Abstract
Purpose
Excess iodine in drinking water has emerged as a public health issue in China. This study assesses the effectiveness of removing iodized salt on reducing the iodine excess in populations living in high-iodine areas and also to identify the threshold value for safe levels of iodine in water.
Methods
Twelve villages from 5 cities of Hebei Province with iodine content in drinking water ranging from 39 to 313 µg/l were selected to compare the urinary iodine content of children aged 8–10 years before and after removing iodized salt from their diet.
Results
For 3 villages where median water iodine content (MWIC) was below 110 µg/l, following the removal of iodized salt (the intervention), the median urinary iodine content (MUIC) reduced to under 300 µg/l decreasing from 365, 380, 351 to 247, 240, 281 µg/l, respectively. However, the MUIC in the 9 villages with MWIC above 110 µg/l remained higher than 300 µg/l. The children’s MUIC correlated positively with the MWIC in the 12 villages (p ≤ 0.001). The linear regression equation after removing iodized salt was MUIC = 0.6761MWIC + 225.67, indicating that to keep the MUIC below 300 µg/l (the iodine excess threshold recommended by the WHO) requires the MWIC to be under 110 µg/l.
Conclusion
Removing iodized salt could only correct the iodine excess in the population living in the areas with MWIC below 110 µg/l. In the areas with water iodine above 110 µg/l, interventions should be focused on seeking water with lower iodine content. This study suggests a threshold value of 110 µg/l of iodine in drinking water to maintain a safe level of dietary iodine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iodine deficiency disorders (IDD) were prevalent in China until the end of the twentieth century. In order to eliminate IDD, universal salt iodization was implemented around the country in 1995 [1]. Following the successful management of IDD, in recent years, public attention has transferred to iodine excess and this has emerged as an important public health issue. In China, iodine excess is mainly attributed to underground drinking water with high iodine content, which was first identified in the early 1980s [2]. According to the Chinese criteria for excessive iodine, an area with iodine content in underground drinking water above 150 µg/l is defined as a high-iodine area (HIA) [3]. Comprehensive studies on the distribution of HIA in China during the 1990s and early 2000s have revealed that there is widespread distribution of HIAs in the down stream region of the Yellow River, concentrated in 11 provinces and potentially affecting a population of nearly 40 million [4, 5].
Iodine excess may cause hypothyroidism, hyperthyroidism, thyroiditis and goiter [2, 6]. A number of Chinese studies reported high goiter prevalence of between 8 and 15 % in children aged 8–10 years in these areas [7–9]. Our recent study found a goiter prevalence of over 30 % in children in these areas using the WHO assessment criteria [10]. Varied elevation of urinary iodine content is another marker of excessive iodine intake. Urinary iodine in children living in these areas is usually well above 300 µg/l [4], the criteria of iodine excess defined by the WHO [11]. To prevent the potential health consequences caused by iodine excess, a policy of removing iodized salt from HIA was implemented by the Chinese government in 2010. The supply of iodized salt was replaced by non-iodized salt through retail outlets in these HIAs. To date, the effectiveness of this intervention on iodine excess in the general population in these areas has not been assessed.
There is a widespread distribution of HIAs in Hebei Province. According to the national criteria, a town that contains 5 systematically sampled villages with a median water iodine above 150 µg/l is defined as a high-iodine town (HIT). In Hebei Province, 172 HITs were identified during 2003–2004. These towns are scattered across 5 cities containing a population of over 6 million people [12]. Iodized salt was gradually replaced by non-iodized in these HITs in the second half of 2010. However, due to the Fukushima nuclear disaster in March of 2011, most of the families in HIAs resumed consuming iodized salt because of a rumor that iodized salt can prevent nuclear radiation. The local families purchased and stored a considerable amount of iodized salt. However, according to annual surveillance of edible salt in the HIAs, the iodized salt was gradually used up by March of 2012.
Due to the uneven distribution of high-iodine water, in a given HIT, low water iodine (below 150 µg/l) villages exist, though removal of iodized salt was carried out in all the villages of the HIT. Hence, the impact of removing iodized salt on the iodine nutrition of people drinking low-iodine water can also be assessed. In this study, we selected 12 villages with iodine content in drinking water ranging from 39 to 313 µg/l in 10 HITs from 5 cities of Hebei Province to monitor the change of urinary iodine content associated with the removal of iodized salt in the children aged 8–10 years. The baseline survey was conducted from May to June in 2010 when iodized salt was still available in these areas. The second phase survey was carried out from September to October in 2012 by which time the iodized salt had been removed for about 6–10 months. The aim of the present study was to assess whether removing iodized salt can correct the iodine excess in the population living in these areas and also to explore the possible threshold value of water iodine, which can provide adequate iodine to the general population without causing iodine excess. Such a study is important as it will contribute to a more evidence-based refinement of the current intervention measures to reduce iodine excess in China.
Materials and methods
Selection of investigated villages
The selection of investigated villages was divided into 2 steps. The first step was to select HITs from the cities containing HITs. The second step was to choose the villages from the selected HITs. In order to cover all the HIAs of Hebei Province, 2 HITs were randomly selected in each of the 5 cities containing the HITs of Hebei Province. In each of the HITs selected, the villages with known iodine content in the drinking water were identified based on previous surveys. Then, all the villages with water iodine between 1 and 350 µg/l were divided into 7 groups using an iodine content interval of 50 µg/l, i.e., water iodine content of the first group was 1–49, 50–99 µg/l for the second group, and so on. Two villages with a population over 2000 were randomly selected in each group to ensure that there were at least 30 children aged 8–10 years in each of the selected villages, consistent with the WHO sample size recommendation [11]. We selected a total of 14 villages in 10 HITs from the 5 cities for the baseline survey. Since the drinking water sources in 2 selected villages were changed during the study and their iodine content changed greatly, they were excluded from the study. A total of 12 villages were included in the study, and their water iodine ranged from 39 to 313 µg/l.
Collection of urine samples of children aged 8–10 years
The urine sample collection was conducted at the primary school of each selected village. Only those healthy children who lived in the investigated villages for at least 1 year were included. All the eligible children aged 8–10 years in the selected villages were asked to collect their spot urine samples at their schools.
This study was conducted in line with the guidelines of the Declaration of Helsinki. It was approved by the Hebei Provincial Bureau of Science and Technology. Since urine sample collection is noninvasive, oral consent was obtained from the headmasters of the investigated schools. Verbal consent was witnessed and formally recorded.
Collection of drinking water samples
The number of drinking water samples depended on the number of water sources. The drinking water supply was centralized (tap water) in 11 out of the 12 selected villages, and hence, only 2 water samples were randomly collected from 2 households in each of these 11 villages. In the twelfth village, there were more than 5 wells and here, water samples were collected using a systematic sampling method based on their location. In brief, five water samples from 5 households were gathered in the eastern, western, southern, northern and central part of the village.
Collection of edible salt samples
Edible salt samples were also collected at the investigated villages. A systematic sampling method was used such that four households were randomly selected in each location (central, north, south, east, west of the village) to collect edible salt. A total of 20 salt samples were collected in each village.
The field sample collection was completed in 2 phases. The first phase of sample collection was conducted from May to June in 2010 when iodized salt was still available in the investigated villages. The second phase was carried out from September to October in 2012 by which time the iodized salt had been removed for about 6–10 months.
All samples were transferred rapidly to the IDD laboratories at the municipal Center for Disease Control and prevention (CDC) of the corresponding city. The water and urine samples were kept under 8 °C before measurement of iodine content. The salt samples were kept at room temperature sealed in plastic bags.
Laboratory measurement for iodine content
The iodine content of urine samples was measured by the method of Sandell–Kolthoff reaction for which the basis of the analysis is the reduction of ceric ion in the presence of arsenious acid [13]. WHO defines iodine excess where an MUIC of a given population is above 300 µg/l [11].
The iodine content of salt was determined quantitatively using a titration method [14]. According to the Chinese criteria for iodized salt, edible salt with less than 5 mg/kg iodine is classified as non-iodized salt, and edible salt with iodine content higher than 5 mg/kg is defined as iodized salt [15].
The iodine content in drinking water was determined by the method of arsenic-cerium oxidation–reduction spectrophotometry [16]. Drinking water containing more than 150 µg/l iodine is classified as iodine excessive [2].
All the 5 municipal IDD laboratories were accredited to detect iodine content in urine, water and salt samples by the National IDD Reference Laboratory, through passing the tests for measuring spiked samples and certified reference materials. The recovery rates in the 5 municipal IDD laboratories were between 95 and 105 %. To apply quality control to the measurement of iodine content in the 5 municipal IDD laboratories, the provincial IDD laboratory conducted duplicate analysis for 5 % of all collected samples. The accordance between the provincial IDD laboratory and the 5 municipal IDD laboratories was above 90 %.
Data processing and statistical analysis
Data processing and statistical analyses were performed using statistical software packages Epi–Info™ 2002 (Centers for Disease Control and Prevention, Atlanta, GA, USA) and SPSS version 13.0 (SPSS Inc., Chicago, IL, USA). Since the distributions of iodine in edible salt, drinking water and children’s urine are not normal, the median was used to describe their central tendency. The differences in children’s MUIC between before and after removing iodized salt were tested by the Mann–Whitney test. The differences in the ratios of children’s urine samples with iodine content above 300 µg/l before and after removing iodized salt were tested using the Chi-squared test. The One-Sample Kolmogorov–Smirnov test was used to analyze the distributions of MUIC, MWIC and MSIC. Spearman’s correlation was used to determine associations between children’s MUIC and MWIC and MSIC. Following the correlation analysis, a linear regression model was developed.
Results
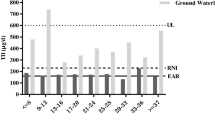
Iodine content in drinking water
In the baseline survey, the median water iodine content (MWIC) ranged from 39 to 313 µg/l. The number of villages with MWIC in the intervals of 1–49, 50–99, 100–149, 150–199, 200–249, 250–299 and 300–350 µg/l was 1, 2, 2, 2, 2, 1 and 2, respectively. Following the iodized salt removal intervention, in the second phase, the MWIC of each village was similar to that of the baseline survey, though the MWIC in one village had decreased from the 100–149 µg/l group to the 50–99 µg/l group. The MWIC for each of the 12 villages during the two phases of data collection is provided in Table 1.
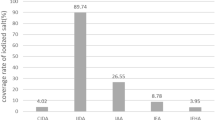
Iodine content in edible salt
In the baseline survey (phase 1), the edible salt in all investigated households was iodized. The median salt iodine content (MSIC) for each of the 12 villages varied from 17 to 39 mg/kg. In the second phase, over 90 % of the edible salt in the investigated households was non-iodized. The MSIC of each village was below 5 mg/kg (refer to Table 1).
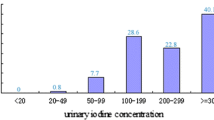
Iodine content in urine of children aged 8–10 years
In the baseline survey, the median urinary iodine content (MUIC) of children aged 8–10 years in each of the 12 villages was higher than 300 µg/l, the criteria for iodine excess recommended by WHO [11], ranging from 351 to 541 µg/l. In the second phase, the MUIC for 3 villages, Gaozhuang, Xiaodu and Cuicun, decreased below 300 µg/l, while levels remained higher than 300 µg/l in the remaining 9 villages. However, compared with the baseline, the MUIC in each of the 12 villages decreased dramatically following iodized salt removal and this decrease was statistically significant in 8 out of the 12 villages. The MUIC of each village in the two phases of data collection and their comparisons are shown in Table 2.
The percentage of urine samples with iodine content higher than 300 µg/l in each of the 12 villages was very high in the baseline survey, varying from 63.3 to 92.9 %. In the second phase, it decreased sharply in each of the 12 villages, with a statistically significant difference identified in 9 out of 12 villages. It dropped below 50 % in the 3 villages with MWIC lower than 100 µg/l. The details are shown in Table 3.
The urine sample size for both gender stratification and age-groups of 8, 9 and 10 years in the village of Dagaocun was more than 30, so the impact of removing iodized salt on children’s MUIC in gender and age-group was specifically assessed using these data. Compared with the baseline, the MUIC declined significantly both in boys (p = 0.001) and in girls (p = 0.001) in the second phase. Moreover, a significant decrease in MUIC was also identified in each age-group (8 years: p ≤ 0.0017; 9 years: p = 0.008; 10 years: p = 0.016.). The MUIC in each gender and age-group for the 2 phases of data collection and their comparisons are shown in Table 4.
Correlation between children’s MUIC and MWIC
The respective associations between MUIC and MWIC, MUIC and MSIC in the 12 villages were analyzed using SPSS 13.0. For the baseline data, children’s MUIC was positively correlated with the MWIC in the 12 villages (Spearman, R = 0.893, p = 0.001), though it did not correlate significantly with the MSIC of the villages (Spearman, R = −0.536, p = 0.073). In the second phase of data collection, the children’s MUIC also correlated positively with the MWIC in the 12 villages (Spearman, R = 0.951, p = 0.001), and again it did not correlate significantly with the MSIC of the villages (Spearman, R = 0.115, p = 0.721).
The One-Sample Kolmogorov–Smirnov test found that children’s MUIC and MWIC in the 12 villages were all normally distributed for both phases of data collection (In the baseline survey, MUIC: Z = 0.361, p = 0.968; MWIC: Z = 0.384, p = 0.998; In the second phase, MUIC: Z = 0.503, p = 0.997; MWIC: Z = 0.591, p = 0.969). Hence, the relationships between children’s MUIC and MWIC in the 12 villages for the two phases were analyzed by linear regression. The regression equation for the relationship between MUIC and MWIC for the baseline and second phase was MUIC = 0.5819MWIC + 325.14 and MUIC = 0.6761MWIC + 225.67, respectively. Both linear regression models were statistically significant (For the baseline, F = 48.330, p = 0.0. For the second phase, F = 80.511, p = 0.0), and the two regression lines representing the relationship are provided in Fig. 1. The distance between the two lines is around 90 µg/l, which suggests that removal of iodized salt has lowered children’s urinary iodine by approximately 90 µg/l. Furthermore, the second regression equation which is based on the post-intervention (removed iodized salt) data collection indicates that to reach a MUIC of 300 µg/l (equivalent to the WHO iodine excess guideline), around 110 µg/l MWIC is needed.
Discussion
This study has identified that when iodized salt was provided in the HIAs (first phase or baseline data collection), children’s MUIC in each of the 12 villages exceeded 300 µg/l, the WHO criterion for iodine excess. However, following the removal of iodized salt, the children’s MUIC in 8 out of 12 villages decreased significantly and the percentage of urine samples with iodine content above 300 µg/l decreased significantly in 9 out of 12 villages. There are a number of reasons for the insignificant decreases in children’s MUIC and in the percentage of urine samples with iodine content above 300 µg/l between the two phases. Firstly, the results indicate that removing iodized salt can only reduce urinary iodine by around 90 µg/l, which is insufficient to produce a statistically significant decrease in children’s UIC for those who lived in the villages with high water iodine. Secondly, iodized salt was not completely removed in some villages. Since the HITs are usually close to areas with low iodine content where iodized salt is still supplied, the local residents may still consume iodized salt bought from nearby villages. This explanation cannot be verified as individual household exposure to iodized salt was not measured in this study.
Only in children living in the 3 villages with MWIC below 110 µg/l, the MUIC was reduced to under 300 µg/l. The percentage of urine samples with iodine content above 300 µg/l also dropped below 50 % in these 3 villages. In contrast, in the 9 villages with MWIC above 110 µg/l, children’s MUIC remained above 300 µg/l. These results indicate that removing iodized salt could only partly counter the iodine excess in the population living in areas with iodine content in drinking water below 110 µg/l. Iodized salt removal was less effective for the population whose drinking water contained iodine above 110 µg/l, and since the children’s MUIC had a positive linear correlation with MWIC, the iodine excess could mainly be attributed to the water iodine.
The threshold value for iodine content in drinking water in China remains under debate. In the present study, the regression equation between the MUIC and MWIC in the 2 phases of survey indicates that 0 and 110 µg/l of MWIC are needed (with and without iodized salt) to attain the MUIC WHO guideline of 300 µg/l, suggesting that consumption of non-iodized salt and MWIC levels below 110 µg/l would be acceptable to reduce iodine excess problems. In other studies conducted in China, different threshold values for water iodine have been proposed. Based on research in Shandong Province, 90 µg/l was proposed as the threshold value [17]. However, this study did not investigate the population’s MUIC in the range of 100–140 µg/l of MWIC, and hence, this threshold value relates to the more limited range of exposures estimated in this area. Li et al. [18] conducted a more extensive study on the threshold value in HIAs in 3 provinces in China, suggesting that the threshold value could be above 100 µg/l.
Since some seaweed contains high iodine content, it is an important confounding factor for the population’s iodine intake. Unlike Li et al. [18], in the present study, we did not exclude the children who ate seaweed, nor did we account for dietary iodine consumption in our analysis of urine iodine concentration. Though this may account for some of the urine iodine concentrations measured, it is a difficult exposure to control due to the difficulties in restricting the range of individual diets of children. Hence, the threshold for median water iodine concentration identified for this study of 110 µg/l represents an appropriate threshold level to assist in decision making about choices of water and locations for intervention.
The present study found that with and without iodized salt, children’s MUIC correlated positively with the MWIC in the villages where the children lived. This finding is consistent with other studies conducted in the HIAs in China [19, 20]. These studies suggested that the population’s iodine excess in the HIA was mainly caused by drinking water with high iodine content. After iodized salt is removed in the HIAs of China where elevated levels of iodine naturally occur in water, usually above 110 µg/l, the local residents’ iodine intake remains high to excessive. Hence, intervention strategies to reduce iodine should be focused on finding alternative, lower-iodine drinking water sources. Some options for this include deep underground water (usually below 100 m in depth), which may contain lower iodine concentrations, ground surface water, such as river water, lake water and rainwater harvesting. It should be noted that the removal of iodized salt and changing drinking water sources apply only to these specific HIA regions as in most other areas of China, there is low iodine content in the environment, and salt iodization remains necessary and extremely beneficial.
Conclusion
Iodine excess caused by high-iodine drinking water has emerged as a public health issue in China in recent years. In response to this issue, the Chinese government implemented a policy of removing iodized salt from HIAs in 2010. However, the effectiveness of this intervention on the iodine excess in the general population has not been fully characterized, and the threshold value for ‘safe’ iodine content in drinking water remains under debate. For the first time in China, this study assessed the impacts of this iodized salt removal intervention through field data collection. It revealed that removing iodized salt significantly reduced urinary iodine concentrations in the sample population of children 8–10 years old in the majority of villages studied. However, it also found that removing iodized salt could only adequately counter the iodine excess in the population living in areas with a MWIC below 110 µg/l, indicating a threshold value of iodine in drinking water to be 110 µg/l. In the HIAs with water iodine above 110 µg/l, additional intervention measures are required to ensure drinking water supplies with iodine content below this level. Deep well water, surface water use and rainwater harvesting are potential options that warrant investigation in these high-iodine water areas.
References
Lv SM, Xie LJ, Zhou RH et al (2009) Control of iodine deficiency disorders following 10-year universal salt iodization in Hebei province of China. Biomed Environ Sci 22:472–479
Yu ZH, Zhu HM, Chen CY et al (1999) Proceedings on endemic goiter induced by high iodine. Chin J Endem 18:301–305 (in Chinese)
Ministry of Health (2003) National criteria for classifying high iodine regions. MOH, Beijing
Zhao JK, Chen ZP, Maberly G (1998) Iodine-rich drinking water of natural origin in China. Lancet 352:2024
Shen HM, Liu SJ, Sun DJ et al (2011) Geographical distribution of drinking-water with high iodine level and association between high iodine level in drinking-water and goitre: a Chinese national investigation. Br J Nutr 106:243–247
Burgi H (2010) Iodine excess. Best Pract Res Clin Endoc Met 25:107–115
Wang Y, Zheng HM, Wang CG et al (2005) Epidemiological investigation on water-sourced high level iodine goiter in Yellow river delta in Henan province. Chin J Endem 23:231–233 (in Chinese)
Zhang XD, Jia QZ, Wang ZH et al (2007) Epidemiological survey of inland water- borne high iodine in drinking water in Shanxi Province. Chin Tropl Med 17:679–681 (in Chinese)
Zhang ZZ, Fan J, Guo HY et al (2007) Distribution and goiter status of areas with high iodine in Inner Mongolia. J Baotou Med 23:566–568 (in Chinese)
Lv S, Xu D, Wang Y et al (2014) Goitre prevalence and epidemiological features in children living in areas with mildly excessive iodine in drinking-water. Br J Nutr 111:186–192
WHO/UNICEF/ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination, 3rd ed. WHO, Geneva
Lv SM, Zhao J, Xu D et al (2012) An epidemiological survey of children’s iodine nutrition and goitre status in regions with mildly excessive iodine in drinking water in Hebei Province, China. Public Health Nutr 15:1168–1173
Pino S, Fang SL, Braverman LE (1998) Ammonium persulfate: a new and safe method for measuring urinary iodine by ammonium persulfate oxidation. Exp Clin Endocrinol Diabetes 106(Suppl 3):S22–S27
United Nations Children’s Fund (UNICEF) ROSCA (1998) The use of iodised salt in the prevention of iodine deficiency disorders—a handbook of monitoring and quality control. UNICEF ROSCA, New Delhi
Ministry of Health (2007) National surveillance plan for iodine deficiency disorders. MOH, Beijing (in Chinese)
Ministry of Health (2006) The standard test method for drinking water. MOH, Beijing (in Chinese)
Guo XW, Qin QL, Liu CJ et al (2007) Study on iodine nutritional status of target population due to different iodine concentrations in drinking water after stopping iodized salt. J Hyg Res 36:427–431 (in Chinese)
Li SM, Zhang GH, Gu YY et al (2009) Study on changing of iodine nutrition level of the people with unexcessive iodine drinking water in iodine excess area s after stopping supplies of iodized salt. Chin J Ctrl Endem Dis 24:107–109 (in Chinese)
Lv SM, Wang YC, Xu D et al (2013) Drinking water contributes to excessive iodine intake among children in Hebei, China. Eur J Clin Nutr 67:961–965
Guo XW, Qin QL, Chen ZP et al (2007) Iodine nutrition status of population in the areas with different iodine concentrations of drinking water. Acta Nutr Sin 29:526–530 (in Chinese)
Acknowledgments
This study was supported by Hebei Provincial Bureau of Science and Technology (Grant Numbers: 11276103D-3) and did not receive any other specific grant from commercial or not-for-profit sector, so the authors declare no conflict of interest. Shengmin Lv was responsible for the study design, data analysis, paper writing and investigation training. Yinglu Zhao, Yanxia Li, Yuchun Wang, Hua Liu and Yang Li were in charge of the field investigation and laboratory measurement in Xingtai, Handan, Hengshui, Cangzhou and Langfang city. Jun Zhao did the quality control of laboratory detection. Dr. Shannon Rutherford did the revision and English polishing. The authors thank the staff in endemic control department of CDC of the relevant counties involved in this study for their assistance in the field investigation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lv, S., Zhao, Y., Li, Y. et al. Impact of removing iodized salt on the iodine nutrition of children living in areas with variable iodine content in drinking water. Eur J Nutr 54, 905–912 (2015). https://doi.org/10.1007/s00394-014-0767-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-014-0767-z