Abstract
Purpose
Current modes of diagnosing and monitoring knee osteoarthritis (OA) are based on weight bearing radiographs usually made by the time joint destruction is already established. Cartilage oligomeric matrix protein (COMP) is a breakdown product of cartilage and its serum levels may be a potential indicator of early destruction in OA. This study aimed to ascertain the usefulness of serum COMP (sCOMP) in diagnosis and monitoring of knee joint OA within the study environment.
Methods
Ninety consenting adults were recruited. In the control group, 45 subjects having a diagnosis of knee OA had clinical and radiological grading done and blood samples taken for assay of sCOMP using the sandwich ELISA method. Forty-five volunteers with no features of osteoarthritis also had serum collected for sCOMP assay. Values obtained were then cross referenced with demographic indices, clinical and radiological severity grade to assess for relationships.
Results
Serum COMP was found to be significantly elevated (p = 0.0001) in the study group. The mean values and standard deviation of sCOMP were 3400 ± 1042.9 ng/ml and 2222 ± 605.6 ng/ml for the study and control groups, respectively. Higher values of sCOMP were found to be associated with higher clinical and radiological grades of OA.
Conclusion
The study demonstrates that sCOMP is significantly higher in patients with knee OA than in those without the disease. Values of sCOMP were also found to increase with severity of knee OA, indicating the possibility of its use as a marker of diagnosis and severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early changes in OA are largely radiographically silent. Current modes of diagnosing and monitoring the disease are based on weight-bearing radiographs usually made by the time joint destruction is already established [1]. Consequently, sensitive pre-radiographic diagnostic tools allow adoption of early interventions which may delay irreversible joint damage. Various potentially disease modifying intervention strategies for OA, such as biological regenerative therapy, chondroplasty, and autologous chondrocyte transfer, increase the need to identify specific factors that can accurately detect the presence and progression of OA at the earliest phase before onset of irreversible bony and soft tissue complications [2,3,4].
A possible method of early detection would be to measure metabolic products of cartilage repair and degradation to reflect variations in joint remodeling. One metabolic product which may serve as a predictive diagnostic biomarker of OA is COMP [5].
Osteoarthritis is induced by the gradual disintegration of articular cartilage which results in tearing of the collagen scaffold and subsequent release of COMP into the extracellular space and excretion into the synovial fluid, serum, and urine. COMP, also known as thrombospondin-5, is synthesized by chondrocytes and synovial cells after activation by inflammatory cytokines. Chondrocytes function primarily to maintain cartilage homeostasis [6]. In OA however, this function tends to diminish as evidenced by telomerase shortening [7] and increased senescence-associated β-galactosidase [8]. These changes impair chondrocyte function with decreased synthetic ability and sparse proteoglycans [9].
The earliest notable changes, while the cartilage is still macroscopically intact, are an increase in water content of the cartilage and increased permeability to the matrix proteoglycans as well as cartilage degradation products such as COMP [6]. At a slightly later stage, there is loss of proteoglycans and defects appear in the cartilage collagen scaffold. Microscopically, surface flaking and fibrillations which appear as vertical clefts develop along the normally smooth articular cartilage on the surface of a diseased joint. As the disease progresses, continued cartilage loss leads to loss of joint space as noted on radiographs [10].
Elevated serum levels of COMP (sCOMP) which may show evidence of cartilage damage have been demonstrated in persons with OA compared with healthy persons [11,12,13]. A recent systemic review and meta-analysis by Hao HQ et al. [14] concluded that sCOMP performed moderately in distinguishing between patients with knee and hip osteoarthritis when compared with controls. Variations in sCOMP may also be due to geographical variations in bone density and metabolism, body composition, skeletal and joint size, and cartilage tendon mass as suggested by Jordan et al. [15]. To our knowledge, this is the first study on the applicability of COMP as a biomarker for OA in Africans. Consequently, establishment of sCOMP as a marker of diagnosis and severity may serve as a pivotal tool for institution of early therapy and obviate the need for undesirable radiation exposure in diagnosis, monitoring disease progression and treatment.
This was a prospective case-control study which aimed to determine serum levels of COMP in patients with knee OA. Values obtained were compared with those of disease-free individuals with the aim of evaluating the use of sCOMP as a predictive marker in diagnosis and grading of severity. The study was based on the hypothesis that there might be a significant relationship between sCOMP and the presence and severity of knee OA.
Methods
Patients
All consecutive patients seen in the out-patients department with knee joint OA fulfilling the American College of Rheumatology (ACR) criteria were identified following routine history and examination. All those found eligible who chose to participate were recruited. Those who had clinically apparent OA of other joints, previous surgical intervention or trauma to the affected knee(s), and previous intra-articular steroid injections or visco-supplementation within the previous six weeks and analgesic use within the previous two weeks were excluded. In addition, healthy volunteers matched for age and sex who presented at the wellness center for their annual general medical assessments and had no apparent OA in any joint or the spine following clinical screening were recruited as controls for the study.
The clinical grading of severity form for those with OA was completed by the individuals themselves and collated a single orthopaedic surgeon, and patients thereafter had weight-bearing plain antero-posterior and lateral radiographs of both knees taken. Clinical grading was done using the Lequesne index of severity which assesses three parameters: pain or discomfort, maximum distance walked, and activities of daily living [16]. Data obtained was entered into a structured proforma and totaled to determine patient’s handicap.
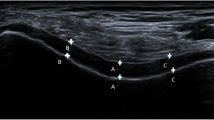
Radiographs were classified using the Kellgren and Lawrence scoring system by a single radiologist who was blinded to the results of the clinical grading of severity [17].
Ethics and consent
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Ethical approval was obtained from the Ethics and Research Committee of Obafemi Awolowo University Teaching Hospital, Ile-Ife, Osun State, Nigeria (IRB/IEC/0004553). Verbal and written informed consent was obtained from all patients and volunteers for the study and the publication of findings.
Immunoassay
Subjects had 5 ml of venous blood drawn after a 30 minute period of rest under aseptic conditions into a plain sample bottle. Clotted blood samples were then centrifuged for 15 minutes at 3000 rpm (rpm) to remove particulates and extract serum. Serum samples were then transferred into another plain bottle and stored at − 20° centigrade and pooled for 30 days. Assay for COMP was then done by a chemical pathologist alongside the investigator using the commercial human COMP ELISA kit (Picokine™ ELISA kit EKO913 Bosterbio Biomedicals, Pleasanton, CA, USA) sandwich technique which employs a biotinylated monoclonal antibody. The kit is specific for thrombospondin-5/COMP tissue; abundantly expressed in the chondrocyte extracellular matrix, but also found in the bone, tendon, ligament, and synovium and blood vessels with a sensitivity of < 10 pg/ml and detection limits between 156 and 10,000 pg/ml (study values expressed in ng/ml due to multiplication of the dilution factor to the concentrations.).
For the assay, stored serum was divided into aliquots of 0.1 ml per well which were pre-coated with biotinylated monoclonal antibodies. The diluent buffer, working solution, and the color developer agents were sequentially added after incubation and washing for 90 minutes, 60 minutes, and 20 minutes, respectively. The sandwich created was then washed four times to remove unbound antibodies. A standard curve was then plotted following spectrophotometry based on the optical densities generated relative to the standard solution, and sCOMP values were interpolated from the curve. Care was taken to multiply the dilution factor to the concentrations. Values obtained were then cross referenced with demographic indices, clinical and radiological severity grade to assess for relationships. Analyses were performed without knowledge of the clinical and radiological data.
Data analysis
The data obtained from the study was subjected to computer analysis using the Statistical Package for Social Sciences (SPSS) software for Windows version 20 (SPSS Inc., Chicago, IL, USA). Calculations of mean, range, and standard deviation were done.
Comparisons between categorical variables were done using the chi-square test. Mean values of sCOMP were compared between control subjects and those with knee OA using the Students t test, while correlations between severity and sCOMP in those with knee OA were determined using Pearson’s correlation coefficient. The relationship between sCOMP and BMI, clinical grade, and Maximum Index Score was assessed using analysis of variance (ANOVA). For all statistical tests, a p value of < 0.05 was considered significant.
Results
A total of ninety subjects were recruited into the study with forty-five patients each in the study and control groups. Both groups were matched for age and sex. Their ages ranged between 41 and 80 years with a mean and standard deviation of 65.53 ± 9.74 years in the study group and 61.20 ± 9.46 years in the control group. The study population consisted of 19 males (42.2%) and 26 females (57.8%) with a male to female ratio of 1:1.4 while the control group had 16 males (35.6%) and 29 females (64.4%).
An almost equal number of subjects were found to be overweight in both groups with 19 patients (42.2%) in the study group and 20 patients (44.4%) in the control group. However, more patients were obese in the study group (18 patients/40.0%) than in the control group (9 patients/20.0%). The mean BMI in the study group was higher (28.28 ± 4.2 kg/m2) than that of the control group (24.62 ± 3.6 kg/m2). This difference was statistically significant (p = 0.014).
The mean duration of symptoms in months was 45.1 ± 11.7. The duration ranged between two and 180 months. A majority presented between ten and 72 months after onset.
Clinical severity for those with OA was assessed using the Lequesne algofunctional index scoring system and a majority of patients presented with at least a severe form of disease on clinical grading as follows: mild three (6.7%), moderate ten (22.2%), severe 15 (33.3%), very severe 13 (28.9%), and extremely severe four (8.9%).
Serum COMP values in the study group ranged between 1400 and 5400 ng/ml, while in the control group, the range of values was between 1100 and 4400 ng/ml. Higher values were recorded for the study group than controls. The mean values and standard deviation of sCOMP in the study group was 3400 ± 1042.9 ng/ml while that of the control group was 2222 ± 605.6 ng/ml. Values of sCOMP in the control group are shown to be concentrated at levels between 1400 and 2500 ng/ml after which there is a steep and steady decline in sCOMP levels. More subjects in the case group are shown to have sCOMP levels greater than 2500 ng/ml (Fig. 1).
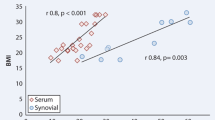
Association between sCOMP and duration of symptoms was also tested (among the study group (n = 45) and found to be statistically significant (p = 0.010). A large number of the patients presented after three years (42.2%) and higher levels of sCOMP (> 3601 ng/ml) were found in them. A significant association was also found between increasing age and higher sCOMP values in both groups (p = 0.006). Higher sCOMP values were also found to be associated with higher BMI in both groups (p = 0.017). Differences between sCOMP values in males and females were not statistically significant (p = 0.626) (Table 1).
A significant association between sCOMP and clinical grade (p = 0.0001) is shown in Table 2. A breakdown of the clinical severity score into its three different components showed a moderately positive correlation between sCOMP levels and the pain score which was also statistically significant (p = 0.0001) (Table 3).
Radiological severity was found to be significantly associated with increasing sCOMP values (p = 0.002) (Table 4)
Discussion
To our knowledge, this is the first study on the applicability of COMP as a biomarker for OA in Africans. This study reveals that sCOMP values were significantly higher in patients with knee OA than in control subjects. Values of sCOMP were also found to increase with severity of knee OA. These findings suggest the possibility of its use as a predictive marker of diagnosis, severity, and progression in knee OA.
Study data demonstrate that more patients presented with at least severe disease on the Lequesne algofunctional index and ≥ Grade 3 on the Kellgren and Lawrence radiological grading system in this study. Values of sCOMP were found to positively predict higher clinical and radiological levels of OA as noted by Hao et al. and several other investigators [5, 11, 14, 18]. This may give credence to the evaluation of COMP as an alternative (or synergistic investigation) to radiological assessment. This will however require larger validation studies. Chaganti et al. [19] however noted that the rate of increase in severity may not necessarily be directly proportional to the rise in sCOMP levels. The explanation for this may be that in the early phase, cartilage is more metabolically active and undergoes more attempts at repair following focal damage. The early phase may also be accompanied by synovitis. Synovium is another established source of COMP and may contribute to higher levels seen at this phase of the disease [20]. However in later stages following repeated insult, overall degeneration may overtake attempts at repair resulting in less metabolically active cartilage and as such less sCOMP elaboration.
The individual sections assessed under the clinical grading index were tested against sCOMP for associations. Higher sCOMP values were found in those with higher pain scores, more so than in those with high scores for walking distance and limitations in activities of daily living on the clinical grading index. This implies that the pain score may be the most representative aspect of the Lequesne scoring system with regard to clinical severity and sCOMP levels. Clinical grading may also be subjective in determining the actual degree of joint destruction as noted by El Arman et al. [21]. Overall, sCOMP levels in this study were found to be significantly increased with increasing clinical and radiological severity. This may suggest that serum assay can be utilized as a marker of disease severity in the study environment. However, an absence of standardized sCOMP values as expected for healthy individuals and those with knee OA may limit its applicability.
Data obtained from the study showed mean values and standard deviation of sCOMP were significantly higher in the study group (3400 ± 1042.9 ng/ml) than in the control group (2222 ± 605.6 ng/ml). This suggests the probability of more sCOMP being released from degenerating cartilage in OA. Higher variability in COMP values was noted in the control group; however, associated pathologies which may have been responsible for the few high COMP values were not found in the control group.
Various studies comparing levels of sCOMP in healthy individuals to that of patients with knee OA have shown significantly higher levels in the knee OA group [6]. Wakitani et al. [22] using a human ELISA method with monoclonal antibody found a mean level of sCOMP among those with knee OA of 1572 ± 182 ng/ml which was higher than what was found in healthy individuals (1030 ± 150 ng/ml). This study utilized a similar method as Wakitani et al. with higher values obtained within the study environment. This may be explained by increased predisposition of Africans to degeneration from repetitive use in form of long trekking distances on uneven surfaces, menial jobs, trauma, and early infections. It may also be due to geographical variations in bone density and metabolism, body composition, skeletal and joint size, and cartilage/tendon mass as suggested by Jordan et al.106
On the other hand, using a human ELISA method with polyclonal antibody, Neidhart et al. [6] found mean values of sCOMP to be 5700 ± 3200 ng/ml in knee OA group and 1700 ± 1400 ng/ml in healthy individuals. El-Arman et al. [21] in Egypt also used an polyclonal method of assay and found sCOMP levels of 4100 ± 1900 ng/ml in those without OA and 7170 ± 3000 ng/ml in patients with OA. International standard values for sCOMP are not available, and this accounts for the large variations in values noted across these studies. One possible reason for these variations is the method of assay. This study, as well as all the studies assessed, used a commercial human ELISA kit for sCOMP assay. However, there were differences in the antibody used which was either monoclonal or polyclonal. A monoclonal antibody was used in this study, and this is thought to have a better specificity and sensitivity for sCOMP. Stabler et al. compared various methods of sCOMP assay and concluded that the purity of the standard solution may account for the differences in values [23]. One way to ascertain which ELISA kit is the best at detecting sCOMP levels is by comparing each assay technique with serum samples from the same subjects. If the assay method is standardized, similar values may be generated to determine normal ranges. This will permit the use of sCOMP in screening for early knee OA and institution of intervention strategies with the hope of averting or delaying irreversible joint damage.
Another possible reason for variations in values may be the secretion of sCOMP by other tissues [24, 25]. Cartilage is thought to be the major source of sCOMP; however, lower levels have been detected in synovium and the menisci [20]. Synovial sCOMP was however found to be 100 times lower than that of cartilage [11]. This may confound the specificity of sCOMP in screening for cartilage degeneration solely. In this study, screening for OA in other large joints including the spine was done clinically. This screening method may be inadequate in excluding the presence of OA in other joints serving as a confounding factor. Further investigations on sCOMP may require more sensitive screening methods such as magnetic resonance image scans to rule out the presence of OA in other joints and increase the strength of such studies.
This study was limited by the investigation of a single biomarker (COMP) in identification of OA as well as the use of clinical screening in ruling out OA of other joints among the control group. The number of patients is also quite limited.
Conclusion
This study demonstrates that sCOMP is significantly higher in patients with knee OA than in those without the disease. Values of sCOMP were also found to increase with severity of knee OA, thus verifying the possibility of its use as a predictive marker of diagnosis and severity. Overall, sCOMP shows promise for eventual adoption as a marker for diagnosis of early OA thus permitting early intervention to avert or delay disease progression.
Data availability
Available on request.
References
Johannes WJ, Bijlsma M, Francis B, Floris L (2011) OA: an update with relevance for clinical practice. Lancet 377:2115–2126
Kon E, Buda R, Filardo G, Di Martino A, Timoncini A, Cenacchi A et al (2010) Platelet-rich plasma: intra-articular knee injections produced favorable results on degenerative cartilage lesions. Knee Surg Sports Traumatol Arthrosc 4:472–479
Murphy M, Barry F (2015) Cellular Chondroplasty: a new technology for joint regeneration. Journal of Knee Surgery 28(01):45–50
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010 Jun) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38(6):1117–1124
Susan TA, Hari R, Paul ED (2009) Cartilage oligomeric matrix protein: a biomarker of OA. Biomark Insights 4:33–44
Bi X (2018) Correlation of serum cartilage oligomeric matrix protein with knee OA diagnosis: a meta-analysis. J Orthop Surg Res 13(1):262
Martin JA, Buckwalter JA (2002) Aging, articular cartilage chondrocyte senescence and OA. Biogerontology. 3(5):257–264
Martin JA, Buckwalter JA (2003) The role of chondrocyte senescence in the pathogenesis of OA and in limiting cartilage repair. J Bone Joint Surg Am 85(suppl 2):106–110
Bolton MC, Dudhia J, Bayliss MT (1999 Jan 1) Age-related changes in the synthesis of link protein and aggrecan in human articular cartilage: implications for aggregate stability. Biochem J 337(1):77–82
Wirth W, Nevitt M, Hellio Le Graverand MP, Lynch J, Maschek S et al (2014) Lateral and medial joint space narrowing predict subsequent cartilage loss in the narrowed, but not in the non-narrowed femorotibial compartment – data from the OA. Initiative OA and Cartilage 22:63–70
Vilim V, Vytasek R, Olejarova M, Machasek S, Gatterova J, Prochazka B et al (2001) Serum cartilage oligomeric matrix protein reflects the presence of clinically diagnosed synovitis in patients with knee OA. OA Cart 9:612–618
Conrozier T, Saxne T, Fan CS, Mathieu P, Tron AM, Heinegard D et al (1998) Serum concentrations of cartilage oligomeric matrix protein and bone sialoprotein in hip OA: a one year prospective study. Ann Rheum Dis 57:527–532
Sharif M, Saxne T, Shepstone L, Kirwan JR, Elson CJ, Heinegard D et al (1995) Relationship between serum cartilage oligomeric matrix protein levels and disease progression in OA of the knee joint. Br J Rheumatol 34:306–310
Hao HQ, Zhang JF, He QQ, Wang Z (2019) Cartilage oligomeric matrix protein, C-terminal cross-linking telopeptide of type II collagen, and matrix metalloproteinase-3 as biomarkers for knee and hip OA (OA) diagnosis: a systematic review and meta-analysis. OA and Cartilage. 27(5):726–736
Jordan JM, Luta G, Stabler T, Renner JB, Dragomir AD, Vilim V, Hochberg MC, Helmick CG, Kraus VB (2003) Ethnic and sex differences in serum levels of cartilage oligomeric matrix protein: the Johnston County OA project. Arthritis & Rheumatism 48(3):675–681
Lequesne MG (1997) The algofunctional indices for hip and knee OA. J Rheumatol 24:779–781
Schiphof D, De Klerk BM, Kerkhof HJM, Hofman A, Koes BW, Boers M, Bierma-Zeinstra SMA (2011) Impact of different descriptions of the Kellgren and Lawrence classification criteria on the diagnosis of knee OA. Ann Rheum Dis 70:1422–1427
Petersson IF, Boegard T, Svensson B, Heinegard D, Saxne T (1998) Changes in cartilage and bone metabolism identified by serum markers in early OA of the knee joint. Br J Rheumatol 37:46–50
Chaganti RK, Kelman A, Lui L, Yao W, Javaid MK, Bauer D, Nevitt M, Lane NE (2008) Change in serum measurements of cartilage oligomeric matrix protein and association with the development and worsening of radiographic hip OA. OA and Cartilage 16(5):566–571
Recklies AD, Baillargeon L, White C (1998) Regulation of cartilage oligomeric matrix protein synthesis in human synovial cells and articular chondrocytes. Arthritis & Rheumatology 41(6):997–1006
El-Arman MM, El-Fayoumi G, El-Shal E, El-Boghdady I, El-Ghaweet A (2010) Aggrecan and cartilage oligomeric matrix protein in serum and synovial fluid of patients with knee OA. HSS J 6(2):171–176
Wakitani S, Nawata M, Kawaguchi A, Okabe T, Takaoka K, Tsuchiya T, Nakaoka R, Masuda H, Miyazaki K (2007) Serum keratan sulfate is a promising marker of early articular cartilage breakdown. Rheumatology. 46(11):1652–1656
Stabler T, Fang F, Jordan J, Vilim V, Kraus VB (2007) 131 A comparison of methods for measuring cartilage oligomeric protein (comp) in human subjects with knee OA. OA and Cartilage. 15:c81–c82
Hedbom E, Antonsson P, Hjerpe A, Aeschlimann D, Paulsson M, Rosa-Pimentel E, Sommarin Y, Wendel M, Oldberg A, Heinegård D (1992) Cartilage matrix proteins. An acidic oligomeric protein (COMP) detected only in cartilage. J Biol Chem 267(9):6132–6136
Müller G, Michel A, Altenburg E (1998) COMP (cartilage oligomeric matrix protein) is synthesized in ligament, tendon, meniscus, and articular cartilage. Connect Tissue Res 39(4):233–244
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and design of the work. All authors also contributed to the acquisition, analysis, and interpretation of data. The drafted work was critically revised and approved for publication by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethical approval was obtained from the Ethics and Research Committee of Obafemi Awolowo University Teaching Hospital, Ile-Ife, Osun State, Nigeria (IRB/IEC/0004553).
Consent to participate
Verbal and written informed consent was obtained from all participants for the study.
Consent for publication
Verbal and written informed consent was obtained from all patients and volunteers for publication of the study findings.
Code availability
N/A.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akinmade, A., Oginni, L.M., Adegbehingbe, O.O. et al. Serum cartilage oligomeric matrix protein as a biomarker for predicting development and progression of knee osteoarthritis. International Orthopaedics (SICOT) 45, 551–557 (2021). https://doi.org/10.1007/s00264-021-04943-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-04943-4