Abstract
We report here a case of orthochromatic leukodystrophy with spheroids. A 40-year-old woman developed forgetfulness. About 1 year after the onset, clinical examination confirmed global intellectual deterioration with amnesia, spatiotemporal disorientation, and impairment of judgment. At age 43, she experienced tonic-clonic convulsions several times, and died of pneumonia at the age of 44. Alzheimer’s disease was suspected clinically. Pathologically, there was severe diffuse demyelination of the deep white matter of the frontal, parietal and occipital lobes with relative preservation of the subcortical U fibers. In the central demyelinated areas, myelin loss was severe with diffuse gliosis, moderate loss of axons, and many axonal spheroids. At the periphery of the severely degenerated regions, there were a lot of macrophages and most had non-metachromatic lipid granules. The cerebral cortex was intact. The neuropathological findings of this case are consistent with hereditary diffuse leukoencephalopathy with spheroids (HDLS). Ten cases of HDLS were reviewed and presented many findings in common. The gray matter was intact and U fibers were well preserved in most cases. In white matter lesions, severe loss of myelin, moderate to severe axonal loss, much axonal swelling, and the presence of macrophages and hypertrophic astrocytes were common findings. In some cases with HDLS, dementia appeared without obvious neurological manifestations in the early stage. We should remember that some cases with HDLS show clinical symptoms similar to Alzheimer’s disease, especially in the early stage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthochromatic (sudanophilic) leukodystrophy (OLD) is a heterogeneous group of neurological disorders morphologically characterized by progressive demyelination of the brain with nonmetachromatic or sudanophilic lipid degradation [10]. In a considerable proportion of the patients, the basic biochemical or gene defect remains unknown, despite the sometimes clear evidence of inheritability [12]. Hereditary diffuse leukoencephalopathy with spheroids (HDLS) is thought to be one of the disease entities included in OLD, and neuropathologically characterized by a combination of leukodystrophy and the presence of neuroaxonal spheroids [11].
Clinically, OLD frequently shows severe spastic paraplegia, but patients with OLD are occasionally clinically suspected of Alzheimer’s disease. We examined an autopsy case with HDLS who initially showed forgetfulness and was clinically suspected of Alzheimer’s disease. Therefore, we report the case and review cases with similar neuropathological findings.
Case report
Four years before her death, a 40-year-old housewife developed progressive intellectual deterioration. She bought same things frequently, often forgot to do what she was told to do, and could cook only simple dishes. Her intellectual impairment progressively increased, and she was examined by neurologists about a year after the onset of her illness.
Clinical examination confirmed global intellectual deterioration with amnesia, spatiotemporal disorientation, and impairment of judgment. She had also frontal lobe syndrome: she was usually indifferent, abulic, and her vocabulary was reduced in size. She showed a slightly forward-leaning posture, but neither rigidity nor involuntary movement was recognized. Deep tendon reflexes were within normal limits with no pathological reflex.
Routine laboratory tests, examination of the fundus oculi, and endocrine screening tests were normal. Detailed metabolic investigations were not performed. The revised Hasegawa dementia scale rating was 12 points (full score 30 points). A computer tomographic scan of the head at age 41 revealed slight atrophy of the frontal lobes and enlargement of the anterior horn of the lateral ventricles without obvious periventricular lucency (Fig. 1a). Single photon emission CT (99mTc-ECD) showed hypoperfusion in the frontoparietal region (Fig. 1b). The electroencephalogram showed slow α activity (9 c/s).
At age 41, she became unable to cook. She was abulic all day and forgot that she had eaten soon after a meal. Gradually, she became unable to wear her clothes because of dressing apraxia and frequently showed urinary incontinence. She was admitted to a hospital at age 42. At age 43, she experienced tonic-clonic convulsions several times, and became bedridden. She showed no bone fractures during her clinical course, and died of pneumonia at age 44. During her 4-year disease course she was suspected clinically of having Alzheimer’s disease.
Family history
The patient’s mother also suffered from presenile dementia. She became forgetful at the age of 57. She gradually grew worse, became bedridden, and died at the age of 65. The patient’s elder sister and younger brother said that the clinical signs of the patient’s mother were similar to those of the patient. However, no more detailed information was gained. The pattern of inheritance is suspected to be autosomal dominant, although the possibility of cytoplasmic inheritance cannot be excluded in the pedigree.
Neuropathological findings
The fixed brain weighed 1,160 g. Mild brain atrophy was observed in the frontoparietal lobes. Meninges and vessels were normal. Moderate enlargement of the lateral ventricle, especially the anterior horns, and severe thinning of the corpus callosum were also found. Coronal sections of the cerebral hemispheres showed symmetrical, diffuse, grayish, gelatinous lesions in the cerebral white matter. Most of the subcortical U fibers in the cerebral white matter were preserved, and the white matter of the temporal lobes showed less involvement. The spinal cord and peripheral nerves were not available for histological examination.
Tissue blocks were taken from many regions of the brain: midfrontal and orbitofrontal areas; superior, middle and inferior temporal, inferior parietal, and occipital cortices; anterior cingulate; amygdala; hippocampus; striatum; thalamus; midbrain; pons; medulla; and cerebellum. Six-micrometer-thick sections of formalin-fixed, paraffin-embedded tissue were stained with Gallyas-Braak and Bodian silver impregnations, Holzer, PAS, toluidine blue, and Berlin blue stains, besides hematoxylin-eosin (HE) and Klüver-Barrera staining.
The following immunocytochemical markers were used: anti-α-synuclein (C-20, an antibody against the C terminus of human α-synuclein; goat polyclonal; 1:100; Santa Cruz, USA) and anti-phosphorylated tau (AT8, an antibody against phosphorylated tau at Ser202 and Thr 205; mouse monoclonal; 1:1,000; Innogenetics, Belgium). Deparaffinized sections were incubated with 1% H2O2 in methanol for 30 min to eliminate endogenous peroxidase activity in the tissue. The anti-α-synuclein antibody was used after pretreatment of the sections with formic acid (99%, 5 min; Sigma, USA). After blocking with 10% normal serum, sections were incubated overnight at 4°C with one of the primary antibodies. The sections were washed in PBS and incubated with biotinylated secondary antibodies, followed by avidin-biotinylated horseradish peroxidase complex (ABC Elite kit, Vector, USA). The reaction was visualized with 0.2% 3,3′-diaminobenzidine in 50 mM TRIS-HCl buffer, pH 7.4, containing 0.003% H2O2. Counterstaining was carried out with hematoxylin.
For electron microscopy, portions of the frontal and parietal white matter were taken from the formalin-fixed brain. The materials were fixed in 2.5% glutaraldehyde, post-fixed in 2% osmium tetroxide, dehydrated, and then embedded in Epon. Ultrathin sections were stained with uranyl acetate and lead citrate and examined with a JOEL JEM-1010 electron microscope at 80 kV.
Microscopic findings
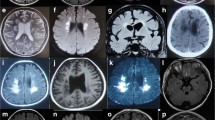
Microscopic examination showed severe diffuse demyelination of the deep white matter of the frontal, parietal, and occipital lobes with relative preservation of the subcortical U fibers (Fig. 2). The involvement of the internal capsule and corpus callosum was also severe, but the white matter of the temporal lobes showed less involvement (Fig. 2c).
Frontal lobe, b parieto-occipital lobes, c coronal section of the cerebrum at the level of amygdala, d thalamus and subthalamic nucleus. Klüver-Barrera (left side) and Holzer staining (right side) of the cerebrum. Severe diffuse demyelination of the deep white matter of the frontal (a), parietal (b) and occipital (b) lobes with relative preservation of the subcortical U fibers (a–c) is seen. The involvement of the internal capsule and corpus callosum is also severe (c), but the white matter of the temporal lobes shows less involvement (c). Mild gliosis is observed in the globus pallidus, thalamus and subthalamic nucleus (c, d). Bar 1 cm
In the central demyelinated areas, myelin loss was severe with diffuse gliosis, moderate loss of axons and many axonal spheroids. At the periphery of the severely degenerated regions, many macrophages were noted (Fig. 3a). The macrophages sometimes contained nonmetachromatic lipid granules that were stained positively by Sudan III and Sudan Black (Fig. 3b–d). Macrophages and astrocytes occasionally contained light-brown or dark-yellow iron-positive pigment. There was no infiltration of inflammatory cells, and vascular lesions were absent. There were also no globoid cells or Rosenthal fibers. The cerebral cortex was intact without senile plaques, neurofibrillary tangles, or axonal spheroids.
Microscopic findings. a Macrophages at the periphery of the severely degenerated regions in the orbitofrontal lobe. b, c Lipid granules of macrophages in the parietal lobe are stained positively by Sudan III (b) and Sudan Black (c). d Lipid granules of macrophages in the frontal lobe are nonmetachromatic with toluidine blue staining. e, f Many axonal spheroids are present in the internal capsule (e) and cerebral peduncle of the midbrain (f). Bars a 10 μm, b–f 50 μm
Mild gliosis were observed in the globus pallidus, thalamus, and subthalamic nucleus (Fig. 2c, d). In the brain stem, the substantia nigra and locus ceruleus were well preserved. Myelin pallor and gliosis were present in the pyramidal tract, and axonal spheroids were also observed (Fig. 3e, 3f). In the cerebellum, gliosis was found only in the hilus dentate, without involvement of the cerebellar cortex. The dentate nucleus was well preserved. The spinal cord and peripheral nerves were not available for histological examination.
Immunohistochemistry for α-synuclein and phosphorylated tau revealed no remarkable accumulation in the brain.
Ultrastructural study
Electron microscopy of the cerebral white matter showed a severe loss of myelin sheaths, dilatations of the periaxonal spaces, and partially split or broken myelin sheaths. Spheroids in the cerebral white matter were filled with numerous neurofilaments, and closely packed organelles were pushed out to the peripheral region (Fig. 4).
Electron microscopy. a Axonal spheroid in the white matter of the frontal lobe. b Part of the spheroid in a. The axonal spheroid is filled with numerous neurofilaments, and closely packed organelles are mainly pushed out to the peripheral region. Due to postmortem artifacts, details cannot be evaluated. Bars a 2 μm; b 200 nm
Discussion
Differential diagnosis
From the neuropathological findings, this case was grossly classified as diffuse sclerosis. However, there were no globoid cells or Rosenthal fibers. Lipid granules in macrophages showed no metachromasia, and tigroid demyelination, which is a characteristic finding in Pelizaeus-Merzbacher disease, was not present. This case was female, and the frontoparietal dominancy of the demyelination in this case was quite different from the occipital dominancy of the demyelination in adrenoleukodystrophy. Therefore, this case was classified as OLD.
Neuropathologically, this case was characterized by orthochromatic leukodystrophy and the presence of many neuroaxonal spheroids in the abnormal white matter. The neuropathological findings of this patient are consistent with pure forms of OLD. Peiffer [9] divided the pure forms of OLD into the simple type and OLD with pigmented scavenger and glial cells (pigmentary type). The absence of macrophages and astrocytes containing a light-brown, iron-positive lipopigment in this case is consistent with the diagnosis of the simple type of OLD.
There have been several reports of patients who showed pathological features similar to the present case. Seitelberger [11] recognized a combination of leukoencephalopathy and the presence of neuroaxonal spheroids in the abnormal white matter. He classified such cases as neuroaxonal leukodystrophy and cited several examples, including two siblings of dermatoleukodystrophy with spheroids (DLDS) [4], patients with Nasu-Hakola disease [5, 6], those with HDLS [2], and two patients reported by Yazawa [7, 13].
Nasu-Hakola disease is one of the entities to consider in a differential diagnosis. It is an autosomal recessive disorder usually characterized by a combination of bone disease, cerebral white matter disease, and calcium depositions in the basal ganglia [1, 6]. In most patients, the disease begins with ankle or wrist pain after a strain during the third decade, followed by fractures caused by cystic lesions in the bones of the extremities. Frontal lobe syndrome and dementia begin to develop by age 30, leading to death by age 40 [8]. Neuroimaging disclosed abnormally high and progressively increasing bicaudate ratios and calcifications in the basal ganglia [8]. Yazawa et al. [13] summarized the neuropathological characteristics of Nasu-Hakola disease as the occurrence of intense fibrillary gliosis accompanied by slight loss of myelin sheaths in the cerebral white matter, distribution of spheroids in the cerebral white matter with no concentration in the pyramidal tracts, numerous depositions of pseudocalcium in the pallidal nuclei, and the ultrastructural presence of spheroids with an accumulation of various organelles that have small amounts of neurofilaments. In the present case, severe loss of myelin sheaths, distribution of spheroids with concentration in the pyramidal tract, no deposition of calcium or pseudocalcium in the pallidal nuclei, no obvious atrophy of the caudate nucleus, and the ultrastructure of spheroids with abundant neurofilaments suggested differences between Nasu-Hakola disease and the present case. Also, our case had not complained of pain in her extremities, and did not experience bone fracture in her clinical course. Therefore, although we cannot rule out the possibility that the present case is Nasu-Hakola disease, the probability is low.
DLDS produces neuropathological findings similar to those of Nasu-Hakola disease and shows autosomal recessive inheritance, but DLDS has an early infantile onset and results in early death [4]. DLDS also shows a characteristic dermatosis, and our case did not experience this. Therefore, the probability that our case suffered from DLDS is very low.
The neuropathological findings of the present case are consistent with the diagnosis of HDLS.
Hereditary diffuse leukoencephalopathy with spheroids
Table 1 shows the clinical symptoms of ten cases of HDLS, including our case [2, 12, 13]. The age at onset was 15–55 years (33.6±14.0 years), and at death 17–89 years (42.6±19.5 years). The initial symptoms were seizures in three cases, motor symptoms in four cases, memory disturbance in two cases, and apathy in one case. In all cases, amnesia, disorientation, and gait disturbance were reported. In some cases, including our case, who showed memory disturbance without obvious neurological signs in the early stage, Alzheimer’s disease is a disease to consider in the differential diagnosis. Spasticity was recorded in nine of nine cases, and epileptic seizure was common (six of nine cases).
The neuropathological findings are summarized in Table 2 [2, 12, 13]. Brain weights were 1,110–1,470 g, and gyral atrophy was not severe. Macroscopically, white matter lesions were noted in the frontal lobe in seven of ten cases, and moderate to severe narrowing of the corpus callosum was also reported. Microscopically, gray matter was intact, and U fibers were well preserved in most cases. In white matter lesions, severe loss of myelin, moderate to severe axonal loss, frequent axonal swelling, and the presence of macrophages and hypertrophic astrocytes were common findings. Basal ganglia, especially in the caudate nucleus and putamen, were relatively intact, but in five of seven cases, thalamic lesions were described. The internal capsule and pyramidal tract in the brain stem were also severely affected. Many common findings were present in these ten cases.
In our case, there is a discrepancy between mild abnormalities observed on head CT scan and the severity of the white matter lesions at neuropathological examination. In recent literature, few white matter abnormalities on head MRI including FLAIR sequences in hereditary leukodystrophy have been described [3]. These data suggest that it is sometimes difficult to estimate white matter lesions exactly in cases with leukoencephalopathy without histological materials.
Summary
We report a case with OLD with spheroids. The neuropathological findings of this case are consistent with HDLS. In some cases with HDLS, dementia appears without obvious neurological manifestation in the early stage. The fact that some cases with HDLS might show clinical symptoms similar to Alzheimer’s disease, especially in their early stage, should be borne in mind.
References
Araki T, Ohba H, Monzawa S, Sakuyama K, Hachiya J, Seki T, Takahashi Y, Yamaguchi M (1991) Membranous lipodystrophy: MR imaging appearance of the brain. Radiology 180:793–797
Axelsson R, Roytta M, Sourander P, Akesson HO, Andersen O (1984) Hereditary diffuse leucoencephalopathy with spheroids. Acta Psychiatr Scand Suppl 314:1–65
Letournel F, Etcharry-Bouyx F, Verny C, Barthelaix A, Dubas F (2003) Two clinicopathological cases of a dominantly inherited, adult onset orthochromatic leucodystrophy. J Neurol Neurosurg Psychiatry 74:671–673
Matsuyama H, Watanabe I, Mihm MC, Richardson EP Jr (1978) Dermatoleukodystrophy with neuroaxonal spheroids. Arch Neurol 35:329–336
Minagawa M, Maeshiro H, Kato K, Shioda K (1980) A rare case of leucodystrophy—neuroaxonal leucodystrophy (Seitelberger) (in Japanese). Seishin Shinkeigaku Zasshi 82:488–503
Minagawa M, Maeshiro H, Shioda K, Hirano A (1985) Membranous lipodystrophy (Nasu disease): clinical and neuropathological study of a case. Clin Neuropathol 4:38–45
Oda M, Ejima H, Abe H, Ariga T, Miyatake T, Tokuta S (1981) Familial sudanophilic leukodystrophy with multiple and semisystematic spongy foci: autopsy report of three adult females. International Symposium on the leukodystrophy and allied diseases in Kyoto. Neuropathology (Suppl) 1:173–185
Paloneva J, Autti T, Raininko R, Partanen J, Salonen O, Puranen M, Hakola P, Haltia M (2001) CNS manifestations of Nasu-Hakola disease: a frontal dementia with bone cysts. Neurology 56:1552–1558
Peiffer J (1970) The pure leucodystrophic forms of orthochromatic leucodystrophies (simple type, pigment type). Handb Clin Neurol 10:105–119
Seiser A, Jellinger K, Brainin M (1990) Pigmentary type of orthochromatic leukodystrophy with early onset and protracted course. Neuropediatrics 21:48–52
Seitelberger F (1986) Neuroaxonal dystrophy: its relation to aging and neurological disease. Handb Clin Neurol 49:391–415
Van der Knaap MS, Naidu S, Kleinschmidt-Demasters BK, Kamphorst W, Weinstein HC (2000) Autosomal dominant diffuse leukoencephalopathy with neuroaxonal spheroids. Neurology 54:463–468
Yazawa I, Nakano I, Yamada H, Oda M (1997) Long tract degeneration in familial sudanophilic leukodystrophy with prominent spheroids. J Neurol Sci 147:185–191
Acknowledgement
The authors thank Ms M. Onbe and Ms A. Kajitani for their skillful technical assistance. This study was partly supported by a research grant from the Zikei Institute of Psychiatry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terada, S., Ishizu, H., Yokota, O. et al. An autopsy case of hereditary diffuse leukoencephalopathy with spheroids, clinically suspected of Alzheimer’s disease. Acta Neuropathol 108, 538–545 (2004). https://doi.org/10.1007/s00401-004-0920-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-004-0920-5