Abstract
It is widely accepted that the rapid rate of growth of the brain during the last third of gestation and the early postnatal stage makes it vulnerable to an inadequate diet, although brain development continues into adulthood and micronutrient status can influence functioning beyond infancy. A deficiency of various micro-nutrients in developing countries has been found to have long-term implication for cognitive development. Vitamin A plays a critical role in visual perception and a deficiency is the leading cause of childhood blindness. A lack of iodine during a critical period in brain development is associated with reduced intellectual ability. Iron shortage is a widespread problem in the developing world but also in industrialized countries. There is evidence that iron deficiency in early life adversely effects brain development. In addition in industrialized countries a role for folate in the prevention of neural tube defects is well established and in a few individuals impaired cognitive functioning is associated with the inadequate provision of vitamin B12. The controversial suggestions that sub-clinical deficiencies of micronutrients may in industrialized societies influence anti-social behavior and intelligence are also discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In much of the population there appears to be a ready predisposition to see diet as both the cause of behavioral problems and the means of solving them. More specifically there is a widespread belief that micro-nutrient intake is deficient; it is often suggested that it results from the consumption of too many refined foods or as a consequence of farming methods in industrialized countries. A British survey found that thirty-two percent of boys up to ten years of age took supplements although it fell to fourteen percent in an older group. The comparable figures for girls were 23% when under seven years, 16% between seven and fourteen and 22% after this age. The probability of taking supplements was related to social background with the children of manual workers being less likely to consume supplements [45]. The high number of parents who purchase micro-nutrient supplements demonstrates a widespread concern that dietary deficiencies may occur.
Typically nutritional surveys find that the diet of children is a cause for only limited concern. For example the British survey of the diet of 2,600 children concluded that “average intakes of all vitamins except vitamin A were well above reference nutrient intakes” [45]. Blood analysis showed a generally good nutritional status for vitamins A, B12 and E and for magnesium, selenium and copper. There was, however, some evidence that some individuals had a poor nutritional status for iron, vitamin D, vitamin C, folic acid, riboflavin and thiamine. Biesalski et al. [23] considered the risk of micronutrient deficiencies in Europe and concluded that although a balanced diet is generally available the intake of some micronutrients is often marginal; iron, iodine, folic acid, vitamin D and vitamin B12.
Although all nutrients are required for bodily functioning, with many there is little evidence that the level of intake influences brain development and cognition. However, there is good evidence that the deficiency of some micro-nutrients influence the cognition and behavior of children. As it is beyond the capability of one paper to consider in detail the entire topic the more limited objective is to offer an introduction and overview. Where appropriate the main themes and conclusions will be summarized and attention drawn to review articles that allow those interested to go further. Attention is given particularly to those nutrients that are known to markedly influence cognitive development. As global deficiencies of vitamin A, iron, iodine and zinc have a major impact on child development in developing countries, these are considered initially. The suggestion is also considered that sub-clinical deficiencies occur in industrialized countries to the extent that cognition is disrupted, although such a suggestion is controversial.
Vitamin A
Vitamin A plays a critical role in visual perception and a deficiency is the leading cause of childhood blindness in developing countries. It has been estimated that 127 million preschool-aged children and 7 million pregnant women are vitamin A deficient [97]. Vitamin A also has a role in cell differentiation, the immune system and reproduction. Vitamin A is particularly important during periods of rapid growth, both during pregnancy and in early childhood. Globally, 4.4 million preschool children have xerophthalmia (dry eye) that is caused specifically by vitamin A deficiency. Six million mothers suffer night blindness during pregnancy. There is clear evidence that severe vitamin A deficiency can impair the visual system [82]. Vitamin A in combination with specific proteins (opsin) forms rhodopsin or visual purple. It is found in both types of photo-receptors in the retina, although in greater quantities in rods rather than cones. Under conditions of mild to moderate vitamin A deficiency dark adaptation is compromised and night-blindness results. With more severe and prolonged deficiency the eye becomes dry; small foamy spots form over the conjuntival surface, so called Bitot’s spots; ulcers may develop and total blindness result.
Vitamin A derivatives, retinoids, are involved in a complex signaling pathway that regulates gene expression. As the foetus develops, it must not be exposed to too much or too little vitamin A as either can have teratogenic consequences [74]. Pregnant women in industrialized countries should ensure that any vitamin supplements do not result in too large in the intake.
The role of vitamin A in the brain is poorly understood. The retinoids control the differentiation of neurones and a role has been suggested in memory, sleep, depression, Parkinson disease, and Alzheimer disease [84]. For example studies in the rat have found retinoid receptors in the hippocampus, an area of the brain important for memory, and that vitamin A deficiency disrupts memory [29]. We await evidence of similar effects in humans, although they are most likely to be observed in those in developing countries with a clinical deficiency. Given the typical intakes in industrialized countries it is less likely that variations in vitamin A intake within the normal range will have functional implications.
Vitamin A deficiency is also associated with an increased risk of morbidity, mortality, wasting and stunting in children. Reductions of child mortality of 19–54% following vitamin A treatment have been reported [97]. A meta-analysis of trials of vitamin A supplementation found a decrease of 23% in mortality [96]. Although in those with clinical signs of deficiency growth is delayed, when Bhandari et al. [22] considered seven double-blind trials of vitamin A supplementation they found little or no evidence that it increases the rate of growth. However, the evidence was not sufficient to comment on the benefit to children with clinical symptoms of vitamin A deficiency. Indirect benefits may result. In Sri Lanka, Mahawithanage et al. [58] examined the influence of Vitamin A supplementation on the absenteeism of school children. In a randomized controlled trial over a period of 13 months vitamin A status improved school attendance but not the anthropometric status of these children.
Pilch [71] considered vitamin A status in the US National Health and Nutrition Examination Surveys I–III and found some but not many individuals with low values, but values not so low that there was a high likelihood of functional impairment. These low values were more common in blacks than whites and those below the poverty line.
As supplementation increases the levels of serum retinol in those with baseline values less than 1.05 µmol/l, this value has been taken as an indication of potential suboptimal status. In the USA 16.7–33.9% children aged 4–8 years and 3.6–14.2% children aged 9–13 years, depending on sex and racial/ethnic group, had serum values below this level [9].
Iodine
Worldwide iodine deficiency disorders are amongst the most common nutritional problems. It is clear that in areas of low iodine provision there are serious implications for schooling and economic development. Worldwide it has been estimated that this deficiency afflicts over one billion people [34]. The only confirmed function of the trace element iodine is the role played in the synthesis of thyroid hormones. Thyroid hormones play a critical role in the metabolism of all cells and in the early growth of most organs, in particular the brain. Zimmermann and Delange [105] suggested that a low level of thyroid stimulating hormone in the newborn could indicate mild iodine deficiency in late pregnancy, an important observation as brain development in humans is particularly rapid at this stage. A deficit of iodine and/or thyroid hormone during this critical period will result in irreversible problems of brain development. A Turkish study demonstrated, using imaging techniques, that the levels of N-acetylaspartate, an amino acid found in neurones that is used as an index of neuronal density, was lower in the frontal white matter, parietal white matter and the thalamus of the brains of neonates living in a iodine deficient area. After treatment with thyroxine the levels returned to normal [1].
A lack of iodine during a critical period in brain development, the end of the first trimester and the early part of the second trimester of gestation, is associated with cretinism and a reduction in intellectual ability. However, only 5–10% of those with Iodine Deficiency Disorder will develop cretinism, even when there is a serious lack of iodine in the diet. In those who appear normal there is some evidence that psychological functioning may be compromised. In China it has been calculated that in areas with severe iodine deficiency there is a loss of 10–15 IQ points in those who are apparently normal [85]. In Papua New Guinea performance on tests of visual perception and motor control was better in children, aged 10–11 years, if their mothers had higher levels of thyroid hormones in their blood during pregnancy [70]. Similarly there are general problems of psycho-motor coordination and hearing that respond to iodine supplementation during childhood [8, 25, 96].
There are also claims that in later life impaired mental functioning may be associated with reduced levels of circulating thyroxine, although the evidence behind such claims is less substantial. The data from randomized trials that have examined the effect of iodine supplementation on cognitive performance are limited. For example the iodine supplementation of 10–12 year old moderately iodine-deficient children, in rural Albania, resulted in improved information processing, fine motor skills, and visual problem solving [104]. In a ten year prospective study 11 of 16 children born in a moderately iodine-deficient area of Italy developed attention deficit hyperactivity disorder (ADHD): in contrast not one child out of the eleven followed up in a marginally iodine-sufficient area received the diagnosis [92]. Zimmerman [103] after reviewing the topic concluded that “iodine repletion in moderately iodine-deficient school-age children has clear benefits: it improves cognitive and motor function; it also increases concentrations of insulin-like growth factor 1 and insulin-like growth factor-binding protein 3, and improves somatic growth.”
In the United States the average level of bodily iodine is well within the normal range established by the World Health Organization. However, as there are some in the population with levels below the acceptable range the American Thyroid Association has recommended iodine supplements during pregnancy and lactation, and that all prenatal vitamin/mineral preparations should contain iodine [13]. Zimmermann [103] reported that the iodine requirement increases during pregnancy and suggested that the recommended intake should be in the range of 220–250 µg/day. The World Health Organization recommends that the urinary iodine concentration should be greater than 250 µg/l and but less than 500 µg/l, a range that suggests that many pregnant women in Western Europe have inadequate intakes. After reviewing the literature on iodine status in Europe, Zimmermann and Delange [105] found that although “most women in Europe are iodine deficient during pregnancy, less than 50% receive supplementation with iodine” and concluded that in “most European countries, pregnant women and women planning a pregnancy should receive an iodine-containing supplement (approximately 150 µg/day)”. The long-term implications for the child of a mild iodine deficiency during pregnancy are unclear as there are no long-term studies [103].
Iron
In both industrialized and developing countries it is well established that both marginal and deficient intakes of iron are common. The deficiency disease, iron-deficit anaemia, is associated with general tiredness, lowered mood and an inability to concentrate and remember. Although iron shortage is a particular problem in the developing world, it is also a widespread problem in industrialized countries. It has been estimated that about 20% of the world’s population is deficient in iron. For example in Britain in all children, except older boys, the mean intakes of iron “were well below the RDA” [37]. Another British survey found that three percent of boys and eight percent of girls aged four to six years had blood haemoglobin levels below 11.0 g/dl, the WHO limit defining anaemia for children aged 6 months to 6 years. Thirteen percent of older boys and 27% of older girls had low serum ferritin levels that may indicate low iron stores [45]. As iron deficiency occurs commonly in the USA Bogen et al. [26] studied children, aged 9–30 months old, who attended inner-city clinics. Eight percent were anaemic with another 7% iron deficit but not anaemic. Schneider et al. [79] looked at children participating in the Special Supplemental Nutrition Program in California. Anaemia was found in 11.1% of those between 1 and 2 years.
There is increasing evidence that low iron status adversely influences psychological functioning that is believed to result from decreased activity of iron-containing enzymes in the brain, in addition to reduced haemoglobin synthesis [67, 73]. When the body is short of iron it is preferentially directed away from the brain to make red blood cells. It is therefore possible that the levels of iron in an individual’s brain will become depleted when the intake is marginal, although the individual may not be as yet anaemic.
The extensive literature on the influence of iron deficiency has been reviewed on many occasions. Iannotti et al. [50] found in 26 controlled trials of the impact of children living in developing countries that reduced cognitive and motor development were observed in iron-deficient or anaemic children, particularly if it was of a longer-duration. Sachdev et al. [76] similarly reviewed the literature and concluded that “iron supplementation improves mental development score modestly: in children over seven years the effect size was 0.41 (95% CI 0.20–0.62) when IQ scores were examined.” Lozoff [57] concluded that “there is compelling evidence that 6- to 24-month-old infants with iron-deficiency anemia are at risk for poorer cognitive, motor, social-emotional, and neurophysiologic development in the short- and long-term.” In addition the age at which iron deficiency occurs is important Beard and Connor [12] concluded that there is evidence that in early life iron deficiency results in delayed development and if it occurs early in life the problems persist even if subsequently the intake of iron is adequate. In contrast the consequences of iron deficiency in preschool and older children appear to be reversed by a subsequently adequate supply.
It has been shown on a number of occasions that iron deficiency changes the myelination of neurones and dopamine metabolism, changes that persist when iron was deficient in the neonatal period. Based on animal studies Lozoff [57] concluded that a deficiency of iron during the spurt in brain growth results in alterations in metabolism, neurotransmission and myelination. For example pregnant rats were fed a diet that either contained iron or was deficient [99], although subsequently the pups were fed an iron-sufficient diet. There was less myelination of subcortical white matter and the fimbria of the hippocampus. Behavioral impairments, for example a poorer righting reflex, also resulted.
Although the majority of double-blind placebo controlled studies on this topic have been carried out in the developing world, it would be surprising if the conclusion that improved iron status improves psychological functioning was not supported in industrialized countries. For example in an inner-city English sample of 18 month old children, Aukett et al. [7] found that those who received iron supplements for 2 months, in a double-blind trial, had an increased rate of weight gain and achieved more than the expected psycho-motor development.
The importance of a marginal intake of iron is unclear, where reserves are depleted although anaemia has not developed. The topic has been subject to little examination, although Bruner et al. [27] noted that 25% of adolescent girls in the USA are iron deficient. In a double-blind trial they found that the iron supplementation of non-anaemic but iron-deficient adolescent girls improved verbal learning and memory.
Kretchmer et al. [52] listed key unresolved questions as establishing the relative effect of acute and chronic iron deficiency; considering the importance of the severity of iron deficiency; examining the biological, psychological and social consequences of deficiency to establish the causal mechanism.
Zinc
Maret and Sandstead [61] estimated that 20% of the world population was zinc deficient. They found that the study of rodents and non-human primates has shown that zinc deficiency during gestation and suckling results in behavioral impairment that persists in spite of a subsequent adequate intake. Zinc plays a central role in the growth of cells. It is involved with the activity of over two hundred enzymes, in particular those necessary for the synthesis of RNA and DNA. It is found in high levels in the brain where it plays both structural and functional roles [24]. A deficiency of zinc slows growth and delays sexual maturation. In a Cochrane review Mahomed et al. [59] summarized trials that involved over 9,000 mothers and their babies and found that supplementation resulted in a 14% reduction in preterm births although the number of low birth weights was not reduced. The studies came from both developing and industrialized countries.
When considering the developmental role of zinc the age of the child may be important. Low levels of plasma zinc have been reported during infancy and adolescence, times of rapid growth [28]. In juvenile monkeys zinc deficiency was associated with reduced activity and poorer memory and attention [42]. A review of the animal studies noted that the decline in food intake associated with zinc deficiency may result in other nutritional deficiencies. Severe zinc deficiency during the period of brain growth has a similar impact to protein-energy-malnutrition [43]. In immature animals zinc deprivation increases emotionality, decreases appetite, reduces activity and disrupts memory and attention. At a physiological level there is increasing evidence that zinc is involved in the development of NMDA receptors, a site at which glutamate acts as a neurotransmitter, particularly in the hippocampus a region of the brain involved in learning and memory [55].
In humans there is also a need to distinguish the age when zinc supplementation took place. Wasantwisut [96] concluded that in particular preterm infants benefit from zinc supplementation. There is evidence that when it is given to the mother, or with the new-born it is added to the milk, that zinc may have an impact. In Canada low birth-weight babies were randomly allocated to a baby formula with or without a zinc supplement and their development was assessed for 12 months. Those with the additional zinc grew more quickly and displayed better motor development [38]. Similarly low zinc status has been associated with decreased activity in Indian children [78] and poorer attention in Egyptian infants [51]. It seems possible that any influence of zinc may prove to be mediated via changes in activity or emotionality.
In contrast in older children there is less evidence that zinc supplementation has a beneficial impact on cognition. However, in Canada zinc supplementation of 5–7 year old boys, for 12 months, did not influence attention span or taste acuity although a sub-group of boys with low hair zinc levels responded with increased growth [41]. A study of Chinese children, aged 6–9 years, for the first time reported that a zinc supplement improved neuro-psychological functioning [68]. This study also found that zinc when combined with other micro-nutrients had a larger influence on growth rate than either zinc or the other micro-nutrients by themselves. A meta-analysis found that zinc supplementation had a significant yet small influence (0.22 of a standard deviation) on the growth on children up to 13 years of age [22].
There are reports in American samples that elevated serum copper and depressed plasma zinc levels both found in those with a history of aggression [94]. Animal studies have also related a zinc deficiency diet during gestation to aggression when adult [69]. Arnold and DiSilvestro [6] reviewed the evidence that zinc deficiency may play a role in ADHD. They found numerous cross-sectional studies that reported lower zinc tissue levels in children who have ADHD, compared to normal controls or population norms. They noted that the positive findings from placebo-controlled trials came from Turkey and Iran, areas with suspected endemic zinc deficiency. They concluded, however, that it was unclear how the evidence applies to middle-class American children. Arnold et al. [5] therefore related serum zinc to parent and teacher ratings of inattention and found a significant negative relationship. There remains a need for intervention trials in countries where the zinc in the diet is not particularly low.
In summary, although the role of zinc in brain functioning is poorly understood it is essential both before and after birth for normal development. A deficiency in late pregnancy impairs neuronal replication and synaptogenesis. Irrespective of the mechanism, a deficiency in animals disrupts learning and memory later in life. Sandstead [77] noted that it was unknown if similar influences occur in humans but it was possible that a zinc-induced disruption of foetal growth had long-term consequences for brain functioning.
Choline
Choline can be made by the body but is classified, at least in the USA, as an essential nutrient as the demand cannot be satisfied by de novo synthesis. It has three major functions: it is a precursor for the neurotransmitter acetylcholine, the methyl donor betaine and phospholipids. Zeisel [100] concluded that choline is critical while the foetus is in the womb: “when it influences stem cell proliferation and apoptosis, thereby altering brain and spinal cord structure and function and influencing risk for neural tube defects and lifelong memory function.” Neonates have a higher level of plasma choline (40 µg/l) than adults (7–20 µg/l) although values fall during the first year of life [30]. As choline influences the proliferation of stem cells and apoptosis it alters the structure and functioning of the brain. Zeisel and Niculescu [102] suggested that in rodents memory is permanently enhanced if they are exposed to choline towards the end of gestation. Similarly a deficiency during this sensitive period for brain development is associated with deficits in memory and cognition. In animals Zeisel [101] concluded that the evidence that choline influenced the hippocampus, an area of the brain involved with memory, was compelling, although we await evidence of similar effects in humans. McCann et al. [62] reviewed thirty-four animal studies that had related the availability of choline during gestation to subsequent neurological functioning. They concluded that “choline supplementation during development results in improved performance of offspring in cognitive or behavioral tests.”
Although there is substantial evidence that choline plays an important role in brain development there is to date no reason to suggest that in humans its provision limits neural development. After reviewing the topic Colombo et al. [30] were unable to find evidence that there was a beneficial effect of supplementing infant formulae with choline.
Folic acid
A role for folate in the prevention of neural tube defects is well established so that women capable of becoming pregnant are encouraged to consume this vitamin [72]. Adequate folate status is important for the normal growth of the foetus, as supplementation during pregnancy has been found to decrease the incidence of immaturity [11] and to favourably affect the weight and the condition of the newborn child [86]. Mental retardation is associated with genetically determined errors of folate metabolism [54]. In rodents the feeding of a diet low in folate to pregnant mothers adversely influenced the maze learning ability of the offspring [98] and there are adverse consequences for brain development [31]. After reviewing the topic Reynolds [75] concluded that folates were of fundamental importance for brain development, effects that probably reflect an influence on nucleotide synthesis, DNA integrity and transcription.
However, although the possibility arises that folate status during pregnancy may influence human brain development, there are only two studies of the influence of the folate status of the mother during pregnancy on child development. Gross et al. [46] found that infants born to mothers with severe folate deficiency during pregnancy showed abnormal or delayed development. However, Tamura et al. [88] reported that the folate status of mothers in the second half of pregnancy had little impact on the neurodevelopment of their children at five years of age. They suggested that the most likely explanation of the discrepancy in the results of these two studies was that in the latter the classification of low-folate status relied on biochemical measures rather than clinical signs such as megablastic anaemia. As both these studies took place before the fortification of grain products it may prove impossible to further study the phenomenon in countries where this occurs.
Al-Tahan et al. [2] considered the dietary intake and the folate status of adolescents living in Europe. In girls they found evidence for a possible deficiency of folate and that the wide variations in intake made a deficiency likely in parts of the population.
Vitamin B12
If appropriate care is not taken when constructing a vegetarian diet problems can result. Vitamin B12 attracts particular attention as only animal products offer significant amounts, although milk, cheese and eggs offer a source for the vegetarian. Vegans, who consume no animal products, are advised to take a vitamin B12 supplement although many vegan foods are fortified. The primary functions of this vitamin are roles in the formation of red blood cells, the synthesis of DNA and the maintenance of a healthy nervous system. Deficiency can result in pernicious anaemia with consequent tiredness, breathlessness and fatigue. Vitamin B12 plays a role in the metabolism of the fatty acids needed to produce myelin the sheath around the neuronal axon. Thus deficiency can result in vitamin B12 neuropathy with its associated degeneration of nerve fibres and irreversible brain damage.
However, if carefully planned, vegetarian diets can be adequate at all stages of the life cycle including pregnancy, lactation, infancy and childhood. A review considered potentially problem nutrients for vegetarians that include protein, iron, zinc, calcium, vitamin D, riboflavin, vitamin B12, vitamin A, n-3 fatty acids and iodine. It concluded that needs may be met by a vegetarian diet although in some cases by using fortified foods [4].
Louwan et al. [56] related impaired cognitive functioning to a marginal vitamin B12 status. Control subjects performed better on a range of psychological tests than those with a low vitamin status due to the consumption of a macrobiotic diet. There was a significant correlation between the degree of cobalamin deficiency and a non-verbal measure of intelligence. As a deficiency can cause brain damage in infants an adequate supply of vitamin B12 is particularly important for children and pregnant or breastfeeding women. Graham et al. [44] reviewed the long-term consequences of vitamin B12 deficiency in infancy and reported a consistent clinical pattern of irritability, anorexia and failure to thrive associated with marked developmental regression and poor brain growth. For example von Schenck et al. [93] described a fourteen month boy with severe dietary vitamin B12 deficiency that resulted from the vegan diet of the mother. Magnetic resonance imaging (MRI) of the brain showed severe frontal and fronto-parietal atrophy. After six weeks of vitamin B12 supplementation the EEG became normal and MRI showed that the structural abnormalities had disappeared. Unfortunately at the age of two years cognitive and language development remained seriously retarded suggesting that vitamin B12 deficiency in infancy may have lasting consequences. Louwman et al. [56] examined the cognitive functioning of adolescents, aged ten to sixteen years, who had marginal vitamin B12 status from the consumption of a vegan diet up to an average age of six, but who had subsequently consumed a vegetarian or omnivorous diet. They found that vitamin B12 deficiency up to the age of six was associated with poorer fluid intelligence as adolescents. A strict vegan diet in early childhood was associated with a poorer vitamin B12 status in later life even when a vegan diet was not subsequently consumed.
Other vitamins
The idea that a clinical deficiency of thiamine may disrupt cognitive functioning is readily accepted as problems of memory can occur in the late stages of the deficiency disease Beri beri. It is, however, interesting to recall the study of Harrell [48] who examined children who ate a diet that supplied 1 mg of thiamine a day. The Recommended Daily Allowance for the boys in this study was 1 mg a day, and for girls it was 0.9 mg. A priori this diet would have been said to supply an adequate amount of thiamine. Yet after taking 2 mg thiamine, each day for a year, in a double-blind study those who took the vitamin were significantly taller, had better eye-sight, quicker reaction times, and scored better on tests of memory and intelligence. Such an isolated finding is difficult to evaluate but the study was well designed, the outcome was striking and deserves some attention.
Vitamin B6 is a co-factor for decarboxylase enzymes that are important in the synthesis of amino-acid neurotransmitters. Animal research has found that vitamin B6 deficiency during gestation and lactation alters the functioning of the N-methyl-D-aspartate receptor (NMDA) thought to be important in learning and memory [47]. Numerous studies report that some pregnant and lactating women have an intake of vitamin B6 below the recommended levels, such that the vitamin status of the infant is affected. Low vitamin B6 status has been associated with the slower growth of breast-fed infants [49]. In Egyptian infants the level of vitamin B6 in the mothers’ milk predicted how often the child cried. Mothers with low levels of vitamin B6 were less responsive to their child’s distress. The authors concluded that low vitamin B6 status influenced both the behavior of the child and the mother [63]. Although it has been suggested that there is a relationship between vitamin B6 intake and autism a critical review [65] rejected most studies on methodological grounds leaving only three studies that were of satisfactory design. They concluded that due to the small number of studies, small sample sizes and the methodological quality, the use of vitamin B6-magnesium as a treatment for autism could not be recommended.
Multi vitamins/mineral supplements
Although there are many studies of particular micro-nutrients it is likely that in many instances a diet that is deficient in one respect will be deficient in others. Nutrients do not function in isolation. Given that most poor diets will result in an inadequate intake of a range of nutrients, it is arguable that it is more likely that a positive response will come from the use of a multi-vitamin / mineral supplement. It is possible that on occasions a beneficial response to the supplementation of a single deficient nutrient has not been observed because the functioning of other aspects of a chain of necessary reactions has been inhibited by other deficiencies. Thus a case can be made for examining the response to a multi-vitamin / mineral supplement.
SUMMIT [83] compared mothers in Indonesia who received either a multi-micronutrient supplement or a combination of iron and folic acid. In a double-blind trial involving 31,290 pregnant women there was an 18% reduction in early infant mortality after taking the multi-micronutrients rather than iron and folic acid, and a 14% reduction in the incidence of low birthweight. In double-blind trial Vazir et al. [91] gave a drink fortified with micronutrients to Indian children aged 6–15 years with middle-income parents. Over a 14 month period supplementation improved attention/concentration but not intelligence, memory or achievement in school. Similarly Kumar et al. [53] gave a supplement of iron, iodine, calcium and seven vitamins to 7–11 year old Indian children. With four out of the seven memory tests, and a test of attention, those receiving supplementation had better scores than a control group, although a measure of intelligence was not influenced.
It is more controversial to suggest a benefit of micro-nutrient supplementation in industrialized countries. In the United Kingdom Benton and Roberts [21], in a randomized double-blind placebo controlled study, gave children aged 12–13 years either a placebo or a multi- vitamin/mineral supplement for eight months. Whereas scores on a verbal intelligence were not influenced by supplementation, scores on a non-verbal test of intelligence increased significantly. When Benton [16] reviewed the topic he found ten out of thirteen studies had reported a positive response in at least a sub-group of children. Importantly the response was always with non-verbal and never with verbal measures of intelligence. This highly selective response suggested a genuine phenomenon.
More recently Osendarp et al. [66] for a year gave children aged 6–11 years, in Australia and Indonesia, drinks that contained two minerals and five vitamins, or omega-3 fatty acids, or both. In both girls and boys in Australia and girls in Indonesia those receiving the micronutrients rather than a placebo had better scores on tests of verbal learning, although neither general intelligence nor attention were influenced. The omega-3 fatty acid supplementation did not influence any of the cognitive tests. It was concluded that “in well-nourished school-aged children, fortification with multiple micronutrients can result in improvements in verbal learning and memory.”
Benton [16] concluded that the topic was at an early stage and there was a need for large-scale trials that considered the composition of the supplement, the dietary styles of the children and the nature of the influence on cognition. Which of the nutrients in the multi-vitamin / mineral supplements were important and at what dose are questions that have not been addressed? There is no suggestion that all children respond, in fact it has been suggested that it is a minority. An explanation for the inconsistencies in this area is that it is possible that only children who are poorly nourished respond to supplementation. Benton and Buts [18]studied children in seven Belgium schools who kept a daily diary for fifteen days. It was a minority of children who responded to supplementation in this study, those whose diets offered a low intake of a range of micro-nutrients. It appeared that rather than suggesting that the micro-nutrient supplementation was improving intelligence it was more accurate to suggest that a poor diet was detrimental. These children tended to come from less economically privileged areas and from schools for the less academically able.
Externalizing
In industrialized societies there have also been suggestions that a diet sub-optimal in micro-nutrients may in adolescents predispose to anti-social behavior [17]. Schoenthaler et al. [80] examined the influence of vitamin/mineral supplementation in a double-blind trial. In imprisoned juveniles with a diagnosis of ‘Aggressive’ using DSM-III criteria, over three months the incidence of violence was 28% less in those receiving a supplement rather than placebo. When blood samples taken before and after supplementation were considered there was no difference in the incidence of violence in those whose vitamin status did not change during the study. In those whose vitamin status improved there was a marked decline in the incidence of violence. The assumption was that an improvement in vitamin status is indicative of an initially poor vitamin status and that over time supplementation had replenished reserves. Similarly a well designed study [40] found that the disciplinary record of young offenders responded to micro-nutrient supplementation. The greatest reduction occurred in more serious violent offences. It this study it is unclear whether the response was to vitamins, minerals or fatty acids, although previous research suggested that all may be involved. The impact of micro-nutrient supplementation has also been studied in school-children [81]. Violent and non-violent delinquency was measured using the official school disciplinary record. During the 4 month intervention those receiving the supplements were disciplined significantly less frequently than those taking the placebo. It was suggested that there was a general decline in “impulsive misconduct.” Thus there are three well designed studies that report a decrease in anti-social behavior after consuming vitamin/mineral supplements. Although the findings are suggestive, additional evidence will be required before the phenomenon is widely accepted and the active ingredients and doses have been established.
Discussion
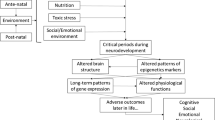
It has been commonly asked whether there are critical periods during which micro-nutrient deficiencies results in changes in brain development that have long-term consequences. It is widely accepted that the rapid rate of growth of the brain during the last third of gestation and the early postnatal stage makes it vulnerable to an inadequate diet. It has become apparent that at this stage certain nutrients are more likely to be influential than others. The implications of a nutrient deficiency will depend on the stage of development, the degree to which provision is deficient and for how long it lasts.
Between 24 weeks after conception and birth the brain develops from a mostly smooth structure with two lobes to an organ that in external appearance resembles the adult brain. The process of myelination and the development of synaptic connections begins prior to birth. Myelination is the major cause of the increase in the size of the brain; it begins in the last third of gestation but continues into adulthood. The brain of a full-term infant has many more synapses than the adult but this is followed by apoptosis, or programmed cell death. The rate that it occurs depends on the area of the brain [89]. For example the number of synapses in the visual area peak about four months after birth after which it falls to reach adult levels about 5 years of age. A similar profile occurs for the areas dealing with language and hearing, although the peak number of synapses occurs about 8 months. The pattern differs with the pre-frontal cortex, the area of the brain that deals with the planning and organization of behavior. In this instance the number of synapses peak about one year of age and the adult number is reached about 15 years of age. Clearly there are important aspects of brain development that take place after the first 3 years. These patterns of creating and destroying synapses raise the question of possible critical periods during which both environmental stimulation and nutrition may be influential. However, Thompson and Nelson [89] stressed that critical periods are not typical of human development as they imply a narrow window of opportunity. Rather they suggest, given the longer time period, that they are better described as sensitive periods. For example exposure to speech in the first years encourages the ability to discriminate sounds and exposure to visual stimulation in the first few years is essential for some aspects of visual processing such as binocular depth perception. It is tempting to suggest the use of such profiles to direct the choice of tests of neural functioning when the adequacy of nutrition is varied at different stages of development. However, Georgieff [39] noted that such an approach is impracticable as infants have a limited range of behavioral expressions although by four months, as the cortex plays a greater role, the possibilities of the measurement of cognition increase. In addition the effects of particular aspects of nutrition can be global or alternatively several nutrients can have a similar influence, for example protein-energy, iron and zinc malnutrition all influence the development of the hippocampus and hence memory. Alternatively the underlying mechanism may be general such that it cannot be assessed by a specific test. For example Kretchmer et al. [52] suggested that iron status influences attention or arousal that in turn may effect many aspects of cognition.
Although all nutrients play a role in brain development some are critical, because they play important roles and are more likely to be deficient. Georgieff [39] concluded that the “rapidly developing brain is more vulnerable to nutrient insufficiency” and that certain nutrients have a greater effects on brain development than others including “protein, energy, certain fats, iron, zinc, copper, iodine, selenium, vitamin A, choline, and folate”.
Iron is rapidly taken up by the foetus during the last trimester of pregnancy and is needed for the production of the neurotransmitter dopamine, myelination and energy metabolism [12]. Iron deficiency in the perinatal period reduces oxidative metabolism in the frontal cortex and hippocampus. De Deungria et al. [33] concluded that “perinatal iron deficiency differentially reduces neuronal metabolic activity, specifically targeting areas of the brain involved in memory processing”. Although the majority of work on the implication of iron deficiency have been carried out using animals, Tamura et al. [87] assessed iron status by measuring the level of ferritin, the storage protein for iron, in the umbilical cord of 278 children. At the age of 5 years those with the lowest values had a poorer language and fine-motor skills.
However, received wisdom is that in industrialized societies, beyond the early years of life, the consumption of a balanced diet is likely to result in an adequate intake of micro-nutrients such that supplementation should not be beneficial. This view that deficiencies are unlikely relies greatly on the relationship between assessments of dietary input and the population needs for micro-nutrients as summarized as Dietary Reference Values or Recommended Daily Amounts [36]. The preamble to the British Dietary Reference Values [35] puts these norms into context. They state that “some nutrients may have a variety of physiological effects at different levels of intake. Which of these effects should form the parameter of adequacy is therefore to some extent arbitrary.” In no instance have psychological or behavioral indices been the measure of adequacy used when deriving these reference values. Yet Benton [15] noted that the first symptoms associated with micro-nutrient deficiency are often psychological and that in well controlled double-blind trials micro-nutrient supplementation has been reported to improve mood, memory and attention. For example, in a double-blind trial thiamine supplementation was found to improve mood, although as judged by the usual physiological index of bodily status, erythrocyte transketolase activation, the population was well nourished prior to supplementation [19, 20]. Similarly Harrell [48] reported that improved cognition resulted from thiamine supplements in children whose diet already supplied the recommended level.
Why might psychological variables prove more susceptible to micro-nutrient status than disease states? The brain is the most complex and metabolically active organ in the body, thus behavior reflects the summated outcome of countless millions of metabolic processes. In this way even minor metabolic inefficiencies could create a cumulative adverse effect. Small changes in micro-nutrient status, responsible for differences of only a few percent in the activity of a single enzyme could, when multiplied several million-fold, result in a noticeably different output. If this argument has validity then the functioning of the brain, given its complexity, would be expected to be the first organ to demonstrate disrupted functioning. The progression of disease can take place over decades making the impact of diet difficult to demonstrate, in contrast the output of the brain is almost instantaneous and hence maybe more easily observed.
However, as psychological measures are unfamiliar to most nutritionists, as an alternative one of the many ways in which marginal deficiencies could potentially influence neural functioning is discussed. The decarboxylase enzymes are important in the metabolism of a range of neurotransmitters including serotonin, dopamine and noradrenaline and have as a coenzyme pyridoxal phosphate, the form in which vitamin B6 occurs most commonly in the diet. There is evidence of marginal intakes of this vitamin. Using a biochemical measure of pyridoxal phosphate status there was a sub-group of about ten percent of British children who were deficient [45]. In males the incidence of deficiency increased with age. In young British adults 27.7% of males and 36.6% of females were deficient as judged by the same measure [20]. Bender [14] concluded that although a gross deficiency was rare a marginal inadequacy of vitamin B6 was relatively common, to the extent that it affected amino acid metabolism and the functioning of steroid hormones. In rats varying the dietary intake of vitamin B6 was found to increase the serotonin content of various areas of the brain. It was suggested that this reflected the role of pyridoxal phosphate in the regulation of the decarboxylation of 5-hydroxytryptophan. A continuum existed from deficiency to a moderate excess that was associated with the rate of the synthesis and release of serotonin [32]. Such data indicate one mechanism by which a marginal intake of a micro-nutrient could influence neurochemistry and hence psychological measures.
In summary what conclusions can be drawn and advice offered about the intake of micro-nutrients? It is obvious to suggest that attention should be given in the developing world to the fortification of food where micro-nutrient deficiencies exist [64]. For example South Africa has developed a National Food Fortification Program of wheat, maize flour and sugar to which calcium, iron, zinc, vitamins A, B1, B2, B3, B6 and folate are added. However, Uauy et al. [90] make the important point that in developing countries attempts to improve nutrition should be aware that obesity and its associated problems may develop: that is stunted growth and micronutrient deficiencies may coexist with obesity. Although the origins of obesity are complex the pattern of prenatal and postnatal growth are contributing factors [10]. Uauy et al. [90] suggested that attempts to prevent malnutrition should “emphasize improvements in linear growth in the first 2–3 years of life rather than aim at gaining weight”.
In industrialized societies received wisdom is that women who are or who are planning to become pregnant should take a folic acid supplement to decrease the risk of birth defects. Although after a Cochrane review [60] concluded that “there is not enough evidence to evaluate the effects of vitamin D supplementation during pregnancy”, in some countries supplementation is recommended. For example in the United Kingdom the recommendation is that supplementation should aim to achieve an intake of 10 µg/day [35]. If blood iron levels become low it may be supplemented under medical supervision. A large intake of vitamin A, from diet and supplements, is not advised for those who are pregnant as birth defects may result. In children between 6 months and 4 years the UK Department of Health recommends the taking of supplements of vitamins A, C and D. These recommendations reflect a general concern about the body rather than a specific concern about the brain: vitamin A is needed for vision and skin, vitamin C for bones and body tissues, vitamin D for general growth, bones and teeth. After this stage, the conventional advice is that those consuming a balanced diet will obtain the micro-nutrients they need as they are inevitably associated with macro-nutrients. However, the Committee on Nutrition of the American Academy of Pediatrics [3] suggested that it might be appropriate to use supplements where individuals are unable or unwilling to consume an adequate diet: such as those with poor eating habits, those dieting, those eating a strict vegetarian and pregnant teenagers who are likely to need both iron and folic acid. We await further evidence before conclusions are warranted concerning the possible cognitive benefits of supplementation in those with sub-clinical deficiencies.
References
Akinci A, Sarac K, Gungor S, Mungan I, Aydin O (2006) Brain MR spectroscopy findings in neonates with hypothyroidism born to mothers living in iodine-deficient areas. Am J Neuroradiol 27:2083–2087
Al-Tahan J, González-Gross M, Pietrzik K (2006) B-vitamin status and intake in European adolescents. A review of the literature. Nutr Hosp 21:452–465
American Academy of Pediatrics Committee on Nutrition (1980) Vitamin and mineral supplement needs of normal children in the United States. Pediatrics 66:1015–1020
American Dietetic Association, Dieticians of Canada: Vegetarian diets (2003). J Am Diet Assoc 103:748–765
Arnold LE, Bozzolo H, Hollway J, Cook A, DiSilvestro RA, Bozzolo DR, Crowl L, Ramadan Y, Williams C (2005) Serum zinc correlates with parent- and teacher- rated inattention in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 15:628–636
Arnold LE, DiSilvestro RA (2005) Zinc in attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 15:619–627
Aukett MA, Parks YA, Scott PH, Wharton BA (1986) Treatment with iron increases weight gain and psychomotor development. Arch Dis Child 61:849–857
Azizi F, Saarshar A, Nafarabadi M, Kimiagar M, Noohi S, Rahbar N, Bahrami A, Kalantari S (1993) Impairment of neuromotor and cognitive development in iodine-deficient schoolchildren with normal physical growth. Acta Endocrinol 129:501–504
Ballew C, Bowman BA, Sowell AL, Gillespie C (2001) Serum retinol distributions in residents of the United States: third national health and nutrition examination survey, 1988–1994. Am J Clin Nutr 73:586–593
Barker DJ (2006) Adult consequences of foetal growth restriction. Clin Obstet Gynecol 49:270–283
Baumslag N, Edelstein T, Metz J (1970) Reduction of incidence of prematurity by folic acid supplementation in pregnancy. Br Med J 1(5687):16–17
Beard JL, Connor JR (2003) Iron status and neural functioning. Ann Rev Nutr 23:31–58
Becker DV, Braverman LE, Delange F, Dunn JT, Franklyn JA, Hollowell JG, Lamm SH, Mitchell ML, Pearce E, Robbins J, Rovet JF (2006) Iodine supplementation for pregnancy and lactation-United States and Canada: recommendations of the American thyroid association. Thyroid 16:949–951
Bender DA (1992) Nutritional biochemistry of the vitamins. Cambridge University Press, Cambridge
Benton D (1992) Vitamin-mineral supplements and intelligence. Proc Nutr Soc 51:295–302
Benton D (2001) Micronutrients supplementation and the intelligence of children. Neurosci Biobehav Rev 25:297–309
Benton D (2007) The impact of diet on anti-social behaviour. Neurosci Biobehav Rev 31:752–774
Benton D, Buts J-P (1990) Vitamin/mineral supplementation and intelligence. Lancet 335:1158–1160
Benton D, Griffiths R, Haller J (1997a) Thiamine supplementation mood and cognitive functioning. Psychopharmacol 129:66–71
Benton D, Haller J, Fordy J (1997b) The vitamin status of young British adults. Int J Vit Nutr Res 67:34–40
Benton D, Roberts G (1988) Vitamin and mineral supplementation improves the intelligence of a sample of school children. Lancet 140–143
Bhandari N, Bahl R, Taneja S (2001) Effect of micronutrient supplementation on linear growth of children. Br J Nutr 85(Suppl 2):S131–S137
Biesalski HK, Brummer RJ, König J, O’Connell MA, Ovesen L, Rechkemmer G, Stos K, Thurnham DI (2003) Micronutrient deficiencies. Hohenheim consensus conference. Eur J Nutr 42: 353–363
Black MM (1998) Zinc deficiency and child development. Am J Clin Nutr 68(suppl):464S–469S
Bleichrodt N, Drennth PJ, Queerido A (1980) Effects of iodine deficiency on mental and psychomotor abilities. Am J Phys Anthropol 53:55–67
Bogen DL, Duggan AK, Dover GJ, Wilson MH (2000) Screening for iron deficiency anemia by dietary history in a high-risk population. Pediatrics 105:1254–1259
Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J (1996) Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 348:992–996
Butrimovitz GP, Purdy WC (1978) Zinc nutrition and growth in a childhood population. Am J Clin Nutr 31:1409–1412
Cocco S, Diaz G, Stancampiano R, Diana A, Carta M, Curreli R, Sarais L, Fadda F (2002) Vitamin A deficiency produces spatial learning and memory impairment in rats. Neuroscience 115:475–482
Colombo JP, Garcia-Rodenas C, Guesry PR, Rey J (2003) Potential effects of supplementation with amino acids, choline or sialic acid on cognitive development in young infants. Acta Paediatr Suppl 92:42–46
Craciunescu CN, Brown EC, Mar M-H, Albright CD, Nadeau MR, Zeisel SH (2004) Folic acid deficiency during late gestation decreases progenitor cell proliferation and increases in apoptosis in fetal mouse brain. J Nutr 134:162–166
Dakshinamurti K, Sharma SK, Bonke D (1990) Influence of B vitamin on binding properties of serotonin receptors in the CNS of rats. Klin Wochenschr 68:142–145
de Deungria M, Rao R, Wobken JD, Luciana M, Nelson CA, Georgieff MK (2000) Perinatal iron deficiency decreases cytochrome c oxidase (CytOx) activity in selected regions of neonatal rat brain. Pediatr Res 48:169–176
Delange F (1994) The disorders induced by iodine deficiency. Thyroid 4:107–128
Dietary reference values for food energy and nutrients for the United Kingdom (1991) Her Majesty’s Stationary Office, London
Dietary references intakes (2001) National Academy Press, Washington, DC
Diets of British Schoolchildren (1989) Report on health and social subjects vol 36. Department of Health, H.M.S.O, London
Friel JK, Andrews WL, Matthew JD, Long DR, Cornel AM, Cox AM, McKim E, Zerbe GO (1993) Zinc supplementation in very low birth weight infants. J Pediatr Gastroenterol Nutr 17:97–104
Georgieff MK (2007) Nutrition and the developing brain: nutrient priorities and measurement. Am J Clin Nutr 85:614S–620S
Gesch CB, Hammond SM, Hampson SE, Eves A, Crowder MJ (2002) Influence of supplementary vitamins, minerals and essential fatty acids on the antisocial behaviour of young prisoners. Randomised placebo-controlled trial. Br J Psychiatry 181:22–28
Gibson RS, Vanderkooy PD, MacDonald AC, Goldman A, Ryan BA, Berry M (1989) A growth-limiting, mild zinc-deficiency syndrome in some southern Ontario boys with low height percentiles. Am J Clin Nutr 49:1266–1273
Golub MS, Takeuchi PT, Keen CL, Gershwin ME, Hendricks AG, Lonnerdal B (1994) Modulation of behavioural performance of prepubertal monkeys by moderate dietary zinc deprivation. Am J Clin Nutr 60:238–243
Golub MS, Keen CL, Gershwin ME, Hendricks AG (1995) Developmental zinc deficiency and behavior. J Nutr 125:2263S–2271S
Graham SM, Arvela OM, Wise GA (1992) Nutritional vitamin B12 deficiency. Long-term neurologic consequences of in infants. J Pediatr 121:710–714
Gregory J, Lowe S (2000) National diet and nutrition survey: young people aged 4–18 years. The Stationery Office, London
Gross RL, Newberne PM, Reid JVO (1974) Adverse effects on infant development associated with maternal folic acid deficiency. Nutr Rep Int 10:241–248
Guilarte TR (1993) Vitamin B6 and cognitive development: recent research findings from human and animal studies. Nutr Rev 51:193–198
Harrell RF (1946) Mental responses to added thiamine. J Nutr 31:283–298
Heiskanen K, Siimes MA, Salmenpera L, Perheentupa J (1995) Low vitamin B6 status associated with slow growth in healthy breast-fed infants. Pediatr Res 38:740–746
Iannotti LL, Tielsch JM, Black MM, Black RE (2006) Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr 84:1261–1276
Kirksey A, Wachs TD, Yunis F (1994) Relation of maternal zinc nutritiure to pregnancy outcome and infant development in an Egyptian village. Am J Clin Nutr 60:782–792
Kretchmer N, Beard JL, Carlson S (1996) The role of nutrition in the development of normal cognition. Am J Clin Nutr 63:997S–1001S
Kumar MV, Rajagopalan S (2007) Multiple micronutrient fortification of salt and its effect on cognition in Chennai school children. Asia Pac J Clin Nutr 16:505–511
Lanzkowsky P, Erlandson ME, Bezan AI (1969) Isolated defect of folic acid absorption associated with mental retardation and cerebral calcification. Blood 34:452–465
Levenson CW (2006) Regulation of the NMDA receptor: implications for neuropsychological development. Nutr Rev 64:428–432
Louwman MW, van Dusseldorp M, van de Vijver FJ, Thomas CM, Schneede J, Ueland PM, Refsum H, van Staveren WA (2000) Signs of impaired cognitive function in adolescents with marginal cobalamin status. Am J Clin Nutr 72:762–769
Lozoff B (2007) Iron deficiency and child development. Food Nutr Bull 28(Suppl 4):S560–S571
Mahawithanage ST, Kannangara KK, Wickremasinghe R, Chandrika UG, Jansz ER, Karunaweera ND, Wickremasinghe AR (2007) Impact of vitamin A supplementation on health status and absenteeism of school children in Sri Lanka. Asia Pac J Clin Nutr 16:94–102
Mahomed K, Bhutta Z, Middleton P (2007) Zinc supplementation for improving pregnancy and infant outcome. Cochrane Database Syst Rev CD000230
Mahomed K, Gulmezoglu AM (2000) Vitamin D supplementation in pregnancy. Cochrane Database Syst Rev CD000228
Maret W, Sandstead HH (2007) Possible roles of zinc nutriture in the foetal origins of disease. Exp Gerontol 2007 Oct 22 email
McCann JC, Hudes M, Ames BN (2006) An overview of evidence for a causal relationship between dietary availability of choline during development and cognitive function in offspring. Neurosci Biobehav Rev 30:696–712
McCullough AL, Kirksey A, Wachs TD, McCabe GP, Bassily NS, Bishry Z, Galal OM, Harrison GG, Jerone NW (1990) Vitmain B6 status of Egyptian mothers: relation to infant behavior and maternal-infant interactions. Am J Clin Nutr 51:1067–1074
Nutrition Service of the World Food Program (2006) Micronutrient fortification: WFP experiences and ways forward. Food Nutr Bull 27:67–75
Nye C., Brice A (2005) Combined vitamin B6-magnesium treatment in autism spectrum disorders. Cochrane Database Syst. Rev 4: CD003497
Osendarp SJ, Baghurst KI, Bryan J, Calvaresi E, Hughes D, Hussaini M, Karyadi SJ, van Klinken BJ, van der Knaap HC, Lukito W, Mikarsa W, Transler C, Wilson C, NEMO Study Group (2007) Effect of a 12-mo micronutrient intervention on learning and memory in well-nourished and marginally nourished school-aged children: 2 parallel, randomized, placebo-controlled studies in Australia and Indonesia. Am J Clin Nutr 86:1082–1093
Oski FA (1979) The nonhematologic manifestations of iron deficiency. Am J Dis Child 133:315–322
Penland JG, Sandstead HH, Alcok NW, Dayal HH, Chen XC, Li JS, Zhao F, Yang JJ (1997) A preliminary report: effects of zinc and micro-nutrient repletion on growth and neuro-psycholoigcal function of urban Chinese children. J Am Coll Nutr 16:268–272
Peters DP (1978) Effects of prenatal nutritional deficiency on affiliation and aggression in rats. Physiol Behav 20:359–362
Pharoah POD, Connolly KJ, Ekins RP, Harding AG (1984) Maternal thyroid hormone levels in pregnancy and subsequent cogntive and motor performance of the children. Clin Endocrinol 21:265–270
Pilch SM (1987) Analysis of vitamin A data from the health and nutrition examination surveys. J Nutr 117: 636–640
Pitkin RM (2007) Folate and neural tube defects. Am J Clin Nutr 85:285S–288S
Pollitt E, Leibel RL (1976) Iron deficiency and behaviour. J Pediatr 88:372–381
Reifen R, Ghebremeskel K (2001) Vitamin A during pregnancy. Nutr Health 15:237–243
Reynolds E (2006) Vitamin B12, folic acid, and the nervous system. Lancet 5:949–960
Sachdev H, Gera T, Nestel P (2005) Effect of iron supplementation on mental and motor development in children: systematic review of randomised controlled trials. Public Health Nutr 8:117–132
Sandstead HH (2003) Zinc is essential for brain development and function. J Trace Elements Exp Med 16:165–173
Sazawal S, Bentley M, Black RE, Dhingra P, George S, Bhan MK (1996) Effect of zinc supplementation on observed activity in low socioeconomic Indian preschool children. Pediatrics 98:1132–1137
Schneider JM, Fujii M, Lamp CL, Lonnerdal B, Dewey KG, Zidenberg-Cherr S (2005) Anemia, iron deficiency, and iron deficiency anemia in 12–36-mo-old children from low-income families. Am J Clin Nutr 82:1269–1275
Schoenthaler SJ, Amos S, Doraz W, Kelly MA, Muedeking G, Wakefield J (1997) The effect of randomized vitamin-mineral supplementation on violent and non-violent anti-social behavior among incarcerated juveniles. J Nutr Environ Med 7:343–352
Schoenthaler SJ, Bier ID (2000) The effect of vitamin-mineral supplementation on juvenile delinquency among American schoolchildren: a randomized, double blind placebo-controlled trial. J Altern Comp Med 6:7–17
Sommer A (1982) Nutritional blindness, xerophthalmia and keratomalacia. Oxford University Press, New York
Supplementation with Multiple Micronutrients Intervention Trial (SUMMIT) Study Group, Shankar AH, Jahari AB, Sebayang SK, Aditiawarman , Apriatni M, Harefa B, Muadz H, Soesbandoro SD, Tjiong R, Fachry A, Shankar AV, Atmarita , Prihatini S, Sofia G (2008) Effect of maternal multiple micronutrient supplementation on fetal loss and infant death in Indonesia: a double-blind cluster-randomised trial. Lancet 371:215–227
Tafti M, Ghyselinck NB (2007) Functional implication of the vitamin A signalling pathway in the brain. Arch Neurol 64:1706–1711
Tai M (1997) The devastating consequences of iodine deficiency. Southeast Asian J Trop Med Public Health 28(Suppl 2):75–77
Tamura T, Goldenberg RL, Freeberg LE, Cliver SP, Hoffman HJ (1992) Maternal serum folate and zinc concentrations and their relationship to pregnancy outcome. Am J Clin Nutr 56:365–370
Tamura T, Goldenberg RL, Hou J, Johnston KE, Cliver SP, Ramey SL, Nelson KG (2002) Cord serum ferritin concentrations and mental and psychomotor development of children at 5 years of age. J Pediatr 140:165–170
Tamura T, Goldenberg RL, Chapman VR, Johnston KE, Ramey SL, Nelson KG (2005) Folate status of mothers during pregnancy and mental and psychomotor development of their children at 5 years of age. Pediatrics 116:703–708
Thompson RA, Nelson CA (2001) Developmental science and the media. Early brain development Am Psychol 56:5–15
Uauy R, Kain J, Mericq V, Rojas J, Corvalán C (2008) Nutrition, child growth, and chronic disease prevention. Ann Med 40:11–20
Vazir S, Nagalla B, Thangiah V, Kamasamudram V, Bhattiprolu S (2006) Effect of micronutrient supplement on health and nutritional status of schoolchildren: mental function. Nutrition 22(Suppl 1):S26–S32
Vermiglo F, Lo Presti VP, Moleti M, Sidoti M, Tortorella G, Scaffidi G, Castagna MG, Mattina F, Violi MA, Crisa A, Artemisia A, Trimarchi F (2004) Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. J Clin Endocrinol Metab 89:6054–6060
von Schenck U, Bender-Gotze C, Koletzko B (1997) Persistence of neurological damage induced by dietary vitamin B-12 deficiency in infancy. Arch Dis Child 77:137–139
Walsh WJ, Isaacson HR, Rehman F, Hall A (1997) Elevated blood copper/zinc ratios in assaultive young males. Physiol Behav 62:327–329
Wang YY, Yang SH (1985) Improvement in hearing among otherwise normal schoolchildren in iodine-deficient areas of Guizhou, China, following use of iodized salt. Lancet 2:518–520
Wasantwisut E (1997) Nutrition and development: other micronutrients’ effect on growth and cognition. Southeast Asian J Trop Med Public Health 28(Suppl 2):78–82
West KP (2003) Vitamin A deficiency disorders in children and women. Food Nutr Bull 24(Suppl 4):S78–S90
Whitley JR, O’Dell BL, Hogan AG (1951) Effect of diet on maze learning in second-generation rats. J Nutr 45:153–160
Wu LL, Zhang L, Shao J, Qin YF, Yang RW, Zhao ZY (2008) Effect of perinatal iron deficiency on myelination and associated behaviours in rat pups. Behav Brain Res 188:263–270
Zeisel SH (2006) Choline: critical role during fetal development and dietary requirements in adults. Annu Rev Nutr 26:229–250
Zeisel SH (2006) The fetal origins of memory: the role of dietary choline in optimal brain development. J Pediatr 149(Suppl 5):S131–S136
Zeisel SH, Niculescu MD (2006) Perinatal choline influences brain structure and function. Nutr Rev 64:197–203
Zimmermann MB (2007) The adverse effects of mild-to-moderate iodine deficiency during pregnancy and childhood: a review. Thyroid 17: 829–835
Zimmermann MB, Connolly K, Bozo M, Bridson J, Rohner F, Grimci L (2006) Iodine supplementation improves cognition in iodine-deficient schoolchildren in Albania: a randomized, controlled, double-blind study. Am J Clin Nutr 83:108–114
Zimmermann M, Delange F (2004) Iodine supplementation of pregnant women in Europe: a review and recommendations. Eur J Clin Nutr 58:979–984
Acknowledgments
The authors would like to thank the reviewers Bonnie Kaplan and Joachim Westenhöfer for their useful comments and discussions. This work was commissioned by the Nutrition and Mental Performance Task Force of the European branch of the International Life Sciences Institute (ILSI Europe). Industry members of this task force are Barilla G.&R. Fratelli, Coca-Cola European Union Group, DSM, Groupe Danone, Kraft Foods, Nestlé, Südzucker/BENEO Group, Unilever and Wild Flavors. For further information about ILSI Europe, please call +32-2-771.00.14 or email info@ilsieurope.be. The opinions expressed herein are those of the authors and do not necessarily represent the views of ILSI Europe.
Conflict of interests The author has no financial or other interests that might conflict with the views expressed.
Author information
Authors and Affiliations
Consortia
Rights and permissions
About this article
Cite this article
Benton, D., ILSI Europe a.i.s.b.l.. Micronutrient status, cognition and behavioral problems in childhood. Eur J Nutr 47 (Suppl 3), 38–50 (2008). https://doi.org/10.1007/s00394-008-3004-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-008-3004-9