Abstract
Purpose of Review
Diet and lifestyle patterns are considered major contributory factors for cardiovascular disease (CVD) and mortality. In particular, consuming a diet higher in carbohydrates (not inclusive of fruits and vegetables, but more processed carbohydrates) has been associated with metabolic abnormalities that subsequently may increase the risk of CVD and related mortality. Glycemic index (GI) and glycemic load (GL) are values given to foods based on how fast the body converts carbohydrates into glucose also referred to as the glycemic burden of carbohydrates from foods. Conflicting associations of how high GI and GL influence CVDs have been observed even in high-quality meta-analysis studies. We synthesize and report the associations of high GI and GL with various CVDs by sex, obesity, and geographical locations using an updated review of meta-analysis and observational studies.
Recent Findings
We identified high GI or high GL is associated with an increased risk of CVD events including diabetes (DM), metabolic syndrome (MS), coronary heart disease (CHD), stroke, and stroke mortality in the general population, and the risk of CVD outcomes appears to be stratified by sex, obesity status, and preexisting CVD. Both high GI and GL are associated with DM and CHD in the general population. However, high GI is strongly associated with DM/MS, while high GL is strongly associated with an increased risk of CHD in females. In addition, high GL is also associated with incident stroke, and appears to be associated with CVD mortality in subjects with preexisting CVD or high BMI and all-cause mortality in non-obese DM subjects. However, high GI appears to be associated with CVD or all-cause mortality only in females without CVD.
Summary
High GI/GL is an important risk factor for CVD outcomes in the general population. High GI seems to be markedly associated with DM/MS, and it may enhance the risk of CVD or all-cause mortality in both sexes and predominately females. Although both high GI and high GL are risk factors for CHD in females, high GL is associated with CVD outcomes in at-risk populations for CVD. These data suggest that while high GI increases the propensity of CVD risk factors and mortality in healthy individuals, high GL contributes to the risk of severe heart diseases including CVD or all-cause mortality, particularly in at-risk populations. These data indicate dietary interventions designed for focusing carbohydrate quality by lowering both GI and GL are recommended for preventing CVD outcomes across all populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the major cause of morbidity and mortality worldwide [1, 2]. Continuous rise in obesity and metabolic syndrome has led to major growth in CVD outcomes globally [3]. The increasing trend in obesity and metabolic abnormalities associated with CVD outcomes has been strongly associated with suboptimal diet quality and lifestyles [4, 5]. Specifically, a diet consisting of high carbohydrates which are predominantly coming from processed foods containing fats has been adversely associated with glucose metabolism and lipid accumulation [6]. Dietary carbohydrates impact postprandial blood glucose levels by altering the physiological responses of carbohydrate digestion. These include differences in their physical forms, chemical structures, particle sizes, food processing and storage, and fiber contents [7••]. Hence, highly processed simple sugars or high carbohydrate diets have been associated with several CVD risk factors. The global burden of disease study reported diet is a major determinant of CVD risk factors [8, 9]. Physicians and researchers around the world have raised concerns related to high carbohydrate intake associated with increased risk of CVDs. However, the consensus is that the suboptimal diet quality measured using the quality of carbohydrate diets (measured by amounts and types of carbohydrates, fats, proteins, sugars, fibers, and its impact on blood glucose level) is more important than the quantity of carbohydrate diets (simply high versus low carbohydrate diets) in improving population health [10, 11]. Glycemic index (GI) and glycemic load (GL) are used as markers for measuring the quality of carbohydrate diets. The GI characterizes the rate of absorption of a carbohydrate food as glucose compared with a reference standard carbohydrate food, whereas GL measures the overall glycemic burden after food consumption by accounting for the quantity of carbohydrates in foods [12, 13]. The association of poor quality diet especially indicated through the high GI and high GL with CVD incident and mortality has been studied intensively [14•]. However, the associations have been inconsistent in studies depending on the study population and type of CVD event [15, 16]. Since dietary intake is a modifiable factor, it becomes critical to understand the associations of GI and GL with CVD and mortality. Due to inconsistent associations, the relevance of the topic and associated public health implications for developing prevention strategies, multiple meta-analyses have been conducted over the years which have yielded conflicting findings [17, 18]. Although a study recently highlighted the higher quality of evidence of dietary fibers or quality food sources (whole grains) over the GI/GL in relation to CVDs [19••], our primary focus of this review is to assess the effects of high GI and high GL diets on CVD outcomes.
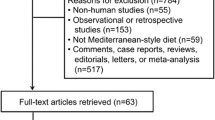
We performed a comprehensive, qualitative, and conceptual review by utilizing meta-analysis and observational studies to update the understanding of GI/GL and CVD association. The primary focus of our review is to summarize the effects of continuous GI/GL as well as categorized GI/GL (highest quantile vs. lowest quantile) on CVD outcomes including coronary heart disease (CHD), heart failure (HF), myocardial infarction (MI), stroke, and all-cause mortality in general and at-risk populations. In addition, we also generated evidence for diabetes, hypertension, and subclinical coronary atherosclerosis in relation to GI/GL. The controversial association was mostly pertaining to obesity or high body mass index (BMI) [14•, 20], pre-existing CVDs [14•, 21, 22], and sex [20, 23, 24], and thus, we attempt to synthesize evidence according to these prominent components. Given the data relating GI/GL with CVD is limited for low- and middle-income countries (LMIC) even with a high incidence of CVD deaths in LMIC and heterogeneity in dietary patterns [14•], we further evaluated the relationship of GI/GL with CVD outcomes according to different geographic regions. Table 1 provides the meta-analysis studies for the association between GI/GL with CVD risk factors, while Table 2 provides the studies used for summarizing the evidence for the association between GI/GL with CVD outcomes. Table 3 displays data from intervention studies. The magnitude of the effect or association was summarized with a relative risk (RR) measure either with risk ratio or hazard ratio (HR) or odds ratio (OR), or mean differences (weight mean difference (WMD) or standardized mean difference (SMD)) along with 95% confidence interval (CI).
Associations of GI and GL with CVD Risk Factors
A number of studies yielded a positive association between high GI/GL and risk of diabetes due to increasing postprandial glycemia or bodyweight that subsequently leads to increased hyperglycemia, hyperinsulinemia, and beta-cell dysfunctions [25]. We found 8 meta-analysis studies confirming the significant association between high GI and the increased risk of diabetes with RR varying between 1.12 and 1.40 [18, 19••, 23, 26–29, 30••]. These associations remained statistically significant even with continuous increases in GI levels. The magnitude of association varies between 1.08 and 1.27 depending on a 5–10-point increase in GI levels [19••, 23, 27, 28]. Similarly, the majority of meta-analysis studies except Reynolds et al. [19••] further confirmed a strong association between high GL and the increased risk of diabetes with RR varying between 1.13 and 1.27. The association between increased GL levels and an increased risk of diabetes was consistent with varying effect sizes (RR: 1.03–1.45) depending on a 20–100 unit increase in GL levels. Reynolds et al. [19••] did not find any association of categorized GL (RR = 1.01; 95%CI: 0·92–1.11) or continuous GL (RR = 0·99; 9%%CI: 0·98 to 1·00) with an increased risk of diabetes using a meta-analysis of 15 datasets. This may be due to the inclusion of European studies as 4 out of 5 European studies did not show any association between GL and incident diabetes. This observation was validated by a large meta-analysis study [30••] based on 40 studies yielding no significant effect of increased GI/GL on diabetes in European studies compared to the USA and Asian studies. However, this study reported a greater effect of GL on diabetes (RR = 1.26; 95%CI: 1.08, 1.47) among high BMI individuals in European studies. Moreover, the positive association of GI/GL with diabetes was consistently observed across countries among high BMI individuals [30••]. Although limited meta-analysis studies [23, 28, 30••] reported the association between GI/GL and diabetes by sex, it seems both GI and GL strongly associated with diabetes in females, while only GI associated with an increased risk of diabetes in males. Two meta-analysis studies [31, 32] were available for determining an association between GI/GL and metabolic syndrome (MS). Both meta-analysis studies produced a strong association between high GI and increased odds of MS. However, the association between GL and MS was not statistically significant regardless of sex. Furthermore, the increased levels of GI were associated with the increased odds of MS in both sexes. These findings altogether suggest that high GI and GL are associated with increased risk of diabetes in the general population and across countries. Both measures are critical for preventing diabetes in females and high BMI individuals, while the GI measure is useful for diabetes in males as well as for MS in both sexes. In European individuals, GL might be a more useful measure for diabetes risk stratification than GI.
Associations of GI and GL with CVD and CHD
High carbohydrate intake, and specifically those carbohydrates which increase GI, has been linked with hyperglycemia and hypertriglyceridemia by manipulating lipid profile which eventually can increase the risk of CHD [33]. Only two meta-analysis studies [16, 19••] reported the association of GI/GL with CVD events. One of these studies [16] yielded a strong association of CVD events with high GI and high GL particularly in females, while the other meta-analysis study [19••] based on two studies showed no association between GI and CVD events. However, this meta-analysis using one study showed a 10-unit increase in GL levels significantly associated with a 4% increased risk of CVD events. A total of 9 meta-analysis studies were available for examining the association between GI/GL and CHD [6, 7••, 16, 18, 19••, 24, 26, 30••, 34]. Of these studies, seven studies reported the pooled association between GI/GL and CHD, while one study [30••] reported the association separately for geographical locations, and another study [34] reported the combined association of GI or GL with CHD. Of eight meta-analysis studies, 6 studies [7••, 16, 18, 24, 26, 34] confirmed a strong positive association (RR: 1.13–1.25) between high GI and the increased risk of CHD. Although not statistically significant, the other two studies [6, 19••] showed a marginal association (RR = 1.11; 95%CI: 0.99–1.24; RR = 1.08; 95%CI: 0.96–1.20) between high GI and CHD. The association between high GI and increased risk of CHD was further confirmed with a dose–response meta-analysis study (RR = 1.24; 95%CI: 1.12–1.38) by Livesey et al. [24] and a larger study by Jenkins et al. [14•] representing a more diverse population (RR = 1.14; 95%CI 1.02–1.27). All meta-analysis studies [6, 7••, 24, 26, 34] reporting association separately for each sex showed no association between high GI and CHD in males (RR range: 0.87–1.10); however, studies consistently reported a strong association between high GI and CHD in females (RR range: 1.24–1.69) and confirmed in the dose–response analysis as well (RR = 1.24; 95%CI: 1.12–1.38). No association between high GI and the risk of CHD in males was persistently found regardless of obesity status or geographical status. Jenkins et al. [12] reported that subjects with high GI had an increased risk of CHD among those with preexisting CVD (RR = 1.49; 95%CI: 1.20–1.85) or high BMI (RR = 1.38; 95%CI: 1.22–1.55). Furthermore, high GI was associated with the increased risk of CHD among overweight or obese individuals in a large study particularly in women and European studies [7••, 30••]. High GL was also associated with an increased risk of CHD (RR range: 1.13–1.36) except for one meta-analysis study that was based on merely two studies [18] and one cohort study [14•]. The magnitude of association was higher for GL compared to GI in relation to CHD outcome, albeit to a greater extent than GI in dose–response analysis. Like GI, the majority of meta-analysis studies reported high GL as a significant risk factor for CHD in females but not in males. Livesey et al. [24] and Sieri et al. [20] exceptionally found a strong link between high GL and CHD in males. The association between high GL and increased risk of CHD was markedly high in high BMI individuals particularly in female studies (RR = 1.82; 95%CI: 1.44–2.31) [7••], a US study (RR = 1.97; 95%CI: 1.31–2.96) [30••], European studies (RR = 1.63; 95%CI: 1.28–2.07) [30••], and an Asian study (RR = 1.87; 95%CI: 0.98–3.55) [30••]. Subjects with CVD had also shown an increased risk of CHD in relation to high GL (RR = 1.31; 95%CI: 1.02–1.69) [14•]. A cross-sectional study [35] on 28,429 asymptomatic Korean subjects demonstrated a greater adjusted prevalence of detectable coronary artery calcium, a major risk factor for coronary atherosclerosis, in the highest quintile of GI (1.74; 95%CI:1.08–2.81) and GL (3.04; 95%CI: 1.43–6.46). Turati et al. [36] estimated that a high dietary GL intake adhering to the Mediterranean diet was associated with a high incidence of CHD in males and subjects with higher BMIs. These findings suggest that high dietary GI/GL is a risk factor for CHD in normal individuals. Higher GL levels significantly increase the risk of CHD albeit to a greater extent than high GI in the general population. Both measures are significantly associated with CHD only in females and high BMI females across geographical locations. However, the combined use of high GI/GL is more appropriate for evaluating the risk of CHD particularly in females, while the GL measure is more useful among high BMI or CVD individuals across geographic locations. In males, a higher increase (50–65 g/day) of GL may be useful for evaluating the risk of CHD.
Associations of GI and GL with Stroke, MI, and HF
High GI and GL diets can induce endothelial and vessel dysfunctions by affecting glycemic mediated oxidative stress, inflammation, glucose homeostasis, hormonal responses, and adipose-related pathways [7••, 33, 37]. These changes may lead to various CVDs including atherosclerosis, coronary artery disease, stroke, MI, and HF. A total of 7 meta-analysis studies (5 GI studies, 6 GL studies, 1 GI/GL study by geographic locations) were included to synthesize findings associated with stroke risk in relation to high GI/GL [7••, 16, 18, 19••, 30••, 38, 39]. None of the GI studies showed a significant association with stroke risk (RR range = 1.00–1.10) except for one study [19••] which also did not find a significant association with a continuous form of GI measure. However, Jenkins et al. [14•] showed a high risk of stroke associated with high GI in subjects with (RR = 1.71; 95%CI: 1.21–2.40) or without (RR = 1.24; 95%CI: 1.02–1.50) CVD. High GI appears to be also associated with an increased risk of stroke in high BMI individuals in a US study (RR = 1.39) and in males of European studies (RR = 1.12) and females of an Asian study (RR = 1.19) [30••]. In contrast, high GL was consistently associated with increased risk (RR range: 1.19–1.23) of stroke particularly for ischemic stroke than hemorrhagic stroke [39] and the association was confirmed in the dose–response analysis of GL as well[19••]. Only one meta-analysis based on only two studies [18] did not show a significantly increased risk of stroke with high GL (RR = 1.28; 95%CI: 0.83, 1.98). Although not statistically significant, a high risk of stroke associated with high GL (RR = 1.45; 95%CI: 0.98–2.14) was also observed in Jenkins et al. study [14•]. In the stratified analysis of geographical location, a strong association between high GL and incident CHD was also observed in high BMI individuals (RR = 1.60) in the USA and females (RR = 1.26) in Asia [30••]. Additionally, two cohort studies [40, 41] yielded no significant association between GI or GL with MI in middle-aged and older Swedish men or Swedish women. Similarly, a cohort study [42] did not find a statistically significant increased risk of HF in relation to high GI (RR = 1.12; 95%CI: 0.87–1.45) or GL (RR = 1.30; 95%CI: 0.87–1.93) in middle-aged and elderly Swedish women. These findings suggest that high GL but not high GI is a risk factor for incident stroke in general and high BMI subjects. Furthermore, it seems high GI/GL is associated with an increased risk of stroke among at-risk individuals (with preexisting CVD or high BMI) as well. However, no clear association has been established between high GI/GL with the increased risk of HF or MI based on limited studies.
Associations of GI and GL with CVD, CHD or Stroke Mortality and All-Cause Mortality
There were four meta-analysis studies available for evaluating the effect of high GI/GL on all-cause mortality or cause-specific mortality [7••, 15, 19••, 30••]. Most of these studies reported the effect of high GI/GL on all-cause mortality in the overall population with one exception [15] that also reported sex-specific effects of GI/GL on all-cause mortality. None of the studies showed a significant adverse effect of high GI/GL on all-cause mortality in the overall population. However, one large meta-analysis based on 18 studies [15] including 251,497 subjects demonstrated a significant association between high GI and all-cause mortality (RR = 1.17; 95%CI: 1.02–1.35) in women only. Although not significant, this study also showed a higher risk of all-cause mortality associated with high GL (RR = 1.31; 95%CI: 0.95–1.80). In addition, Burger et al. [22] found that high GL was associated with an increased risk of all-cause mortality only (RR = 1.42; 95%CI: 1.07–1.88) in non-obese diabetic individuals. The meta-analysis studies indicating a non-significant association between GI/GL and all-cause mortality could not present data separately for DM and non-DM populations due to limited studies. Other than one meta-analysis study [19••] (RR with high GI = 1.23; 95%CI: 1.06–1.41), none of the studies yielded a pooled significant association between CVD mortality and high GI/GL or according to sex (RR range: 0.96–1.18). Subjects with CVD were identified at increased risk of CVD mortality associated with high GL (RR = 1.46; 95%CI: 1.01–2.10), while high GI (RR = 1.32; 95%CI: 1.08–1.61) was associated with CVD mortality in subjects without CVD [14•]. Compared to low GL, high GL was also associated with an increased hazard of CVD mortality (RR = 2.02; 95%CI: 1.06–3.82) among high BMI individuals consuming the Mediterranean diet [36]. In addition, stroke mortality was also found to be associated with a high GI (RR = 1.58; 95%CI: 1.29–1.93) and with per 10 unit increase in GL levels (RR = 1.10; 95%CI: 1.06–1.14) [19••]. Although not statistically significant, another meta-analysis study [7••] showed a higher risk of stroke mortality associated with a high GI (RR: 1.43; 95%CI: 0.98–2.09). For CHD mortality, one study [19••] reported no association between GI/GL and CHD mortality. Based on the preliminary evidence, we can infer that high GI/GL levels seem to be associated with stroke mortality, while high GI levels may be associated with all-cause mortality or CVD mortality only in specific population particularly in women or without CVD populations. Moreover, high GL seems to be associated with an increased risk of CVD mortality in subjects with a history of CVD/obesity and with all-cause mortality in non-obese DM subjects.
Effect of low GI/GL diets on CVD Risk Factors
Although no meta-analysis study is available to demonstrate a direct effect of GI/GL on CVD events, most of the interventional studies showed a positive influence of dietary intervention with low GI or GL on CVD risk factors. Reducing the GI/GL has consistently shown improvements in fasting blood glucose (FBG), hemoglobin A1C (HbA1c), and body weight (BW) in diabetes [43–45, 46•, 47, 48••] but not in general individuals [19••, 46•, 49, 50]. However, a large meta-analysis [51] showed a stronger effect of reduction in GI/GL diets on glycemic control including FBG, HbA1c, insulin sensitivity, and fasting insulin in the general population. Fasting triglycerides and BW were also improved with a greater reduction in GL than GI. A higher reduction in GI (> 19 units) was also associated with a significant reduction in HbA1c [46•]. Furthermore, significant improvements in fat mass (FM), BMI or weight loss, total cholesterol (TC), and low-density lipoprotein (LDL) after low GI diets were observed in DM and general populations [48••, 49, 52, 53] with an exception of a DM study[47]. However, a favorable effect of low GI/GL on triglycerides and inflammatory markers (C-reactive protein-CRP or interleukin-6) was noticed in only two meta-analysis studies [47, 48••]. A meta-analysis on DM subjects [45] reporting stratified analysis by geographic location showed that low GI diet interventions significantly reduced HbA1c in Australian and American studies but not in European studies. Short-term improvements in postprandial blood glucose levels were also noticed by lowering breakfast GI/GL in metabolically impaired or healthy subjects [54]. In overweight/obese adult subjects, a significant effect of low GI/GL intervention was also observed on HbA1c or FBG [46•] or fasting insulin [55], lipids (TC and LDL) [56], adiposity measures, and CRP [55, 56]. However, a reduction in GI by 20 points showed improvements in BW, body fat, and TC, and LDL but not in HDL and triglycerides among overweight and obese individuals [49]. The effect of low GI/GL on triglycerides and insulin resistance was significant but not on other parameters in overweight and obese children [57]. Women with gestation diabetes also had improvements in glycemic controls and neonatal outcomes after low GI/GL diets compared to controls [58], particularly in the Chinese population with more changes associated with low GL than low GI diet interventions [59] but not in another meta-analysis study [60]. Furthermore, a reduction in GI showed improvement in diastolic blood pressure, while a reduction in GL showed improvements on both systolic and diastolic blood pressures [61]. These studies indicate that combined reduction in GI/GL produces favorable benefits in improving glycemic control, BW and BMI, TC, and LDL in average-risk/general, obese, or DM populations. A higher reduction in GI/GL appears to be more associated with lipids and body weight improvements.
Summary and Conclusions
In this review, we present a framework for the association between high GI/GL and CVD or mortality in the general and specific subpopulations (Fig. 1A) and summarize the effect of low GI/GL diets on different cardiometabolic parameters (Fig. 1B). Our data indicate that high GI is associated with CVD outcomes in average-risk or general subjects, while high GL is associated with CVD outcomes in at-risk populations. The increased levels of GL are expected to produce more harmful effects than GI as GL incorporates both quality and quantity of carbohydrate content of diets [7••]. Compared to high GI, individuals with high GL diets may require higher insulin demand that may accelerate metabolic imbalances resulting in the increased risk of more severe heart diseases, particularly in at-risk populations. Furthermore, reducing GL intake showed improvements on both systolic and diastolic blood pressures, while low GI diets only showed improvements in diastolic blood pressure in addition to fasting blood glucose, HbA1C, and fasting insulin suggesting managing GL might be more useful for preventing severe heart diseases. The association between high GL and stroke has been consistently observed in our review yet the association between high GI and stroke is unclear and this may be partly due to combined analysis of two different subtypes of stroke and non-linear relationship [62]. Although the association of high GL with CHD and stroke is more pronounced than high GI, the association of high GI with DM, MS, and stroke and CVD mortality was markedly stronger than high GL in the general/average-risk population. This could be due to differences in GI and GL measures and related clinical outcomes. By definition, diets with low GI and high carbohydrates can have the same GL with diets having high GI and low carbohydrates. However, while having the same GL with these different combinations can have different effects on metabolic outcomes [63]. Thus, there may be a non-linear relationship between GL levels and CVD risk factors in average-risk populations as a study [64] identified lower risk of abnormal metabolic profiles and diabetes associated with moderate levels of GL rather than lower or higher levels of GL. Moreover, the heterogeneous and complex nature of GL further explains differential clinical outcomes associated with GL compared to GI [15]. Our review clearly implies that a joint evaluation of GI and GL with an optimum threshold is more useful than a single measure for the prevention and management of CVDs.
A Summary for the association between GI/GL and CVD outcomes. B Summary effect of GI/GL on glycemic control, blood lipids, adiposity, inflammatory markers, and blood pressure. The thick line indicates a stronger association compared to a thin line. GI glycemic index, GL glycemic load, DM diabetes mellitus, MS metabolic syndrome, CHD coronary heart disease, CVD cardiovascular disease, BMI body mass index, BW body weight, WL weight loss, WC waist circumference, FM fat mass, FFM fat free mass, CRP C-reactive protein, IL-6 interleukin-6, HbA1c hemoglobin A1C, TG triglyceride, TC total cholesterol, LDL low-density lipoprotein, HDL high-density lipoprotein, SBP systolic blood pressure, DBP diastolic blood pressure
Although the relationship between high GI/GL with DM/MS was prominent irrespective of sex, the association between GI/GL and CHD was only consistent in females but not in males. There could be multiple reasons for this finding: (1) high glycemic diet response was associated with greater increase in serum triglycerides and a greater decrease in serum HDL concentrations in women than in men [65]; (2) more elevated serum triglyceride concentrations[66] and dietary GI/GL induced diabetes are strongest risk factors of CVDs in women [20, 40, 67]; (3) there is an interplay between dietary intake, obesity, insulin resistance, and androgen status in women [68–70] as low GI/GL diet intervention has been shown to be associated with improvements in cardiometabolic and androgen status in polycystic ovary syndrome women [71]; (4) variations in GI/GL levels between men and women yielded more variation in GI levels in men than women producing different statistical powers for detecting significant associations [6]; (5) genetic and racial/ethnic differences appear to impact these associations as high GL is associated with CHD in Asian and European males [30••]; and lastly (6), there appears to be a different threshold due to non-linear relationships between GI/GL and CHD in males when compared to females [62, 64]. There also appears to be a reporting bias and measurement errors of GI/GL diets between sexes [6], and adjustment or stratification based on other factors such as fat, protein, sugar intake, and comorbidities may produce different associations between GI/GL and CHD by sex. Regardless of sex differences, it is difficult to disassociate the effect of GI/GL on CVDs from high-quality food sources, fibers, proteins, and fat. However, the effect sizes of high GI/GL associated with DM/MS, CHD, stroke, and stroke mortality were either similar or even found to be greater than the effect sizes reported for high fiber or whole grains in another study [19••]. Although not too strong, the association of high GI/GL with incident DM and CHD particularly in females that appears to be causal as confirmed by most criteria of Bradford-Hill including the strength of association displaying an even lower confidence limit of RR is greater than 1.10, consistency of association confirmed in multiple meta-analysis studies, specificity was met by various sensitivity and adjusted analyses, temporality was met by the cohort design of studies included in most meta-analysis studies, dose–response was also met in the dose–response meta-analysis studies, and plausibility, experimental, analogy, and coherence criteria were met with the possible underlying mechanisms which were testified with interventional studies [25]. Meta-analysis of interventional studies also demonstrated the potential benefits of low GI/GL diets on glycemic control, weight changes, and lipids [46•, 48••, 51].
Some discrepancies in meta-analysis results are expected in this review, and the quality of the studies may be low for multifactorial reasons to include (1) the majority of the meta-analysis studies reported results after combining studies with different quantile ranges of GI/GL; (2) the results were not adjusted for different ranges of GI/GL across studies; (3) limited studies performed the dose–response meta-analysis; (4) studies included varying dietary instruments, sometimes inadequately validated instruments for measuring GI/GL, and measurement bias due to non-standardized protocols for measuring GI/GL from a wide range of diets; (5) studies did not also account for overall dietary patterns including macronutrient ratios, micronutrients contents, and food sources varying within geographic regions; (6) performed analyses based on heterogeneous studies in terms of follow up, factors adjustment, and effect size measures and concluded possibly in the presence of heterogeneity, publication bias, and lack of high-quality studies; and (7) lastly, not all studies reported subgroup analysis by known modifiers such as sex, geographical regions, and preexisting comorbidities. Baseline measures of GI/GL have been used in most of these studies and longitudinal changes in GI/GL measures may further provide more insightful information between GI/GL with CVDs. Despite these limitations in studies included in this umbrella review, the most convincing evidence is that high GI/GL or an increased level of GI/GL is associated with increased incidents of CVDs including DM/MS and stroke in the general population and CHD in females.
In conclusion, high GI and GL are risk factors for CVDs in average and at-risk populations. However, the association of GI/GL is modified by sex, obesity or CVD status, and racial/ethnic populations. Although limited evidence, high GI/GL may also influence CVD and all-cause mortality in some specific populations. The association of high GI/GL is not clear with heart failure, myocardial infarction, atrial fibrillation, and sudden cardiac death due to limited or no studies. A lower GI/GL can be more flexibly achieved in different settings by promoting food and dietary patterns with high-quality food sources of carbohydrates such as whole grains and fruits, high soluble fiber and plant protein intakes, and reducing saturated fat and simple sugars, and these may offer favorable health benefits including a reduction in CVD risk compared to regional specific foods. Given the feasibility of adapting low GI/GL diets, high-quality diets with low GI/GL carbohydrates should be encouraged for improving CVD and population health along with other lifestyle changes. However, high-quality interventional research is needed to assess the longitudinal changes in GI/GL diets associated with improvements in CVD conditions with proper risk stratifications using metabolically unhealthy obesity status and cardiorespiratory fitness levels by incorporating clinical, genetic, sex, food quality, and racial/ethnic differences to identify the optimum threshold and target populations for achieving favorable benefits from dietary interventions designed for lowing GI/GL levels.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Azimova K, San Juan Z, Mukherjee D. Cardiovascular safety profile of currently available diabetic drugs. Ochsner J. 2014;14(4):616–32.
Mukherjee D, Eagle KA. Improving quality of cardiovascular care in the real world: how can we remove the barriers? Am J Manag Care. 2004;10(7 Pt 2):471–2.
Dwivedi AK, Dubey P, Cistola DP, Reddy SY. Association between obesity and cardiovascular outcomes: updated evidence from meta-analysis studies. Curr Cardiol Rep. 2020;22(4):25. https://doi.org/10.1007/s11886-020-1273-y.
Liu B, Du Y, Wu Y, Snetselaar LG, Wallace RB, Bao W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011–18: population based study. BMJ. 2021;372: n365. https://doi.org/10.1136/bmj.n365.
Lee SE, Han K, Kang YM, Kim SO, Cho YK, Ko KS, et al. Trends in the prevalence of metabolic syndrome and its components in South Korea: findings from the Korean National Health Insurance Service Database (2009–2013). PLoS ONE. 2018;13(3): e0194490. https://doi.org/10.1371/journal.pone.0194490.
Mirrahimi A, de Souza RJ, Chiavaroli L, Sievenpiper JL, Beyene J, Hanley AJ, et al. Associations of glycemic index and load with coronary heart disease events: a systematic review and meta-analysis of prospective cohorts. J Am Heart Assoc. 2012;1(5): e000752. https://doi.org/10.1161/JAHA.112.000752.
•• Fan J, Song Y, Wang Y, Hui R, Zhang W. Dietary glycemic index, glycemic load, and risk of coronary heart disease, stroke, and stroke mortality: a systematic review with meta-analysis. PLoS ONE. 2012;7(12): e52182. https://doi.org/10.1371/journal.pone.0052182. (This is one of the first meta-analysis studies reporting the effects of quantitive and categorized GI and GL on CVD outcomes by gender and obesity status.)
Anand SS, Hawkes C, de Souza RJ, Mente A, Dehghan M, Nugent R, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system: a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015;66(14):1590–614. https://doi.org/10.1016/j.jacc.2015.07.050.
Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343(1):16–22. https://doi.org/10.1056/NEJM200007063430103.
Sievenpiper JL. Low-carbohydrate diets and cardiometabolic health: the importance of carbohydrate quality over quantity. Nutr Rev. 2020;78(Suppl 1):69–77. https://doi.org/10.1093/nutrit/nuz082.
Riccardi G, Costabile G. Carbohydrate quality is key for a healthy and sustainable diet. Nat Rev Endocrinol. 2019;15(5):257–8. https://doi.org/10.1038/s41574-019-0190-x.
Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, et al. Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr. 1981;34(3):362–6. https://doi.org/10.1093/ajcn/34.3.362.
Salmeron J, Ascherio A, Rimm EB, Colditz GA, Spiegelman D, Jenkins DJ, et al. Dietary fiber, glycemic load, and risk of NIDDM in men. Diabetes Care. 1997;20(4):545–50. https://doi.org/10.2337/diacare.20.4.545.
• Jenkins DJA, Dehghan M, Mente A, Bangdiwala SI, Rangarajan S, Srichaikul K, et al. Glycemic index, glycemic load, and cardiovascular disease and mortality. N Engl J Med. 2021;384(14):1312–22. https://doi.org/10.1056/NEJMoa2007123. (This is an important cohort study that included a large sample size, representing a geographically diverse population with a median follow up of 9.5 years and reported the effects of GI and GL by CVD and obesity status.)
Shahdadian F, Saneei P, Milajerdi A, Esmaillzadeh A. Dietary glycemic index, glycemic load, and risk of mortality from all causes and cardiovascular diseases: a systematic review and dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2019;110(4):921–37. https://doi.org/10.1093/ajcn/nqz061.
Ma XY, Liu JP, Song ZY. Glycemic load, glycemic index and risk of cardiovascular diseases: meta-analyses of prospective studies. Atherosclerosis. 2012;223(2):491–6. https://doi.org/10.1016/j.atherosclerosis.2012.05.028.
Jayedi A, Soltani S, Jenkins D, Sievenpiper J, Shab-Bidar S. Dietary glycemic index, glycemic load, and chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Crit Rev Food Sci Nutr. 2020:1–10. https://doi.org/10.1080/10408398.2020.1854168.
Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, et al. Glycemic index, glycemic load, and chronic disease risk—a meta-analysis of observational studies. Am J Clin Nutr. 2008;87(3):627–37. https://doi.org/10.1093/ajcn/87.3.627.
•• Reynolds A, Mann J, Cummings J, Winter N, Mete E, Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393(10170):434–45. https://doi.org/10.1016/S0140-6736(18)31809-9. (This is the first meta-analysis study to distinguish the predictive potential of critical markers (dietary fiber, whole grains, GI and GL) of carbohydrate quality on CVD outcomes.)
Sieri S, Brighenti F, Agnoli C, Grioni S, Masala G, Bendinelli B, et al. Dietary glycemic load and glycemic index and risk of cerebrovascular disease in the EPICOR cohort. PLoS ONE. 2013;8(5): e62625. https://doi.org/10.1371/journal.pone.0062625.
Levitan EB, Mittleman MA, Wolk A. Dietary glycemic index, dietary glycemic load and mortality among men with established cardiovascular disease. Eur J Clin Nutr. 2009;63(4):552–7. https://doi.org/10.1038/sj.ejcn.1602970.
Burger KN, Beulens JW, van der Schouw YT, Sluijs I, Spijkerman AM, Sluik D, et al. Dietary fiber, carbohydrate quality and quantity, and mortality risk of individuals with diabetes mellitus. PLoS ONE. 2012;7(8): e43127. https://doi.org/10.1371/journal.pone.0043127.
Livesey G, Taylor R, Livesey HF, Buyken AE, Jenkins DJA, Augustin LSA et al. Dietary glycemic index and load and the risk of type 2 diabetes: a systematic review and updated meta-analyses of prospective cohort studies. Nutrients. 2019;11(6). https://doi.org/10.3390/nu11061280.
Livesey G, Livesey H. Coronary heart disease and dietary carbohydrate, glycemic index, and glycemic load: dose-response meta-analyses of prospective cohort studies. Mayo Clin Proc Innov Qual Outcomes. 2019;3(1):52–69. https://doi.org/10.1016/j.mayocpiqo.2018.12.007.
Livesey G, Taylor R, Livesey HF, Buyken AE, Jenkins DJA, Augustin LSA et al. Dietary glycemic index and load and the risk of type 2 diabetes: assessment of causal relations. Nutrients. 2019;11(6). https://doi.org/10.3390/nu11061436.
Dong JY, Zhang L, Zhang YH, Qin LQ. Dietary glycaemic index and glycaemic load in relation to the risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Br J Nutr. 2011;106(11):1649–54. https://doi.org/10.1017/S000711451100540X.
Greenwood DC, Threapleton DE, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, et al. Glycemic index, glycemic load, carbohydrates, and type 2 diabetes: systematic review and dose-response meta-analysis of prospective studies. Diabetes Care. 2013;36(12):4166–71. https://doi.org/10.2337/dc13-0325.
Livesey G, Taylor R, Livesey H, Liu S. Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies. Am J Clin Nutr. 2013;97(3):584–96. https://doi.org/10.3945/ajcn.112.041467.
Bhupathiraju SN, Tobias DK, Malik VS, Pan A, Hruby A, Manson JE, et al. Glycemic index, glycemic load, and risk of type 2 diabetes: results from 3 large US cohorts and an updated meta-analysis. Am J Clin Nutr. 2014;100(1):218–32. https://doi.org/10.3945/ajcn.113.079533.
•• Hardy DS, Garvin JT, Xu H. Carbohydrate quality, glycemic index, glycemic load and cardiometabolic risks in the US, Europe and Asia: a dose-response meta-analysis. Nutr Metab Cardiovasc Dis. 2020;30(6):853–71. https://doi.org/10.1016/j.numecd.2019.12.050. (This is the most comprehensive meta-analysis study reporting the associations of GI and GL with CVD outcomes in the overall population and according to sex and obesity status separately for geographic locations.)
Zhang JY, Jiang YT, Liu YS, Chang Q, Zhao YH, Wu QJ. The association between glycemic index, glycemic load, and metabolic syndrome: a systematic review and dose-response meta-analysis of observational studies. Eur J Nutr. 2020;59(2):451–63. https://doi.org/10.1007/s00394-019-02124-z.
Askari M, Dehghani A, Abshirini M, Raeisi T, Alizadeh S. Glycemic index, but not glycemic load, is associated with an increased risk of metabolic syndrome: meta-analysis of observational studies. Int J Clin Pract. 2021:e14295. https://doi.org/10.1111/ijcp.14295.
Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002;287(18):2414–23. https://doi.org/10.1001/jama.287.18.2414.
Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69. https://doi.org/10.1001/archinternmed.2009.38.
Choi Y, Chang Y, Ryu S, Cho J, Kim MK, Ahn Y, et al. Relation of dietary glycemic index and glycemic load to coronary artery calcium in asymptomatic korean adults. Am J Cardiol. 2015;116(4):520–6. https://doi.org/10.1016/j.amjcard.2015.05.005.
Turati F, Dilis V, Rossi M, Lagiou P, Benetou V, Katsoulis M, et al. Glycemic load and coronary heart disease in a Mediterranean population: the EPIC Greek cohort study. Nutr Metab Cardiovasc Dis. 2015;25(3):336–42. https://doi.org/10.1016/j.numecd.2014.12.002.
Yuzbashian E, Asghari G, Aghayan M, Hedayati M, Zarkesh M, Mirmiran P, et al. Dietary glycemic index and dietary glycemic load is associated with apelin gene expression in visceral and subcutaneous adipose tissues of adults. Nutr Metab (Lond). 2019;16:68. https://doi.org/10.1186/s12986-019-0389-9.
Cai X, Wang C, Wang S, Cao G, Jin C, Yu J, et al. Carbohydrate intake, glycemic index, glycemic load, and stroke: a meta-analysis of prospective cohort studies. Asia Pac J Public Health. 2015;27(5):486–96. https://doi.org/10.1177/1010539514566742.
Rossi M, Turati F, Lagiou P, Trichopoulos D, La Vecchia C, Trichopoulou A. Relation of dietary glycemic load with ischemic and hemorrhagic stroke: a cohort study in Greece and a meta-analysis. Eur J Nutr. 2015;54(2):215–22. https://doi.org/10.1007/s00394-014-0702-3.
Levitan EB, Mittleman MA, Hakansson N, Wolk A. Dietary glycemic index, dietary glycemic load, and cardiovascular disease in middle-aged and older Swedish men. Am J Clin Nutr. 2007;85(6):1521–6. https://doi.org/10.1093/ajcn/85.6.1521.
Levitan EB, Mittleman MA, Wolk A. Dietary glycaemic index, dietary glycaemic load and incidence of myocardial infarction in women. Br J Nutr. 2010;103(7):1049–55. https://doi.org/10.1017/S0007114509992674.
Levitan EB, Mittleman MA, Wolk A. Dietary glycemic index, dietary glycemic load, and incidence of heart failure events: a prospective study of middle-aged and elderly women. J Am Coll Nutr. 2010;29(1):65–71. https://doi.org/10.1080/07315724.2010.10719818.
Brand-Miller JC, Petocz P, Colagiuri S. Meta-analysis of low-glycemic index diets in the management of diabetes: response to Franz. Diabetes Care. 2003;26(12):3363–4; author reply 4–5. https://doi.org/10.2337/diacare.26.12.3363.
Thomas D, Elliott EJ. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database Syst Rev. 2009(1):CD006296. https://doi.org/10.1002/14651858.CD006296.pub2.
Wang Q, Xia W, Zhao Z, Zhang H. Effects comparison between low glycemic index diets and high glycemic index diets on HbA1c and fructosamine for patients with diabetes: A systematic review and meta-analysis. Prim Care Diabetes. 2015;9(5):362–9. https://doi.org/10.1016/j.pcd.2014.10.008.
• Zafar MI, Mills KE, Zheng J, Regmi A, Hu SQ, Gou L, et al. Low-glycemic index diets as an intervention for diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2019;110(4):891–902. https://doi.org/10.1093/ajcn/nqz149. (This comprehensive meta-analysis investigated the effects of variety of dietary interventions lowering GI on cardiometabolic risk factors and reported effect sizes according to diet type, obesity, diabetes, and other subpopulation status.)
Ojo O, Ojo OO, Adebowale F, Wang XH. The effect of dietary glycaemic index on glycaemia in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2018;10(3). https://doi.org/10.3390/nu10030373.
•• Chiavaroli L, Lee D, Ahmed A, Cheung A, Khan TA, Blanco S, et al. Effect of low glycaemic index or load dietary patterns on glycaemic control and cardiometabolic risk factors in diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ. 2021;374: n1651. https://doi.org/10.1136/bmj.n1651.ThisisthemostrecentstudyevaluatingtheeffectoflowGI/GLoncomprehensivecardiometabolicfactorsinrandomizedcontrolledtrials. (This study generates evidence for small but favorable benefits of low GI/GL dietary interventions on cardiometabolic risk factors.)
Zafar MI, Mills KE, Zheng J, Peng MM, Ye X, Chen LL. Low glycaemic index diets as an intervention for obesity: a systematic review and meta-analysis. Obes Rev. 2019;20(2):290–315. https://doi.org/10.1111/obr.12791.
Clar C, Al-Khudairy L, Loveman E, Kelly SA, Hartley L, Flowers N et al. Low glycaemic index diets for the prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;7:CD004467. https://doi.org/10.1002/14651858.CD004467.pub3.
Livesey G, Taylor R, Hulshof T, Howlett J. Glycemic response and health—a systematic review and meta-analysis: relations between dietary glycemic properties and health outcomes. Am J Clin Nutr. 2008;87(1):258S-S268. https://doi.org/10.1093/ajcn/87.1.258S.
Fleming P, Godwin M. Low-glycaemic index diets in the management of blood lipids: a systematic review and meta-analysis. Fam Pract. 2013;30(5):485–91. https://doi.org/10.1093/fampra/cmt029.
Goff LM, Cowland DE, Hooper L, Frost GS. Low glycaemic index diets and blood lipids: a systematic review and meta-analysis of randomised controlled trials. Nutr Metab Cardiovasc Dis. 2013;23(1):1–10. https://doi.org/10.1016/j.numecd.2012.06.002.
Toh DWK, Koh ES, Kim JE. Lowering breakfast glycemic index and glycemic load attenuates postprandial glycemic response: a systematically searched meta-analysis of randomized controlled trials. Nutrition. 2020;71: 110634. https://doi.org/10.1016/j.nut.2019.110634.
Schwingshackl L, Hoffmann G. Long-term effects of low glycemic index/load vs. high glycemic index/load diets on parameters of obesity and obesity-associated risks: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2013;23(8):699–706.https://doi.org/10.1016/j.numecd.2013.04.008.
Thomas DE, Elliott EJ, Baur L. Low glycaemic index or low glycaemic load diets for overweight and obesity. Cochrane Database Syst Rev. 2007(3):CD005105. https://doi.org/10.1002/14651858.CD005105.pub2.
Schwingshackl L, Hobl LP, Hoffmann G. Effects of low glycaemic index/low glycaemic load vs. high glycaemic index/high glycaemic load diets on overweight/obesity and associated risk factors in children and adolescents: a systematic review and meta-analysis. Nutr J. 2015;14:87. https://doi.org/10.1186/s12937-015-0077-1.
Wei J, Heng W, Gao J. Effects of low glycemic index diets on gestational diabetes mellitus: a meta-analysis of randomized controlled clinical trials. Medicine (Baltimore). 2016;95(22): e3792. https://doi.org/10.1097/MD.0000000000003792.
Wan CS, Nankervis A, Teede H, Aroni R. Dietary intervention strategies for ethnic Chinese women with gestational diabetes mellitus: a systematic review and meta-analysis. Nutr Diet. 2019;76(2):211–32. https://doi.org/10.1111/1747-0080.12524.
Xu J, Ye S. Influence of low-glycemic index diet for gestational diabetes: a meta-analysis of randomized controlled trials. J Matern Fetal Neonatal Med. 2020;33(4):687–92. https://doi.org/10.1080/14767058.2018.1497595.
Evans CE, Greenwood DC, Threapleton DE, Gale CP, Cleghorn CL, Burley VJ. Glycemic index, glycemic load, and blood pressure: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2017;105(5):1176–90. https://doi.org/10.3945/ajcn.116.143685.
Yu D, Zhang X, Shu XO, Cai H, Li H, Ding D, et al. Dietary glycemic index, glycemic load, and refined carbohydrates are associated with risk of stroke: a prospective cohort study in urban Chinese women. Am J Clin Nutr. 2016;104(5):1345–51. https://doi.org/10.3945/ajcn.115.129379.
Barclay AW, Brand-Miller JC, Wolever TM. Glycemic index, glycemic load, and glycemic response are not the same. Diabetes Care. 2005;28(7):1839–40. https://doi.org/10.2337/diacare.28.7.1839.
He F, Chen C, Li F, Qi Y, Lin X, Liang P, et al. An optimal glycemic load range is better for reducing obesity and diabetes risk among middle-aged and elderly adults. Nutr Metab (Lond). 2021;18(1):31. https://doi.org/10.1186/s12986-020-00504-5.
Knopp RH, Paramsothy P, Retzlaff BM, Fish B, Walden C, Dowdy A, et al. Sex differences in lipoprotein metabolism and dietary response: basis in hormonal differences and implications for cardiovascular disease. Curr Cardiol Rep. 2006;8(6):452–9. https://doi.org/10.1007/s11886-006-0104-0.
Austin MA, Hokanson JE, Edwards KL. Hypertriglyceridemia as a cardiovascular risk factor. Am J Cardiol. 1998;81(4A):7B-12B. https://doi.org/10.1016/s0002-9149(98)00031-9.
Tavani A, Bosetti C, Negri E, Augustin LS, Jenkins DJ, La Vecchia C. Carbohydrates, dietary glycaemic load and glycaemic index, and risk of acute myocardial infarction. Heart. 2003;89(7):722–6. https://doi.org/10.1136/heart.89.7.722.
Dubey P, Reddy SY, Alvarado L, Manuel SL, Dwivedi AK. Prevalence of at-risk hyperandrogenism by age and race/ethnicity among females in the United States using NHANES III. Eur J Obstet Gynecol Reprod Biol. 2021;260:189–97. https://doi.org/10.1016/j.ejogrb.2021.03.033.
Dubey P, Thakur V, Chattopadhyay M. Role of minerals and trace elements in diabetes and insulin resistance. Nutrients. 2020;12(6). https://doi.org/10.3390/nu12061864.
Pallavi Dubey SR, Sarah Boyd, Christina Bracamontes, Sheralyn Sanchez, Munmun Chattopadhyay, Alok Dwivedi. Effect of nutritional supplementation on oxidative stress and hormonal and lipid profiles in PCOS-affected females. Nutrients. 2021;13:2938. https://doi.org/10.3390/nu13092938.
Kazemi M, Hadi A, Pierson RA, Lujan ME, Zello GA, Chilibeck PD. Effects of dietary glycemic index and glycemic load on cardiometabolic and reproductive profiles in women with polycystic ovary syndrome: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2021;12(1):161–78. https://doi.org/10.1093/advances/nmaa092.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alok Kumar Dwivedi, Pallavi Dubey, Sireesha Y. Reddy, and Deborah J. Clegg declare that they do not have any conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Dwivedi, A.K., Dubey, P., Reddy, S.Y. et al. Associations of Glycemic Index and Glycemic Load with Cardiovascular Disease: Updated Evidence from Meta-analysis and Cohort Studies. Curr Cardiol Rep 24, 141–161 (2022). https://doi.org/10.1007/s11886-022-01635-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01635-2