionally found on inflammatory cells in the parenchyma at the edge of two of inactive lesions. It has been reported that endothelial cells in chronic inflammatory diseases, such as rheumatoid arthritis, can be activated to phenotypically resemble high endothelial venules [15]. Such blood vessels are more likely to be involved in leukocyte recruitment into the inflamed tissue [39, 51]. JAM-B mRNA expression has also shown to be associated with sites of inflammation in lung and kidney tissues. Furthermore, within primary neoplasms JAM-B expression was only observed in vessels within or adjacent to the tumour; normal tissue did not show expression [31]. At these sites it is thought to act as ligand for T, NK and dendritic cells through JAM-C and may therefore be involved in the process of T lymphocyte, NK cell and dendritic cell trafficking and recruitment to sites of inflammation. It is of interest that in MS tissue samples that we and others have previously shown that small numbers of dendritic cells are present within perivascular cuffs in active lesions [48, 54]. An increased expression of JAM-B, if only at the surface of a few blood vessels in active lesions, may contribute to this migration of the most potent antigen-presenting cells.
β-Catenin can play different roles in the cell, both as a structural protein at cell–cell adherens junctions, as an anchor for the actin cytoskeleton and as a transcriptional signalling molecule [19, 64]. Its role in the development of tumours has been extensively studied but we are unaware of any other studies of its expression in MS tissue samples. In contrast to the variable level of expression of the TJ specific proteins ZO-1 and JAM-A, β-catenin was uniformly expressed on all sizes of blood vessels in all MS and control tissue categories. In both active and inactive lesions a low level of β-catenin expression was also apparent on cells with the appearance of astrocytes in the tissue parenchyma. Such parenchymal expression is possibly due to the transcriptional activity of β-catenin in the cells present in the parenchyma. It is of interest to note that Chlamydia pneumoniae, an organism that has been associated with multiple sclerosis, has the effect of increasing β-catenin expression on cultured human brain microvascular endothelial cells [33].
The present study supports our earlier suggestion that TJ pathology is an important factor both in new lesion formation and in contributing to the persistent low amplitude leakage associated with long-term inactive lesions [25, 29, 47]. The resultant increased vascular permeability both in lesion and non-lesional white matter is likely to impair homeostasis behind the blood–brain barrier that affects disease progression and repair. Furthermore, we have shown using antibody to β-catenin, that there is no detectable disruption of the closely associated ‘adherens’ component of the interendothelial junctional complex in any of the MS tissue categories studied.
The results of this and previous studies are consistent with the occurrence in MS brain vessels of pathologically-induced deviations from the normal barrier status in respect of key TJ molecular components. The present work which demonstrates focal abnormalities in JAM-A expression suggests the additional possibility that mechanisms and patterns of leukocyte trafficking including dendritic cell entry into the brain may also be focally affected in established MS. This may have effects on the nature and pattern of subsequent leukocyte trafficking and immunological upregulation.
References
Abbott NJ (2000) Inflammatory mediators and modulation of blood–brain barrier permeability. Cell Mol Neurobiol 20:131–147
Aurrand-Lions M, Duncan L, Ballestrem C, Imhof BA (2001) JAM-2, a novel immunoglobulin superfamily molecule, expressed by endothelial and lymphatic cells. J Biol Chem 276:2733–2741
Ballabh P, Furong HU, Kumarasiri M, Braun A, Nedergaard M (2005) Development of tight junction molecules in blood vessels of germinal matrix, cerebral cortex and white matter. Pediatr Res 58:791–798
Barton ES, Forrest JC, Connolly JL, Chappell JD, Liu Y, Schnell FJ, Nusrat A, Parkos CA, Dermody TS (2001) Junction adhesion molecule is a receptor for reovirus. Cell 104:441–451
Bazzoni G (2000) Interaction of junctional adhesion molecule with the tight junction components ZO-1, cingulin, and occludin. J Biol Chem 275:20520–20526
Bo L, Peterson JW, Mork S, Hoffman PA, Gallatin WM, Ransohoff RM, Trapp BD (1996) Distribution of immunoglobulin superfamily members ICAM-1, -2, -3, and the beta 2 integrin LFA-1 in multiple sclerosis lesions. J Neuropathol Exp Neurol 55:1060–1072
Bolton SJ, Anthony DC, Perry VH (1998) Loss of the tight junction proteins occludin and zonula occludens-1 from the cerebral vascular endothelium during neutrophill-induced blood–brain barrier breakdown in vivo. Neuroscience 86:1245–1257
Braga VM, Del Maschio A, Machesky L, Dejana E (1999) Regulation of cadherin function by Rho and Rac: modulation by junction maturation and cellular context. Mol Biol Cell 10:9–22
Carman CV, Springer TA (2004) A transmigratory cup in leukocyte diapedesis both through individual vascular endothelial cells and between them. J Cell Biol 167:377–388
Dore-Duffy P, Washington R, Dragovic L (1993) Expression of endothelial cell activation antigens in microvessels from patients with multiple sclerosis. Adv Exp Med Biol 331:243–248
Ebnet K, Suzuki A, Ohno S, Vestweber D (2004) Junctional adhesion molecules (JAMs): more molecules with dual functions. J Cell Sci 117:19–29
Estes ML, Rudick RA, Barnett GH, Ransohoff RM (1990) Stereotactic biopsy of an active multiple sclerosis lesion. Immunocytochemical analysis and neuropathologic correlation with magnetic resonance imaging. Arch Neurol 47:1299–1303
Filippi M, Tortorella C, Bozzali M (1999) Normal-appearing white matter changes in multiple sclerosis: the contribution of magnetic resonance techniques. Mult Scler 5:273–282
Furuse M, Sasaki H, Fujimoto K, Tsukita S (1998). A single gene product, claudin-1 or -2 reconstitutes tight junction strands and recruits occluding in fibroblasts. J Cell Biol 143:391–401
Girard J-P, Springer TA (1995) High endothelial venules: specialized endothelium for lymphocyte migration ismmunol. Today 16:449–457
Greenberg DA, Jin K (2005) From angiogenesis to neuropathology. Nature 438:954–959
Hawkins CP, Mackenzie F, Tofts P, du Boulay EP McDonald WI (1991) Patterns of blood–brain barrier breakdown in inflammatory demyelination. Brain 114:801–810
Hogg N, Laschinger M, Giles K, McDowall A (2003) T-cell integrins: more than just sticking points. J Cell Sci 116:4695–4705
Ilyas M, Tomlinson IP (1997) The interaction of APC, E-cadherin and beta-catenin in tumour development and progression. J Pathol 182:128–137
Ilyas M, Tomlinson IP, Rowan A, Pignatelli M, Bodmer WF (1997) Beta-catenin mutations in cell lines established from human colorectal cancers. Proc Natl Acad Sci USA 94:10330–10334
Itoh M, Sasaki H, Furuse M, Ozaki H, Kita T, Tsukita S (2001) Junctional adhesion molecule (JAM) binds to PAR-3: a possible mechanism for the recruitment of PAR-3 to tight junctions. J Cell Biol 154:491–497
Johnson-Leger CA, Aurrand-Lions M, Beltraminelli N, Fasel N, Imhof BA (2002) Junctional adhesion molecule-2 (JAM-2) promotes lymphocyte transendothelial migration. Blood 100:2479–2486
Kermode AG, Thompson AJ, Tofts P, MacManus DG, Kendall BE, Kingsley DP, Moseley IF, Rudge P, McDonald WI (1990) Breakdown of the blood–brain barrier precedes symptoms and other MRI signs of new lesions in multiple sclerosis. Pathogenetic and clinical implications. Brain 113:1477–1489
Kirk J, Zhou A-L (1996) Viral infection at the blood–brain barrier in multiple sclerosis: an ultrastructural study of tissues from a U.K. regional brain bank. Mult Scler Clin Lab Res 1:242–252
Kirk J, Plumb J, Mirakhur M, McQuaid S (2003) Tight junctional abnormality in multiple sclerosis white matter affects all calibres of vessel and is associated with blood–brain barrier leakage and active demyelination. J Pathol 201:319–327
Kirk S, Frank JA, Karlik S (2004) Angiogenesis in multiple sclerosis: is it good, bad or an epiphenomenon?. J Neurol Sci 217:125–130
Lai M, Hodgson T, Gawne-Cain M, Webb S, MacManus D, McDonald WI, Thompson AJ, Miller DH (1996) A preliminary study into the sensitivity of disease activity detection by serial weekly magnetic resonance imaging in multiple sclerosis. Neurol Neurosurg Psychiatry 60:339–341
Lassmann H, Wekerle H (2005) The pathology of multiple sclerosis, chapter 12. In: Compston A et al (eds) McAlpine’s multiple sclerosis, 4th edn. Churchill Livingstone, London, pp 557–600
Leech S, Kirk J, Plumb J, McQuaid S (2006) Persistent endothelial abnormalities and blood–brain barrier leak in primary and secondary progressive multiple sclerosis. Neuropathol Appl Neurobiol (in press)
Liang TW, DeMarco RA, Mrsny RJ, Gurney A, Gray A, Hooley J, Aaron HL, Huang A, Klassen T, Tumas DB, Fong S (2000) Characterization of huJAM: evidence for involvement in cell–cell contact and tight junction regulation. Am J Physiol Cell Physiol 279:C1733–C1743
Liang TW, Chiu HH, Gurney A, Sidle A, Tumas DB, Schow P, Foster J, Klassen T, Dennis K, DeMarco RA, Pham T, Frantz G, Fong S (2002) Vascular endothelial-junctional adhesion molecule (VE-JAM)/JAM 2 interacts with T, NK and dendritic cells through JAM-3. J Immunol 168:1618–1626
Liu Y, Nusrat A, Schnell FJ, Reaves TA, Walsh S, Pochet M, Parkos CA (2000) Human junction adhesion molecule regulates the junction resealing in epithelia. J Cell Sci 113:2363–2374
MacIntyre A, Hammond CJ, Little CS, Appelt DM, Balin BJ (2002) Chlamydia pneumoniae infection alters the junctional complex of human brain microvascular endothelial cells. FEMS Microbiol Lett 217:167–172
Makino A, Shimojima M, Miyazawa T, Kato K, Tohya Y, Akashi H (2006) Junctional adhesion molecule 1 is a receptor for feline calicivirus. J Virol 80: 4482–4490
Mandell KJ, Holley GP, Parkos CA, Edelhauser HF (2006) Antibody blockade of junctional adhesion molecule-A in rabbit corneal endothelial tight junctions produces corneal swelling. Invest Ophthalmol Vis Sci 47:2408–2416
Martin-Padura I, Lostaglio S, Schneemann M, Williams L, Romano M, Fruscella P, Panzeri C, Stoppacciaro A, Ruco L, Villa A, Simmons D, Dejana E (1998) Junctional adhesion molecule, a novel member of the immunoglobulin superfamily that distributes at intercellular junctions and modulates monocyte transmigration. J Cell Biol 142:117–127
Matthews PM, Arnold DL (2001) Magnetic resonance imaging of multiple sclerosis: new insights linking pathology to clinical evolution. Curr Opin Neurol 14:279–287
McRae BL, Kennedy MK, Tan LJ, Del Canto MC, Picha KS, Miller SD (1992) Induction of active and adoptive relapsing experimental autoimmune encephalomyelitis (EAE) using an encephalitogenic epitope of proteolipid protein. J Neuroimmunl 38:229–240
Michie SA, Streeter PR, Bolt PA, Butcher EC, Picker LJ (1993) The human peripheral lymph node vascular addressin. An inducible endothelial antigen involved in lymphocyte homing. Am J Pathol 143:1688–1698
Minagar A, AlexanderJS (2003) Blood–brain barrier disruption in multiple sclerosis. Mult Scler 9:540–549
Morrissey SP, Deichmann R, Syha J, Simonis C, Zettl U, Archelos JJ, Jung S, Stodal H, Lassmann H, Toyka KV, Haase A, Hartung HP (1996) Partial inhibition of AT-EAE by an antibody to ICAM-1: clinico-histological and MRI studies. J Neuroimmunol 69:85–93
Naik MU, Mousa SA, Parkos CA, Naik UP (2003) Signaling through JAM-1 and alphavbeta3 is required for the angiogenic action of bFGF: dissociation of the JAM-1 and alphavbeta3 complex. Blood 102:2108–2114
Ostermann G, Weber KS, Zernecke A, Schroder A, Weber C (2002) JAM-1 is a ligand of the beta (2) integrin LFA-1 involved in transendothelial migration of leukocytes. Nat Immunol 3:116–118
Palmeri D, van Zante A, Huang CC, Hemmerich S, Rosen SD (2000) Vascular endothelial junction-associated molecule, a novel member of the immunoglobulin superfamily, is localized to intercellular boundaries of endothelial cells. J Biol Chem 275:19139–19145
Palmeri D, Feng-Rong Z, Rosen SD, Hemmerich S (2004) Differential gene expression profile of human tonsil high endothelial cells: implications for lymphocyte trafficking. J Leukoc Biol 75:910–927
Petty MA, Lo EH (2002) Junctional complexes of the blood–brain barrier: permeability changes in neuroinflammation. Prog Neurobiol 68:311–323
Plumb J, McQuaid S, Mirakhur M, Kirk J (2002) Abnormal endothelial tight junctions in active lesions and normal-appearing white matter in multiple sclerosis. Brain Pathol 12:154–169
Plumb J, Armstrong MA, Mirakhur M, McQuaid S (2003) CD83-positive dendritic cells are present in occasional perivascular cuffs in multiple sclerosis lesions. Mult Scler 9:142–147
Proescholdt MA, Jacobson S, Tresser N, Oldfield EH, Merrill MJ (2003) Vascular endothelial growth factor is expressed in multiple sclerosis plaques and can induce inflammatory lesions in experimental allergic encephalomyelitis. J Neuropathol Exp Neurol 61:914–925
Reese TS, Karnovsky MJ (1967) Fine structural localization of a blood–brain barrier to exogenous peroxidase. J Cell Biol 34:207–217
Rosen SD (1999) Endothelial ligands for l-selectin: from lymphocyte recirculation to allograft rejection. Am J Pathol 155:1013–1020
Schule C, Firth JA (1993) Immunohistochemical localiation of adherens junctions components in blood–brain barrier microvessel of the rat. J Cell Sci 104:773–782
Seidensticker MJ, Behrens J (2000) Biochemical interactions in the Wnt pathway. Biochim Biophys Acta 1495:168–182
Serafini B, Rosicarelli B, Magliozzi R, Stiglano E, Capello E, Mancardi GL, Aloisi F (2006) Dendritic cells in multiple sclerosis lesions: maturation stage, myelin uptake and interaction with proliferating T cells. Neuropathol Exp Neurol 65:124–141
Sharief MK, Noori MA, Ciardi M, Cirelli A, Thompson EJ (1993) Increased levels of circulating ICAM-1 in serum and cerebrospinal fluid of patients with active multiple sclerosis. Correlation with TNF-α and blood brain barrier damage. J Neuroimmunol 43:15–22
Sobocka MB, Sobocki T, Babinski A, Hartwig JH, Li M, Ehrlich YH, Kornecki E (2004) Signaling pathways of the F11 receptor (F11R: a.k.a. JAM-1, JAM-A) in human platelets: F11R dimerization, phosphorylation and complex formation with the integrin GPIIIa. J Recept Signal Transduct Res 24:85–105
Tajouri L, Mellick AS, Ashton KJ, Tannenberg AE, Nagra RM, Tourtellotte WW, Griffiths LR (2003) Quantitative and qualitative changes in gene expression patterns characterize the activity of plaques in multiple sclerosis. Brain Res Mol Brain Res 119:170–183
Werring DJ, Clark CA, Droogan AG, Barker GJ, Miller DH, Thompson AJ (2001) Water diffusion is elevated in widespread regions of normal-appearing white matter in multiple sclerosis and correlates with diffusion in focal lesions. Mult Scler 7:83–89
Williams LA, Martin-Padura I, Dejana E, Hogg N, Simmons DL (1999). Identification and characterisation of human junctional adhesion molecule (JAM). Mol Immunol 36:1175–1188
Wolburg H, Wolburg-Buchholz K, Engelhardt B (2005) Diapedesis of mononuclear cells across cerebral venules during experimental autoimmune encephalomyelitis leaves tight junctions intact. Acta Neuropathol (Berl) 109:181–190
Woodroofe MN, Cuzner ML (1993) Cytokine mRNA expression in inflammatory multiple sclerosis lesions: detection by non-radioactive in situ hybridization. Cytokine 5:583–588
Xu H, Dawson R, Crane IJ, Liversidge J (2005) Leukocyte diapedesis in vivo induces transient loss of tight junction protein at the blood–retina barrier. Invest Ophthalmol Vis Sci 46:2487–2494
Yap AS, Brieher WM, Gumbiner BM (1997) Molecular and functional analysis of cadherin-based adherens junctions. Annu Rev Cell Dev Biol 13:119–146
Zhurinsky J, Shtutman M, Ben-Ze’ev A (2000) Plakoglobin and beta-catenin: protein interactions, regulation and biological roles. J Cell Sci 113:3127–3139
Acknowledgments
Suzie Leech was the recipient of a 1-year post-doctoral fellowship from MS Ireland. The Leica SP2 confocal microscope was purchased with a Wellcome Trust Equipment grant (069411/Z/02/Z). Tissue samples were supplied by the UK Multiple Sclerosis Tissue Bank, funded by the Multiple Sclerosis Society of Great Britain and Northern Ireland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Padden, M., Leech, S., Craig, B. et al. Differences in expression of junctional adhesion molecule-A and β-catenin in multiple sclerosis brain tissue: increasing evidence for the role of tight junction pathology. Acta Neuropathol 113, 177–186 (2007). https://doi.org/10.1007/s00401-006-0145-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-006-0145-x