Abstract
Angiotensin II (Ang II), a potent precursor of hypertrophy and heart failure, upregulates neuronal nitric oxide synthase (nNOS or NOS1) in the myocardium. Here, we investigate the involvement of type 1 and 2 angiotensin receptors (AT1R and AT2R) and molecular mechanisms mediating Ang II-upregulation of nNOS. Our results showed that pre-treatment of left ventricular (LV) myocytes with antagonists of AT1R or AT2R (losartan, PD123319) and ROS scavengers (apocynin, tiron or PEG-catalase) blocked Ang II-upregulation of nNOS. Surface biotinylation or immunocytochemistry experiments demonstrated that AT1R expression in plasma membrane was progressively decreased (internalization), whereas AT2R was increased (membrane trafficking) by Ang II. Inhibition of AT1R or ROS scavengers prevented Ang II-induced translocation of AT2R to plasma membrane, suggesting an alignment of AT1R-ROS-AT2R. Furthermore, Ang II increased eNOS-Ser1177 but decreased eNOS-Thr495, indicating concomitant activation of eNOS. Intriguingly, ROS scavengers but not AT2R antagonist prevented Ang II-activation of eNOS. NOS inhibitor (L-NG-Nitroarginine Methyl Ester, L-NAME) or eNOS gene deletion (eNOS−/−) abolished Ang II-induced membrane trafficking of AT2R, nNOS protein expression and activity. Mechanistically, S-nitrosation of AT2R was increased by sodium nitroprusside (SNP), a NO donor. Site-specific mutagenesis analysis reveals that C-terminal cysteine 349 in AT2R is essential in AT2R translocation to plasma membrane. Taken together, we demonstrate, for the first time, that Ang II upregulates nNOS protein expression and activity via AT1R/ROS/eNOS-dependent S-nitrosation and membrane translocation of AT2R. Our results suggest a novel crosstalk between AT1R and AT2R in regulating nNOS via eNOS in the myocardium under pathogenic stimuli.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The renin–angiotensin system (RAS) exerts pleiotropic roles in normal cardiovascular functions and in various cardiovascular diseases. Angiotensin II (Ang II) is the major active peptide that is produced locally and systematically that mediates the effects of RAS by disturbing intracellular ion homeostasis, oxidative stress and abnormal signaling pathways, consequently leading to hypertension, hypertrophy, heart failure and atherosclerosis [25, 33, 37, 38]. The multitudinous effects of Ang II are predominantly mediated by type 1 Ang II receptor (AT1R) activation of various signaling cascades including NADPH oxidase and resultant reactive oxygen species (ROS) and protein kinases trigger an array of diverse signaling pathways to promote cardiovascular pathogenesis [14, 28]. On the other hand, type 2 Ang II receptor (AT2R) counteracts the detrimental effects of AT1R and cardiac oxidase-derived oxidative stress and protects the heart from disease development [17, 20, 26]. In fact, AT2R exerts these functions by activating protein phosphatases, protein tyrosine phosphatase and protein phosphatase 2A, and dephosphorylation of downstream effector proteins modifies their activities. Alternatively, AT2R are well established to activate nitric oxide synthase (NOS)/NO—cyclic guanosine 3′,5′-monophosphate (cGMP) signaling to exert protective effects in cardiovascular system [13, 20, 26].
The general consensus is that endothelial NOS (eNOS) is the downstream target of AT2R [24, 26]. However, despite that neuronal NOS (nNOS) is the predominant NOS that regulates cardiac contractility and intracellular Ca2+ homeostasis in cardiac myocytes, the involvement of nNOS in AT2R-mediated downstream signaling is unknown. nNOS differs from eNOS in the subcellular location and it plays pivotal roles in regulating intracellular Ca2+ handlings, redox homeostasis and cardiac contraction [1, 34, 40, 42, 44]. Importantly, whilst eNOS is “uncoupled” and becomes the source of ROS [35] or it is downregulated in the failing heart [39], nNOS is upregulated and prevents the myocardium from oxidative stress, attenuates adverse remodeling and delays the progression towards heart failure [2, 9, 19].
Recently, our results have shown that Ang II increases nNOS protein expression and activity in isolated cardiac myocytes, which in turn, reduces NADPH oxidase production of cellular superoxide and promotes diastolic function [18]. In the present study, we examined molecular mechanisms mediating Ang II-stimulation of nNOS.
Materials and methods
Animals and left ventricular myocytes
LV myocytes were isolated from Sprague–Dawley rats (12 weeks old, male) and from eNOS+/+ and eNOS−/− mice (Tohoku University Graduate School of Medicine) using a standard enzymatic dispersion technique. The rats were anesthetized with pentobarbital sodium (30 mg/kg, i.p.) and the mice were humanely killed with cervical dislocation. Briefly, the hearts from rats and mice were extracted and mounted onto the Langendorff perfusion system and were perfused with a nominal Ca2+ -free solution (in mM; NaCl 135, KCl 5.4, MgCl2 3.5, glucose 5, HEPES 5, Na2HPO4 0.4, Taurine 20 at a pH of 7.4), followed by a further 8 min with enzymes added (collagenase, 1 mg/ml, Worthington Biochemical Co.; protease, 0.133 mg/ml, Sigma-Aldrich; BSA 1.65 mg/ml; Ca2+, 0.05 mM). Myocytes were harvested from LV chamber of the heart following further 5- and 10-min digestion periods in a separate flask containing fresh collagenase-only solution, washed and re-suspended in storage solution (in mM; NaCl 120, KCl 5.4, MgSO4 5, CaCl2 0.2, Na-pyruvate 5, glucose 5.5, Taurine 20, HEPES 10, Mannitol 29, pH 7.4, NaOH). The myocyte suspension was stored at RT and cells were used within 8 h of isolation. The study protocol was in accordance with the Guide for the Care and Use of Laboratory Animals by the US National Institutes of Health (NIH Publication No. 85–23, revised 1996), and also conforms to the Institutional Animal Care and Use Committee (IACUC) in Seoul National University (IACUC approval No.: SNU-101012-3).
qRT-PCR
Total RNA was extracted using a TRizol reagent (Invitrogen) and its purified concentration was determined spectrophotometrically at 260 nm. cDNA was produced using SuperScript™ III First-Strand Synthesis System (Invitrogen) according to manufacturer’s instructions. Primers were: GAPDH (forward, 5′-GCC AAG GCT GTG GGC AAG GT-3′; reverse, 5′-GAG CAA TGC CAG CCC CAG CA-3′), nNOS (forward, 5′-CTG CAA AGC CCT AAG TCC AG-3′; reverse, 5′-AGT GTT CCT CTC CTC CAG CA-3′). cDNAs were amplified with SYBR green (TOPreal™ qPCR 2X PreMIX) using a real-time PCR system (Applied Biosystems 7500 Real-time PCR) under the conditions: 95 °C for 10 min, 40 cycles at 95 °C for 10 s, 60 °C for 15 s and 72 °C for 15 s. Specificity of amplification products was assessed by melting curve analysis. Relative gene expression was calculated using the comparative threshold (C t) method (\(2^{{ - \Delta \Delta C_{\text{t}} }}\)).
Immunoblotting
Proteins were extracted from LV myocytes using lysis buffer containing 0.5 M EDTA, 25 mM Tris–HCl, 150 mM NaCl, 0.5 % CHAPS or 1 % Triton X-100 with phosphatase inhibitor and protease inhibitor cocktail (Roche), pH 7.4. After boiling at 95 °C for 5 min, lysates were fractionated by SDS/PAGE and transferred to PVDF membranes in 25 mM Tris, 192 mM glycine, 0.01 % SDS, 20 % methanol. Membranes were blocked in 1X TBS containing 1 % Tween-20 and 5 % BSA (blocking solution) for 1 h at RT with gentle rocking. Membranes were then incubated overnight at 4 °C with nNOS (Santa Cruz Biotechnology), eNOS (BD Transduction Laboratories), phospho-eNOS Ser1177, phospho-eNOS Thr495, Akt, Phospho-Akt Ser473 (Cell Signaling Technology), AT1R, AT2R, GAPDH (Santa Cruz Biotechnology) and Na+-K+ ATPase (Abcam) primary antibodies followed by relevant secondary antibodies after washing. Blots were developed using ECL Plus western blotting detection reagents (Amersham Bioscience). Membranes were stripped of antibodies using stripping buffer (Pierce Chemical) for 15 min at RT. The relative densities were calculated by normalizing each blot with GAPDH.
Nitrite assay
NO production was detected by measuring nitrite content in LV myocytes using NO assay kit (Griess Reagent System). LV myocytes were homogenized with Krebs Henseleit solution (NaCl 118 mM, NaHCO3 25 mM, Glucose 5.6 mM, KCl 4.7 mM, KH2PO4 1.2 mM, MgSO4 1.1 mM, CaCl2 1.8 mM). Protein concentration was determined by Bradford method. Sodium nitrite (Sigma) was used as the standard. The samples were added and mixed with sulfanilamide solution and incubated for 5–10 min at RT in the dark. The same volume of naphthylethylenediamine dihydrochloride (Sigma) solution was added to all wells and incubated for 5–10 min at RT, protected from light. Absorbance of the mixture at 540 nm was measured with a microplate reader, PowerWave™ XS Microplate Spectrophotometer (BioTek Instruments, Winooski, VT, USA).
AT2R DNA constructs
The AT2R wild type was cloned into pEGFP-N1 as described previously [41]. Cysteine mutants at C70A, C71A, C319A, C349A in intracellular region of AT2R were generated using QuikChange XL Site-Directed Mutagenesis Kit (Agilent Technologies). The DNA sequences were confirmed by direct sequencing.
Cell culture and transient transfection
HEK293T cells were cultured in Dulbecco’s modified Eagle’s medium (Gibco), supplemented with 10 % fetal bovine serum (FBS). Cells were maintained at 37 °C and 5 % CO2. Cells were transiently transfected with 500 ng of AT2R-GFP wild type (WT), AT2R C70A-GFP, AT2R C71A-GFP, AT2R C319A-GFP and AT2R C349A-GFP mutants for 48 h using X-tremeGENE HP DNA transfection Reagent (Roche) according to manufacturer’s instructions.
Immunocytochemistry and confocal imaging
Isolated LV myocytes were attached to laminin (Sigma)-coated coverslips for 1 h at 37 °C. After treated with Ang II, L-NAME + Ang II or SNP for 30 min, cells were fixed with 4 % PFA for 30 min in RT and washed with PBS for three times. Fixed cells (not permeabilized) were incubated in blocking solution (5 % FBS in PBS) for 1 h, followed by an incubation with extracellular membrane targeting anti-rabbit AT2R polyclonal antibody (1:100, Alomone labs) for overnight at 4 °C. After three washes in PBS for 10 min, cells were incubated with Alexa Fluor 488-conjugated goat anti-rabbit (1:500, Invitrogen/Molecular Probes) for 1 h. Finally, the cells were mounted with fluorescent mounting medium (Vectashield).
Similarly, HEK 293T cells (transfected with GFP-tagged wild type or mutant AT2R) were attached to twelve-well plates pre-coated with poly-l-lysine and were randomly assigned for control or SNP (10 μM for 30 min) groups. Cells were fixed with 4 % PFA for 30 min, followed by Alexa Fluor 555 conjugated Wheat Germ Agglutinin (WGA, 5.0 ug/mL, Invitrogen/Molecular Probes) and 4′,6-Diamidino-2-phenylindole (DAPI, Sigma) for 1 min in RT. The immunostained LV myocytes and AT2R transfected HEK293T cells were imaged using a laser scanning confocal microscope (Olympus, FluoView 1000) with an oil immersion objective of 100×.
Surface biotinylation
Densities of AT1R and AT2R in the plasma membrane following Ang II treatment (0–30 min) were detected in rat LV myocytes using surface biotinylation method. 0.25 mg/mL Sulfo-NHE-SS-Biotin (Pierce) in PBS was added to the cell suspension and gently shaken for 1 h at 4 °C. After quenching free biotin by adding 50 mM Tris–Cl (pH 7.4), LV myocytes were lysed in lysis buffer (0.5 M EDTA, 25 mM Tris–Cl pH 7.4, 150 mM NaCl, 1 % Triton X-100) and centrifuged at 13,000g for 10 min. Supernatants were incubated with solution containing NeutrAvidin Agarose Resins (Pierce) for 1 h at RT. Beads were washed two times with 0.1 % TBS-T. Avidin-binding proteins were eluted with elution buffer (62.5 mM Tris–Cl pH 6.8, 1 % SDS, 10 % glycerol, 50 mM DTT) and loaded onto an SDS 10 % polyacrylamide gel. Immunoblotting was performed by AT1R (Santa Cruz Biotechnology), AT2R (Santa Cruz Biotechnology) primary antibody. AT2R surface densities in the plasma membrane following SNP treatment (30 min) were detected in AT2R-transfected HEK293T cells under the same condition. Membrane expression of AT2R protein in plasma membrane was confirmed with GFP (Invitrogen/Molecular probes) antibody in immunoblotting.
S-nitrosation
S-nitrosation of AT2R was analyzed by biotin-switch method. S-nitrosated cysteine residues of AT2R were covalently labeled with maleimide-biotin according to the manufacturer’s instructions (S-nitrosated protein detection assay kit; Cayman Chemical). Biotin-conjugated proteins were then isolated with Streptavidin-coupled Dynabeads (Life Technologies) overnight at 4 °C. After washing with PBS-T (buffer composition—50 mM Tris–Cl, pH 8.0; 150 mM NaCl, 1 mM EDTA and 1 % Tween 20), the proteins bound to the beads were eluted by boiling for 10 min in sodium dodecyl sulfate containing buffer and the S-nitrosated proteins were subjected to SDS-PAGE and western blot analysis with AT2R antibody. S-nitrosation of AT2R was compared in LV myocytes before and after SNP treatment.
Statistics
Data were expressed as mean ± SE and n indicates the number of samples used. For all comparisons, primary cells were obtained from a minimum of three hearts per treatment group per protocol. Data were indicated as n paired or unpaired Student’s t test that was used for statistical analysis. A value of P < 0.05 was considered to be statistically significant.
Results
AT1R, intracellular ROS and AT2R mediates Ang II-stimulation of nNOS protein expression
As shown in Fig. 1a, Ang II (1 μM, 3 h) significantly increased the protein expression of nNOS in rat LV myocyte homogenates (P = 0.02, n = 7). Unlike nNOS, eNOS protein expression was not affected by Ang II (P = 0.9, n = 7, Fig. 1b), suggesting that nNOS is upregulated by Ang II in cardiac myocytes. Pre-treatment of LV myocytes with AT1R antagonist, losartan (1 μM, 30 min followed by co-incubation with Ang II 1 μM, 3 h), abolished Ang II-stimulation of nNOS protein (P = 0.005, between Ang II and losartan + Ang II, n = 5, respectively, Fig. 1a).
Inhibition of AT1R and intracellular ROS reduced Ang II-stimulation of nNOS mRNA and protein expressions and NO production in LV myocytes. a Isolated LV myocytes were incubated with Ang II (1 μM), Losartan (1 μM) and Losartan + Ang II for 3 h. nNOS protein was detected by western blotting. GAPDH was used as a loading control. b eNOS protein expression was not affected after Ang II treatment (3 h). c Real-time PCR results showed that apocynin (100 μM) or tiron (1 mM) pre-treatment blocked Ang II-stimulation of nNOS mRNA. Mean ratios of nNOS mRNA relative to control (GAPDH) in control and Ang II-treated LV myocyte homogenates. d Apocynin, tiron and PEG-catalase (352 Units/ml) pre-treatment prevented Ang II-induced nNOS protein expression. e NO production (nitrite assay) was greater in LV myocyte homogenates following Ang II treatment (3 h). Losartan, apocynin or tiron abolished the effect of Ang II on NO production
Intracellular ROS are upstream regulators of transcription of proteins and are associated with cardiac NOS protein expression and activity [5, 32]. Therefore, we tested whether intracellular ROS subsequent to AT1R activation (NADPH oxidase, xanthine oxidoreductase or mitochondria) is involved in Ang II-upregulation of nNOS. Figure 1c shows that Ang II (1 μM, 3 h) increased mRNA expression of nNOS in LV myocyte homogenates (P = 0.04, n = 4). Pre-incubation of LV myocytes with apocynin (100 μM), an antioxidant that has been shown to inhibit NADPH oxidase or superoxide scavenger, tiron (1 mM) (30 min followed by co-incubation with Ang II for 3 h) abolished Ang II-stimulation of nNOS mRNA (P = 0.04 between Ang II and Ang II + apocynin, n = 4; P = 0.009 between Ang II and tiron + Ang II, n = 4, Fig. 1c). Furthermore, pre-treatment of LV myocytes with apocynin, tiron or H2O2 catalase-polyethylene glycol (PEG-catalase, 352 Units/ml) abolished Ang II-induced increases in nNOS protein expression (P < 0.001 between Ctr and Ang II, n = 10; P = 0.002 between Ang II and Ang II + apocynin, n = 6; P < 0.001 between Ang II and Ang II + tiron, n = 6; P = 0.03 between Ang II and Ang II + PEG-catalase, n = 5, Fig. 1d). Importantly, losartan, apocynin and tiron blocked Ang II-induced increase in NO production, respectively (P = 0.004 between Ang II and losartan + Ang II, n = 12; P = 0.001, Ang II and apocynin + Ang II, n = 6; P < 0.0001, between Ang II and tiron + Ang II, n = 5, Fig. 1e).
Involvement of AT2R in Ang II-induced nNOS protein expression was examined by incubating LV myocytes with a specific antagonist of AT2R, PD123319. PD123319 pre-incubation (1 μM, 30 min followed by co-incubation with Ang II for 3 h) blocked Ang II-induced increase in nNOS protein expression (P < 0.001 between Ang II and Ang II + PD123319, n = 5, respectively, Fig. 2a) and NO production (P = 0.001 between Ang II and PD123319 + Ang II, n = 12, Fig. 2b). Conversely, AT2R agonist, CGP 42112A (1 μM), significantly increased nNOS protein expression in LV myocytes (P = 0.04, n = 4, Fig. 2c).
AT2R antagonist blocks Ang II-stimulation of nNOS protein expression and activity in LV myocytes. a Isolated LV myocytes were pre-incubated with AT2R antagonist, PD123319 (1 μM). PD123319 blocked Ang II-stimulation of nNOS protein expression. b PD123319 prevented Ang II-induced increase in NO production. c AT2R agonist, CGP42112A (1 μM, 3 h), significantly increased nNOS protein expression
Taken together, these results suggest that AT1R, intracellular ROS and AT2R are pivotal upstream regulators of nNOS protein expression and activity in cardiac myocytes.
AT1R and intracellular ROS determine AT2R translocation to plasma membrane
Involvement of both pathogenic AT1R/ROS and counterbalancing AT2R in Ang II-stimulation of nNOS suggest that there maybe crosstalks between Ang II receptors. Therefore, using plasma membrane biotinylation and western blotting analysis, we examined membrane expressions of the two Ang II receptors following Ang II treatment.
Figure 3a shows that 30-min incubation with Ang II did not affect total protein levels of AT1R and AT2R in cardiac myocytes (P = 0.9, n = 4 for AT1R; P = 0.8, n = 4 for AT2R, Fig. 3a). However, AT1R in biotinylated membrane fraction was reduced in time-dependent manner with Ang II (at 30 min, P = 0.03 between Ctr and Ang II, n = 3, Fig. 3b). In contrast, AT2R in biotinylated membrane fraction was increased with Ang II (at 30 min, P = 0.02 between control and Ang II, n = 9, Fig. 3b). Intriguingly, pre-treatment of LV myocytes with losartan blocked Ang II-induced AT2R translocation to plasma membrane (AT2R density in biotinylated membrane fraction was reduced, P = 0.01 between Ang II and Ang II + losartan, n = 6, Fig. 3c, d). Similarly, apocynin or tiron pre-treatment blocked Ang II-induced AT2R translocation to the plasma membrane (P = 0.02 between Ang II and Ang II + apocynin, n = 6; P = 0.04 between Ang II and Ang II + tiron, n = 6, Fig. 3c, d).
Time-dependent expressions of AT1R and AT2R in the surface membrane of LV myocytes following Ang II treatment (3 h) and the effect of ROS scavengers on their expression. a Representative AT1R and AT2R blottings before and after Ang II treatment (5, 10, 20 and 30 min) in LV myocytes. GAPDH was used as a loading control. b Immunoblottings and the mean ratios of AT1R and AT2R (surface/total) at 0, 10, 20 and 30 min after Ang II treatment. c Immunoblotting (left) and the mean ratio of AT2R (surface/total) (right). Losartan (1 μM), apocynin (100 μM) and tiron (1 mM) were pre-treated in LV myocytes, respectively
These results clearly suggest that AT1R-cardiac oxidase-derived ROS axis promotes AT2R translocation to plasma membrane and AT2R-mediated Ang II-stimulation of nNOS protein expression.
eNOS is activated by Ang II and intracellular ROS
Next, we detected whether eNOS activity is also regulated by Ang II and if so, how does eNOS affect nNOS protein expression. Figure 4a shows that Ang II time-dependently increased AKT phosphorylation in cardiac myocytes (P = 0.01 between control and Ang II 30 min, n = 3). Similarly, eNOS Ser1177 was increased by Ang II, whereas eNOS Thr495 was reduced (P = 0.03 and P < 0.001 between control and Ang II 30 min, respectively, n = 4, Fig. 4b), suggesting that eNOS activity is increased. In addition, unlike SMTC (nNOS inhibitor), which prevented Ang II-increment of NO (P < 0.001, between Ang II and Ang II + SMTC, n = 9, Fig. 4c), L-NAME diminished NO level in the absence and presence of Ang II (P < 0.001, n = 12, Fig. 4c), indicating that eNOS activity is increased and contributes significantly to the cellular NO level in cardiac myocytes.
Ang II and intracellular ROS regulation of eNOS phosphorylation and activity. a Total and phosphorylated Akt (Akt-Ser473) in response to Ang II (5, 10, 30 min) was detected in isolated LV myocytes with immunoblotting. b eNOS-Ser1177 and eNOS-Thr495 phosphorylations in Ang II-treated LV myocytes (5, 10, 20, 30 min). Representative immunoblottings and averaged ratios for eNOS-Ser1177/eNOS and eNOS-Thr495/eNOS. c Nitrite level in control, Ang II and Ang II + SMTC Ang II + L-NAME. d Immunoblottings and averaged ratios for eNOS-Ser1177/eNOS and eNOS-Thr495/eNOS after pre-treatment with apocynin (100 μM, 30 min)
Furthermore, apocynin pre-treatment decreased eNOS Ser1177 phosphorylation and blocked eNOS Thr495 dephosphorylations by Ang II (P = 0.006 and P = 0.63 between control and Ang II 30 min, respectively, n = 4, Fig. 4d), suggesting that increased intracellular ROS is responsible for Ang II-regulation of eNOS.
Taken together, these results suggest that Ang II treatment activates “coupled” eNOS and intracellular ROS mediate Ang II-activation of eNOS.
Pivotal role of eNOS in Ang II-induced AT2R translocation and nNOS protein expression
Interestingly, inhibition of AT2R by PD123319 did not prevent Ang II-induced eNOS phosphorylations (data not shown), suggesting that eNOS phosphorylation and activity are not subject to AT2R-dependent activation. Therefore, we examined the role of eNOS in Ang II-induced and AT1R/ROS-mediated AT2R translocation to plasma membrane and nNOS protein expression.
As shown in Fig. 5a, AT2R translocation to plasma membrane was observed with immunocytochemistry in non-permeabilized primary LV myocytes. Fluorescent intensity for extracellular membrane-specific AT2R antibody was significantly increased after Ang II or SNP treatment. However, Ang II failed to induce surface expression of AT2R in L-NAME pre-treated LV myocytes. In addition, AT2R density in biotinylated membrane fractions was significantly reduced in L-NAME pre-treated LV myocytes (P = 0.02 between Ang II and L-NAME + Ang II, n = 5, Fig. 5b).
Effect of eNOS inhibition or gene deletion on AT2R translocation to plasma membrane and Ang II-stimulation of nNOS protein expression. a Ang II and SNP-dependent AT2R translocation to plasma membrane was detected by immunocytochemistry with anti-AT2Rextracellular antibody (green) in non-permeabilized LV myocytes. Ang II and SNP increased AT2R expression in the plasma membrane, whereas L-NAME abolished AT2R translocation. b Surface biotinylation of AT2R after LV myocytes was treated by Ang II and Ang II + L-NAME. L-NAME prevented AT2R expression in plasma membrane. c L-NAME pre-treatment blocked Ang II-stimulation of nNOS protein expression. d Isolated LV myocytes in eNOS+/+ and eNOS−/− mice were treated with Ang II (1 μM) for 3 h. nNOS protein expression was increased by Ang II in eNOS+/+ but not in eNOS−/− LV myocytes
Because eNOS functions as an upstream regulator of AT2R, we tested the hypothesis that eNOS mediates Ang II-stimulation of cardiac nNOS. Indeed, L-NAME pre-treatment abolished Ang II-induced nNOS protein expression (P = 0.03 between Ang II and L-NAME + Ang II, n = 4, Fig. 5c). To confirm the role of eNOS in Ang II-induced nNOS protein expression, we detected the effect of Ang II on nNOS protein expression in LV myocytes from eNOS+/+ and eNOS−/− mice. As shown in Fig. 5d, Ang II increased nNOS protein expression in eNOS+/+ LV myocytes (P = 0.01, n = 4, Fig. 5d). However, nNOS protein expression was unaffected by Ang II in eNOS−/− LV myocytes (P = 0.95, n = 4, Fig. 5d).
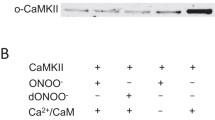
S-nitrosation of AT2R by NO
Increased eNOS production of NO may prompt AT2R translocation via S-nitrosation. Therefore, we aimed to determine whether AT2R could be S-nitrosated by NO increment. Ang II treatment did not affect S-nitrosation of AT2R (data not shown), possibly due to high reducing environment in LV myocytes. However, SNP significantly increased S-nitrosation of AT2R (P = 0.02, n = 3, Fig. 6a). Conversely, pre-incubation of LV myocytes with a strong reducing agent, DTT (1 mM), abolished Ang II-increase of nNOS protein expression (P = 0.018, n = 5, Fig. 6b).
S-nitrosation of AT2R is necessary for Ang II-stimulation of nNOS protein expression. a Representative immunoblots and mean ratios of AT2R S-nitrosation (relative to total AT2R) in the presence and absence of SNP (10 μM). S-nitrosated AT2R was increased by SNP. b DTT pre-treatment (1 mM, 30 min) abolished Ang II-induction of nNOS protein expression
C-terminal cysteine 349 of AT2R is essential in membrane trafficking
Using site-directed mutagenesis on DNA construct of GFP-conjugated AT2R, we went on and analyzed potential target of NO in AT2R that may convey membrane trafficking. We determined to test the 4 cysteine residues on the intracellular region of AT2R due to the bioavailable environment of NO in cytosol (Fig. 7a). Wild type and cysteine 70, 71, 319 and 349 mutations to alanine were transfected in HEK293T cells; NO-dependent membrane trafficking of AT2R was determined using surface biotinylation and immunocytochemistry. As shown in Fig. 7b, surface to total AT2R ratio was significantly increased by SNP (10 μM, 30 min) in wild type AT2R (P = 0.004 between Ctr and SNP in AT2R-WT, n = 3). Similar increases in surface to total AT2R ratios by SNP were observed in C70A, C71A, C319A mutants (P = 0.02, between Ctr and SNP in AT2R-C70A; P = 0.03, between Ctr and SNP in AT2R-C71A; P = 0.01, between Ctr and SNP in AT2R-C319A, respectively, n = 3, Fig. 7b). Unexpectedly, C349A mutation increased AT2R translocation to plasma membrane before SNP treatment (P = 0.005 between AT2R-WT and AT2R-C349A, n = 3, Fig. 7b). And this increase was sustained by SNP treatment in C349A transfected cells. In concordance with surface biotinylation data, AT2R-C349A expression was increased in plasma membrane before SNP treatment and remained to the same level after SNP treatment (Fig. 7c). In contrast, AT2R translocation to plasma membrane was increased by SNP in AT2R-WT, C70A, C71A, C319A transfected cell (Fig. 7c).
Cystein 349 is an important region for the translocation of AT2R to the plasma membrane. a Amino acid sequence and the mutated cysteine residues in AT2R. The AT2R protein has four cysteine residues in intracellular region. The arrowhead indicates the position where GFP was inserted to make GFP-tagged AT2R (AT2R-GFP). b HEK293T cells were transfected with AT2R-WT, C70A, C71A, C319A, C349A mutants, respectively. Each mutant was treated with SNP (10 μM). Quantification of the mutants were identified by GFP protein. Na+-K+ ATPase (NKA) was detected as a loading control for surface fraction. Bar graph represents the ratio of surface to total GFP protein. c Overexpressed AT2R-GFP (green) was localized in the cytoplasm in the HEK293T cell. The surface expression of AT2R-GFP was identified by WGA (red). The right panel showed the intensities of AT2R-GFP (green) and WGA (red) on yellowed dashed lines of the images. Scale bar 5 μm
These results suggest that cysteine 349 of AT2R is a key regulatory site for AT2R translocation to the plasma membrane. Furthermore, AT2R translocation by eNOS activation is important in mediating Ang II-induced increase in nNOS protein expression in rat LV myocytes.
Discussion
In the present study, we demonstrate that (1) Ang II-mediated activation of AT1R and intracellular ROS led to the translocation of AT2R to plasma membrane and AT2R is instrumental in stimulating nNOS transcription/protein expression/activity in murine cardiac myocytes; (2) eNOS is activated by Ang II and intracellular ROS and mediates Ang II-stimulation of AT2R translocation to plasma membrane; (3) eNOS activation is important in Ang II-stimulation of nNOS protein expression in cardiac myocytes. (4) Furthermore, we show direct evidence that AT2R can be S-nitrosated by NO; C-terminal cysteine 349 of AT2R is a critical site for the membrane trafficking of AT2R. To our knowledge, this is the first study to reveal interplays between AT1R/NADPH oxidase—AT2R and eNOS—nNOS in cardiac myocytes. The schematic diagram of the cascade is shown in Fig. 8.
Schematic diagram illustrating the mechanistic links of Ang II-upregulation of nNOS protein expression in cardiac myocytes. Ang II stimulates AT1R in cardiomyocyte plasma membrane and quickly internalized, leading to activation of cardiac oxidases such as NADPH oxidase. Intracellular ROS, in turn, activates Akt and phosphorylates endogenous eNOS to activate the enzyme. Subsequently, S-nitrosation of AT2R near cysteine 349 residue contributes to AT2R translocation to the plasma membrane and was stimulated by Ang II. This leads to a rise in nNOS protein and NO generation
AT1R has been implicated in the activation of constitutive NOS in cardiovascular system. For example, using transgenic mice model that expresses constitutively active AT1R in endothelial cells, Ang II increased endothelial eNOS activity and led to hypotension in these mice [30]. Similar increase in eNOS protein expression by Ang II was shown in endothelial cells in vitro [5] or in myocardium [31, 36]. Conversely, losartan reduced NO production in cardiac myocytes and impaired NO bioavailability was partially responsible for larger infarct size following ischemia [16]. Here, our results clearly showed that acute application of Ang II did not affect eNOS protein expression (at 3 h), indicating that eNOS and nNOS may differ in their transcription from very early stage of disease progression. The relationship between AT2R and nNOS protein expression has been discussed previously. For example, AT2R agonist, C21, treatment significantly upregulated nNOS expression in the paraventricular hypothalamic nucleus (PVN) and rostral ventrolateral medulla (RVLM) and negatively regulated sympathetic outflow and improved baroreflex sensitivity via a nNOS-dependent mechanism [11, 12]. Conversely, inhibition of AT2R abolishes relaxin-induced nNOS protein expression and phosphorylation, and subsequently prevents antifibrotic actions of relaxin [6]. In addition, nNOS protein expression has been shown to be unaffected in the infarcted myocardium from AT2R-deficient mice [3], in contrast to the upregulation of nNOS protein in failing myocardium [2, 9]. More intriguingly, our results also showed that intracellular ROS mediated Ang II-stimulation of nNOS protein expression/activity. Although cardiac oxidases and intracellular ROS have been known to function as upstream regulators of eNOS in endothelial cells [5] or nNOS in kidney [27], our results are the first to demonstrate that intracellular ROS downstream of Ang II controls AT2R translocation to plasma membrane, for AT2R to promote nNOS protein expression in cardiac myocytes.
In the present study, we also show that eNOS activity is increased by Ang II (30 min) and eNOS-derived NO is necessary for AT2R trafficking to increase nNOS protein expression (eNOS begets nNOS). We are not stating that eNOS is the exclusive mechanism to induce nNOS in cardiac myocytes. In fact, nNOS compensates for reduced NO bioavailability in the absence of eNOS in the cardiovasculature under stress [7, 9, 15]. eNOS may become a key player in AT1R-NADPH oxidase-AT2R axis due to its influences on AT2R translocation and activation, despite the fact that eNOS-regulation of myocardial contraction is trivial both under basal conditions and with β-adrenergic stimulation [29, 42]. In essence, eNOS is activated by Ang II (mediated by ROS) and is necessary as an early signal to mediate Ang II-stimulation of nNOS. Notably, Ang II progressively increased eNOS-Ser1177 but reduced eNOS-Thr495, which were blocked by apocynin (Fig. 4b), suggesting contrasting regulation mechanism. One possibility is that Ang II causes protein phosphatase 2A (PP2A) activation with time (downstream of AT2R) and dephosphorylates eNOS-Thr495, whereas eNOS-Ser1177 is more sensitive to ROS-activating protein kinases (e.g., Akt). On the other hand, apocynin without Ang II significantly increased eNOS-Ser1177 (Fig. 4d). Since PP2A activity is known to be suppressed by antioxidants (e.g., ascorbate), followed by enhanced AMPK-dependent eNOS-Ser1177 [23], eNOS-Ser1177 can be actively regulated by PP2A under basal conditions. Furthermore, we have demonstrated NO-dependent S-nitrosation of AT2R in LV myocytes. This effect was observed in primary LV myocytes only with SNP but not by Ang II. The lack of response of Ang II does not exclude eNOS-dependent S-nitrosation of AT2R since it may occur at local compartments and is difficult to detect in myocyte lysates; however, this remains elusive and may require more sensitive measurement to pinpoint the regulation.
To further explore the cysteine residues in AT2R which are responsible for NO-dependent AT2R translocation, we tested site-directed mutagenesis of DNA constructs of AT2R conjugated with GFP. Wild type AT2R translocated to the plasma membrane in response to NO and AT2R Δ7 (7 aa deletions in C terminus) was failed (consistent with Dr Wu’s results [41], data not shown). Alanine mutations of 4 intracellular cysteine residues (C70, 71, 319 and 349) reveal that C-terminal C349A exhibits a “gain of function mutation” and induces AT2R translocation to plasma membrane. These results show the requirement of C349 but the functional significance of its S-nitrosation remains clarified. One possibility is that S-nitrosation of AT2R is the prerequisite and transfer of –NO to adjacent target (e.g., transnitrosylation) accomplishes AT2R translocation. It is not possible to exclude, however, the possibility of C349 oxidation under our experimental conditions. The detailed regulatory mechanisms of cysteine residues of AT2R in the presence of RNS or ROS and their functional relevance in the myocardium remain to be determined.
Ang II has been established to be converted to Ang (1–7) via type 2 angiotensin converting enzyme (ACE2) [28]. Ang (1–7) then stimulates NOS through Mas receptor-dependent [10] or Mas receptor-independent (AT2R-dependent) signaling in cardiac myocytes [8]. Our preliminary results suggested that inhibition of Mas receptors with A779 attenuates Ang II-increase of nNOS protein expression. Both Mas receptors and AT2R play protective roles in diseased heart; whether Mas receptor shares common pathways with AT2R in regulating cardiac NOSs warrants further study.
Growing evidence shows that nNOS upregulation protects the heart from stress by inhibiting oxidases (e.g., xanthine oxidoreductase [22] or NADPH oxidases [18, 43] and mitochondria ROS production [4]), reduces oxidative stress and suppresses adverse myocardial remodeling. On the other hand, nNOS activity in vascular smooth muscles improves blood flow and oxygen tension [7, 21], so as to determine the contractile function of receiving muscles. In the heart, nNOS facilitates LV myocyte relaxation both under basal conditions [45] and after Ang II treatment [18] via promoting phospholamban phosphorylation and SERCA reuptake of Ca2+ into the sarcoplasmic reticulum. Since increased oxidative stress and diastolic dysfunction are often associated with hypertension, hypertrophy or heart failure, the lusitropic effect of nNOS acts in concert with reducing oxidative stress or improving oxygen supply to the myocardium to antagonize the heart from failing. Factors blocking nNOS upregulation may assist the deterioration of the myocardium under stress. Indeed, factors that prevent nNOS protein expression (losartan, PD123319, apocynin or tiron) all blocked faster relaxation by Ang II. These results suggest that pharmacological treatments aim to reduce AT1R activity and oxidative stress may concomitantly change nNOS regulation of myocardial contractility. Taken together, nNOS upregulation in LV myocytes from diseased heart is important in understanding the cardiac protective mechanism.
In essence, we revealed that AT1R-intracellular oxidase-derived ROS-AT2R axis links Ang II-stimulation of nNOS protein expression in cardiac myocytes. Recognition of this pathway downstream of enhanced RAS may improve the effectiveness of AT1R or ACE inhibitors on treating heart failure patients.
References
Barouch LA, Harrison RW, Skaf MW, Rosas GO, Cappola TP, Kobeissi ZA, Hobai IA, Lemmon CA, Burnett AL, O’Rourke B, Rodriguez ER, Huang PL, Lima JA, Berkowitz DE, Hare JM (2002) Nitric oxide regulates the heart by spatial confinement of nitric oxide synthase isoforms. Nature 416:337–339. doi:10.1016/S0002-9149(01)02321-9
Bendall JK, Damy T, Ratajczak P, Loyer X, Monceau V, Marty I, Milliez P, Robidel E, Marotte F, Samuel JL, Heymes C (2004) Role of myocardial neuronal nitric oxide synthase-derived nitric oxide in beta-adrenergic hyporesponsiveness after myocardial infarction-induced heart failure in rat. Circulation 110:2368–2375. doi:10.1161/01.CIR.0000145160.04084.AC
Brede M, Roell W, Ritter O, Wiesmann F, Jahns R, Haase A, Fleischmann BK, Hein L (2003) Cardiac hypertrophy is associated with decreased eNOS expression in angiotensin AT2 receptor-deficient mice. Hypertension 42:1177–1182. doi:10.1161/01.HYP.0000100445.80029.8E
Burkard N, Williams T, Czolbe M, Blömer N, Panther F, Link M, Fraccarollo D, Widder JD, Hu K, Han H, Hofmann U, Frantz S, Nordbeck P, Bulla J, Schuh K, Ritter O (2010) Conditional overexpression of neuronal nitric oxide synthase is cardioprotective in ischemia/reperfusion. Circulation 122:1588–1603. doi:10.1161/CIRCULATIONAHA.109.933630
Cai H, Li Z, Dikalov S, Holland SM, Hwang J, Jo H, Dudley SC Jr, Harrison DG (2002) NAD(P)H oxidase-derived hydrogen peroxide mediates endothelial nitric oxide production in response to angiotensin II. J Biol Chem 277:48311–48317. doi:10.1074/jbc.M208884200
Chow BS, Kocan M, Bosnyak S, Sarwar M, Wigg B, Jones ES, Widdop RE, Summers RJ, Bathgate RA, Hewitson TD, Samuel CS (2014) Relaxin requires the angiotensin II type 2 receptor to abrogate renal interstitial fibrosis. Kidney Int 86:75–85. doi:10.1038/ki.2013.518
Copp SW, Hirai DM, Ferguson SK, Holdsworth CT, Musch TI, Poole DC (2012) Effects of chronic heart failure on neuronal nitric oxide synthase-mediated control of microvascular O2 pressure in contracting rat skeletal muscle. J Physiol 590:3585–3596. doi:10.1113/jphysiol.2012.235929
Costa MA, Lopez Verrilli MA, Gomez KA, Nakagawa P, Peña C, Arranz C, Gironacci MM (2010) Angiotensin-(1-7) upregulates cardiac nitric oxide synthase in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 299:H1205–H1211. doi:10.1152/ajpheart.00850.2009
Damy T, Ratajczak P, Shah AM, Camors E, Marty I, Hasenfuss G, Marotte F, Samuel JL, Heymes C (2004) Increased neuronal nitric oxide synthase-derived NO production in the failing human heart. Lancet 363:1365–1367. doi:10.1016/S0140-6736(04)16048-0
Dias-Peixoto MF, Santos RA, Gomes ER, Alves MN, Almeida PW, Greco L, Rosa M, Fauler B, Bader M, Alenina N, Guatimosim S (2008) Molecular mechanisms involved in the angiotensin-(1-7)/Mas signaling pathway in cardiomyocytes. Hypertension 52:542–548. doi:10.1161/HYPERTENSIONAHA.108.114280
Gao J, Zucker IH, Gao L (2014) Activation of central angiotensin type 2 receptors by compound 21 improves arterial baroreflex sensitivity in rats with heart failure. Am J Hypertens 27:1248–1256. doi:10.1093/ajh/hpu044
Gao J, Zhang H, Le KD, Chao J, Gao L (2011) Activation of central angiotensin type 2 receptors suppresses norepinephrine excretion and blood pressure in conscious rats. Am J Hypertens 24:724–730. doi:10.1038/ajh.2011.33
Heusch G, Post H, Michel MC, Kelm M, Schulz R (2000) Endogenous nitric oxide and myocardial adaptation to ischemia. Circ Res 87:146–152. doi:10.1161/01.RES.87.2.146
Heusch G, Schulz R (2011) A radical view on the contractile machinery in human heart failure. J Am Coll Cardiol 57:310–312. doi:10.1016/j.jacc.2010.06.057
Huang A, Sun D, Shesely EG, Levee EM, Koller A, Kaley G (2002) Neuronal NOS-dependent dilation to flow in coronary arteries of male eNOS-KO mice. Am J Physiol Heart Circ Physiol 282:H429–H436. doi:10.1152/ajpheart.00501.2001
Huisamen B, Pêrel SJ, Friedrich SO, Salie R, Strijdom H, Lochner A (2011) ANG II type I receptor antagonism improved nitric oxide production and enhanced eNOS and PKB/Akt expression in hearts from a rat model of insulin resistance. Mol Cell Biochem 349:21–31. doi:10.1007/s11010-010-0656-6
Jalowy A, Schulz R, Dörge H, Behrends M, Heusch G (1998) Infart size reduction by AT1-receptor blockade through a signal cascade of AT2-receptor activation, bradykinin and prostaglandins in pigs. J Am Coll Cardiol 32:1787–1796. doi:10.1016/S0735-1097(98)00441-0
Jin CZ, Jang JH, Wang Y, Kim JG, Bae YM, Shi J, Che CR, Kim SJ, Zhang YH (2012) Neuronal nitric oxide synthase is up-regulated by angiotensin II and attenuates NADPH oxidase activity and facilitates relaxation in murine left ventricular myocytes. J Mol Cell Cardiol 52:1274–1281. doi:10.1016/j.yjmcc.2012.03.013
Jin CZ, Jang JH, Kim HJ, Wang Y, Hwang IC, Sadayappan S, Park BM, Kim SH, Jin ZH, Seo EY, Kim KH, Kim YJ, Kim SJ, Zhang YH (2013) Myofilament Ca2+ desensitization mediates positive lusitropic effect of neuronal nitric oxide synthase in left ventricular myocytes from murine hypertensive heart. J Mol Cell Cardiol 60:107–115. doi:10.1016/j.yjmcc.2013.04.017
Jones ES, Vinh A, McCarthy CA, Gaspari TA, Widdop RE (2008) AT2 receptors: functional relevance in cardiovascular disease. Pharmacol Ther 120:292–316. doi:10.1016/j.pharmthera.2008.08.009
Kellogg DL Jr, Zhao JL, Wu Y (2008) Neuronal nitric oxide synthase control mechanisms in the cutaneous vasculature of humans in vivo. J Physiol 586:847–857. doi:10.1113/jphysiol.2007.144642
Kinugawa S, Huang H, Wang Z, Kaminski PM, Wolin MS, Hintze TH (2005) A defect of neuronal nitric oxide synthase increases xanthine oxidase-derived superoxide anion and attenuates the control of myocardial oxygen consumption by nitric oxide derived from endothelial nitric oxide synthase. Circ Res 96:355–362. doi:10.1161/01.RES.0000155331.09458.A7
Ladurner A, Schmitt CA, Schachner D, Atanasov AG, Werner ER, Dirsch VM, Heiss EH (2012) Ascorbate stimulates endothelial nitric oxide synthase enzyme activity by rapid modulation of its phosphorylation status. Free Radic Biol Med 52(10):2082–2090. doi:10.1016/j.freeradbiomed.2012.03.022
Nguyen Dinh Cat A, Montezano AC, Burger D, Touyz RM (2013) Angiotensin II, NADPH oxidase, and redox signaling in the vasculature. Antioxid Redox Signal 19:1110–1120. doi:10.1089/ars.2012.4641
Oyamada S, Bianchi C, Takai S, Robich MP, Clements RT, Chu L, Sellke FW (2010) Impact of acute myocardial ischemia reperfusion on the tissue and blood-borne renin–angiotensin system. Basic Res Cardiol 105:513–522. doi:10.1007/s00395-010-0093-4
Padia SH, Carey RM (2013) AT2 receptors: beneficial counter-regulatory role in cardiovascular and renal function. Pflugers Arch 465:99–110. doi:10.1007/s00424-012-1146-3
Paliege A, Pasumarthy A, Mizel D, Yang T, Schnermann J, Bachmann S (2006) Effect of apocynin treatment on renal expression of COX-2, NOS1, and renin in Wistar-Kyoto and spontaneously hypertensive rats. Am J Physiol Regul Integr Comp Physiol 290:694–700. doi:10.1152/ajpregu.00219.2005
Patel KP, Schultz HD (2012) Angiotensin Peptides and Nitric Oxide in Cardiovascular Disease. Antioxid Redox Signal 19:1121–1132. doi:10.1089/ars.2012.4614
Post H, Schulz R, Gres P, Heusch G (2001) No involvement of nitric oxide in the limitation of beta-adrenergic inotropic responsiveness during ischemia. Am J Physiol Heart Circ Physiol 281:H2392–H2397
Ramchandran R, Takezako T, Saad Y, Stull L, Fink B, Yamada H, Dikalov S, Harrison DG, Moravec C, Karnik SS (2006) Angiotensinergic stimulation of vascular endothelium in mice causes hypotension, bradycardia, and attenuated angiotensin response. Proc Natl Acad Sci USA 103:19087–19092. doi:10.1073/pnas.0602715103
Ritter O, Schuh K, Brede M, Röthlein N, Burkard N, Hein L, Neyses L (2003) AT2 receptor activation regulates myocardial eNOS expression via the calcineurin-NF-AT pathway. FASEB J 17:283–285. doi:10.1096/fj.02-0321fje
Sartoretto JL, Kalwa H, Pluth MD, Lippard SJ, Michel T (2011) Hydrogen peroxide differentially modulates cardiac myocyte nitric oxide synthesis. Proc Natl Acad Sci USA 108:15792–15797. doi:10.1073/pnas.1111331108
Schmieder RE, Hilgers KF, Schlaich MP, Schmidt BM (2007) Renin–angiotensin system and cardiovascular risk. Lancet 369:1208–1219. doi:10.1016/S0140-6736(07)60242-6
Sears CE, Bryant SM, Ashley EA, Lygate CA, Rakovic S, Wallis HL, Neubauer S, Terrar DA, Casadei B (2003) Cardiac neuronal nitric oxide synthase isoform regulates myocardial contraction and calcium handling. Circ Res 92:e52–e59. doi:10.1161/01.RES.0000064585.95749.6D
Takimoto E, Champion HC, Li M, Ren S, Rodriguez ER, Tavazzi B, Lazzarino G, Paolocci N, Gabrielson KL, Wang Y, Kass DA (2005) Oxidant stress from nitric oxide synthase-3 uncoupling stimulates cardiac pathologic remodeling from chronic pressure load. J Clin Invest 115:1221–1231. doi:10.1172/JCI21968
Tambascia RC, Fonseca PM, Corat PD, Moreno H Jr, Saad MJ, Franchini KG (2001) Expression and distribution of NOS1 and NOS3 in the myocardium of angiotensin II-infused rats. Hypertension 37:1423–1428. doi:10.1161/01.HYP.37.6.1423
Unger T (2002) The role of the renin–angiotensin system in the development of cardiovascular disease. Am J Cardiol 89:3A–10A. doi:10.1016/S0002-9149(01)02321-9
Varagic J, Frohlich ED (2002) Local cardiac renin–angiotensin system: hypertension and cardiac failure. J Mol Cell Cardiol 34:1435–1442. doi:10.1006/jmcc.2002.2075
Wiemer G, Itter G, Malinski T, Linz W (2001) Decreased nitric oxide availability in normotensive and hypertensive rats with failing hearts after myocardial infarction. Hypertension 38:1367–1371. doi:10.1161/hy1101.096115
Xu KY, Huso DL, Dawson TM, Bredt DS, Becker LC (1999) Nitric oxide synthase in cardiac sarcoplasmic reticulum. Proc Natl Acad Sci USA 96:657–662. doi:10.1073/pnas.96.2.657
Zhang X, Dong C, Wu QJ, Balch WE, Wu G (2011) Di-acidic motifs in the membrane-distal C termini modulate the transport of angiotensin II receptors from the endoplasmic reticulum to the cell surface. J Biol Chem 286:20525–20535. doi:10.1074/jbc.M111.222034
Zhang YH, Casadei B (2012) Sub-cellular targeting of constitutive NOS in health and disease. J Mol Cell Cardiol 52:341–350. doi:10.1016/j.yjmcc.2011.09.006
Zhang YH, Dingle L, Hall R, Casadei B (2009) The role of nitric oxide and reactive oxygen species in the positive inotropic response to mechanical stretch in the mammalian myocardium. Biochim Biophys Acta 1787:811–817. doi:10.1016/j.bbabio.2009.03.020
Zhang YH, Jin CZ, Jang JH, Wang Y (2014) Molecular mechanisms of neuronal nitric oxide synthase in cardiac function and pathophysiology. J Physiol 592:3189–3200. doi:10.1113/jphysiol.2013.270306
Zhang YH, Zhang MH, Sears CE, Emanuel K, Redwood C, El-Armouche A, Kranias EG, Casadei B (2008) Reduced phospholamban phosphorylation is associated with impaired relaxation in left ventricular myocytes from neuronal NO synthase-deficient mice. Circ Res 102:242–249. doi:10.1161/CIRCRESAHA.107.164798
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2013068067); by the Brain Korea 21 Graduate Programme of the Korean Ministry of Education, Science and Technology, Seoul National University Hospital, the Korean Society of Hypertension (2013), SK Telecom Research Fund (no. 3420130290) and from the National Natural Science Foundation of China (NSFC, 31460265). National Institutes of Health grant R01GM076167.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Jang, J.H., Chun, J.N., Godo, S. et al. ROS and endothelial nitric oxide synthase (eNOS)-dependent trafficking of angiotensin II type 2 receptor begets neuronal NOS in cardiac myocytes. Basic Res Cardiol 110, 21 (2015). https://doi.org/10.1007/s00395-015-0477-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-015-0477-6