Abstract
Purpose
High glycemic load (GL) has been associated with excess stroke risk. Data suggest a different role of diet in the etiology of ischemic and hemorrhagic stroke.
Methods
We analyzed data from 19,824 participants of the Greek cohort of the population-based European Prospective Investigation into Cancer and nutrition (EPIC), who were free of cardiovascular diseases, cancer, and diabetes at baseline and had not developed diabetes. Diet was assessed at enrollment through a validated, interviewer-administered semi-quantitative food frequency questionnaire. The average daily GL was derived using standard tables. We also conducted a meta-analysis on GL and stroke (overall, ischemic and hemorrhagic), using random-effects models.
Results
In the Greek EPIC cohort, 304 incident stroke cases were identified (67 ischemic, 49 hemorrhagic). Using Cox proportional hazards regression models adjusted for potential confounders, the hazard ratios for the highest versus the lowest GL tertiles were 1.07 [95 % confidence interval (CI) 0.74–1.54] for overall stroke, 1.55 (95 % CI 0.72–3.36) for ischemic and 0.48 (95 % CI 0.18–1.25) for hemorrhagic stroke (p-heterogeneity <0.01). The meta-analysis, including a total of 3,088 incident cases and 247 deaths from stroke (1,469 cases and 126 deaths ischemic; 576 cases and 94 deaths hemorrhagic), estimated pooled relative risks for the highest versus the lowest GL levels of 1.23 (95 % CI 1.07–1.41) for overall, 1.35 (95 % CI 1.06–1.72) for ischemic, and 1.09 (95 % CI 0.81–1.47) for hemorrhagic stroke (p-heterogeneity = 0.275).
Conclusions
This study indicates that GL is an important determinant of the more common ischemic—though not of the hemorrhagic—stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ability of different carbohydrates to rise blood glucose is expressed in terms of glycemic index (GI), which is a characteristic of a food, and glycemic load (GL), which is the product of GI by the amount of carbohydrates, and consequently considers both the quality and the quantity of carbohydrates [16]. GL has been positively associated with the risk of both coronary heart disease (CHD) and stroke in a recent meta-analysis [8]. In particular, pooling data from three studies [8], high levels of GL have been associated with about 20 % increased risk of stroke, of borderline statistical significance. No summary data on ischemic and hemorrhagic stroke separately have been reported. Subsequently, the EPICOR study, part of the Italian segment of the European Prospective Investigation into Cancer and nutrition (EPIC), including 355 stroke cases, found a twofold excess risk of stroke for the highest GL quintile compared to the lowest one [30].
We analyzed data from the Greek segment of EPIC cohort to investigate the relation between GL and stroke [25]. Using the same dataset, Misirli et al. [25] found that a favorable effect of Mediterranean diet (MD) was evident for ischemic but not for hemorrhagic stroke. Thus, we have examined GL in relation to ischemic and hemorrhagic stroke for all incident stroke cases for whom this information was available. Moreover, we summarized evidence on GL and stroke from all prospective studies, using a systematic meta-analytic approach. We also estimated summary relative risks (RR) for ischemic and hemorrhagic stroke separately for the first time.
Methods
Cohort study
The data were derived by the Greek EPIC cohort including 28,572 participants recruited between 1994 and 1999, and followed-up to 2009 [23]. The study protocol was approved by the ethics committees of the International Agency for Research on Cancer and the University of Athens Medical School. All participants provided written informed consent, and all procedures were in accordance with the Declaration of Helsinki.
Trained interviewers collected baseline information on several socio-demographic and lifestyle characteristics, medical history, and medication use. Anthropometric and blood pressure measurements were undertaken by trained personnel. Hypertension was based on the blood pressure measurements and on the information on drug use.
A semi-quantitative food frequency questionnaire (FFQ) was used to assess usual intake of about 150 foods and beverages, as well as several complex recipes commonly used in Greece, during the year preceding enrollment. The questionnaire was administered in person by trained interviewers at recruitment. For each dietary item, participants were asked to report their frequency of consumption and portion size. The questionnaire was validated in terms of dietary records, including those that contributed to the computation of GI and GL [10]. In particular, the intraclass correlation coefficients between two FFQs over a period of 1 year were between 0.5 and 0.7 for total caloric intake, polysaccharides, and fiber, in both men and women.
GI values assigned to individual food items of the questionnaire were obtained from the Foster-Powel table [9], British values [13], and Internet updates (http://www.glycemicindex.com), using glucose as the Ref. [29]. Attention was paid to aspects that might influence the GI, including cooking method, preservation method, type of sugar, and country-specific types of foods. For typical Greek recipes for which a GI had not been determined, we assigned the GI of the nearest comparable food, when available, or the GI of their food components or individual ingredients. Food items containing negligible or no carbohydrates (chiefly meat and fish, fats, eggs) were not assigned any values.
We calculated daily dietary GI of each subject by multiplying the GI value of each food item with its carbohydrate content and frequency of consumption, and dividing the sum of these values over all food items by the total amount of carbohydrates consumed. Daily dietary GL of each subject was calculated in the same manner without dividing by the total amount of carbohydrate consumed.
The MD score was computed according to the definition by Trichopoulou et al. [31]. Total energy intake was calculated using a Greek food composition database [32].
Participants were actively followed to record changes in health status, diet, and lifestyle by means of telephone interviews or next of kin in cases of a participant’s death. Specifically, during follow-up, participants were asked to report any health problem they had developed since the last contact, the date of diagnosis, and the place of hospitalization if applicable. When an incident cerebrovascular event or death from cerebrovascular disease was reported, the information was verified, wherever available, through pathology reports, medical records, discharge diagnoses, or death certificates.
The endpoint of interest was incident stroke (ICD-10: codes I60 to I69; codes G45 and G46) [23]. We included only verified first-ever stroke cases, which were confirmed either through medical records for nonfatal first events or, in the case of first events that were fatal, through death certificates. This was a country-wide study, and several hospitals in the country were unable to provide the type of stroke diagnoses (hemorrhagic vs. ischemic).
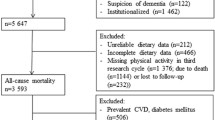
From the initial cohort, we excluded 7,374 participants who had suffered a stroke before enrollment and/or had other selected prevalent conditions (CHD, cancer, diabetes) and/or incident diabetes. After additional exclusion of 928 individuals who could not be traced during the follow-up and of 446 individuals with missing information on at least one of the covariates used in the analysis, the final sample consisted of 19,824 persons.
Time to event was calculated till the date of diagnosis of stroke (for cases) or the date of death from causes other than stroke (censored) or the date of the last contact till December 2009 (censored).
We estimated the hazard ratios (HRs) and corresponding 95 % confidence intervals (CIs), according to tertiles of GL and GI, for stroke overall, as well as for its subtypes, using Cox regression. All estimates were adjusted for sex, age, education, smoking, body mass index (BMI), physical activity, presence of hypertension, MD score, and energy intake without carbohydrates. We presented the results overall and by sex. We also assessed the heterogeneity of the risk across strata of BMI (< and ≥25 kg/m2).
To test for heterogeneity, the likelihood ratio test of the models with and without interaction terms was used.
Meta-analysis
We carried out a literature search of all prospective studies on the relation between GL and the risk of stroke published up to March 2014, using the PubMed and Embase databases, following the rules set up by the PRISMA statement [21]. We used the following string: “(glycemic load OR glycaemic load) AND (stroke OR cerebrovascular).” Studies were included if (1) the outcome was stroke incidence or mortality, (2) they examined the association with GL, (3) they had a prospective design, and (4) they were published as original articles in English. We estimated the pooled RR and the corresponding 95 % CI for the comparison between the highest versus the lowest categories of GL intake. When insufficient information was available to obtain the appropriate effect size, study authors were contacted [2].
Two investigators independently screened titles and abstracts and eventually examined the full text of original articles for study inclusion (Fig. 1). Eighteen publications were identified in PubMed and 44 in Embase, for a total of 45 unique publications. Of these, 37 were excluded by screening of titles and abstracts (30 were not relevant toward the subject matter, and other seven were not original articles), thus leaving eight publications for full-text examination. Among these, one publication [18] did not provide quantitative data on GL and stroke, and one [28] did not provide original data. Thus, considering results from the present cohort, the meta-analysis was based on seven studies [1, 2, 20, 26, 27, 30] including a total of 3,255 cases (3,008 incident stroke, 247 deaths from stroke) overall. Their main characteristics are given in Table 1.
We calculated the summary RR estimate of stroke for the highest versus the lowest category of GL (as reported in each study) using the random-effects model to incorporate between-study heterogeneity [7]. Pooled RRs were calculated also for ischemic and hemorrhagic stroke, separately. The Cochrane Q test and the I 2 statistic were used to evaluate statistical heterogeneity across studies [14].
Results
Cohort study
Overall, 304 incident strokes were identified. Of these, 67 were ischemic and 49 hemorrhagic strokes; no sufficient information on the type of stroke was available for the remaining cases. Table 2 gives HRs of overall stroke, as well as for ischemic stroke and hemorrhagic stroke, in relation to GL tertiles, overall and in strata of sex. The HRs comparing the intermediate and the highest with the lowest GL tertile (baseline) were, respectively, 0.96 (95 % CI 0.72, 1.29) and 1.07 (95 % CI 0.74, 1.54) for overall stroke (p-trend 0.79); 1.30 (95 % CI 0.71, 2.39) and 1.55 (95 % CI 0.72, 3.36) for ischemic stroke (p-trend 0.25); and 0.96 (95 % CI 0.49, 1.90) and 0.48 (95 % CI 0.18, 1.25) for hemorrhagic stroke (p-trend 0.17). The p for heterogeneity for the full models by the type of stroke was significant (<0.01). No clear differences emerged between men and women. However, the numbers were small in strata of sex. We also tested the heterogeneity across strata of BMI, and the risk estimates were consistent in normal and overweight individuals (p for heterogeneity = 0.849).
The results on GI were consistent with those of GL; in particular, the HR for overall stroke was 1.23 (95 % CI 0.90–1.70) for the intermediate and 1.40 (95 % CI 1.03–1.91) for the highest versus the lowest GI tertile (p-trend 0.035).
Meta-analysis
The meta-analysis of GL and stroke is presented in Fig. 2. The pooled RR of stroke for the highest versus the lowest level of GL was 1.23 (95 % CI 1.07–1.41), with low heterogeneity (I 2 = 0.0 %, p = 0.459). Beside our cohort, four other original studies were able to distinguish between ischemic and hemorrhagic stroke, for a total of 1,469 incident cases and 126 deaths from ischemic stroke, and 576 incident cases and 94 deaths from hemorrhagic stroke. The pooled RR was 1.35 (95 % CI 1.06, 1.72; p for heterogeneity among studies = 0.760) for ischemic and 1.09 (95 % CI 0.81, 1.47; p for heterogeneity = 0.193) for hemorrhagic stroke, with a p for heterogeneity between types of stroke of 0.275.
Discussion
The collective evidence points to a positive association between dietary GL and stroke, in line with the previous studies [8, 30]. The association is largely explained by the positive association with ischemic stroke. Available evidence on hemorrhagic stroke from previous studies is less consistent, and our data—as well as results from our meta-analysis—did not support any association.
The apparent heterogeneity in the association of GL with ischemic and hemorrhagic stroke is not surprising, since there is compelling evidence from several studies linking high GL diets with increased incidence of CHD [8], a disease that is overwhelmingly of ischemic nature. The distinct pathogenesis of the two subtypes of stroke is also supported by findings indicating that other aspects of diet, including MD, flavonoids, total antioxidant capacity, and fish consumption, are related to ischemic, but not to hemorrhagic stroke [3, 6, 12, 23]. Moreover, a healthy lifestyle, consisting of abstinence from smoking, low BMI, moderate alcohol consumption, regular exercise, as well as healthy diet, has a greater favorable effect on ischemic than hemorrhagic stroke [4, 18].
High GL diets can lead to the formation of advanced glycation end products, oxidative stress related to hyperglycemia, and consequent inflammation and hence to endothelial impairment and vessel dysfunction [11, 22]. High GL can raise triglycerides and LDL cholesterol concentrations and reduce HDL levels, which are important determinant of ischemic outcomes [22]. Moreover, GL, which leads to more infusion of circulating glucose and higher postprandial insulin levels, has been associated with diabetes [22, 29], a condition that has been found to increase the risk of ischemic but not hemorrhagic stroke [15, 24].
Only one study included in the meta-analysis investigated overall stroke mortality, from a Japanese cohort including 120 deaths among men and 127 among women [26]. GL was not related to overall stroke mortality, but there was a nonsignificant increased risk of both hemorrhagic and ischemic stroke for the highest versus the lowest GL levels in women only [26]. In general, the distinction between ischemic and hemorrhagic stroke, however, is less valid on death certificates than on clinical records on which incidence data frequently are based [19].
Across different populations and countries, there is an appreciable variation in the mean and range of GL. Indeed, data from the EPIC study suggest that the Greek diet considered in this study is characterized by a much lower level of total carbohydrate [5] and GL [33] compared to the Italian and the Dutch diets. Fan et al. [8] in a meta-analysis calculated a pooled RR of 1.05 (95 % CI 1.02–1.08) per 50-unit increment in GL.
Results on the relation between GI and stroke from previous studies were less convincing. Among the six studies [1, 17, 20, 26, 27, 30] on the issue, two cohort studies found a significant positive association with stroke mortality overall [17] and in men [26], whereas the others found null results.
The prospective nature of the study, besides ensuring the temporal relation between exposure and disease, minimizes the likelihood of information bias related to dietary habits recorded after disease occurrence. However, since this is an ongoing study and diet is a modifiable factor, we cannot be confident that the dietary habits of the cohort as recorded at baseline were consistent throughout the follow-up period. This, however, would have probably led to an underestimation of the real association with ischemic stroke. We have excluded individuals with prevalent cardiovascular diseases (including stroke), cancer, and diabetes, as well as incident diabetes, since these conditions may lead to changes in diet after diagnosis. We were not able to evaluate possible differential effects of GL in strata defined by levels of available covariates because of power limitations. As far as confounding is concerned, we were able to adjust for major known or likely risk factors for stroke, including smoking, BMI, physical activity, hypertension, as well as total energy intake.
In conclusion, our data from the Greek EPIC cohort, as well as the analysis of accumulating evidence, indicate that GL is an important determinant of ischemic—but not hemorrhagic—stroke.
References
Beulens JW, de Bruijne LM, Stolk RP, Peeters PH, Bots ML, Grobbee DE, van der Schouw YT (2007) High dietary glycemic load and glycemic index increase risk of cardiovascular disease among middle-aged women: a population-based follow-up study. J Am Coll Cardiol 50:14–21
Burger KN, Beulens JW, Boer JM, Spijkerman AM, Van der AD (2011) Dietary glycemic load and glycemic index and risk of coronary heart disease and stroke in Dutch men and women: the EPIC-MORGEN study. PLoS ONE 6:e25955
Cassidy A, Rimm EB, O’Reilly EJ, Logroscino G, Kay C, Chiuve SE, Rexrode KM (2012) Dietary flavonoids and risk of stroke in women. Stroke 43:946–951
Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB (2008) Primary prevention of stroke by healthy lifestyle. Circulation 118:947–954
Cust AE, Skilton MR, van Bakel MM, Halkjaer J, Olsen A, Agnoli C, Psaltopoulou T, Buurma E, Sonestedt E, Chirlaque MD, Rinaldi S, Tjonneland A, Jensen MK, Clavel-Chapelon F, Boutron-Ruault MC, Kaaks R, Nothlings U, Chloptsios Y, Zylis D, Mattiello A, Caini S, Ocke MC, van der Schouw YT, Skeie G, Parr CL, Molina-Montes E, Manjer J, Johansson I, McTaggart A, Key TJ, Bingham S, Riboli E, Slimani N (2009) Total dietary carbohydrate, sugar, starch and fibre intakes in the European prospective investigation into cancer and nutrition. Eur J Clin Nutr 63(Suppl 4):S37–S60
Del Rio D, Agnoli C, Pellegrini N, Krogh V, Brighenti F, Mazzeo T, Masala G, Bendinelli B, Berrino F, Sieri S, Tumino R, Rollo PC, Gallo V, Sacerdote C, Mattiello A, Chiodini P, Panico S (2011) Total antioxidant capacity of the diet is associated with lower risk of ischemic stroke in a large Italian cohort. J Nutr 141:118–123
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Fan J, Song Y, Wang Y, Hui R, Zhang W (2012) Dietary glycemic index, glycemic load, and risk of coronary heart disease, stroke, and stroke mortality: a systematic review with meta-analysis. PLoS ONE 7:e52182
Foster-Powell K, Holt SH, Brand-Miller JC (2002) International table of glycemic index and glycemic load values: 2002. Am J Clin Nutr 76:5–56
Gnardellis C, Trichopoulou A, Katsouyanni K, Polychronopoulos E, Rimm EB, Trichopoulos D (1995) Reproducibility and validity of an extensive semiquantitative food frequency questionnaire among Greek school teachers. Epidemiology 6:74–77
Goldin A, Beckman JA, Schmidt AM, Creager MA (2006) Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation 114:597–605
He K, Rimm EB, Merchant A, Rosner BA, Stampfer MJ, Willett WC, Ascherio A (2002) Fish consumption and risk of stroke in men. JAMA 288:3130–3136
Henry CJ, Lightowler HJ, Strik CM, Storey M (2005) Glycaemic index values for commercially available potatoes in Great Britain. Br J Nutr 94:917–921
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Janghorbani M, Hu FB, Willett WC, Li TY, Manson JE, Logroscino G, Rexrode KM (2007) Prospective study of type 1 and type 2 diabetes and risk of stroke subtypes: the Nurses’ Health Study. Diabetes Care 30:1730–1735
Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV (1981) Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr 34:362–366
Kaushik S, Wang JJ, Wong TY, Flood V, Barclay A, Brand-Miller J, Mitchell P (2009) Glycemic index, retinal vascular caliber, and stroke mortality. Stroke 40:206–212
Kurth T, Moore SC, Gaziano JM, Kase CS, Stampfer MJ, Berger K, Buring JE (2006) Healthy lifestyle and the risk of stroke in women. Arch Intern Med 166:1403–1409
Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, La Vecchia C (2009) Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: an update. Eur J Cardiovasc Prev Rehabil 16:333–350
Levitan EB, Mittleman MA, Hakansson N, Wolk A (2007) Dietary glycemic index, dietary glycemic load, and cardiovascular disease in middle-aged and older Swedish men. Am J Clin Nutr 85:1521–1526
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Ludwig DS (2002) The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA 287:2414–2423
Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D, Trichopoulou A (2012) Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol 176:1185–1192
Murakami Y, Huxley RR, Lam TH, Tsukinoki R, Fang X, Kim HC, Woodward M (2012) Diabetes, body mass index and the excess risk of coronary heart disease, ischemic and hemorrhagic stroke in the Asia pacific cohort studies collaboration. Prev Med 54:38–41
Neaton JD, Wentworth DN, Cutler J, Stamler J, Kuller L (1993) Risk factors for death from different types of stroke. Multiple risk factor intervention trial research group. Ann Epidemiol 3:493–499
Oba S, Nagata C, Nakamura K, Fujii K, Kawachi T, Takatsuka N, Shimizu H (2010) Dietary glycemic index, glycemic load, and intake of carbohydrate and rice in relation to risk of mortality from stroke and its subtypes in Japanese men and women. Metabolism 59:1574–1582
Oh K, Hu FB, Cho E, Rexrode KM, Stampfer MJ, Manson JE, Liu S, Willett WC (2005) Carbohydrate intake, glycemic index, glycemic load, and dietary fiber in relation to risk of stroke in women. Am J Epidemiol 161:161–169
Ross CM (2005) Re: carbohydrate intake, glycemic index, glycemic load, and dietary fiber in relation to risk of stroke in women. Am J Epidemiol 161:995
Rossi M, Turati F, Lagiou P, Trichopoulos D, Augustin L, La Vecchia C, Trichopoulou A (2013) Mediterranean diet and glycemic load in relation to type 2 diabetes. Diabetologia. doi:10.1007/s00125-013-3013-y
Sieri S, Brighenti F, Agnoli C, Grioni S, Masala G, Bendinelli B, Sacerdote C, Ricceri F, Tumino R, Giurdanella MC, Pala V, Berrino F, Mattiello A, Chiodini P, Panico S, Krogh V (2013) Dietary glycemic load and glycemic index and risk of cerebrovascular disease in the EPICOR cohort. PLoS ONE 8:e62625
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348:2599–2608
Trichopoulou A, Georga K (2004) Composition Tables of Foods and Greek Dishes. Athens, Greece, Parisianos
van Bakel MM, Kaaks R, Feskens EJ, Rohrmann S, Welch AA, Pala V, Avloniti K, van der Schouw YT, van der AD, Du H, Halkjaer J, Tormo MJ, Cust AE, Brighenti F, Beulens JW, Ferrari P, Biessy C, Lentjes M, Spencer EA, Panico S, Masala G, Bueno-de-Mesquita HB, Peeters PH, Trichopoulou A, Psaltopoulou T, Clavel-Chapelon F, Touvier M, Skeie G, Rinaldi S, Sonestedt E, Johansson I, Schulze M, Ardanaz E, Buckland G, Tjonneland A, Overvad K, Bingham S, Riboli E, Slimani N (2009) Dietary glycaemic index and glycaemic load in the European Prospective Investigation into Cancer and Nutrition. Eur J Clin Nutr 63(Suppl 4):S188–S205
Acknowledgments
The research leading to these results has received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under CHANCES Project grant agreement no. HEALTH–F3-2010-242244. The work of CLV, MR, and FT was partially supported by the Italian Foundation for Cancer Research (AIRC), Milan, Italy. The authors thank Ms Garimoldi for editorial assistance.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Carlo La Vecchia and Antonia Trichopoulou share senior co-authorship.
Rights and permissions
About this article
Cite this article
Rossi, M., Turati, F., Lagiou, P. et al. Relation of dietary glycemic load with ischemic and hemorrhagic stroke: a cohort study in Greece and a meta-analysis. Eur J Nutr 54, 215–222 (2015). https://doi.org/10.1007/s00394-014-0702-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-014-0702-3