Abstract
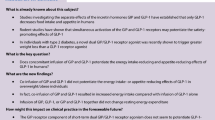
Background
The nutritional control of ghrelin has not been fully clarified yet. Particularly, the influence of aminoacids and lipids is controversial and, moreover, whether the intraluminal gastric contact with nutrients is required or if the modulatory action of nutrients on ghrelin secretion is mediated by insulin is still matter of debate.
Aim of the study
To clarify the role of nutrients in the control of ghrelin secretion evaluating the effects of intravenous and oral lipids and aminoacids compared with glucose and fructose load in healthy subjects.
Methods
A total of 6 healthy overnight-fasted volunteers underwent the following testing sessions: (a) iv arginine (ARG, 0.5 g/kg); (b) oral protein load (PRO, 50 g); (c) iv lipid-heparin infusion (Li He, Intralipid 10% 250 ml); (d) oral fat load (OIL, soy oil 40 g); (e) oral glucose load (OGL, 100 g); (f) oral fructose load (OFL, 100 g); (g) iv saline (SAL, 3 ml); (h) oral water load (WL, 200 ml). Total ghrelin, insulin, and glucose were assayed every 15 min from 0 up to +180 min.
Results
WL and SAL did not modify insulin, glucose and ghrelin. ARG induced a prompt but transient increase (P < 0.05) of insulin and glucose (P < 0.01), without modifying ghrelin secretion. PRO induced a mild but sustained increase of insulin secretion (P < 0.05) without affecting glucose and ghrelin. Li-He progressively increased circulating glucose (P < 0.01) without modifying insulin and ghrelin secretion. No significant variations in circulating glucose, insulin, and ghrelin occurred after OIL. OGL significantly (P < 0.01) increased insulin and glucose levels and progressively decreased (P < 0.05) ghrelin levels. OFL induced a mild (P < 0.05) increase of insulin without modifying glucose levels. Similarly, OFL was followed by a milder decrease (P < 0.05) of ghrelin levels.
Conclusions
Differently from carbohydrates and independently from their modulatory effect on insulin secretion and glucose levels, both lipids and aminoacids play a negligible role in the acute control of ghrelin secretion either after acute enteral and parenteral administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ghrelin is a 28-amino acid peptide predominantly produced by the stomach although a remarkable expression has also been detected in several other central and peripheral endocrine and non-endocrine tissues [1, 2].
Both in animals and in humans, ghrelin circulates in the bloodstream in two different forms endowed with different biological properties [1, 2]. When acylated in serine 3, ghrelin binds with high affinity the GH secretagogues receptor type 1a (GHS-R1a), the activation of which mediates ghrelin’s well-known GH-releasing effect but also other endocrine and non-endocrine actions among which a profound influence on energy metabolism via the hypothalamic modulation of appetite but also at the peripheral level by influencing the endocrine pancreatic function as well as glucose and lipid metabolism [1, 2].
In adulthood, circulating total ghrelin levels mostly reflect gastric secretion [3]. In rats, ghrelin secretion occurs following a pulsatile pattern that is not strictly correlated with GH levels but is markedly influenced by food intake episodes [4]. Similarly, in humans, ghrelin secretion undergoes circadian variations with superimposed remarkable transient decreases after meals [5, 6].
The physiological mechanisms accounting for the meal-induced inhibition of ghrelin secretion have been extensively investigated, but not fully clarified yet. Specifically, the involvement of several factors has been described, including the central activation of the cephalic phase of appetite [7, 8], the caloric content of the ingested meals [9, 10], the glycemic content of nutrients as well as the insulin responses to food intake [5, 11–13], and even several neuro-hormonal intestinal signals [14, 15].
Among all these factors, the direct role of nutrients and of their intraluminal contact with ghrelin-secreting gastric mucosa have obviously been investigated though without definitive results [16–18].
In particular, it is at present unknown whether the signals mediating the meal-related inhibition of ghrelin secretion originate from the gastrointestinal tract or from postabsorptive sites [16–18]. Although parenteral nutrients and/or insulin infusion can suppress ghrelin levels when administered for prolonged periods or at supraphysiological doses both in animals and in humans [13, 19–22], physiological doses that mimic postprandial fluctuations do not modify ghrelin in humans [23, 24]. In contrast, enteral nutrients consistently suppress ghrelin levels, even at low doses [25].
Both after oral and intravenous administration, carbohydrates, mainly glucose, represent one of the most potent inhibitory inputs on ghrelin secretion [21, 22, 26]. In fact, in experimental conditions of prolonged glucose- or fructose-enriched diets, glucose has been shown to inhibit ghrelin secretion more potently than fructose, that on its turn exerts a significantly milder impact also on insulin and glucose levels [26]. On the other hand, discordant results have been reported on the role of lipids and proteins [12, 20, 27–33].
Based on these data, aim of our study was to further investigate the role of lipids and proteins in the regulation of ghrelin secretion in humans, in particular evaluating the potential role of the direct intraluminal contact of nutrients with gastrointestinal mucosa. In particular the effects of intravenous arginine, known as the most potent aminoacid insulin secretagogue [34, 35], administered at a dose commonly used to explore insulin and GH secretion in clinical practice [35] have been compared with those of oral mixed aminoacid load, to mimic aminoacid meal content. Moreover, the effects of intravenous lipid-heparin emulsion and of oral soy oil, characterized by similar free fatty acids content, have been also evaluated. The effects of glucose and fructose loads have been studied as positive controls.
Subjects and methods
A total of 6 healthy young male volunteers (age [mean ± SEM]: 28.3 ± 3.1 year; body mass index: 21.9 ± 0.9 kg/m2] were studied. All the subjects gave their written informed consent to participate to the study, which had been approved by an independent Ethical Committee.
All the subjects underwent the following testing sessions in random order at least 7 days apart:
-
a)
iv arginine (ARG, 0.5 g/kg from 0 min to + 30 min; 150 kcal) (Table 1);
-
b)
oral amino acids load [Protifar, Nutricia, The Netherlands (PRO), 50 g at 0 min; 180 kcal] (Table 1);
-
c)
iv lipid-heparin infusion (Li He, Intralipid 10% 250 ml from 0 min to +120 min; 275 kcal) (Table 1);
-
d)
oral lipid load (OIL, soy oil 40 g at 0 min; 360 kcal) (Table 1);
-
e)
oral glucose load (OGL, 100 g at 0 min; 400 kcal)
-
f)
oral fructose load (OFL, 100 g at 0 min; 400 kcal)
-
g)
saline (SAL, 3 ml iv at 0 min as a bolus); and
-
h)
oral water load (WL, 200 ml at 0 min).
All the tests began at 08:30–09:00 h after an overnight fasting. An indwelling catheter has been placed into a forearm antecubital vein, kept patent by the slow infusion of isotonic saline. Blood samples were taken every 15 min from 0 up to +180 min in order to assay total ghrelin, insulin, and glucose levels.
During all the tests, all the subjects remained seated and no physical exercise, smoking, or other food or water ingestion was allowed till the end of the testing sessions.
Plasma total ghrelin levels (pg/ml) were assayed, after extraction in reverse phase C18 columns, by an immunoradiometric assay (Phoenix Pharmaceuticals, Inc., Belmont, CA) using 125I-labeled bioactive ghrelin as a tracer and a rabbit polyclonal antibody vs. octanoylated and des-octanoylated h-ghrelin. The sensitivity of the assay was 30 pg/tube and the intra-assay coefficient of variation (CV) range was 0.3–10.7%.
Serum insulin levels (mU/l; 1 mU/l = 7.175 pmol/l) were measured in duplicate by radioimmunometric assay (INSIK-5, SORIN Biomedica, Saluggia, Italy). The sensitivity of the assay was 2.5 ± 0.3 mU/l. The inter- and intra-assay CVs were 6.2–10.8% and 5.5–10.6%, respectively.
Plasma FFA levels (mmol/l) were measured by enzymatic analysis using the “NEFA C ACS-ACOD Method” kit provided by Wako Chemicals GmbH (Neuss, Germany).
Plasma glucose levels (mg/dl; 1 mg/dl = 0.05551 mmol/l) were measured by gluco-oxidase colorimetric assay (GLUCOFIX, by Menarini Diagnostici, Firenze, Italy).
All samples from an individual subject were analyzed together.
The hormonal responses are expressed as delta absolute variations.
The statistical analysis was carried out using a non-parametric ANOVA (Friedman test) and then Wilcoxon test, as appropriate.
The results are expressed as mean ± SEM.
Results
Baseline glucose, insulin, and total ghrelin levels were similar in all the testing sessions (Table 2).
Either WL or SAL did not modify fasting insulin (mean Δ variation [mean ± SEM]: −0.4 ± 1.2 and −0.3 ± 1.3 mU/l), glucose (mean Δ variation: −2.0 ± 1.4 and −1.3 ± 1.4 mg/dl), FFA (mean Δ variation: −0.1 ± 0.06 and 0.0 ± 0.05 mmol/l), and ghrelin (mean Δ variation: 20.3 ± 13.2 and 8.1 ± 6.2 pg/ml) levels (Figs. 1, 2).
ARG induced a prompt but transient increase (P < 0.05) of insulin levels peaking at 30 min (Δ peak: 33.6 ± 13.5 mU/l) coupled with a transient increase in glucose levels (Δ peak at 30 min: 7.9 ± 4.8 mg/dl; P < 0.01) (Fig. 1). On the other hand, ARG did not induce any significant variation of ghrelin levels (mean Δ variation: 9.7 ± 7.1 pg/ml) (Fig. 1).
PRO induced a mild but sustained increase (P < 0.05) in insulin levels (mean Δ variation: 6.1 ± 0.7 mU/l) (Fig. 1). On the other hand, PRO administration did not modify either glucose (mean Δ variation: −2.7 ± 1.0 mg/dl) or ghrelin (mean Δ variation: 10.6 ± 23.0 pg/ml) levels (Fig. 1).
As expected Li-He infusion increased FFA levels (mean Δ variation: 2.9 ± 0.6 mg/dl; Δ peak at 150’: 5.4 ± 0.6 mmol/l; P < 0.01) and induced a progressive increase in circulating glucose levels (mean Δ variation: 14.4 ± 4.4 mg/dl; Δ peak at 150’: 20.5 ± 7.6 mU/l; P < 0.01) without significantly modifying insulin levels (mean Δ variation: −2.1 ± 2.9 mU/l) (Fig. 2). Similarly, no significant variations in term of ghrelin levels occurred after Li-He infusion (mean Δ variation: 6.8 ± 11.4 pg/ml).
On the other hand, despite a still significant (P < 0.05) although less pronounced (P < 0.01 vs. Li He) increase of FFA levels (mean Δ variation: 0.5 ± 0.09 mmol/l; Δ peak at 150 min: 1.3 ± 0.06 mmol/l), no significant variations in circulating glucose (mean Δ variation: −0.03 ± 1.3 mg/dl), insulin (mean Δ variation: −0.8 ± 1.6 mU/l), and ghrelin (mean Δ variation: 3.8 ± 21.1 pg/ml) levels were observed after OIL (Fig. 2).
Oral glucose load induced a significant (P < 0.01) increase in insulin (mean Δ variation: 46.7 ± 5.8 mU/l; Δ peak at 30 min: 97.9 ± 8.4 mU/l) and glucose (mean Δ variation: 16.3 ± 2.2 mg/dl; Δ peak at 30 min: 60.5 ± 7.9 mg/dl) levels. After OGL a progressive decrease (P < 0.05) of ghrelin levels was also observed (mean Δ variation: −84.5 ± 51.7 pg/ml) (Fig. 3).
Oral fructose load induced a mild but significant (P < 0.05) increase of insulin levels (mean Δ variation: 9.3 ± 1.3 mU/l) without modifying glucose (mean Δ variation: −2.2 ± 0.6 mg/dl). After OFL a significant (P < 0.05) transient decrease of ghrelin levels was observed (mean Δ variation: −32.1 ± 23.6 pg/ml) (Fig. 3).
The insulin response to OGL was remarkably higher (P < 0.05) than that to ARG, that, in turn was higher (P < 0.05) than that induced by OFL. Similarly the inhibitory effect of OGL on circulating ghrelin levels were significantly more potent than that induced by OFL.
Notably, however, no correlation was found between insulin or glucose and total ghrelin levels after each stimulus.
Discussion
Ghrelin, in its acylated form, is an endogenous ligand of the GHS-R1a that is under intensive investigation due to its tight relationship with feeding behavior and energy metabolism [1, 2]. Consistently with the tight link between nutritional status and ghrelin, its circulating levels are decreased by food intake and overfeeding [5, 6].
Notably, however, despite metabolic and nutritional signals clearly turned out to be the most consistent modulators of ghrelin secretion in humans [1, 2], the exact mechanisms mediating the nutritional regulation of ghrelin secretion are still largely unknown [13, 23, 36, 37].
Based on these data, aim of our study has been to compare for the first time in humans the acute effects of either intravenous and oral lipids and aminoacids on circulating ghrelin levels in the same subjects. To this aim, in separate sessions we tested the effects of oral mixed pure aminoacid load, mimicking aminoacid meal content, compared with intravenous arginine, known as the most potent aminoacid insulin secretagogue [34, 35], administered at a dose commonly used to explore insulin and GH secretion in clinical practice [35] and, then, the effects of soy oil, as commonly used nutritional component, with intravenous lipid-heparin emulsion, characterized by similar free fatty acids content. The effects of glucose and fructose loads have been also studied as positive controls.
The results we obtained show that, at least after acute administration, differently from carbohydrates, both lipids and amino acids do not modify total ghrelin levels and no significant differences occur after enteral or parenteral administration.
Our findings are apparently in contrast with some (but not all [20, 33]) other studies reporting that in humans oral fat administration is able to mildly decrease [27, 28, 30, 32], or to increase [12] circulating ghrelin levels. Similarly, oral protein intake has been variably reported either to increase [12, 27] and not to affect [29, 31] circulating ghrelin levels.
The explanations for these differences are not obvious and several hypothesis could be considered.
First, in contrast with our study in which we tested the effect of pure lipid or protein load, some of the studies in the literature have been performed using mixed protein-enriched or lipid-enriched meals in which the carbohydrates content was not negligible (>5%) [28, 32].
Since a dose-response curve of carbohydrates on ghrelin secretion has never been performed so far, it is theoretically possible that even low carbohydrates doses in mixed meals could play a significant inhibitory role on ghrelin secretion [25].
On the other hand, other studies reported a late stimulatory effect of oral proteins on ghrelin secretion occurring 210 min [29] or 300 min [31] after the ingestion. This time curse would suggest that such stimulatory action on ghrelin secretion could be expression of an indirect metabolic response to amino acid absorption rather than a direct effect.
As expected, both aminoacids and lipid loads induced a remarkable metabolic impact. In fact, both oral amino acids load and even more intravenous arginine strongly stimulated insulin secretion and increased circulating glucose levels likely as the results of the well-known concomitant direct stimulatory effect of arginine on glucagon secretion [38]. On the other hand, free fatty acids infusion induced a remarkable progressive increase of glucose levels, due to the effects of free fatty acids on the inhibition of insulin-stimulated glucose uptake and glycogen synthesis as well as of insulin suppression of endogenous glucose production [39, 40].
Interestingly, however, despite this remarkable impact on insulin and glucose levels, neither aminoacids nor free fatty acids administrations were coupled with significant variations of circulating ghrelin levels. This finding is of particular interest also taking into account that no effect was recorded both after oral and also after intravenous administration despite obvious differences in administration profile and bioavailability. In particular both intravenous lipid-heparin emulsion and arginine administration given as continuous infusion instead of acute bolus for safety reasons, were devoid of any modulatory effect on ghrelin secretion as the oral loads, despite an even stronger impact on insulin and glucose levels, in particular after arginine, known as the most potent aminoacid insulin secretagogue [34, 35]
On the other hand, as previously reported in experimental conditions of prolonged high fructose diet, also in our acute experimental conditions, fructose exerts a mild but still significant inhibitory effect on ghrelin secretion, despite its insulin-secreting effects is lower than that of arginine, that, in turn, as reported above does not modify ghrelin secretion.
Therefore, these data further question the existence of a univocal relationship between insulin or glucose and ghrelin and suggest that the acute nutritional control of ghrelin secretion is regulated by a multifactorial system not simply directly related to glucose metabolism.
In conclusions, the results of the present study show that independently from their modulatory effect on insulin secretion and glucose levels, both lipids and amino acids play a negligible role in the acute control of ghrelin secretion either after acute enteral or parenteral administration. Consistently with the milder impact on insulin and glucose levels, among carbohydrates, fructose exerts a less potent inhibitory effect on ghrelin secretion than glucose.
References
Ghigo E, Broglio F, Arvat E, Maccario M, Papotti M, Muccioli G (2005) Ghrelin: more than a natural GH secretagogue and/or an orexigenic factor. Clin Endocrinol (Oxf) 62:1–17
Kojima M, Kangawa K (2005) Ghrelin: structure and function. Physiol Rev 85:495–522
Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, Suda M, Koh T, Natsui K, Toyooka S, Shirakami G, Usui T, Shimatsu A, Doi K, Hosoda H, Kojima M, Kangawa K, Nakao K (2001) Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab 86:4753–4758
Tolle V, Bassant MH, Zizzari P, Poindessous-Jazat F, Tomasetto C, Epelbaum J, Bluet-Pajot MT (2002) Ultradian rhythmicity of ghrelin secretion in relation with GH, feeding behavior, and sleep-wake patterns in rats. Endocrinology 143:1353–1361
Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS (2001) A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 50:1714–1719
Tschop M, Wawarta R, Riepl RL, Friedrich S, Bidlingmaier M, Landgraf R, Folwaczny C (2001) Post-prandial decrease of circulating human ghrelin levels. J Endocrinol Invest 24:RC19–RC21
Arosio M, Ronchi CL, Beck-Peccoz P, Gebbia C, Giavoli C, Cappiello V, Conte D, Peracchi M (2004) Effects of modified sham feeding on ghrelin levels in healthy human subjects. J Clin Endocrinol Metab 89:5101–5104
Simonian HP, Kresge KM, Boden GH, Parkman HP (2005) Differential effects of sham feeding and meal ingestion on ghrelin and pancreatic polypeptide levels: evidence for vagal efferent stimulation mediating ghrelin release. Neurogastroenterol Motil 17:348–354
Callahan HS, Cummings DE, Pepe MS, Breen PA, Matthys CC, Weigle DS (2004) Postprandial suppression of plasma ghrelin level is proportional to ingested caloric load but does not predict intermeal interval in humans. J Clin Endocrinol Metab 89:1319–1324
Le Roux CW, Patterson M, Vincent RP, Hunt C, Ghatei MA, Bloom SR (2005) Postprandial plasma ghrelin is suppressed proportional to meal calorie content in normal-weight but not obese subjects. J Clin Endocrinol Metab 90:1068–1071
Blom WA, Stafleu A, de GC, Kok FJ, Schaafsma G, Hendriks HF (2005) Ghrelin response to carbohydrate-enriched breakfast is related to insulin. Am J Clin Nutr 81:367–375
Erdmann J, Topsch R, Lippl F, Gussmann P, Schusdziarra V (2004) Postprandial response of plasma ghrelin levels to various test meals in relation to food intake, plasma insulin, and glucose. J Clin Endocrinol Metab 89:3048–3054
Murdolo G, Lucidi P, Di LC, Parlanti N, De CA, Fatone C, Fanelli CG, Bolli GB, Santeusanio F, De FP (2003) Insulin is required for prandial ghrelin suppression in humans. Diabetes 52:2923–2927
Batterham RL, Cohen MA, Ellis SM, Le Roux CW, Withers DJ, Frost GS, Ghatei MA, Bloom SR (2003) Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med 349:941–948
Cohen MA, Ellis SM, Le Roux CW, Batterham RL, Park A, Patterson M, Frost GS, Ghatei MA, Bloom SR (2003) Oxyntomodulin suppresses appetite and reduces food intake in humans. J Clin Endocrinol Metab 88:4696–4701
Overduin J, Frayo RS, Grill HJ, Kaplan JM, Cummings DE (2005) Role of the duodenum and macronutrient type in ghrelin regulation. Endocrinology 146:845–850
Parker BA, Doran S, Wishart J, Horowitz M, Chapman IM (2005) Effects of small intestinal and gastric glucose administration on the suppression of plasma ghrelin concentrations in healthy older men and women. Clin Endocrinol (Oxf) 62:539–546
Williams DL, Cummings DE, Grill HJ, Kaplan JM (2003) Meal-related ghrelin suppression requires postgastric feedback. Endocrinology 144:2765–2767
Lucidi P, Murdolo G, Di LC, De CA, Parlanti N, Fanelli C, Santeusanio F, Bolli GB, De FP (2002) Ghrelin is not necessary for adequate hormonal counter regulation of insulin-induced hypoglycemia. Diabetes 51:2911–2914
Mohlig M, Spranger J, Otto B, Ristow M, Tschop M, Pfeiffer AF (2002) Euglycemic hyperinsulinemia, but not lipid infusion, decreases circulating ghrelin levels in humans. J Endocrinol Invest 25:RC36–RC38
Nakagawa E, Nagaya N, Okumura H, Enomoto M, Oya H, Ono F, Hosoda H, Kojima M, Kangawa K (2002) Hyperglycaemia suppresses the secretion of ghrelin, a novel growth-hormone-releasing peptide: responses to the intravenous and oral administration of glucose. Clin Sci (Lond) 103:325–328
Shiiya T, Nakazato M, Mizuta M, Date Y, Mondal MS, Tanaka M, Nozoe S, Hosoda H, Kangawa K, Matsukura S (2002) Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J Clin Endocrinol Metab 87:240–244
Schaller G, Schmidt A, Pleiner J, Woloszczuk W, Wolzt M, Luger A (2003) Plasma ghrelin concentrations are not regulated by glucose or insulin: a double-blind, placebo-controlled cross- over clamp study. Diabetes 52:16–20
Caixas A, Bashore C, Nash W, Pi-Sunyer F, Laferrere B (2002) Insulin, unlike food intake, does not suppress ghrelin in human subjects. J Clin Endocrinol Metab 87:1902
Gottero C, Bellone S, Rapa A, Van KP, Vivenza D, Prodam F, Benso A, Destefanis S, Gauna C, Bellone J, Hofland L, Van Der Lely AJ, Bona G, Ghigo E, Broglio F (2003) Standard light breakfast inhibits circulating ghrelin level to the same extent of oral glucose load in humans, despite different impact on glucose and insulin levels. J Endocrinol Invest 26:1203–1207
Teff KL, Elliott SS, Tschop M, Kieffer TJ, Rader D, Heiman M, Townsend RR, Keim NL, D’Alessio D, Havel PJ (2004) Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J Clin Endocrinol Metab 89:2963–2972
Erdmann J, Lippl F, Schusdziarra V (2003) Differential effect of protein and fat on plasma ghrelin levels in man. Regul Pept 116:101–107
Greenman Y, Golani N, Gilad S, Yaron M, Limor R, Stern N (2004) Ghrelin secretion is modulated in a nutrient- and gender-specific manner. Clin Endocrinol (Oxf) 60:382–388
Groschl M, Knerr I, Topf HG, Schmid P, Rascher W, Rauh M (2003) Endocrine responses to the oral ingestion of a physiological dose of essential amino acids in humans. J Endocrinol 179:237–244
Heath RB, Jones R, Frayn KN, Robertson MD (2004) Vagal stimulation exaggerates the inhibitory ghrelin response to oral fat in humans. J Endocrinol 180:273–281
Knerr I, Groschl M, Rascher W, Rauh M (2003) Endocrine effects of food intake: insulin, ghrelin, and leptin responses to a single bolus of essential amino acids in humans. Ann Nutr Metab 47:312–318
Monteleone P, Bencivenga R, Longobardi N, Serritella C, Maj M (2003) Differential responses of circulating ghrelin to high-fat or high-carbohydrate meal in healthy women. J Clin Endocrinol Metab 88:5510–5514
Poppitt SD, Leahy FE, Keogh GF, Wang Y, Mulvey TB, Stojkovic M, Chan YK, Choong YS, McArdle BH, Cooper GJ (2005) Effect of high-fat meals and fatty acid saturation on postprandial levels of the hormones ghrelin and leptin in healthy men. Eur J Clin Nutr 60:77–84
van Haeften TW, Voetberg GA, Gerich JE, van der V (1989) Dose-response characteristics for arginine-stimulated insulin secretion in man and influence of hyperglycemia. J Clin Endocrinol Metab 69:1059–1064
Gannon MC, Nuttall JA, Nuttall FQ (2002) Oral arginine does not stimulate an increase in insulin concentration but delays glucose disposal. Am J Clin Nutr 76:1016–1022
Briatore L, Andraghetti G, Cordera R (2003) Acute plasma glucose increase, but not early insulin response, regulates plasma ghrelin. Eur J Endocrinol 149:403–406
Spranger J, Ristow M, Otto B, Heldwein W, Tschop M, Pfeiffer AF, Mohlig M (2003) Post-prandial decrease of human plasma ghrelin in the absence of insulin. J Endocrinol Invest 26:RC19–RC22
Palmer JP, Walter RM, Ensinck JW (1975) Arginine-stimulated acute phase of insulin and glucagon secretion. I. in normal man. Diabetes 24:735–740
Homko CJ, Cheung P, Boden G (2003) Effects of free fatty acids on glucose uptake and utilization in healthy women. Diabetes 52:487–491
Ferrannini E, Barrett EJ, Bevilacqua S, DeFronzo RA (1983) Effect of fatty acids on glucose production and utilization in man. J Clin Invest 72:1737–1747
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prodam, F., Me, E., Riganti, F. et al. The nutritional control of ghrelin secretion in humans. Eur J Nutr 45, 399–405 (2006). https://doi.org/10.1007/s00394-006-0613-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-006-0613-z