Abstract
Purpose
To prospectively evaluate the association of vitamin/mineral supplementation with cancer, cardiovascular, and all-cause mortality.
Methods
In the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Heidelberg), which was recruited in 1994–1998, 23,943 participants without pre-existing cancer and myocardial infarction/stroke at baseline were included in the analyses. Vitamin/mineral supplementation was assessed at baseline and during follow-up. Cox regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs).
Results
After an average follow-up time of 11 years, 1,101 deaths were documented (cancer deaths = 513 and cardiovascular deaths = 264). After adjustment for potential confounders, neither any vitamin/mineral supplementation nor multivitamin supplementation at baseline was statistically significantly associated with cancer, cardiovascular, or all-cause mortality. However, baseline users of antioxidant vitamin supplements had a significantly reduced risk of cancer mortality (HR: 0.52; 95% CI: 0.28, 0.97) and all-cause mortality (HR: 0.58; 95% CI: 0.38, 0.88). In comparison with never users, baseline non-users who started taking vitamin/mineral supplements during follow-up had significantly increased risks of cancer mortality (HR: 1.74; 95% CI: 1.09, 2.77) and all-cause mortality (HR: 1.58; 95% CI: 1.17, 2.14).
Conclusions
Based on limited numbers of users and cases, this cohort study suggests that supplementation of antioxidant vitamins might possibly reduce cancer and all-cause mortality. The significantly increased risks of cancer and all-cause mortality among baseline non-users who started taking supplements during follow-up may suggest a “sick-user effect,” which researchers should be cautious of in future observational studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Taking vitamin/mineral supplements is common in affluent countries. In Germany, a study in 1998 reported that 18% of men and 25% of women were regular users in a sample of population aged 18–79 years [1]. Nowadays the prevalence should be higher, particularly in elderly populations. Some epidemiological studies have investigated the effects of vitamin/mineral supplementation on cancer, cardiovascular disease (CVD), and all-cause mortality. However, the inconsistent findings obtained from these studies do not allow for drawing a clear conclusion. As reported by a US prospective cohort study, long-term daily use of multivitamin supplements was significantly inversely associated with CVD mortality [2], while in another cohort, this inverse association was not observed [3]. In the Cancer Prevention Study II (CPS-II), use of multivitamin plus vitamin A, C, and E was significantly inversely associated with all-cause mortality [4]. Nevertheless, multivitamin supplements alone did not show this beneficial effect in other studies [2, 5]. Surprisingly, two studies have observed a significantly increased risk of cancer mortality among male current smokers who took either multivitamin supplements or non-specific dietary supplements [4, 6], suggesting that vitamin/mineral supplements might be harmful for specific population groups.
In the present study, we evaluated the associations of vitamin/mineral supplementation with cancer, CVD, and all-cause mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Heidelberg).
Subjects and methods
Study population
The EPIC-Heidelberg cohort was recruited in 1994–1998. Detailed recruitment procedures have been described elsewhere [7]. This cohort eventually recruited 25,540 local residents, including 11,928 men (age range: 40–64 years) and 13,612 women (age range: 35–64 years). The Ethics Committee of the Heidelberg University Medical School approved the study protocol. Written informed consents were obtained from all participants. In the present study, we excluded participants who had a diagnosis of cancer (n = 953) or myocardial infarction (MI)/stroke (n = 678) at recruitment stage, leaving 23,943 participants (11,083 men and 12,860 women) for analysis.
Data collection
Assessment of vitamin/mineral supplementation and other exposures
In the EPIC-Heidelberg cohort, vitamin/mineral supplementation was assessed at different time points. In a baseline face-to-face interview, regular use of vitamin/mineral supplements was assessed by asking participants the following question: “Did you regularly take any medications or vitamin/mineral supplements in the last 4 weeks?,” where regular use was defined as daily use that lasted for ≥1 week or non-daily use of ≥5 doses at regular intervals. For participants who answered “yes,” brand names of the supplements were further asked for. In a baseline self-administered food frequency questionnaire (FFQ), participants were also asked whether they had taken vitamin/mineral supplements for ≥4 weeks in the last 12 months. These two baseline assessments produced a weighted Kappa coefficient of 0.87. Regular vitamin/mineral supplementation was reassessed in the 2nd (2001–2003) and the 3rd (2004–2006) self-administered follow-up questionnaire survey using the same definition of regular use as used in the baseline face-to-face interview. The present study analyzed the vitamin/mineral supplementation data from the baseline face-to-face interview. Supplementation data of the 2nd and the 3rd follow-up survey were also used to deal with the question of stability of supplementation. There was no data missing in the baseline face-to-face interview as all participants answered the supplement use question. In follow-up questionnaires, tick boxes that were left unmarked were considered as non-use. Dose data were not collected at all these occasions.
Intakes of 148 food and beverage items in the last 12 months before recruitment were measured using the baseline FFQ, which had been validated by twelve 24-h dietary recalls [8, 9]. Baseline demographic, lifestyle, and other health-related characteristics were measured in a baseline lifestyle questionnaire survey and a baseline physical examination.
Ascertainment of end points
Fatal status was identified by means of regular follow-up surveys. The underlying cause of death was verified by reviewing official death certificate and was coded using the International Classification of Diseases 10th version (ICD-10). In the present study, the end points of interest included cancer deaths (B21 and C00-C97), CVD deaths (I00-I99), and all-cause deaths.
Statistical analysis
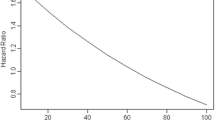
Age- and sex-adjusted baseline characteristics of non-users and users of any vitamin/mineral supplements were compared using analysis of covariance and logistic regression. We further classified any vitamin/mineral supplements into multivitamins, antioxidant vitamins (including vitamin A, C, E, and their combinations), and others. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using Cox proportional hazards models, in which age at recruitment and age at death (or age at the last contact in case of censoring) were used as separate time scales. In order to avoid violation of the proportional hazard assumption, age at recruitment (1-year category) was used as a strata variable. The following possible confounders, which were selected from baseline characteristics using the change-in-estimate method with the entry criterion being a 5% or greater alteration in the exposure-disease effect, were adjusted for: sex, educational level (no/primary, technical/secondary, and university), body mass index (BMI, kg/m2), waist-to-hip ratio, smoking category (never smokers; former smokers, quit ≥10 years, quit <10 years; and current smokers, ≤10, 11–20, >20 cigarettes/day), intake of meat/meat products (g/day), and baseline regular use of non-steroidal anti-inflammatory drugs (NSAIDs, yes/no). As important risk factors for cancer and CVD, physical activity (inactive, moderately inactive, moderately active, and active [10]) and total energy intake (kcal/day) were also adjusted for, although they slightly missed the entry criterion. For any vitamin/mineral supplementation, we also performed a 2-year lag analysis by excluding deaths that occurred in the first 2 years of follow-up and a stratified analysis by sex and smoking status (never, former, and current smoking).
To deal with the question of stability of supplement use during follow-up, we performed a sub-analysis of 19,873 participants who provided supplementation information at all three occasions, i.e. the baseline face-to-face interview, the 2nd and the 3rd follow-up survey. In this sub-analysis, participants were categorized into five groups: (1) never users, defined as participants who did not take vitamin/mineral supplements at all three occasions; (2) new users, defined as baseline non-users who started taking vitamin/mineral supplements during follow-up; (3) former users, defined as baseline users who stopped taking vitamin/mineral supplements during follow-up; (4) consistent users, defined as participants who took vitamin/mineral supplements at all three occasions; and (5) casual users, defined as participants who did not belong to any of the above groups. The sub-analysis counted the survival time from the date of the 3rd follow-up survey and used never users as the reference.
A two-sided p < 0.05 was considered as statistically significant. All analyses were performed with SAS software (version 9.2; SAS Institute, Cary, NC, USA).
Results
According to the face-to-face interview, 34.4% of the EPIC-Heidelberg cohort participants were regular users of any vitamin/mineral supplements. 56.3% of users provided the brand names of the supplements. Among them, multivitamins, with or without minerals, were the most commonly used supplements (28.6%), followed by antioxidant vitamins (18.1%). The prevalence of any vitamin/mineral supplementation kept increasing during follow-up (39.0% in the 2nd and 44.6% in the 3rd follow-up survey).
As shown in Table 1, users of any vitamin/mineral supplements were more likely to have some favorable health-related characteristic, such as having a university degree, being physically active, having a lower BMI and a generally healthier diet, which was indicated by higher intakes of fruits/vegetables and milk/milk products but a lower intake of meat/meat products. On the other hand, users were older than non-users and more likely. To be women and to have a longer smoking duration. Users of any vitamin/mineral supplements were also more likely to take antihypertensive drugs, lipid-lowering drugs, and NSAIDs.
After an average follow-up time of 11 years, 1,101 deaths were documented (cancer deaths = 513 and CVD deaths = 264). In both the age- and sex-adjusted models and the multivariate models, baseline any vitamin/mineral supplementation was not statistically significantly associated with cancer mortality or CVD mortality (Table 2). The association for all-cause mortality was significantly inverse in the age- and sex-adjusted model but attenuated to a non-significant level in the multivariate model. Excluding the deaths that occurred in the first 2 years of follow-up did not substantially change the results, and none of the null associations was modified by sex and smoking status (data not shown).
In multivariate models, multivitamin supplementation was not statistically significantly associated with any of the end points. Antioxidant vitamin supplementation was significantly inversely associated with cancer mortality (HR: 0.52; 95% CI: 0.28, 0.97) and all-cause mortality (HR: 0.58; 95% CI: 0.38, 0.88), but not with CVD mortality (Table 3).
In the sub-analysis, new users, i.e. baseline non-users who started taking supplements during follow-up, had a significantly increased risk of cancer mortality (HR: 1.74; 95% CI: 1.09, 2.77) and all-cause mortality (HR: 1.58; 95% CI: 1.17, 2.14; Table 4). After new users were further separated into new users of antioxidant vitamin supplements (n = 445) and new users of other supplements (n = 3,801), a HR for all-cause mortality of 1.23 (95% CI: 0.57, 2.66) was observed for the former and 1.63 (95% CI: 1.20, 2.21) for the latter. No statistically significant association was observed for cause-specific and all-cause mortality among former users and consistent users, although consistent users had a 50% lower risk of CVD mortality (95% CI: 0.22, 1.17). Among casual users, there was a positive yet not statistically significant association for cancer mortality and all-cause mortality.
Discussion
After an 11-year follow-up of the EPIC-Heidelberg cohort, regularly taking any vitamin/mineral supplements was not statistically significantly associated with cancer, CVD, or all-cause mortality. However, antioxidant vitamin supplementation was significantly inversely associated with cancer mortality and all-cause mortality. In comparison with never users, baseline non-users who started taking vitamin/mineral supplements during follow-up had significantly increased risks of cancer mortality and all-cause mortality.
Cancer mortality
The null association we observed between baseline any vitamin/mineral supplementation and cancer mortality supports the finding of a prior prospective cohort study of Swedish men, in which the investigated supplements were also non-specific [6]. However, we did not see a significantly increased risk of cancer mortality among any vitamin/mineral supplement users who were current smokers as observed in the Swedish male cohort [6]. The null association between multivitamin supplementation and cancer mortality in our cohort is in line with the findings of a cohort study and a randomized clinical trial [2, 11], but not consistent with the statistically significant positive association observed among men of CPS-II [4].
The potential anticancer property of antioxidant vitamins has been suggested by observational studies showing a reduced risk of cancer mortality due to high intakes of fruits and vegetables [12–15], which are abundant in antioxidant vitamins. However, whether antioxidant vitamins from supplements have a similar effect remains undetermined. Two meta-analyses of randomized clinical trials suggest no preventive effect of antioxidant vitamin supplements on cancer incidence or mortality [16, 17], which is not supported by the finding of the present study. In the present study, however, the small number of users of antioxidant vitamin supplements and lack of detailed information on dose, contents, and duration of use may weaken the convincingness of the observed beneficial effect.
Several studies have suggested a possible reverse causality between vitamin/mineral supplementation and cancer mortality by showing that cancer patients tend to take vitamin/mineral supplements after the diagnosis [18–20]. In addition, certain health problems before cancer diagnosis are also possible to lead to use of vitamin/mineral supplements, although this assumption has not been suggested by literatures. The significantly increased risk of cancer mortality we observed among new users was likely to be caused by such a reverse causality. As an attempt to remove this reverse causality, we excluded incident cancer cases that were diagnosed between the baseline and the date of the 3rd follow-up survey, and the association was attenuated to a non-significant level (HR: 1.60; 95% CI: 0.87, 2.94).
CVD mortality
The present study and the Swedish male cohort study [6] are in agreement on the null association between use of any vitamin/mineral supplements and CVD mortality. As for the association between multivitamin supplementation and CVD mortality, previous findings are conflicting. In a large cohort study, the Physicians’ Health Study, multivitamin supplementation was not statistically associated with CVD mortality [3]. In another cohort study, however, the association between multivitamin supplementation in a frequency of 6–7 days/week and CVD mortality was significant and inverse [6]. For antioxidant vitamin supplements, two clinical trials provided no evidence of association with CVD mortality [21, 22], although CPS-II observed an inverse association for ischaemic heart disease mortality [4].
In the sub-analysis, the statistically non-significant inverse association for CVD mortality among consistent users was based on an average follow-up time of 3.0 years and only seven CVD deaths. A future analysis based on a prolonged follow-up time and more CVD deaths might produce more convincing results.
All-cause mortality
Our finding of an inverse although statistically non-significant association between any vitamin/mineral supplementation and all-cause mortality does not fully support the null association observed in the Swedish male cohort (HR: 1.00; 95% CI: 0.90–1.11) [6]. Our finding also does not support the significant positive association between regular multivitamin supplementation and all-cause mortality in CPS-II [4]. However, that positive association observed in CPS-II is likely to be spurious because the study did not exclude baseline pre-existing CVD and cancer cases.
The significant inverse association between antioxidant vitamin supplementation and all-cause mortality in the EPIC-Heidelberg cohort is consistent with the finding of CPS-II [4]. However, two randomized clinical trials suggest that supplementation of beta-carotene or vitamin E in high dose may increase the risk of all-cause mortality in smokers [21, 23]. In the present study, we could not investigate such an adverse effect because of the fewness of antioxidant vitamin supplement users among current smokers (n = 171).
In the sub-analysis, the significantly increased risk of all-cause morality among new users of any vitamin/mineral supplements may suggest a “sick-user effect,” implying that initiation of supplementation during follow-up could be caused by the occurrence of certain health problems. The disparity in the strength of this positive association between new users of antioxidant vitamin supplements and new users of other supplements was possibly due to the potential beneficial effect of antioxidant vitamin supplements on all-cause mortality as suggested by the present study.
In observational studies, the validity of self-reported vitamin/mineral supplementation is difficult to measure, although some researchers used 24-h recall interviews or label transcriptions to identify “real users” [24, 25]. However, different definitions (regular use over weeks or months versus 24-h usage of supplements) make comparisons difficult. In the present study, we could compare two separate assessments at baseline, and the reliability of these self-reported vitamin/mineral supplementation data was high, as suggested by the weighted Kappa coefficient of 0.87. In the present study, we were unable to investigate the dose–response relationship because dose data were not available. Although 43.7% of supplement users did not provide the brand names of the supplements they took, it is unlikely that this causes substantial bias.
As vitamin/mineral supplementation is a changeable behavior among free-living individuals, prospective studies that only perform one single assessment at baseline may suffer from exposure misclassification. The present study assessed vitamin/mineral supplementation not only at baseline but also during follow-up; we thus were allowed to handle this changeable behavior by categorizing participants into various patterns according to their supplementation status at sequential time points. Nevertheless, it needs to be noted that, because the survival time in our sub-analysis was counted from the date of the last assessment, i.e., the 3rd follow-up survey, the average follow-up time of the sub-cohort was only 3.0 years, which is obviously not long enough to evaluate the exposure-disease associations for cancer and CVD.
In conclusion, this study provides no evidence that any vitamin/mineral or multivitamin supplementation may reduce the risks of cancer, CVD, or all-cause mortality. Based on limited numbers of users and cases, this study suggests that supplementation of antioxidant vitamins might possibly reduce cancer and all-cause mortality. The significantly increased risks of cancer and all-cause mortality among baseline non-users who started taking supplements during follow-up may suggest a “sick-user effect,” which researchers should be cautious of in future observational studies.
References
Beitz R, Mensink GB, Fischer B, Thamm M (2002) Vitamins–dietary intake and intake from dietary supplements in Germany. Eur J Clin Nutr 56(6):539–545
Pocobelli G, Peters U, Kristal AR, White E (2009) Use of supplements of multivitamins, vitamin C, and vitamin E in relation to mortality. Am J Epidemiol 170(4):472–483
Muntwyler J, Hennekens CH, Manson JE, Buring JE, Gaziano JM (2002) Vitamin supplement use in a low-risk population of US male physicians and subsequent cardiovascular mortality. Arch Intern Med 162(13):1472–1476
Watkins ML, Erickson JD, Thun MJ, Mulinare J, Heath CW Jr (2000) Multivitamin use and mortality in a large prospective study. Am J Epidemiol 152(2):149–162
Neuhouser ML, Wassertheil-Smoller S, Thomson C, Aragaki A, Anderson GL, Manson JE, Patterson RE, Rohan TE, van HL, Shikany JM, Thomas A, LaCroix A, Prentice RL (2009) Multivitamin use and risk of cancer and cardiovascular disease in the women’s health initiative cohorts. Arch Intern Med 169(3):294–304
Messerer M, Hakansson N, Wolk A, Akesson A (2008) Dietary supplement use and mortality in a cohort of Swedish men. Br J Nutr 99(3):626–631
Boeing H, Korfmann A, Bergmann MM (1999) Recruitment procedures of EPIC-Germany. European investigation into cancer and nutrition. Ann Nutr Metab 43(4):205–215
Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J (1997) Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the German part of the EPIC project. European prospective investigation into cancer and nutrition. Int J Epidemiol 26(Suppl 1):S59–S70
Bohlscheid-Thomas S, Hoting I, Boeing H, Wahrendorf J (1997) Reproducibility and relative validity of energy and macronutrient intake of a food frequency questionnaire developed for the German part of the EPIC project. European prospective investigation into cancer and nutrition. Int J Epidemiol 26(Suppl 1):S71–S81
Wareham NJ, Jakes RW, Rennie KL, Schuit J, Mitchell J, Hennings S, Day NE (2003) Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European prospective investigation into cancer and nutrition (EPIC) study. Public Health Nutr 6(4):407–413
Li JY, Taylor PR, Li B, Dawsey S, Wang GQ, Ershow AG, Guo W, Liu SF, Yang CS, Shen Q (1993) Nutrition intervention trials in Linxian, China: multiple vitamin/mineral supplementation, cancer incidence, and disease-specific mortality among adults with esophageal dysplasia. J Natl Cancer Inst 85(18):1492–1498
Genkinger JM, Platz EA, Hoffman SC, Comstock GW, Helzlsouer KJ (2004) Fruit, vegetable, and antioxidant intake and all-cause, cancer, and cardiovascular disease mortality in a community-dwelling population in Washington County, Maryland. Am J Epidemiol 160(12):1223–1233
Hertog MG, Bueno-de-Mesquita HB, Fehily AM, Sweetnam PM, Elwood PC, Kromhout D (1996) Fruit and vegetable consumption and cancer mortality in the caerphilly study. Cancer Epidemiol Biomarkers Prev 5(9):673–677
Sauvaget C, Nagano J, Hayashi M, Spencer E, Shimizu Y, Allen N (2003) Vegetables and fruit intake and cancer mortality in the Hiroshima/Nagasaki life span study. Br J Cancer 88(5):689–694
Colditz GA, Branch LG, Lipnick RJ, Willett WC, Rosner B, Posner BM, Hennekens CH (1985) Increased green and yellow vegetable intake and lowered cancer deaths in an elderly population. Am J Clin Nutr 41(1):32–36
Myung SK, Kim Y, Ju W, Choi HJ, Bae WK (2010) Effects of antioxidant supplements on cancer prevention: meta-analysis of randomized controlled trials. Ann Oncol 21(1):166–179
Bardia A, Tleyjeh IM, Cerhan JR, Sood AK, Limburg PJ, Erwin PJ, Montori VM (2008) Efficacy of antioxidant supplementation in reducing primary cancer incidence and mortality: systematic review and meta-analysis. Mayo Clin Proc 83(1):23–34
Ferrucci LM, McCorkle R, Smith T, Stein KD, Cartmel B (2009) Factors related to the use of dietary supplements by cancer survivors. J Altern Complement Med 15(6):673–680
Miller MF, Bellizzi KM, Sufian M, Ambs AH, Goldstein MS, Ballard-Barbash R (2008) Dietary supplement use in individuals living with cancer and other chronic conditions: a population-based study. J Am Diet Assoc 108(3):483–494
Velicer CM, Ulrich CM (2008) Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol 26(4):665–673
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, Keogh JP, Meyskens FL, Valanis B, Williams JH, Barnhart S, Hammar S (1996) Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 334(18):1150–1155
Heart protection study collaborative group (2002) MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360(9326):23–33
The alpha-tocopherol, beta-carotene cancer prevention study group (1994) The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med 330(15):1029–1035
Messerer M, Wolk A (2004) Sensitivity and specificity of self-reported use of dietary supplements. Eur J Clin Nutr 58(12):1669–1671
Satia-Abouta J, Patterson RE, King IB, Stratton KL, Shattuck AL, Kristal AR, Potter JD, Thornquist MD, White E (2003) Reliability and validity of self-report of vitamin and mineral supplement use in the vitamins and lifestyle study. Am J Epidemiol 157(10):944–954
Acknowledgments
This study was supported by the Deutsche Krebshilfe [Grant-No.: 70-488-Ha I] and the German Research Foundation, Graduiertenkolleg 793: Epidemiology of communicable and chronic noncommunicable diseases and their interrelationships.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, K., Kaaks, R., Linseisen, J. et al. Vitamin/mineral supplementation and cancer, cardiovascular, and all-cause mortality in a German prospective cohort (EPIC-Heidelberg). Eur J Nutr 51, 407–413 (2012). https://doi.org/10.1007/s00394-011-0224-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-011-0224-1