Abstract
Objectives
The aim of the present study was to investigate whether the following four markers: vitamin B12, selenium, vitamin D, and parvalbumin may be used as compliance markers for fish intake.
Methods
Blood samples from a randomized cross-over herring intervention study (n = 32) were analysed by HPLC and immunochemistry. The criteria were that plasma or serum concentrations of candidate compliance markers after the herring diet should increase significantly compared to starting concentrations. In addition, the reference meat diet should not yield an increase in plasma concentration of the candidate marker.
Results
Vitamin B12 and selenium met the set criteria for indicating a correlation between the marker and fish intake with significant increases in serum concentrations at 8.9 % (p = 0.008) and 4.6 % (p = 0.02), respectively, after a 6-week herring intervention (5 meals a week). Parvalbumin and 25-hydroxy vitamin D3 levels did not increase significantly after the herring interventions.
Conclusions
Vitamin B12 may be suitable as a compliance marker for fish intake. Although selenium also met the criteria, the change in selenium serum concentrations was small compared to the change in vitamin B12 levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eating habits and choice of foods are important factors for human health and may also predict the development of disease. There are several diet-related diseases in the human population such as deficiency syndromes, obesity, diabetes, and cardiovascular disorders. Including fish in the diet has been shown to decrease several risk factors for developing, e.g., coronary heart diseases [1–3]. Fish is therefore recommended as a part of a healthy diet.
Long-term diet intervention and epidemiological studies are important tools to evaluate the effects on disease risk in relation to the composition of diets both in terms of specific effects of individual components and also the overall effects on health and disease. Unfortunately, it is difficult to evaluate intake of specific food items in epidemiological studies and to control compliance in interventions. Various dietary assessment tools are used such as food frequency questionnaires and 24-h recalls. These methods are limited since there is a bias in self-reporting dietary intake. Thus, to be able to objectively estimate food intake of compounds or food groups, we need efficient compliance markers that can easily be measured. To be suitable for medium- and long-term interventions, these markers need to be relatively long-lived in the circulation, before they are incorporated or scavenged by specific tissues. Another criterion for an ideal compliance marker is that it should not be affected by potential conditions of the subject such as allergies and other inflammatory diseases. Also, it should be a constituent of the investigated food and not an indirect measure of a physiological effect. In addition, the definition and more general criteria for a compliance marker should be formulated. The lack of consensus in the evaluation of used markers for food intake and effects, in the nutritional sciences, was recently reported [4] and should be addressed.
Polyunsaturated fatty acids (PUFAs) as (bio) markers for fish intake
Fatty fish such as salmon and herring are rich in the long-chain n-3 polyunsaturated fatty acids (LC n-3 PUFA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Endogenous production of EPA and DHA is considered to be limited, which is an advantage when used as a biomarker for food intake. The content of these LC n-3 PUFAs in plasma/serum phospholipids has therefore been extensively used to reflect seafood intake including fish [5, 6]. Also, fatty acids have a long half-life in the circulation, and changes can be measured days after the intervention. In healthy individuals, seafood generally causes serum DHA and EPA levels to increase. However, inflammatory states may change this pattern since fatty acids may be consumed during the production of eicosanoid-derived mediators such as prostaglandins (PGE2). The consumption of EPA and DHA has been observed during allergic inflammation in a mouse model [7] as well as in the diabetic heart, in a diabetic (type II) rat model [8]. Our laboratory has also found suggestive evidence that this occurs in humans, since women with pronounced allergy had lower proportions of n-3 fatty acids in breast milk and serum compared to non-allergic women, despite higher fish intake [9]. Several other conditions have been associated with low tissue levels of PUFAs, such as Alzheimer’s disease [10] and cystic fibrosis [11]. For this reason, LC n-3 PUFAs alone may not always be the optimal choice of biomarker for fish intake. In addition, lean fish species are low in total LC n-3 PUFA levels, although LC n-3 PUFA has been found to be a marker for habitual lean fish intake, based on dietary recalls and blood sampling [12].
Proposed (bio)markers
Trimethylamine-N-oxide (TMAO) has been proposed as a biomarker for fish intake [13]. TMAO urinary levels are also increased by the ingestion of meats [14]. Another study indicated that urinary TMAO correlated with nitrogen excretion, which is a measure of general protein consumption [15]. Therefore, TMAO does not seem to be specific for fish, and we do not consider it a suitable candidate. An emerging trend is to use heavy metals as markers for fish intake. Arsenic (Ar) and methylated mercury (meHg) have been suggested as useful biomarkers for fish intake [16]. It is important to keep in mind that heavy metals are not desirable elements in fish and therefore primarily serve as markers for chemical exposure instead of reflecting the functional composition of fish. Further, the heavy metal content in fish varies largely with geographical location of the catch, which makes it unreliable.
Vitamin B12, selenium, vitamin D, and parvalbumin as compliance markers
Vitamin B12 (cobalamin) is an essential water-soluble vitamin that cannot be produced in the human body but which have important functions in blood, brain and nervous system [17]. Healthy individuals readily absorb vitamin B12, which remains in the blood stream for about a week [18]. In conditions related to disorders of the gastrointestinal tract, such as pernicious anaemia, vitamin B12 is poorly absorbed [19]. In these cases, vitamin B12 would not serve as a marker for fish intake.
Seafood is rich in vitamin B12, especially clams and oysters, but several fish species (mackerel, herring and salmon) are also good sources of the vitamin. Meat (beef), cheese and eggs also provide humans with vitamin B12 although to a lesser extent than most fish species. One exception is liver (from mammal origin), which is higher in vitamin B12 than fish, but liver products are normally not a major part of the human diet. Using vitamin B12 as a compliance marker would be advantageous since it is routinely analysed in many laboratories. It is also associated with about half the cost compared to the analyses of PUFAs.
Selenium (Se) is an important trace element in humans and is essential for, e.g., enzymatic activity in the cellular glutathione system, which reduces oxidative stress. Fish and other seafoods are relatively rich in Se and Se status may therefore be useful as a marker for seafood intake [20]. Oily fish species contain high levels of vitamin D compared to other foods, e.g., one serving of herring contains about 200–300 % of the daily requirement of vitamin D. There are great variations in vitamin D levels within different fish species but also within the same species due to season and geographical location. Further, sun exposure is the most reliable source for increasing vitamin D status in humans. All these parameters make it difficult to compare vitamin D levels and biological effects between studies. Some of the issues may be overcome by correcting the data for these variations. Several fish species such as cod, mackerel, salmon and herring are rich in the muscle protein parvalbumin. Parvalbumins are small soluble proteins (12 kD) highly resistant to heat and gastrointestinal digestion. The main function of parvalbumin in fish is involving the regulation of calcium (Ca2+) levels in fast-contracting muscles. Fish parvalbumins are present in several isoforms of two major types, α and β. Individuals allergic to fish are in most cases reacting towards fish parvalbumin β, but generally not to parvalbumin α. Fish allergists are non-reactive towards other parvalbumins (human, beef and chicken), indicating that these parvalbumins are specific to fish. Therefore, fish parvalbumin was evaluated as a potential compliance marker for fish intake.
The aim of the present study was to find a potential marker for fish intake, which can be used to confirm compliance in fish-based intervention studies. We wished to focus on four compounds endogenous to fish. These were vitamin B12, selenium (Se), vitamin D and the fish muscle protein parvalbumin. We have used material (serum and plasma) from a randomized, cross-over intervention study done in overweight men conducted in Sweden (2005). The set criteria for the biomarker to be an estimate for fish intake were that plasma end levels after the herring diet should increase compared to starting levels. Also, the reference meat diet should not yield a significant increase in plasma levels of the candidate compliance marker in order to be an estimate for fish intake.
Methods
Subjects
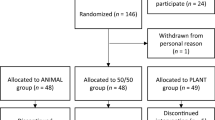
Forty Swedish overweight (BMI >25) men (mean age 48 years, range 35–60) participated in the study. A complete list of subject baseline characteristics was previously described [21]. The subjects were non-smokers, low-consumers of alcohol (<10 units/week), healthy and willing to be on a herring diet for 6 weeks. None of the subjects were on lipid lowering or anti-inflammatory drugs. In addition, their normal diets did not contain high amount of fish or foods containing high levels of long-chain n-3 PUFAs. The subjects have signed a written informed consent before the start of the study.
Study design
The intervention was a randomized, cross-over study (2 × 6 weeks; April–June and September–November). Half of the subjects were having herring meals for 6 weeks, followed by a 12-week washout period before the next intervention period with chicken/lean pork meals for 6 weeks. The other half started with the meat diet and ended the intervention with the herring diet. The subjects were provided with 10 meals every second week and were instructed to have one of these meals at lunch or dinner 5 days/week. Two weeks before the study, the subjects were directed to follow their normal diet, exclude any functional foods, only have two fish meals a week (except from the herring meals provided), and to not consume more than 2 alcohol units/week. The first 6-week intervention took place in the spring of 2005 and the second in the autumn 2005. Fasting blood samples were collected before and after each intervention.
Diet intervention
The intervention meals have been described in detail previously [22]. They were complete meals containing 28E % proteins, 33E % fat and 39E % carbohydrates (about 2,100 kJ/day), and all ingredients were similar between the dishes in the two interventions periods except for the fish/meat. They were either prepared from 150 g of raw herring or chicken, or 130 g of browned pork fillets. The chicken/pork reference meals were chosen to provide as neutral animal protein source as possible. The reference meals were supplemented with a fat mixture to compensate for the lower fat content compared to the herring meals, but were designed to avoid a higher intake of saturated fatty acids than the herring meals. The supplemented fat contained 30 % rapeseed oil, 30 % sunflower oil and 40 % margarine. The herring diet content of EPA and DHA was 1.2 g/day on average, while the reference diet provided insignificant amounts (0.04 g/day). Compliance was followed by 24-h dietary recalls and complemented with analyses of fatty acid concentrations in whole blood [21].
Food preparation
The preparation of intervention meals have been described in detail previously [22]. In brief, fresh fillets of herring were vacuum-packed and frozen with a blast freezer at one time point, since herring content varies during the season, until they were prepared for the meals. The intervention meals were prepared on four occasions at Micvac AB (Mölndal, Sweden). The dishes were cooked, pasteurized and vacuum-packed as complete meals (approx. 430 g/portion). The subjects were instructed to keep the packages at 4–8 °C, until the meals were microwave-heated and consumed.
Vitamin B12 analyses
Vitamin B12 was analysed by an immunochemical method using a competitive electrochemiluminescence technique (ECLIA), which was conducted by an accredited lab (Central lab, Sahlgrenska University hospital, Gothenburg, Sweden). For the analyses, a Cobas 8000 instrument (Roche Diagnostics, Scandinavia) and Elecsys vitamin B12 reagent kit (Roche Diagnostics, Scandinavia; no 11820753322) was used.
Selenium analyses
Selenium was analysed by atomic absorption spectrophotometry using a Solaar AA M6 Furnace (Thermo Electron Corporation), with Zeeman background correction. Palladium was used as matrix modifier. These analyses were also conducted by an accredited lab (Central lab, Sahlgrenska University hospital, Gothenburg, Sweden).
Analysis of 25-hydroxy vitamin D3
Serum samples (500 μl) were prepared for HPLC analyses by adding 500 μl methanol-2-propanol and vortexed for 30 s. Thereafter, hexane (2 ml) was added, and the samples were rocked for 20 min. Samples were centrifuged for 2 min (3,000 rpm) before injection (20 μl). A Dionex system including a p580 pump and a UVD 340 U detector was employed (Sunnyvale, CA, USA). The samples were separated using a Phenomenex Luna C18(2): 3 μm, 100 Å and 250 × 4.6 mm column. The flow rate was 0.8 ml/min. The mobile phase was methanol (96 %) in H2O. The peaks were analysed with Chromeleon software version 6.80 (Dionex).
ELISA measurements of parvalbumin α and β in plasma
Total α and β parvalbumin levels in plasma collected 24–72 h after the interventions were evaluated using a primary monoclonal antibody (m-anti-frogPARV-19; P088, Sigma-Aldrich, St. Louis, MO, USA) specific to both parvalbumin α and β of fish origin. PARV-19 is also reactive towards parvalbumin of several other species such as rabbit and rat, but not porcine and gallus species. As secondary antibody, a goat-anti-mouse IgG conjugated to HRP (A4416; Sigma-Aldrich) was used. The procedure was as following: A 96-well plate was coated with citrate plasma samples in duplicates (20 μl) for 2 h at 37 °C. The plate was washed in PBS-Tween 20 (0.05 %) once and then blocked with blocking and coating stabilizer (Sigma-Aldrich) for 1 h. The plate was incubated with primary antibody (dilution 1:1,000) overnight in 4 °C. The following day, the plate was washed in PBS-T (3×) before the addition of secondary antibody (dilution 1:4,000). Both antibodies were diluted in PBS-T with BSA 1 % (w/v). The secondary antibody was incubated at 25 °C for 3 h. After washing (×3 in PBS-T), the absorbance was detected by incubating the samples with OPD in phosphate-citrate sodium perborate (0.05 M) buffer freshly mixed with hydrogen peroxide (30 %; 4 μl/10 ml). After 30 min, the absorbance at 450 nm was measured with a plate reader (Tecan Saphire II, Gmbh, Austria).
Statistics
Vitamin B12, selenium and parvalbumin levels are shown as mean ± SEM (n = 32). 25-hydroxy vitamin D levels are mean ± SEM (n = 21). Values were compared by Student’s two-tailed paired t test (Microsoft Excel 2011), and changes were considered significant at p < 0.05.
Results
Increased serum concentrations of vitamin B12 and selenium indicate herring intake
Subject serum concentrations of vitamin B12 were significantly increased after the herring diets compared to initial concentrations at the start of the intervention (8.9 %; n = 32; p = 0.008, Table 1). In addition, vitamin B12 was also significantly higher after the herring diet compared to the meat reference diet (9.8 %; n = 32, P = 0.0005). In fact, subject vitamin B12 levels were lower after the meat diet. This is likely to be a consequence of that the subjects on the meat diet were not allowed to have fish more than once a week during the meat intervention and that the meat intervention meals containing chicken and pork were not particularly high in vitamin B12. Vitamin B12 concentrations also reflected the levels of fatty acids DHA and EPA in subject whole blood in the used cohort (Table 1), which had normal levels of circulation inflammatory markers [21]. Selenium concentrations followed the same trends as vitamin B12 in subject whole blood, and thus, they increased with herring intake compared to starting levels (4.6 %; n = 32, p = 0.002) and increased after herring intervention compared to meat intervention (6.7 %; P = 0,0004). However, the changes were smaller compared to those for vitamin B12, which suggest that vitamin B12 has a greater potential as a compliance marker for fish intake than selenium.
25-Hydroxy vitamin D3 is insufficient as a marker for fish consumption
25-Hydroxy vitamin D3 serum concentrations did not change significantly from the start of the herring intervention through the end (n = 21; p = 0.34; Table 1). There was, however, a difference between the levels after herring diets and meat diets (15.2 %; n = 21, p = 0.001). However, sorting the data after the sampling events (data not shown), it was revealed that after finishing the second intervention period (November 2005), 25-hydroxy vitamin D3 levels decreased independent of herring or meat diet, and after the completion of the first intervention (June 2005), the trends were the opposite, independent of herring or meat diet, suggesting a seasonal influence that was greater than the dietary input from herring. For this reason, 25-hydroxy vitamin D3 is not sufficient as a marker for fish intake.
Parvalbumin levels in plasma did not change after the herring intervention periods
Total parvalbumin α and β levels in plasma did not increase after the herring diet (data not shown), which was observed by comparing relative differences in the plasma levels at the start and end of the diet intervention (0.2 %, p = 0.92, n = 32, Fig. 1). There was no significant difference between the herring and reference meat diets (1 %, p = 0.7, n = 32). However, analysing data for the two individual intervention periods separately, it was revealed that plasma parvalbumin levels were significantly increased, comparing before with after herring diet, when the herring diet was consumed between September and November (8 %, P = 0.01, n = 16, Fig. 2a). The opposite trend was observed when having the herring diet between April and June (6.2 %, p = 0.14, n = 16, Fig. 2b). These data suggest an inverse relationship between 25-hydroxy vitamin D3 and parvalbumin serum levels. However, this trend needs to be verified in a cohort with a greater number of subjects.
Seasonal changes in fish parvalbumin α and β levels in subject plasma (n = 16). a The intervention period occurred in the autumn (September–November). A significant increase in plasma parvalbumin levels after the herring diet was observed. b The second intervention period was done in the spring (April–June). No significant changes were observed
Discussion
We investigated the potential of four markers to be used as compliance markers for fish intake. Vitamin B12 met the criteria, and due to its higher abundance in fish than in meats, vitamin B12 may be used as compliance marker for fish intake. Further evaluation is needed.
Vitamin B12 concentration in serum followed the same pattern as LC n-3 PUFA levels (Table 1), which increased with the herring intake. The changes in EPA and DHA levels after the herring diet were greater compared to the changes in vitamin B12 levels, which show that EPA and DHA were sufficient as markers for fish intake in this study. However, one of the advantages of using vitamin B12 as a serum marker for fish intake is that fish in general is high in vitamin B12, not just oily fish, such as herring and salmon. Herring contains 312 % of daily values (DV) of vitamin B12 per 100 g, salmon 302 % and mackerel 317 % [23]. Lean fish such as cod contains 167 % of DV and is therefore also a good source of vitamin B12. Terrestrial animal products such as eggs provide 33 %, cheddar cheese 54 % and beef at the highest may contain 103 % of DV for vitamin B12 per 100 g. The higher vitamin B12 content in seafood compared to meats also strengthens the role for this vitamin as a compliance marker for fish intake. One limitation of using B12 as a marker for fish intake in dietary interventions is that older subjects (>60 years) do not absorb vitamin B12 from foods as readily as younger subjects [24]. This difference has to be considered when choosing the use of compliance markers in a cohort.
In the present study, serum selenium concentrations were significantly increased after the herring diet. The increase was small (4.6 %) and considering that the level of selenium in fish is much lower (2–4 times) than, e.g., in pork and beef, selenium is probably not optimal as a fish intake estimate. The same conclusion must be drawn for vitamin D, due to its seasonal variations. In the 2005 intervention study, the sampling was done on four occasions: before and after each of the two intervention periods. The first period started in late April/beginning of May and was completed in the middle of June. The second period started in the middle of September and ended in the end of October/beginning of November. The subjects all lived in Gothenburg situated at latitude 57°42′ N. Studies on seasonal variation in vitamin D have shown that the population in Nordic European countries have the lowest serum 25-hydroxy vitamin D3 in the late winter (February/March) and the highest in late summer (September) [25]. This supports the data in the present study, in which vitamin D levels decreased between September and November and increased between April and June, independent of diet. Also, the baseline 25-hydroxy vitamin D3 levels of the cohort were low, with values (60–65 nmol/l in average) slightly under optimal values (75–200 nmol/l). The concentrations did not improve after the herring diet, suggesting that sun exposure is more important. The conclusion is that vitamin D is insufficient as a marker for fish intake. Plasma levels of the fish muscle protein parvalbumin did not increase after the two herring intervention periods, despite the high levels of parvalbumin in herring (>200 mg/100 g [26]). The inverse relationship between 25-hydroxy vitamin D3 and parvalbumin levels may be related to these compounds involvement in the regulation of Ca2+ metabolism. During high endurance exercise, such as swimming, calcium intestinal absorption (in the rat) is increased [27]. The increased Ca2+ absorption was associated with up-regulation of both the nuclear receptor for 1, 25-hydroxy vitamin D3 and parvalbumin genes. This link between vitamin D and parvalbumin regulatory functions may imply that parvalbumin is also susceptible to seasonal fluctuations.
Conclusions
In conclusion, this investigation shows that vitamin B12 is a promising candidate as a compliance marker for fish intake. There are at least three reasons for this conclusion: (1) vitamin B12 is far higher in most seafood compared to meats, (2) the circulatory retention of vitamin B12 is sufficient to measure the vitamin days after the intervention and (3) vitamin B12 plasma levels are unaffected by external factors such as sun exposure. Further studies are needed to assess the validity, reproducibility and sensitivity of the use of vitamin B12 as a compliance marker for fish intake, e.g., vitamin B12 serum levels must respond in a dose-dependent manner, the time frame for serum peak concentrations must be determined, and the extent of utilization of serum vitamin B12 in individuals with different vitamin B12 status must be estimated since the measured serum levels reflect both the intake and the tissue need of the nutrient.
References
Undeland I, Ellegård L, Sandberg A-S (2004) Fish and cardiovascular health. Scand J Nutr 48:119–130
He K, Song Y, Daviglus ML, Liu K, Van Horn L, Dyer AR, Greenland P (2004) Accumulated evidence on fish consumption and coronary heart disease mortality: a meta-analysis of cohort studies. Circulation 109(22):2705–2711
Kris-Etherton PM, Harris WS, Appel LJ, for the Nutrition C (2002) Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation 106(21):2747–2757
Vries J, Antoine J-M, Burzykowski T, Chiodini A, Gibney M, Kuhnle G, Méheust A, Pijls L, Rowland I (2013) Markers for nutrition studies: review of criteria for the evaluation of markers. Eur J Nutr:1–15. doi:10.1007/s00394-013-0553-3
Kobayashi M, Sasaki S, Kawabata T, Hasegawa K, Akabane M, Tsugane S (2001) Single measurement of serum phospholipid fatty acid as a biomarker of specific fatty acid intake in middle-aged Japanese men. Eur J Clin Nutr 55(8):643–650
Hjartåker A, Lund E, Bjerve KS (1997) Serum phospholipid fatty acid composition and habitual intake of marine foods registered by a semi-quantitative food frequency questionnaire. Eur J Clin Nutr 51(11):736–742
Johansson S, Lönnqvist A, Östman S, Sandberg AS, Wold AE (2010) Long-chain polyunsaturated fatty acids are consumed during allergic inflammation and affect T helper type 1 (Th1)- and Th2-mediated hypersensitivity differently. Clin Exp Immunol 160(3):411–419. doi:10.1111/j.1365-2249.2010.04107.x
Hou L, Lian K, Yao M, Shi Y, Lu X, Fang L, He T, Jiang L (2012) Reduction of n-3 PUFAs, specifically DHA and EPA, and enhancement of peroxisomal beta-oxidation in type 2 diabetic rat heart. Cardiovasc Diabetol 11(126):1–8
Johansson S, Wold AE, Sandberg AS (2011) Low breast milk levels of long-chain n-3 fatty acids in allergic women, despite frequent fish intake. Clin Exp Allergy 41(4):505–515. doi:10.1111/j.1365-2222.2010.03678.x
Kyle DJ, Schaefer E, Patton G, Beiser A (1999) Low serum docosahexaenoic acid is a significant risk factor for alzheimer’s dementia. Lipids 34(1):S245–S245. doi:10.1007/bf02562306
Aldamiz-Echevarria L, Prieto JA, Andrade F, Elorz J, Sojo A, Lage S, Sanjurjo P, Vazquez C, Rodriguez-Soriano J (2009) Persistence of essential fatty acid deficiency in cystic fibrosis despite nutritional therapy. Pediatr Res 66(5):585–589
Amiano P, Dorronsoro M, de Renobales M, Ruiz de Gordoa J, Irigoen I (2001) Very-long-chain omega-3 fatty acids as markers for habitual fish intake in a population consuming mainly lean fish: the EPIC cohort of Gipuzkoa. Eur J Clin Nutr 55:827–832
Lloyd AJ, Favé G, Beckmann M, Lin W, Tailliart K, Xie L, Mathers JC, Draper J (2011) Use of mass spectrometry fingerprinting to identify urinary metabolites after consumption of specific foods. Am J Clin Nutr 94(4):981–991
Stella C, Beckwith-Hall B, Cloarec O, Holmes E, Lindon JC, Powell J, van der Ouderaa F, Bingham S, Cross AJ, Nicholson JK (2006) Susceptibility of human metabolic phenotypes to dietary modulation. J Proteome Res 5(10):2780–2788. doi:10.1021/pr060265y
Rasmussen LG, Winning H, Savorani F, Toft H, Larsen TM, Dragsted LO, Astrup A, Engelsen SB (2012) Assessment of the effect of high or low protein diet on the human urine metabolome as measured by NMR. Nutrients 4(2):112–131
Brantsæter AL, Haugen M, Thomassen Y, Ellingsen DG, Ydersbond TA, Hagve T-A, Alexander J, Meltzer HM (2010) Exploration of biomarkers for total fish intake in pregnant Norwegian women. Pub Health Nutr 13(01):54–62
Benton D (2008) Micronutrient status, cognition and behavioral problems in childhood. Eur J Nutr 47(3):38–50. doi:10.1007/s00394-008-3004-9
Mollin DL, Pitney WR, Baker SJ, Bradley JE (1956) The plasma clearance and urinary excretion of parenterally administered 58CoB12. Blood 11:31–43
Stabler SP, Allen RH (2004) vitamin B12 deficiency as a worldwide problem. Ann Rev Nutr 24(1):299–326. doi:10.1146/annurev.nutr.24.012003.132440
Berr C, Akbaraly T, Arnaud J, Hininger I, Roussel AM, Barberger Gateau P (2009) Increased selenium intake in elderly high fish consumers may account for health benefits previously ascribed to omega-3 fatty acids. JNHA—J Nutr, Health Aging 13(1):14–18. doi:10.1007/s12603-009-0003-3
Lindqvist HM, Langkilde AM, Undeland I, Sandberg A-S (2009) Herring (Clupea harengus) intake influences lipoproteins but not inflammatory and oxidation markers in overweight men. Br J Nutr 101(03):383–390
Lindqvist H, Sandberg AS, Undeland I, Stener-Victorin E, Larsson BM, Sannaveerappa T, Lönn M, Holmäng A (2009) Influence of herring (Clupea harengus) and herring fractions on metabolic status in rats fed a high energy diet. Acta Physiol 196(3):303–314
USDA National nutrient database for standard reference
Baik HW, Russell RM (1999) Vitamin B12 deficiency in the elderly. Ann Rev Nutr 19(1):357–377. doi:10.1146/annurev.nutr.19.1.357
Viljakainen HT, Palssa A, Kärkkäinen M, Jakobsen J, Cashman KD, Mølgaard C, Lamberg-Allardt C (2006) A seasonal variation of calcitropic hormones, bone turnover and bone mineral density in early and mid-puberty girls—a cross-sectional study. Br J Nutr 96(01):124–130
Kuehn A, Scheuermann T, Hilger C, Hentges F (2010) Important variations in parvalbumin content in common fish species: a factor possibly contributing to variable allergenicity. Int Arch Allergy Immunol 153(4):359–366
Teerapornpuntakit J, Dorkkam N, Wongdee K, Krishnamra N, Charoenphandhu N (2009) Endurance swimming stimulates transepithelial calcium transport and alters the expression of genes related to calcium absorption in the intestine of rats. Am J Physiology—Endocrinol Metabol 296(4):E775–E786
Acknowledgments
The present work was funded by the Region of Västra Götaland (RUN612-0026-08 and RUN612-1102-08) and the Swedish Board of Agriculture (031-0267-08, European Fisheries Fund, Investing in sustainable fisheries). On behalf of all authors, the corresponding author states that there is no conflict of interest. The human intervention study was approved by the Ethical review board, Gothenburg. The study have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scheers, N., Lindqvist, H., Langkilde, A.M. et al. Vitamin B12 as a potential compliance marker for fish intake. Eur J Nutr 53, 1327–1333 (2014). https://doi.org/10.1007/s00394-013-0632-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-013-0632-5