Abstract
To study the incidence and topographic distribution of α-synuclein-positive inclusions in Parkinson’s disease (PD), dementia with LB (DLB), and Alzheimer’s disease (AD), 206 brains of elderly patients, including 53 patients with clinical PD, 110 autopsy-proven AD cases, 22 with dementia with LB (DLB), 1 case with essential tremor, and 20 age-matched controls were investigated using α-synuclein immunohistochemistry. For technical reasons, the olfactory system was not studied. In all PD brains, α-synuclein-positive inclusions and neuronal losses were present in medullary and pontine nuclei, locus coeruleus, and substantia nigra, with additional lesions in amygdala (24%), allocortex (58%), cingulate area (34%), and isocortex (26.5%). All PD cases corresponded to pathology stage 4–6 suggested by Braak et al. (2003, Neurobiol Aging 24:197). In most cases of DLB, the distribution of α-synuclein pathology and neurodegeneration corresponded to stages 5 and 6 of PD pathology. The case with essential tremor and 48.2% of the AD cases showed no LB pathology; in the other AD brains α-synuclein-positive inclusions were seen in various brain areas. None of the controls showed LB pathology. Among 12 cases of incidental Lewy body disease (without clinical parkinsonian signs), 7 corresponded morphologically to PD stage 3 or 4. In further 6 AD cases, 2 with parkinsonian symptoms, considerable damage to locus coeruleus, substantia nigra, nucleus basalis and allocortex with preservation of the medullary nuclei was seen. The preliminary data largely confirm the Braak staging of brain pathology, although some of the clinical PD cases corresponded to stage 3 often considered as “preclinical”. In addition, some cases without demonstrable involvement of medullary nuclei showed extensive PD-like pathology in other brain areas, suggesting deviation from the proposed stereotypic expansion pattern and that incidental LB pathology may affect solely the locus coeruleus and substantia nigra. Striking similarity of LB pathology between DLB and PD suggests close morphological relationship between both disorders. Widespread LB lesions occurred in many sporadic AD cases without parkinsonian symptoms, the pathogenesis and clinical impact of which are unclear. The relationship between AD and PD with particular reference to synaptophysin-positive lesions needs further elucidation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) or brain stem type of Lewy body (LB) disease [51] is the most common neurodegenerative disorder in the elderly, with progressive degeneration of the dopaminergic nigrostriatal system and other neuronal networks caused by progressive loss of neuromelanin-containing projection nuclei in the substantia nigra zona compacta (SNc) and many other subcortical nuclei associated with widespread occurrence of LBs and dystrophic or Lewy neurites (LN) [13, 19, 21, 25, 37, 38, 39, 40].
There is increasing evidence that PD is a multiple system disorder with considerable and widespread extranigral pathology [5, 6, 7, 8, 9, 17, 26, 29, 37, 38, 39, 40, 48]. While previous authors called attention to the presence of inclusions bodies in the dorsal motor nucleus of the glossopharyngeal and vagal nerves (dorsal IX/X motor nucleus/dmX) [18, 26, 44, 45, 56, 61], recent studies demonstrated early involvement of these nuclei and adjoining areas of the reticular formation and raphe system, the coeruleus-subcoeruleus complex (LC), the magnocellular nuclei of the basal forebrain and many subnuclei of the thalamus and amygdala, whereas the neocortex is only inconsistently involved [5, 6, 7, 8, 9, 10, 11, 14]. Studies in cases with incidental LB pathology, i.e., cases with postmortem presence of α-synuclein (AS)-immunoreactive (IR) LBs and LNs in specific vulnerable regions with no or only minor neuronal loss and absence of sensori-motor PD symptoms, indicated that the lesions begin in non-catecholaminergic neurons of the above-cited nuclei in the medulla and in the olfactory system without involvement of the dopaminergic striatonigral system and, in particular, of the SNc. These data suggested that medullary and olfactory system lesions precede classical PD-related pathology [14].
Based on further autopsy studies in a cohort of subjects with the clinical diagnosis of PD, in aged individuals showing the presence of LNs and/or LBs in the aforementioned predilection sites, and in age- and gender-matched controls, Braak et al. [7, 8, 9, 11] proposed a staging of brain pathology related to sporadic/idiopathic PD. They distinguished presymptomatic stages 1 and 2 with LB pathology confined to the medulla oblongata and olfactory bulb, with the nucleus basalis of Meynert (NBM), the SNc and other regions being uninvolved. In stage 3, LC, the central nucleus of the amygdala, the nuclei of the basal forebrain (interstitial nucleus of the diagonal band, NBM) that constitute the “gain setting nuclei” of the lower brain stem [8, 9, 10, 31, 53], and the posterolateral and posteromedial SNc are the focus of initially subtle and, then, severe cytoskeletal changes and neuronal depletion, while the allocortex and isocortex are preserved. In stage 4, the anteromedial temporal limbic and mesocortex are additionally affected. Stages 3 and 4 can be correlated with clinically symptomatic changes, while in terminal stages 5 and 6, the pathological process reaches the telencephalic cortex, first affecting the sensory association cortex and prefrontal areas, later progressing to the primary sensory and motor areas or involving almost the whole neocortex.
A weak point in this study was that, although in most cases with the clinical diagnosis of PD the pathological pattern of these lesions corresponded to the clinical picture, in a large number of cases showing stage 1 to 4 PD pathology there were no clinical data available. Furthermore, it should be considered that LBs and related AS-IR inclusions are found in the brain stem, limbic areas and neocortex of a variety of disorders, including aging and Alzheimer’s disease (AD) [15, 16, 22, 27, 46, 47, 55]. LBs also occur in the SN and brain stem in up to 10% of neurologically normal aged individuals [58], and some of them may correspond to “incidental” LB disease (LBD) or incipient synucleinopathy of no or little clinical relevance, suggesting that subclinical PD is present concurrently in some subjects [12].
AS pathology, both cortical and subcortical, has been observed in up to 14% of subjects over the age of 40 years, with an average of 13% in non-demented and of 23% in demented individuals [55]. Cortical LBs are common in both familial and sporadic forms of AD [3, 12, 15, 27, 46, 47, 55, 60], estimates ranging from 7% to 71% in sporadic AD [3, 46, 55]. AD patients may also have numerous LBs and LNs in the amygdala, even in the absence of subcortical LBs [27, 47]. This has been reported in over 60% of familial AD cases [46], in about 50% of sporadic AD cases [3, 44, 59, 60] and of Down syndrome patients with AD [46, 47]. However, recent studies observed AS pathology in the amygdala only in 15.0% of AD brains associated with LBs in the SNc, LC, medulla and temporal or limbic cortex in several cases, while lesions in the amygdala were seen in 38.3% of AD including the Lewy body variant of AD/LBV/AD). The Braak stages, age, ApoE allele frequency and tau haplotype did not differ between AD cases with and without LB pathology in the amygdala [15]. Parkkinen et al. [55] recently reported AS pathology in 30% of sporadic AD cases, with involvement of one or more of the brain areas SNc, NBM or amygdala. The last region was involved in 30% of the AD brains.
Examining 20 diffuse DLB and 4 AD brains, Ishizawa et al. [36] found tau-immunoreactive LBs in the medulla of 80% of the cases, irrespective of Braak stage. The proportions of tau-positive LBs was greatest in neurons vulnerable to neurofibrillary tangle (NFT) formation, e.g., in LC and NBM, and was lowest in those areas resistant to NFT formation, such as dmX in the medulla. These and other data suggest that tau may coaggregate in LBs, especially in neuronal populations vulnerable for both NFTs and LBs.
In view of the conflicting results on the occurrence and development of LB pathology in PD and AD, we performed a neuropathological study of several types of disorders related to LB pathology (1) to try to control and validate the staging of brain pathology in PD, and (2) to examine the occurrence of LB pathology in AD and its possible relations to PD.
Material and methods
The study included a total of 206 elderly individuals derived from the files of the Institute of Clinical Neurobiology, Vienna, Austria, that neuropathologically serves four large general hospitals (two acute and chronic care units each) in Austria.
Clinical assessment
All clinical notes were retrospectively assessed from hospital charts. The diagnosis of PD required a history of akinesia plus other cardinal symptoms (rest tremor, rigidity, akinesia, impaired postural control, etc.) according to the UK Parkinson’s Disease Society Brain Bank inclusion and exclusion criteria [33, 34]. Dementia was assessed according to the ‘Diagnostic and statistical manual of mental disorders’ (DSM) IV [1] as a loss of intellectual capacity that interfered with social or occupational function. In practice, only patients with moderate to severe cognitive impairment, i.e., Mini-Mental State scores (MMSE) [20] of less than 20 were considered demented.
Neuropathological assessment
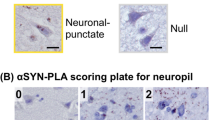
At autopsy, part of the brain was sagittaly sectioned, one half was deep-frozen for biochemistry and the other half was fixed in 4% buffered aqueous solution of formaldehyde. Multiple blocks of neocortical areas (frontal, temporal, parietal, occipital), the hippocampal formation (including amygdala, parahippocampal area and superior temporal lobe), the basal ganglia, midbrain, pons, medulla, and cerebellum were embedded in paraffin. For technical reasons, the olfactory system was not specifically examined. In addition to routine stains, modified Bielschowsky and Campell silver impregnations and immunohistochemistry for GFAP, tau protein (antibody AT-8, Innogenetics, Heiden, Germany), ubiquitin, and AS (monoclonal and polyclonal antibodies, gifts by Dr. D.W. Dickson, Mayo Clinic, Jacksonville, FL) were performed (for methods see [41]). Coexistent AD pathology was rated according to the criteria of the Consortium to Establish a Register on Alzheimer’s disease (CERAD) [52] and the Braak staging of neuritic AD changes [4].
The anatomical distribution of AS-related lesions was assessed using several brain stem atlases [53] and the anatomical descriptions and drawings by Del Tredici et al. [14] and Braak et al. [8, 9]. The severity of the AS-related pathology was assessed semiquantitatively in four degrees (− absent, + mild, ++ moderate, +++ severe), although in many cases no exact staging procedure was possible.
Group selection
Based on neuropathological findings, the following six groups were distinguished:
-
1.
A cohort of 53 individuals with the clinical diagnosis of PD according to established criteria [23, 32, 33] (26 males and 27 females aged at death 60–91 years, mean 76.1 ± 7.6 years), almost all showing Hoehn and Yahr stages IV and V; 23 (43.5%) were reported to have developed dementia. In all brains, there was severe loss of pigmented neurons in SNc, LC and dmX, widespread LBs and considerable extranigral lesions. For technical reasons, the amygdala and C2/3 hippocampal regions could not be assessed in 6 and 10 brains, respectively. The non-demented PD cases scored CERAD 0-A and Braak 0–4 (mean 2.0); the demented ones ranged CERAD A-C and Braak stages 2–5 (mean 4.1).
-
2.
A group of 53 demented patients (31 females, 22 males, aged at death 67–92 years, mean 75.0 ± 7.9 years) with classical, fully developed AD pathology, all scoring CERAD B or C and Braak stages 4.5 to 6 (mean 5.0) without AS pathology.
-
3.
A group of 57 demented patients (32 females, 25 males, aged at death 67–101 years, mean 78.6 ± 8.3 years) all showing fully developed AD pathology scoring CERAD B or C and Braak stages 4.5 to 6 (mean 5.1) in which AS-IR inclusions were found in various parts of the brain. In 5 of these patients, in addition to AD or dementia, some parkinsonian symptoms, like gait disorders, tremor, falls, rigidity, and dysphagia without other definite sensori-motor symptoms were reported.
-
4.
A group of 22 cases of DLB of neocortical and limbic type [51] (12 females, 10 males, aged at death 66–92 years, mean 74.0 ± 6.3 years), 15 representing diffuse forms of DLB with only minor AD-related pathology, and 7 classified as LBV/AD showing a combination of DLB with fully developed AD scoring CERAD B or C and Braak stage 5 [28].
-
5.
One nondemented female aged 88 years with 20 years’ history of essential tremor without typical parkinsonian signs of symptoms, associated with Braak stage 4 of neuritic AD pathology.
-
6.
A group of 20 age-matched individuals (6 males and 14 females) aged at death 78–84 years, mean 76.8 ± 5.7 years) without clinical history of neurological and psychiatric disorder or cognitive impairment. Neuropathology revealed nothing abnormal beyond aged-related changes, with AD pathology scoring CERAD 0 and Braak stages 2–4 (mean 3.2 ± 0.5). None of these brains contained any AS-related pathology.
Results
PD patients
All brains from patients with clinically and neuropathologically confirmed PD revealed LNs and/or LBs in the dorsal IX/X motor nuclei (dmX) (Fig. 1) and in the magnocellular reticular formation of the medulla, in the nucleus of the solitary tract, in the LC, pedunculopontine nucleus, and in the SNc, usually associated with considerable loss of pigmented neurons, dispersion of neuromelanin, and mild proliferation of micro- and astroglia in SNc, LC, and dmX, while the NBM was not affected in 11/50 brains (22%).
Involvement of the amygdala, in particular of the cortical and medial nuclei [6], was seen in 10/47 cases (23.8%), all showing lesions in medulla, pons, and SNc. LBs in the entorhinal and transentorhinal cortex were observed in 28/48 brains (58.3%); all except for 2 (without involvement of the NBM) with damage to brain stem and NBM. LBs in the cingulate cortex were detected in 16/47 cases (34.0%); all except for one with unaffected NBM showed involvement of the aforementioned brain stem and diencephalic nuclei (Table 1). LBs in the isocortex, in particular in the frontal and prefrontal areas, were detected in 13 brains (26.5%), all fulfilling the morphological criteria for PD stage 4 or 5 [7, 8, 9, 11], while they were clinically scored Hoehn and Yahr stage V. Seven of these patients were demented, all showed LBs in entorhinal and anterior cingulate cortex, 4 with considerable lesions in corticomedial amygdala, and 6 of them revealed coexistent severe neuritic AD pathology (Braak stages 4–5 and 5, mean 4.8).
AD patients
The 109 brains of autopsy-confirmed AD, according to the immunohistochemical findings, were separated into two major groups:
-
1.
AD brains with negative AS immunohistochemistry: 53 brains of demented elderly patients with fully developed AD (48.2% of the total) revealed no AS pathology in any of the regions examined, and in none of them had any parkinsonian signs or symptoms been reported.
-
2.
AD brains with positive AS immunohistochemistry: in 56 brains of elderly demented patients with autopsy-proven fully developed AD (all scoring Braak stage 4.5 to 6), AS-IR lesions were seen in various cerebral areas (51.8% of the total AD group). Of these cases 41 showed no medullary lesions, while in 15 brains (8 females, 7 males aged 69–94 years, mean 82.5 years) these were present (Figs. 2, 3), suggesting incidental LBD or sub/preclinical PD (see Table 4). In 3 brains the additional lesions were restricted to LC and SNc, in 6 brains additional AS-positive inclusions were present in entorhinal cortex and/or amygdala. While 18 AD brains showed AS-positive lesions in only one brain area, 30 revealed AS pathology in two or more areas. The incidence and distribution of AS-positive inclusions in AD brains are summarized in Tables 2 and 3.
Fig. 2 Fig. 3 AS-positive fibers and inclusions in magnocellular reticular formation in brain shown in Fig. 2
Table 2 Frequence of AS-positive inclusions in various cerebral regions in AD brains (AD Alzheimer’s disease) Table 3 Combined AS-positive involvement of AD brain areas (LC locus coeruleus)
Considering recent data [8, 9, 10, 14], the group of AD cases with AS-positive inclusions was divided into two groups: brains without involvement of medullary nuclei, and brains with AS pathology in medullary nuclei.
Brains without involvement of medullary nuclei
Lesion of SNc
Involvement of SNc with LBs or LNs with no or only mild neuronal loss was observed in 10 brains, 6 showing isolated affection of SNc, 2 with additional involvement of the amygdala and another 2 with singular LBs in entorhinal and cingulate cortex. In none of the patients were any parkinsonian symptoms recorded.
Lesion of LC and SNc
In 7 brains, isolated affection of LC and SNc without further AS pathology was observed. In further 8 brains, LC and SNc lesions were associated with LBs in the entorhinal cortex (1), in cingulate gyrus (2), amygdala and entorhinal cortex (2), amygdala, cingulate and entorhinal cortex (1), and amygdala, entorhinal and isocortex (1). In 3 of these patients, in addition to dementia, some parkinsonian signs (rigidity, tremor, and gait disorders) had been recorded.
Involvement of NBM without affection of LC and SNc
In 3 brains, isolated affection by LBs or LNs in NBM was detected, in another case associated by AS-positive inclusions in amygdala and entorhinal cortex.
Involvement of LC, SNc and NBM
In 2 brains, AS inclusions were seen in all three nuclei, accompanied by lesions in the amygdala.
Involvement of LC and NBM without affection of SNc
In 1 brain, AS inclusions in LC and NBM as well as in amygdala, entorhinal and cingulate cortex were detected. This patient showed no parkinsonian symptoms.
Involvement of amygdala
AS-positive inclusions in amygdala (Fig. 4) and the hippocampal CA2/3 area (Fig. 5) were observed in 19.8% and 5.6%, respectively. They were associated with lesions in SNc and entorhinal cortex in 7 each (43.4%), LC in 6 (37.5%), and NBM in 5 (31%), while 2 cases each showed additional LBs in CA2/3 hippocampal area and cingulate cortex (12.4%). AD cases without involvement of the amygdala were insignificantly older than those with such lesions (mean 88.7 vs 85.4 years), their mean AD Braak stages were similar (4.7 vs 5.0).
Involvement of allocortical/limbic structures without other AS pathology
Three brains revealed AS-positive lesions in amygdala, 2 in entorhinal and one in cingulate cortex.
AD brains with AS-positive lesions in the amygdala (n = 18, 18%) either occurred isolated (n = 3) or were associated with LBs or LNs in the following regions: SNc (n = 9), LC (n = 8) and entorhinal cortex (n = 7), NBM (n = 4), cingulate cortex and CA2/3 region (n = 3 each), isocortex and oblongata (1 each). Additional inclusions were seen in 1 to 4 other brain areas (n = 3, 1, 5, and 2 cases, respectively).
In none of these patients were any parkinsonian symptoms recorded. Among the AD brains without AS-positive inclusions in the medullary nuclei, there were 6 patients aged 81–91 years (mean 88.2 years) (2 of whom showed some parkinsonian symptoms), who showed rather widespread PD-like lesions including LC and SNc in all. Therefore, at variance to the findings by the Braak group [7, 8, 9, 10, 14], PD pathology without involvement of the caudal brain stem could not be excluded. They are summarized in Table 4.
Brains with AS pathology in medullary nuclei
These cases were divided into two groups:
-
1.
Isolated lesions in medullary nuclei without other AS-positive inclusions. One case each revealed LNs or LBs in the supratrochlear/raphe nucleus and in the mdX.
-
2.
Twelve brains showed involvement of the medullary nuclei and other brain areas, but no parkinsonian signs or symptoms were mentioned in the medical records, suggesting incidental LBD or preclinical PD. The distribution of lesions is shown in Table 5.
Table 5 AD cases with AS pathology in medullary nuclei and other brain regions (“incidental Lewy body disease”?) (Form. ret. formatio reticularis, Entorh. entorhinal, dl dorsolateral nuclei, NE not examined)
Dementia with LBs
Of the 22 examined brains, 21 revealed AS-positive inclusions and lesions in the medullary nuclei (dmX nucleus, reticular formation), in LC, SNc, NBM indistinguishable from those seen in PD; LBs were further present in entorhinal and cingulate cortex in 10 cases (limbic type) and isocortical LBs in 12 neocortical cases, mainly in temporal, insular and frontal areas. (neocortical). The amygdala showed AS pathology in 16/18 cases, the CA2/3 region in 15/19 cases. The morphology and immunohistochemistry of cortical and subcortical LBs and LNs did not differ from those in PD; the pattern and severity of neuronal loss and melanin dispersion in SNc, LC and dmX were not different from that seen in PD or brain stem type of LBD.
The distribution pattern of LBs in our DLB cases differed from the staging proposed by Marui et al. [49], who only considered involvement of the amygdala (stage I), (trans-) entorhinal and insular cortex (stage II), middle, temporal and superior frontal cortex layers 1–II (stage III), and layers V–VI (stage IV), but did not consider the involvement of the brain stem. According to their staging, 4 cases of our cohort would have correlated to stage I and II, all the others to stages III and IV, but severe AD pathology (Braak stage 5) coexisted in brains of both groups.
Essential tremor
In the brain of a nondemented female aged 88 years with essential tremor but no parkinsonian symptoms, neither AS nor typical PD pathology was detected.
Controls
No AS-positive pathology was observed in any of the brains of the 20 aged non-demented individuals without neurological/psychiatric symptoms or cognitive impairment scoring CERAD 0 or A and Braak stages 2–4 (mean 3.1).
Discussion
The present data in a limited number of cases with clinically and autopsy-proven PD largely confirm the staging of pathology in both clinical and preclinical PD (incidental LBD) proposed by Del Tredici et al. [14] and Braak et al. [7, 8, 9, 10, 11]. They suggested initial involvement of the dmX and related nuclei of the “gain setting nuclei” of the lower brain stem with upward progression to SNc, basal forebrain nuclei and allocortex, with later involvement of the isocortex. The progression and distribution pattern of PD-related neuronal pathology is summarized in Figs. 6 and 7. Due to technical reasons, the olfactory system was not included in our study, and no correlations between the duration and clinical staging of illness with the morphological stages was performed. Around 20% of our PD cohort showed lesions corresponding to stage 3 by Braak et al., who did not mention clinical PD symptoms in the majority of cases in this group. Almost 30% of our PD cases with involvement of the SNc corresponded to Braak’s stage 4 [8], who mentioned clinical PD in less than 60% of their cases, while 25% each of our material showed PD pathology corresponding to Braak’s stages 5 and 6; all clinically presenting Hoehn and Yahr stages IV and V. Dementia was recorded in 8/15 (53.3%) of our PD stage 5 cases with neuritic AD Braak stages 2–4 (mean 3.2), and in 66% of PD patients with pathological stage 6, their AD stages scored 2–5 (mean 4.8). All demented PD cases stage 6 revealed LBs in entorhinal and cingulate cortex and 4 had involvement of the amygdala. These data suggest that dementia in PD is not exclusively due to coexistent severe neuritic Alzheimer pathology [41], but may also be related to cortical LB pathology [2, 30, 34, 40, 50], in particular LB formation in limbic areas [43]. However, the impact and mutual relationship between both cortical types of lesion are still under discussion.
Progress and distribution pattern of PD-related neuronal pathology. Red stage 1–2, green stage 3–4, yellow stage 5–6 [ab accessory basal nucleus of amygdala, ac accessory cortical nucleus of amygdala, ad anterodorsal nucleus of amygdala, am anteromedial nucleus of thalamus, an abducens motor nucleus, ba basal nucleus of amygdala, bn basal nucleus of Meynert, ca1 first Ammon’s horn sector, ca2 second Ammon’s horn sector, ca caudate nucleus, cc corpus callosum, ce central nuclei of amygdala, cg central gray of mesencephalon, cl claustrum, co cortical nuclei of amygdala, cr central nucleus of raphe, db nucleus of the diagonal band, dm dorsomedial hypothalamic nucleus, dr dorsal nucleus of raphe, ds decussation of superior cerebellar peduncles, dv dorsal nuclear complex of vagal nerve, en entorhinal region, fn facial motor nucleus, fo fornix, gi gigantocellular reticular nucleus, gr granular nucleus of amygdala, hn hypoglossal motor nucleus, in infundibular nucleus, ir intermediate reticular zone, lc locus coeruleus, ld laterodorsal nucleus of the thalamus, lg lateral geniculate body, li nucleus limitans thalami, lt lateral nuclei of the thalamus, md mediodorsal nuclei of thalamus, me medial nuclei of amygdala, mf medial longitudinal fasciculus, mg medial geniculate body, ml medial lemniscus, mm medial mamillary nucleus, ms medial septal nucleus, mt mamillothalamic tract, mv dorsal motor nucleus of vagal nerve, oi oliva inferior, os oliva superior, ot optic tract, pe external pallidum, pf parafascicular nucleus, ph posterior hypothalamic nucleus, pi internal pallidum, po pontine gray, pr praepositus nucleus, pu putamen, pv paraventricular nucleus, re reticular nucleus of the thalamus, rm nucleus raphes magnus, ru nucleus ruber, sb subiculum, sc superior cerebellar peduncle, sf solitary fascicle, so supraoptic nucleus, sn substantia nigra, sp subpeduncular nucleus, st nucleus of the stria terminalis, sn subthalamic nucleus, te transentorhinal region, tl lateral tuberal nucleus, tm tuberomamillary nucleus, tp tegmental pedunculopontine nucleus, vl ventrolateral nuclei of thalamus, vm ventromedial hypothalamic nucleus, vn vestibular nuclei, vt dopaminergic nuclei of ventral tegmentum (paranigral nucleus and pigmented parabrachial nucleus), zi zona incerta]
Progression of PD-related pathology (modified from [8]). Asterisks: may not be involved in rare cases of AD without/occasionally with mild parkinsonian symptoms and AS-positive lesions equivalent to stages 3 and 4
In 7 of 11 demented patients with autopsy-proven fully developed AD neuropathology revealed PD-typical changes in medullary, pontine and mesencephalic nuclei with considerable neuronal loss and depigmentation in SNc, corresponding to stage 3, while one third of these brains showed additional AS-positive pathology in NBM with or without LBs in hippocampal CA2/3 areas and entorhinal cortex, equivalent to stage 4 [7, 8, 9, 11, 14]. Since none of these patients showed any parkinsonian signs and symptoms, they are considered “incidental LBD” or pre/subclinical PD that obviously follow similar topographic involvement and progression as symptomatic PD.
While the majority of symptomatic PD cases of our cohort thus fulfilled the morphological criteria of progressed PD stages proposed by Braak et al. [7, 8, 9] (Fig. 5), in presymptomatic cases (incidental LB disease), earlier stages 3 and 4 were observed (Table 5).
Although the Braak group proposed a stereotypic topographic expansion pattern of the lesions in both PD [7, 8, 9, 11] and in AD [4], deviations in the topographic distribution and extension have been observed in both these disorders [24, 39, 57]. Such exceptions are to be considered in a small number of cases in our cohort of autopsy-proven AD, where LB pathology and neurodegenerative lesions were observed in LC, SNc and NBM indistinguishable from PD stage 3, while in others they were associated with AS-positive lesions in amygdala and/or entorhinal cortex and cingulate area, as seen in PD stage 4 [7, 8, 9]. Since in 2 of these 6 demented patients additional parkinsonian signs or rigidity were reported, they may represent early stages of PD or incidental LBD. However, in these cases definite AS-positive inclusions or cellular lesions in the medullary nuclei, suggested to represent classical initial lesions in PD, were not detected (Tables 2, 3). The question of whether such rare cases represent atypical forms of preclinical or symptomatic PD, or there may be exceptions of the “stereotypic” development of PD pathology in the brain stem [7, 8, 9, 14] needs further clinico-pathological examination. Parkkinen et al [55], in a large series of elderly brains, recently discovered 6 subjects with AS pathology only in the SN without involvement of the lower brain stem. In contrast to our findings, all were free of AD pathology. Since they showed no history of neurological or psychiatric disorders, they argued that incidental LB pathology may occur solely in the SN.
The nosological relationship between DLB, PD, and AD are under discussion [2, 12, 35, 42, 51]. It should be emphasized that in 22 of 23 personal cases of autopsy-proven DLB, the morphology and distribution pattern of AS-positive subcortical pathology and the quality of cortical LBs did not differ from classical PD (brain stem type of LBD), while there were only differences in the quantity and distribution of cortical LBs. These similarities were independent of coexistent neuritic AD pathology, while only one single patient with limbic type of LBV/AD (male aged 83 years with severe dementia without parkinsonian symptoms) revealed no PD-like pathology in the medullary nuclei. These data, suggesting close morphological relationship between DLB and classical PD, also need further confirmation and validation.
LBs and other AS-positive inclusions in various cortical and subcortical brain areas have been reported in both aging brain and in up to 70% of sporadic AD, with involvement of the amygdala in 15% to over 50% (see above). In none of these patients had parkinsonian signs and symptoms been recorded. In 48.2% of a large cohort of demented patients with autopsy-proven AD and in a series of age-matched controls without clinical and pathological abnormalities, no AS-positive lesions were observed in any of the examined brain areas. On the other hand, such lesions in various brain areas were detected in 51.8% of the 109 autopsy-proven AD brains, only 3 with a history of additional clinical signs of parkinsonism. The majority of these lesions were observed in the pontine and mesencephalic catecholaminergic nuclei (34% in SNc and 28% in LC), in amygdala and entorhinal cortex (19.6% and 19.0%, respectively), in NBM and medulla oblongata (14–16%), in cingulate cortex (9%), and in CA2/3 hippocampal area (5.6%), but only in 2% in neocortex. While AS-positive inclusions were only observed in 2 AD brains in the medullary nuclei (dmX and supratrochlear nucleus/raphe nucleus of oblongata, respectively), most other inclusions occurred in several brain areas, e.g., in LC and SNc, with or (mostly) without involvement of the medullary nuclei. Affection of the amygdala was much less frequent than previously reported [27, 29, 47, 55], and similar to the incidence in another small cohort [15] (19.8% vs 15%). Additional AS inclusions in other brain areas, e.g., SNc, LC, NBM and allocortex, however, were more frequent in our material than in a previous sample [15]. Only 2 of these demented patients with LB-pathology in amygdala, SNC, LC, and entorhinal cortex but without medullary PD-like lesions, had a history of some parkinsonian signs and symptoms (rigidity, gait disorder). As in another cohort [15], the mean age at death was similar between cases with and without involvement of the amygdala (88.7 vs. 85.4 years), the MMSE scores (not shown) and the Braak AD stages (4.7 vs. 5.0) suggesting that AS-positive lesions in the amygdala cannot be predicted by disease severity/cognitive dysfunction, and patient’s age. It should be emphasized that interpretation of abnormal accumulations may be influenced by the conditioning of staining, the antibodies used, of fixation. To elucidate possible pathogenic relations between LB pathology in AD brain with extrapyramidal signs and symptoms, further clinico-pathological studies are in progression.
In conclusion, neuropathological studies using AS-immunohistochemistry in a cohort of patients with clinically and autopsy-proven PD and of incidental LBD/presymptomatic PD confirmed the staging of PD-related pathology with upward progression from medullary nuclei via pons, midbrain to the cortex proposed by Del Tredici et al. [14] and Braak et al. [7, 8, 9, 10, 11] (Fig. 6). While PD cases with extensive damage to SNc and Hoehn and Yahr stages IV–V showed AS-positive lesions corresponding to Braak stages 4–6, in some cases with clinical PD and in some AD brains the PD lesions extended to SNc, corresponding to stage 3. At variance to the staging of PD pathology proposed by Braak et al. [7, 8, 9, 10, 11], these data suggest that sensori-motor PD symptoms may already occur with lesions equivalent to pathological stage 3 (Fig. 7), and may not necessarily extend to stage 4.
In some AD cases without parkinsonian symptoms or incidental LBD, the distribution of PD lesions was equivalent to stages 3 and 4. However, we observed some AD cases without or, rarely, with additional parkinsonian signs showing PD-typical pathology in pons and midbrain with or without additional involvement of the allocortex in which no medullary lesions were detected. Whether they represent atypical forms of (sub-) clinical PD or indicate deviations from the proposed stereotypic topographical expansion pattern of AS pathology remains to be determined. The quality and distribution pattern of subcortical PD-related lesions in a small number of DLB cases were identical to those seen in PD, suggesting close morphological relations between both disorders. The staging of LB pathology proposed for DLB [49], correlating stages I and II predominantly with the limbic type, was not used in our cohort, since this staging does not consider brain stem involvement and coexistent neuritic AD pathology was present in at least one third of our cases. LB pathology was not only present in PD and related disorders, but was also observed in almost 52% of a cohort of cases with autopsy-proven AD, but parkinsonian signs had been reported in only 3 patients. The AS-positive lesions mainly involve pontine and mesencephalic nuclei usually affected in PD, less often allocortical and medullary areas, in particular the amygdala, the involvement of which appears independent of age and severity of AD pathology. In view of recent and partly controversial data on the incidence and topography of AS pathology in PD, AD and DLB, its pathogenesis, evolution pattern and clinical impact in these disorders need further elucidation.
References
American Psychiatric Association (1999) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington
Apaydin H, Ahlskog JE, Parisi JE, Boeve BF, Dickson DW (2002) Parkinson disease neuropathology: later-developing dementia and loss of the levodopa response. Arch Neurol 59:102–112
Arai Y, Yamazaki M, Mori O, Muramatsu H, Asano G, Katayama Y (2001) α-Synuclein-positive structures in cases with sporadic Alzheimer’s disease: morphology and its relationship to tau aggregation. Brain Res 888:287–296
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82:239–259
Braak H, Braak E, Yilmazer D, Vos RA de, Jansen EN, Bohl J (1996) Pattern of brain destruction in Parkinson’s and Alzheimer’s diseases. J Neural Transm 103:455–490
Braak H, Braak E, Yilmazer D, Vos RA de, Jansen EN, Bohl J, Jellinger K (1994) Amygdala pathology in Parkinson’s disease. Acta Neuropathol 88:493–500
Braak H, Del Tredici K, Bratzke H, Hamm-Clement J, Sandmann-Keil D, Rüb U (2002) Staging of the intracerebral inclusion body pathology associated with idiopathic Parkinson’s disease (preclinical and clinical stages). J Neurol 249(Suppl 3):III/1–5
Braak H, Del Tredici K, Rüb U, Vos RA de, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Braak H, Rüb U, Braak E (2000) Neuroanatomie des Morbus Parkinson. Veränderungen des neuronalen Zytoskeletts in nur wenigen für den Krankheitsprozess empfänglichen Nervenzelltypen führen zur progredienten Zerstörung umschriebener Bereiche des limbischen und des motorischen Systems. Nervenarzt 71:459–469
Braak H, Rüb U, Gai WP, Del Tredici K (2003) Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm. doi:10.1007/s00702-002-0808-2 (published online March 5, 2003)
Braak H, Rüb U, Sandmann-Keil D, Gai WP, Vos RA de, Jansen Steur EN, Arai K, Braak E (2000) Parkinson’s disease: affection of brain stem nuclei controlling premotor and motor neurons of the somatomotor system. Acta Neuropathol 99:489–495
Brown DF, Dababo MA, Bigio EH, Risser RC, Eagan KP, Hladik CL, White CL 3rd (1998) Neuropathologic evidence that the Lewy body variant of Alzheimer disease represents coexistence of Alzheimer disease and idiopathic Parkinson disease. J Neuropathol Exp Neurol 57:39–46
Damier P, Hirsch EC, Agid Y, Graybiel AM (1999) The substantia nigra of the human brain. II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain 122:1437–1448
Del Tredici K, Rüb U, De Vos RA, Bohl JR, Braak H (2002) Where does parkinson disease pathology begin in the brain? J Neuropathol Exp Neurol 61:413–426
DeLucia MW, Cookson N, Dickson DW (2002) Synuclein-immunoreactive Lewy bodies are detected in the amygdala in less than 20% of Alzheimer’s disease (AD) cases. J Neuropathol Exp Neurol 61:454
Dickson DW (2001) α-Synuclein and the Lewy body disorders. Curr Opin Neurol 14:423–432
Duda JE, Giasson BI, Mabon ME, Lee VM, Trojanowski JQ (2002) Novel antibodies to synuclein show abundant striatal pathology in Lewy body diseases. Ann Neurol 52:205–210
Eadie MJ (1963) The pathology of certain medullary nuclei in parkinsonism. Brain 86:781–795
Fearnley JM, Lees AJ (1994) Pathology of Parkinson disease. In: Calne DB (ed) Neurodegenerative diseases. Saunders, Philadelphia, pp 545–554
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-Mental” state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Forno LS (1996) Neuropathology of Parkinson’s disease. J Neuropathol Exp Neurol 55:259–272
Gai WP, Blumbergs PC, Geffen LB, Blessing WW (1992) Age-related loss of dorsal vagal neurons in Parkinson’s disease. Neurology 42:2106–2111
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
Gertz HJ, Xuereb J, Huppert F, Brayne C, McGee MA, Paykel E, Harrington C, Mukaetova-Ladinska E, Arendt T, Wischik CM (1998) Examination of the validity of the hierarchical model of neuropathological staging in normal aging and Alzheimer’s disease. Acta Neuropathol 95:154–158
Gibb WR, Lees AJ (1989) The significance of the Lewy body in the diagnosis of idiopathic Parkinson’s disease. Neuropathol Appl Neurobiol 15:27–44
Halliday GM, Li YW, Blumbergs PC, Joh TH, Cotton RG, Howe PR, Blessing WW, Geffen LB (1990) Neuropathology of immunohistochemically identified brain stem neurons in Parkinson’s disease. Ann Neurol 27:373–385
Hamilton RL (2000) Lewy bodies in Alzheimer’s disease: a neuropathological review of 145 cases using α-synuclein immunohistochemistry. Brain Pathol 10:378–384
Hansen L, Salmon D, Galasko D, et al (1990) The Lewy body variant of Alzheimer’s disease: a clinical and pathologic entity. Neurology 40:1–8
Harding AJ, Stimson E, Henderson JM, Halliday GM (2002) Clinical correlates of selective pathology in the amygdala of patients with Parkinson’s disease. Brain 125:2431–2445
Haroutunian V, Serby M, Purohit DP, Perl DP, Marin D, Lantz M, Mohs RC, Davis KL (2000) Contribution of Lewy body inclusions to dementia in patients with and without Alzheimer disease neuropathological conditions. Arch Neurol 57:1145–1150
Holstege G (1996) The somatic motor system. Prog Brain Res 107:9–26
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Hughes AJ, Daniel SE, Ben-Shlomo Y, Lees AJ (2002) The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain 125:861–870
Hurtig HI, Trojanowski JQ, Galvin J, Ewbank D, Schmidt ML, Lee VM, Clark CM, Glosser G, Stern MB, Gollomp SM, Arnold SE (2000) α-Synuclein cortical Lewy bodies correlate with dementia in Parkinson’s disease. Neurology 54:1916–1921
Ince PG, Perry EK, Morris CM (1998) Dementia with Lewy bodies. A distinct non-Alzheimer dementia syndrome? Brain Pathol 8:299–324
Ishizawa T, Mattila P, Davies P, Wang D, Dickson DW (2003) Colocalization of tau and α-synuclein epitopes in Lewy bodies. J Neuropathol Exp Neurol 62:389–397
Jellinger K (1991) Pathology of Parkinson’s disease. Changes other than the nigrostriatal pathway. Mol Chem Neuropathol 14:153–197
Jellinger KA (2001) The pathology of Parkinson’s disease. Adv Neurol 86:55–72
Jellinger KA, Bancher C (1998) Neuropathology of Alzheimer’s disease: a critical update. J Neural Transm Suppl 54:77–95
Jellinger KA, Mizuno Y (2003) Parkinson disease. In: Dickson DW, et al (eds) Neurodegeneration and dementias. ISN Press, Los Angeles (in press)
Jellinger KA, Seppi K, Wenning GK, Poewe W (2002) Impact of coexistent Alzheimer pathology on the natural history of Parkinson’s disease. J Neural Transm 109:329–339
Jellinger KA, Seppi K, Wenning GK (2003) Neuropathologic changes in Parkinson disease with late onset of dementia. (Letter) Arch Neurol 60:452–454
Kövari E, Gold G, Herrmenn FR, Canuto A, Hof PK, Bouras G, Giannakopoulos P (2003) Lewy body densities in the entorhinal and anterior cingulate cortex predict cognitive deficits in Parkinson disease. Acta Neuropathol 106:83–88
Lewy F (1913) Zur pathologischen Anatomie der Paralysis agitans. Dtsch Z Nervenheilkd 50:50–55
Lewy FH (1912) Paralysis agitans. Pathologische Anatomie. In: Lewandowsky M (ed) Handbuch der Neurologie. Springer, Berlin, pp 920–933
Lippa CF, Fujiwara H, Mann DM, Giasson B, Baba M, Schmidt ML, Nee LE, O’Connell B, Pollen DA, St George-Hyslop P, Ghetti B, Nochlin D, Bird TD, Cairns NJ, Lee VM, Iwatsubo T, Trojanowski JQ (1998) Lewy bodies contain altered α-synuclein in brains of many familial Alzheimer’s disease patients with mutations in presenilin and amyloid precursor protein genes. Am J Pathol 153:1365–1370
Lippa CF, Schmidt ML, Lee VM, Trojanowski JQ (1999) Antibodies to α-synuclein detect Lewy bodies in many Down’s syndrome brains with Alzheimer’s disease. Ann Neurol 45:353–357
Lowe J, Leigh PN (2002) Disorders of movement and system degenerations. In: Graham D, Lantos PL (eds) Greenfield’s neuropathology, 7th edn. Arnold, London, pp 325–430
Marui W, Iseki E, Nakai T, Miura S, Kato M, Ueda K, Kosaka K (2002) Progression and staging of Lewy pathology in brains from patients with dementia with Lewy bodies. J Neurol Sci 195:153–159
Mattila PM, Rinne JO, Helenius H, Dickson DW, Roytta M (2000) α-Synuclein-immunoreactive cortical Lewy bodies are associated with cognitive impairment in Parkinson’s disease. Acta Neuropathol 100:285–290
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, Lennox G, Quinn NP, Edwardson JA, Ince PG, Bergeron C, Burns A, Miller BL, Lovestone S, Collerton D, Jansen EN, Ballard C, Vos RA de, Wilcock GK, Jellinger KA, Perry RH (1996) Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 47:1113–1124
Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, Vogel FS, Hughes JP, Belle G van, Berg L (1991) The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41:479–486
Nieuwenhuys R (1996) The greater limbic system, the emotional motor system and the brain. Prog Brain Res 107:551–580
Olszewski J, Baxter D (1982) Cytoarchitecture of the human brain stem, 2nd edn. Karger, Basel
Parkkinen L, Soininen H, Alafuzoff I (2003) Regional distribution of α-synuclein pathology in unimpaired aging and Alzheimer disease. J Neuropathol Exp Neurol 62:363–367
Pearce RK, Hawkes CH, Daniel SE (1995) The anterior olfactory nucleus in Parkinson’s disease. Mov Disord 10:283–287
Perl DP, Purohit DP, Haroutunian V (1997) Clinicopathologic correlations of the Alzheimer disease staging system introduced by Braak and Braak. J Neuropathol Exp Neurol 56:577
Perry RH, Irving D, Tomlinson BE (1990) Lewy body prevalence in the aging brain: relationship to neuropsychiatric disorders, Alzheimer-type pathology and catecholaminergic nuclei. J Neurol Sci 100:223–233
Schmidt ML, Martin JA, Lee VM, Trojanowski JQ (1996) Convergence of Lewy bodies and neurofibrillary tangles in amygdala neurons of Alzheimer’s disease and Lewy body disorders. Acta Neuropathol 91:475–481
Trembath Y, Rosenberg C, Ervin JF, Schmechel DE, Gaskell P, Pericak-Vance M, Vance J, Hulette CM (2003) Lewy body pathology is a frequent co-pathology in familial Alzheimer’s disease. Acta Neuropathol 105:484–488
Wakabayashi K, Toyoshima Y, Awamori K, Anezaki T, Yoshimoto M, Tsuji S, Takahashi H (1999) Restricted occurrence of Lewy bodies in the dorsal vagal nucleus in a patient with late-onset parkinsonism. J Neurol Sci 165:188–191
Mikolaenko L, Kwan CH, O’Brien R, Petnikov O, Troncoso JC (2003) Abstr. 6th International Conference AD|PD 2003; Seville, Spain, 8–12 May 2003; p 133
Acknowledgements
The author thanks the medical staff of Lainz Hospital, Wienerwald Geriatric Hospital, Otto Wagner Hospital, Vienna, and the Wagner-Jauregg Hospital, Linz, for clinical data, the pathologists of these hospital for autopsy reports and brain material, Mrs. V. Rappelsberger for excellent laboratory work, and E. Mitter-Ferstl, PhD, for secretarial and computer work. The study was supported by the Society for Support of Research in Experimental Neurology, Vienna, Austria.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00401-003-0780-4
An erratum to this article is available at http://dx.doi.org/10.1007/s00401-003-0780-4.
Rights and permissions
About this article
Cite this article
Jellinger, K.A. α-Synuclein pathology in Parkinson’s and Alzheimer’s disease brain: incidence and topographic distribution—a pilot study. Acta Neuropathol 106, 191–202 (2003). https://doi.org/10.1007/s00401-003-0725-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-003-0725-y