Abstract
Objective
To assess cartilage oligomeric matrix protein (COMP) levels in serum and synovial fluid in patients with early and established rheumatoid arthritis (RA), and to correlate the levels with clinical, laboratory and radiological characteristics.
Patients and methods
The study included 24 female RA patients. Full medical history was taken, thorough clinical examination and laboratory investigations performed, and body mass index (BMI) recorded. Radiological damage was assessed according to the modified Larsen score. Disease activity score 28 (DAS28) was calculated. The control group comprised 30 age- and gender-matched healthy subjects. Serum and synovial COMP levels were determined by enzyme-linked immunosorbent assay (ELISA).
Results
Mean patient age was 44.04 ± 10.5 years. Of the 24 patients, 12 had early RA and 12 had established disease with joint destruction; 5 of each group had knee effusion. Serum COMP was significantly higher in patients (19.54 ± 5.47 µg/ml) compared to controls (5.93 ± 1.95 µg/ml; p < 0.001) and was also significantly higher in patients with established disease (23.9 ± 3.1 µg/ml) compared to those in early stages (15.1 ± 3.2 µg/ml; p < 0.001). Synovial COMP was also significantly increased in established compared to early-stage RA (31.2 ± 9.8 µg/ml vs. 51.6 ± 10.4 µg/ml; p = 0.013). Serum and synovial COMP significantly correlated with age, disease duration, BMI, DAS28 and modified Larsen score. On performing regression analysis in RA patients, only BMI could predict the serum level of COMP (p = 0.02).
Conclusion
COMP is a promising biomarker for disease activity in RA, making it a potential therapeutic target. The obvious correlation with the BMI throws light on the importance of weight control not only in osteoarthritis (OA), but also in RA.
Zusammenfassung
Ziel
Die COMP(oligomeres Knorpelmatrixprotein)-Konzentrationen im Serum und in der Synovialflüssigkeit von Patienten mit früher und mit etablierter rheumatoider Arthritis (RA) sollten bestimmt und auf mögliche Beziehungen zu klinischen, laborchemischen und radiologischen Charakteristika untersucht werden.
Patienten und Methoden
In die Studie aufgenommen wurden 24 RA-Patienten. Eine ausführliche Anamnese wurde erhoben, gründliche klinische und laborchemische Untersuchungen wurden durchgeführt und der BMI (Body-Mass-Index) dokumentiert. Radiologisch sichtbare Schädigungen wurden bestimmt anhand des modifizierten Larsen-Scores, der DAS (Disease Activity Score) 28 wurde errechnet. Die Kontrollgruppe bestand aus 30 alters- und geschlechtsgematchten gesunden Personen. Serum- und synoviale COMP-Konzentrationen wurden mittels ELISA („enzyme-linked immunosorbent assay“) gemessen.
Ergebnisse
Das Durchschnittsalter der Patienten lag bei 44,04 ± 10,5 Jahren. Von 24 Patienten litten 12 an früher und 12 an etablierter RA mit Gelenkzerstörung, einen Kniegelenkerguss hatten jeweils 5 Patienten in jeder Gruppe. COMP im Serum war in der Patientengruppe höher als in der Kontrollgruppe (19,54 ± 5,47 vs. 5,93 ± 1,95 µg/ml; p < 0,001) und auch signifikant höher bei Patienten mit länger bestehender Erkrankung (23,9 ± 3,1 µg/ml) im Vergleich zu denen mit RA in frühen Stadien (15,1 ± 3,2 µg/ml; p < 0,001). Im Vergleich zu letztgenannten waren auch die synovialen COMP-Konzentrationen signifikant erhöht bei Patienten mit etablierter RA (31,2 ± 9,8 vs. 51,6 ± 10,4 µg/ml; p = 0,013). Serum- und synoviale COMP-Konzentrationen korrelierten signifikant mit Alter, Erkrankungsdauer, BMI, DAS28 und modifiziertem Larsen-Score. Die Regressionsanalyse der RA-Patienten-Werte ergab, dass eine Vorhersage der Serum-COMP-Werte nur anhand des BMI möglich war (p = 0,02).
Schlussfolgerung
COMP ist ein viel versprechender Biomarker für die Krankheitsaktivität bei RA und damit ein potenzielles therapeutisches Target. Die offensichtliche Korrelation mit dem BMI wirft ein Schlaglicht darauf, wie entscheidend die Kontrolle des Körpergewichts ist – nicht nur bei Arthrose, sondern auch bei RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Advances in the understanding of the pathogenesis of rheumatoid arthritis (RA) have led to identification of novel cellular and molecular therapeutic targets [1]. Many factors and processes were implicated in the pathogenesis of RA including cytokine overproduction [2] and oxidative stress [3]. Despite the clinical success of anti-tumor necrosis factor (TNF) therapy for RA, there is still a need for therapeutic strategies that prevent extensive cartilage and bone loss [4]. Advances in the treatment of RA-related cartilage destruction require profound insights into the molecular mechanisms involved in cartilage degradation [5].
Cartilage oligomeric matrix protein (COMP) is a major non-collagenous component of cartilage [6], which accounts for approximately 1 % of the wet weight of articular tissue. COMP fragments have been detected in the cartilage, synovial fluid and serum of patients with knee injuries, osteoarthritis (OA) and RA [7]. The role of COMP in Egyptian patients with OA has been reported [8, 9, 10].
Monoclonal antibodies to COMP contribute to the development of arthritis [6]. In RA, COMP has a pathogenetic role independent of the mechanisms regulating inflammatory processes [11] and is involved in the regeneration efforts of cartilage tissue matrix breakdown [12]. Elevation of COMP may reflect joint damage that is dependent on the synovial inflammatory process in early-stage RA in the subset of patients with high serum C-reactive protein (CRP), matrix metalloproteinase-3 and MRI-proven bone erosion [13]. The high diagnostic specificity of COMP for RA patients with early joint inflammation has been reported. Raised serum COMP levels indicated cartilage involvement in both self-limiting and non-erosive disease [14]. The performance of COMP as a biomarker that can predict radiographic progression in early RA was comparable to traditional markers [15].
The potential use of COMP as a marker for measuring not only articular cartilage damage but also therapeutic efficacy in RA has been demonstrated [16]. Low (< 10 µg/ml) serum COMP prior to starting anti-TNF-α treatment predicts a rapid (within 3 months) and high response in RA [17].
The aim of the present work was to assess COMP levels in serum and synovial fluid in patients with early and established rheumatoid arthritis (RA), and correlate the levels with clinical, laboratory and radiological characteristics.
Patients and methods
Patients
A total of 24 female RA patients diagnosed according to the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) RA classification criteria [18] were consecutively recruited from the rheumatology outpatient clinics and departments of Cairo University Hospitals. Full medical history was taken, and thorough clinical examination and laboratory investigations were performed for all patients. Radiological grading of the hands and feet of the studied RA patients was assessed according to the modified Larsen score [19]. The body mass index (BMI) was recorded for all patients. The control group comprised 30 healthy age- and gender-matched subjects. Patients or controls known to have OA or any other rheumatic disease were excluded. The study was approved by the local university ethical committee and the study conforms to the provisions of the Declaration of Helsinki, 1995. All patients gave informed consent prior to their inclusion in the study.
Disease severity and COMP assay
Based on juxta-articular osteopenia, joint space abnormalities, and characteristics of cysts and erosions, the severity of destruction was graded as follows: grade 1: periarticular soft tissue swelling, osteoporosis and slight joint space narrowing; grade 2: erosion and joint space narrowing corresponding to definite early abnormality; grade 3: medium destructive abnormality; grade 4: severe destructive abnormality; and grade 5: mutilating abnormality. Grades ≥ 3 are considered signs of articular destruction [19]. All patients were regularly receiving methotrexate with or without corticosteroids or hydroxychloroquine. Disease activity score in 28 joints (DAS28) was calculated [20]. Functional disability was graded using the Steinbrocker functional classification [21].
Serum and synovial COMP levels were determined by enzyme-linked immunosorbent assay (ELISA), using a kit supplied by AnaMar Medical AB, Lund, Sweden. Each test was assayed in duplicate and all data are covered by the standards.
Statistical analysis
The data were collected, tabulated and analysed using the SPSS package version 15 (SPSS Inc., Chicago, IL, USA). Data were summarized as mean ± standard deviation (SD) and median/25th–75th quartiles. Mann–Whitney U tests were used for comparative analysis of two quantitative variables. Spearman’s correlation analysis was used for detection of the relationship between two variables. Logistic regression analysis was applied to detect predictors for the elevated COMP level in serum and synovial fluid. Results were considered significant at p < 0.05.
Results
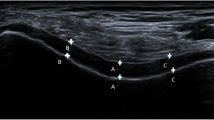
The 24 included female RA patients had a mean age of 44.04 ± 10.5 years (median 46; 25th–75th quartile 36–50 years). Patients were subdivided into two groups according to disease duration. Group 1 included 12 early-stage RA patients without joint destruction. Disease duration ranged from 6 months to 2.5 years, with a mean of 1.6 ± 0.6 years (median 2.8; 25th–75th quartile 1.5–11.8 years). Group 2 included 12 long-standing (> 3 years) RA patients with joint destruction. A total of 10 patients had concomitant knee effusions, 5 in each group. The control group comprised 30 healthy females, whose age (mean 45.4 ± 9.04 years; median 48; 25th–75th quartile 40–50.3 years) was comparable to that of the patients (p = 0.61). Serum COMP was significantly increased in RA patients (19.54 ± 5.47 µg/ml; median 19.5; 25th–75th quartile 15.5–24.2 µg/ml) compared to controls (5.93 ± 1.95 µg/ml; median 5.4; 25th–75th quartile 4.8–7.2 µg/ml; p < 0.001). Knee effusion was accessible in 10 patients; 5 with early and 5 with established RA. The synovial COMP level was 41.4 ± 14.4 μg/ml (median 41; 25th–75th quartile 29.3–55 μg/ml). Patients were receiving intramuscular methotrexate (12.6 ± 8.4 mg/week; median 15; 25th–75th quartile 2.5–17.5 mg/week), hydroxychloroquine 400 mg/d and prednisolone (2.9 ± 5.1 mg/d). The majority of patients were not receiving oral steroids or were on low doses. The medications used were comparable between both groups. Characteristics of the early and established RA patients are shown in Tab. 1 In those with early RA, 7 had grade 1 and 5 had grade 2 disease, while those with established RA had grade 3 in 6 cases, grade 4 in 4 and grade 5 in 2 cases.
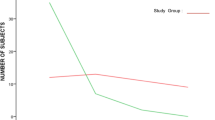
No significant correlation of COMP levels was found with the laboratory findings or medications received. On performing regression analysis in the RA patients, only BMI could predict the level of serum COMP (beta = 0.45, p = 0.02). However, age (beta = 0.84, p = 0.007), disease duration (beta = 0.43, p = 0.03), BMI (beta = 0.3, p = 0.04) and modified Larsen score (beta = − 0.56, p = 0.03) could significantly predict the level of synovial COMP (Tab. 2). The correlation of BMI with the serum and synovial COMP is shown in Fig. 1 Serum and synovial COMP showed a significant correlation (r = 0.89, p = 0.001).
Discussion
Imbalance between cartilage formation and breakdown biomarkers such as COMP is associated with joint destruction and prognosis of destruction [22]. The detection of COMP fragments and anti-COMP antibodies in RA serum and/or synovial fluid supports the theory that latent, subpathogenic autoimmune reactions directed against cartilage matrix proteins eventually contribute to manifestation of human arthritis [23].
In the current work, serum COMP was significantly elevated in established compared to early-stage RA patients. Patients at risk of progressive joint damage are diagnosed early by measuring synovial COMP, in order to detect molecular events leading to cartilage destruction and to monitor disease progression [24]. In a previous study, the COMP level was significantly higher in systemic sclerosis (SSc) patients with subclinical RA [25]. Among pre-RA cases prior to diagnosis, raised COMP (> 12 U/l) was seen in a greater proportion of those with a negative anti-cyclic citrullinated peptide (CCP) result [26]. In the present study, the serum COMP level in the control group was 5.93 ± 1.95 µg/ml and in the patient group 19.54 ± 5.47 µg/ml. Similarly, other studies have shown that in the serum of the normal population the COMP level was 5 µg/ml, whereas it was 10.4 ± 3.6 µg/ml in RA patients. Additionally, an increased level of COMP in the synovial fluid was described in early-stage RA, whereas in advanced stages, the level of COMP decreased. The average value of the serum COMP level in RA patients was 10.4 ± 3.6 U/l [27]. The higher serum COMP levels in late onset RA could be due to concomitant osteoarthritic processes in larger joints, which are not symptomatic [28].
Serum COMP was also significantly elevated compared to the control group in the present study. The synovial level was increased more than twofold compared to the serum level. It has previously been reported that COMP concentrations in synovial fluid are ten-times higher than in serum, and higher COMP concentrations have been observed in patients with higher radiographic destruction grades [29, 30]. Elevation of COMP may reflect joint damage that is dependent on the synovial inflammatory process in early-stage RA [31].
In the present study, both the serum and synovial COMP levels significantly correlated with the age of RA patients. Other studies have also shown a correlation between the serum COMP level and the age of RA patients [27] and those with knee OA [32].
Disease activity tended to be higher in established compared to early-stage RA patients, and significantly correlated with the serum and synovial COMP levels. Similarly, in a study of 20 Egyptian RA patients, the significantly elevated serum COMP was significantly related to disease activity score and cartilage destruction [33]. Furthermore, serum COMP correlates with disease activity (DAS28) in RA and is a valuable marker to identify those patients achieving remission [27, 34, 35]. Similarly, serum and synovial fluid COMP levels in RA patients not only reflect cartilage destruction, but also correlated with ESR and CRP levels, which are indicators of the acute-phase response [36]. Contrastingly, in another study, levels did not correlate with ESR or other acute phase indicators of inflammation. It was reported that serum COMP was found to be a specific marker for cartilage degradation in RA, but not related to the nonspecific inflammatory process [30]. Although COMP is not unique to cartilage and there is a reported lack of correlation with CRP in RA, there is a clear role for COMP as a marker reflecting processes not directly linked to inflammation. On the basis of this characteristic, COMP is an additional variable that should prove useful if included in the evaluation of potentially tissue-protective antirheumatic drugs [37].
The modified Larsen score was significantly higher in the established than the early-stage RA patients and correlated significantly with both serum and synovial COMP levels. Increasing COMP levels correlated with radiological joint damage progression and erosion score in patients with early RA [38]. The severity of RA can be measured objectively by radiographic progression, and biomarkers such as COMP could increase the prognostic ability of these approaches [39]. In early-stage RA, COMP was associated with MRI-proven joint edema, erosion and synovitis score [31, 40]. In RA, a significant correlation was found between serum levels of COMP at baseline and deterioration of Larsen score, even after 5 years. COMP may thus be used as a prognostic marker for cartilage degradation in patients with established RA [41]. On the other hand, another study found no association between radiographic progression and baseline serum levels of COMP in RA [42]. Serum levels of COMP tended to correlate with joint damage score in early RA and with later joint destruction [43].
In the present study, there was no significant correlation of the COMP levels with the functional class of the RA patients, which is in accordance with a previous study [44].
BMI was significantly higher in established compared to early-stage RA patients and also correlated significantly with both serum and synovial COMP levels.
A decrease in the serum COMP (sCOMP) level correlated significantly with weight loss in obese patients with knee OA [45, 46], and COMP significantly correlated with BMI in patients with knee OA [32].
Conclusion
COMP is not only involved in the pathogenesis of RA, but is also considered a prominent biomarker of disease activity in early-stage and established RA patients, thus making COMP a potential therapeutic target. The obvious correlation with the BMI throws light on the importance of weight control not only in OA, but also in RA. In order to confirm the present results, it is recommended that a further study be performed on a larger scale, with a longitudinal design.
References
Agarwal SK (2011) Biologic agents in rheumatoid arthritis: an update for managed care professionals. J. Manag. Care Pharm 17(9 Suppl B):S14–S18
Gheita TA, Azkalany GS, Gaber W, Mohey A (2015) Clinical significance of serum TNFα and 308 G/A promoter polymorphism in Rheumatoid Arthritis. Egyptian Rheumatol 37(2):49–54
Gheita TA, Kenawy SA (2012) Effectiveness of Nigella sativa oil in the management of rheumatoid arthritis patients: a placebo controlled study. Phytother Res 26(8):1246–1248
Otero M, Goldring MB (2008) Cells of the synovium in rheumatoid arthritis. Chondrocytes. Arthritis Res Ther 10:401
Andreas K, Lübke C, Häupl T et al (2008) Key regulatory molecules of cartilage destruction in rheumatoid arthritis: an in vitro study. Arthritis Res Ther 10:R9
Geng H, Nandakumar KS, Pramhed A et al (2012) Cartilage oligomeric matrix protein specific antibodies are pathogenic. Arthritis Res Ther 14(4):R191
Guo F, Lai Y, Tian Q et al (2010) Granulin-epithelin precursor binds directly to ADAMTS-7 and ADAMTS-12 and inhibits their degradation of cartilage oligomeric matrix protein. Arthritis Rheum 62(7):2023–2036
Fawzy SM, El-Sherbeni HH, Rashad A, El-demellawy HH (2011) Serum COMP and their correlations with various disease parameters in patients with systemic lupus erythematosus and osteoarthritis. Egyptian Rheumatol 33(1):13–19
Darwish AF, Abdel-Ghany HS, El-Sherbini YM (2012) Diagnostic and prognostic value of some biochemical markers in early knee osteoarthritis. Egyptian Rheumatol 34(1):1–8
Hammad YH, Magid HR, Sobhy MM (2015) Clinical and biochemical study of the comparative efficacy of topical versus oral glucosamine/chondroitin sulfate on osteoarthritis of the knee. Egyptian Rheumatol 37(2):85–91
Morozzi G, Fabbroni M, Bellisai F et al (2007) Cartilage oligomeric matrix protein level in rheumatic diseases: potential use as a marker for measuring articular cartilage damage and/or the therapeutic efficacy of treatments. Ann N Y Acad Sci 1108:398–407
Koelling S, Clauditz TS, Kaste M, Miosge N (2006) Cartilage oligomeric matrix protein is involved in human limb development and in the pathogenesis of osteoarthritis. Arthritis Res Ther 8(3):R56
Fujikawa K, Kawakami A, Tamai M et al (2009) High serum cartilage oligomeric matrix protein determines the subset of patients with early-stage rheumatoid arthritis with high serum C-Reactive Protein, Matrix Metalloproteinase-3, and MRI-Proven Bone Erosion. J Rheumatol 36(6):1126–1129
Soderlin MK, Kastbom A, Kautiainen H et al (2004) Antibodies against cyclic citrullinated peptide (CCP) and levels of cartilage oligomeric matrix protein (COMP) in very early arthritis: relation to diagnosis and disease activity. Scand J Rheumatol 33(3):185–188
Young-Min S, Cawston T, Marshall N et al (2007) Biomarkers predict radiographic progression in early rheumatoid arthritis and perform well compared with traditional markers. Arthritis Rheum 56(10):3236–3247
Lindqvist E, Eberhardt K, Bendtzen K et al (2005) Prognostic laboratory markers of joint damage in rheumatoid arthritis. Ann Rheum Dis 64(2):196–201
Morozzi G, Fabbroni M, Bellisai F et al (2007) Low serum level of COMP, a cartilage turnover marker, predicts rapid and high ACR70 response to adalimumab therapy in rheumatoid arthritis. Clin Rheumatol 26(8):1335–1338
Aletaha D, Neogi T, Silman AJ et al (2010) 2010 Rheumatoid arthritis classification criteria an American College of Rheumatology/European league against rheumatism. Arthritis Rheum 62(9):2569–2581
Larsen A (1995) How to apply Larsen score in evaluating radiographs of rheumatoid arthritis in longterm studies? J Rheumatol 22:1974–1975
Prevoo MLL, Hof van’t MA, Kuper HH et al (1995) Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Steinbrocker O, Traeger CH, Batterman RC (1949) Therapeutic criteria in rheumatoid arthritis. JAMA 140:659–662
Dénarié D, Constant E, Thomas T, Marotte H (2014) Could biomarkers of bone, cartilage or synovium turnover be used for relapse prediction in rheumatoid arthritis patients? Mediators Inflamm 2014:537324
Kinne RW (2013) (Auto)immunity to cartilage matrix proteins-a time bomb? Arthritis Res Ther 15(1):101
Ahrman E, Lorenzo P, Holmgren K et al (2014) Novel Cartilage Oligomeric Matrix Protein (COMP) neoepitopes identified in synovial fluids from patients with joint diseases using affinity chromatography and mass spectrometry. J Biol Chem 289(30):20908–20916
Gheita TA, Hussein H (2012) Cartilage Oligomeric Matrix Protein (COMP) in systemic sclerosis (SSc): role in disease severity and subclinical rheumatoid arthritis overlap. Joint Bone Spine 79(1):51–56
Turesson C, Bergström U, Jacobsson LT et al (2011) Increased cartilage turnover and circulating autoantibodies in different subsets before the clinical onset of rheumatoid arthritis. Ann Rheum Dis 70(3):520–522
Wisłowska M, Jabłońska B (2005) Serum cartilage oligomeric matrix protein (COMP) in rheumatoid arthritis and knee osteoarthritis. Clin Rheumatol 24(3):278–284
Kolarz G, Hermann J, Krajnc I et al (2002) Functional capacity and cartilage oligomeric protein (COMP) in serum of patients with maturity-onset polyarthritis. Z Rheumatol 61(4):435–439
Kokebie R, Aggarwal R, Lidder S et al (2011) The role of synovial fluid markers of catabolism and anabolism in osteoarthritis, rheumatoid arthritis and asymptomatic organ donors. Arthritis Res Ther 13(2):R50
Tseng S, Reddi AH, Di Cesare PE (2009) Cartilage Oligomeric Matrix Protein (COMP): a Biomarker of Arthritis. Biomark Insights 4:33–44
Fujikawa K, Kawakami A, Tamai M et al (2009) High serum cartilage oligomeric matrix protein determines the subset of patients with early-stage rheumatoid arthritis with high serum C-reactive protein, matrix metalloproteinase-3, and MRI-proven bone erosion. J Rheumatol 36(6):1126–1129
Verma P, Dalal K (2013) Serum cartilage oligomeric matrix protein (COMP) in knee osteoarthritis: a novel diagnostic and prognostic biomarker. J Orthop Res 31(7):999–1006
Algergawy SA, Abd El-Sabour M, Osman AS et al (2013) Early diagnostic and prognostic values of anti-cyclic citrullinated peptide antibody and cartilage oligomeric matrix protein in rheumatoid arthritis. Egypt J Immunol 20(2):11–20
Kawashiri SY, Kawakami A, Ueki Y et al (2010) Decrement of serum cartilage oligomeric matrix protein (COMP) in rheumatoid arthritis (RA) patients achieving remission after 6 months of etanercept treatment: comparison with CRP, IgM-RF, MMP-3 and anti-CCP Ab. Joint Bone Spine 77(5):418–420
Happonen KE, Saxne T, Aspberg A et al (2010) Regulation of complement by cartilage oligomeric matrix protein allows for a novel molecular diagnostic principle in rheumatoid arthritis. Arthritis Rheum 62(12):3574–3583
Momohara S, Yamanaka H, Holledge MM et al (2004) Cartilage oligomeric matrix protein in serum and synovial fluid of rheumatoid arthritis: potential use as a marker for joint cartilage damage. Mod Rheumatol 14(5):356–360
Crnkic M, Månsson B, Larsson L et al (2003) Serum cartilage oligomeric matrix protein (COMP) decreases in rheumatoid arthritis patients treated with infliximab or etanercept. Arthritis Res Ther 5(4):R181–R185
Andersson ML, Svensson B, Petersson IF et al (2013) Early increase in serum-COMP is associated with joint damage progression over the first five years in patients with rheumatoid arthritis. BMC Musculoskelet Disord 14:229
Krabben A, Huizinga TW, Mil AH (2015) Biomarkers for radiographic progression in rheumatoid arthritis. Curr Pharm Des 21(2):147–169
Christensen AF, Lindegaard H, Hørslev-Petersen K et al (2011) Cartilage oligomeric matrix protein associates differentially with erosions and synovitis and has a different temporal course in cyclic citrullinated peptide antibody (anti-CCP)-positive versus anti-CCP-negative early rheumatoid arthritis. J Rheumatol 38(8):1563–1568
Skoumal M, Kolarz G, Klingler A (2003) Serum levels of cartilage oligomeric matrix protein: a predicting factor and a valuable parameter for disease management in rheumatoid arthritis. Scand J Rheumatol 32(3):156–161
Syversen SW, Goll GL, Heijde D van der et al (2009) Cartilage and bone biomarkers in rheumatoid arthritis: prediction of 10-year radiographic progression. J Rheumatol 36(2):266–272
Roux-Lombard P, Eberhardt K, Saxne T et al (2001) Cytokines, metalloproteinases, their inhibitors and cartilage oligomeric matrix protein: relationship to radiological progression and inflammation in early rheumatoid arthritis. A prospective 5-year study. Rheumatology (Oxford) 40(5):544–551
Andrade FD, Bender AL, Silveira IG da et al (2009) Cartilage oligomeric matrix protein/thrombospondin-5 (COMP/TSP-5) levels do not correlate to functional class in patients with rheumatoid arthritis. Clin Rheumatol 28(12):1441–1442
Bartels EM, Christensen R, Christensen P et al (2014) Effect of a 16 weeks weight loss program on osteoarthritis biomarkers in obese patients with knee osteoarthritis: a prospective cohort study. Osteoarthritis Cartilage 22(11):1817–1825
Richette P, Poitou C, Garnero P et al (2011) Benefits of massive weight loss on symptoms, systemic inflammation and cartilage turnover in obese patients with knee osteoarthritis. Ann Rheum Dis 70(1):139–144
Compliance with ethical guidelines
Conflict of interest. A.O. El Defrawy, T.A Gheita, H.M Raslan, M.M El Ansary and A.H El Awar state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El Defrawy, A., Gheita, T., Raslan, H. et al. Serum and synovial cartilage oligomeric matrix protein levels in early and established rheumatoid arthritis. Z Rheumatol 75, 917–923 (2016). https://doi.org/10.1007/s00393-015-1647-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-015-1647-5