Abstract
Catheter ablation is an established treatment option for atrial fibrillation (AF), and pulmonary vein isolation (PVI) has become the gold standard in AF ablation. AF recurrence after PVI remains an important clinical problem. Recovery of conduction from the pulmonary veins (PVs) is considered the dominant mechanism for AF recurrence in paroxysmal AF. However, the underlying mechanism of AF recurrence after PVI is more complex in patients with persistent and longstanding persistent AF. Different ablation technologies and energy sources have been developed aimed at improving lesion quality and durability with an acceptable safety profile. Novel technologies are under evaluation which have a great potential to produce permanent PVI after a single ablation procedure. However, clinical value of these novel devices needs to be tested in adequately powered randomized controlled trials. In this article, we review the history of catheter ablation for AF and discuss the present and future ablation technologies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is the most common supraventricular tachyarrhythmia [1] and is associated with reduced quality of life [2], increased mortality [3] and morbidity, including enhanced risk of stroke [4], heart failure [5], and repeated hospitalizations [6]. Due to its significant impact on cardiovascular morbidity and mortality, researchers have sought ways to successfully treat and even cure some types of AF. Over the past decades, percutaneous catheter ablation (CA) has become an important AF treatment modality to restore and maintain sinus rhythm. Pulmonary vein isolation (PVI) is now considered the cornerstone of catheter-based treatment for paroxysmal and early persistent AF [7, 8]. Since the introduction of CA, major advances have been made. Different ablation technologies and energy sources have been designed and the search for improving ablation safety and clinical outcome continues. This article outlines the history and evolution of CA, reviews the currently available AF ablation technologies, and provides a glimpse into future ablation techniques.
History of catheter ablation
The first intra-cardiac use of catheters was described in the 1960s, where the application was limited to signal recording and cardiac stimulation. One of the earliest reports of catheter use is a study performed by Durrer et al. in which application of intracardiac electrical pulses and signal recording was described in patients with Wolff-Parkinson-White (WPW) syndrome [9]. Together with electrophysiological studies performed by Zipes and Wellens in the 1970s, insights into tachycardia mechanisms, including the WPW syndrome, markedly improved [10,11,12].
Probably the first described catheter-mediated ablation was permanent atrioventricular conduction (AV) block accidentally caused in a patient undergoing an electrophysiological study for recurrent syncope in 1979 [13]. During the procedure, the patient required electrical cardioversions for ventricular tachycardia while the intracardiac bipolar recording catheter was reportedly in contact with the bundle of His. Presumably, this led to inadvertent transfer of externally delivered direct current energy over the recording catheter electrodes resulting in complete AV block.
This unintended catheter-mediated induction of AV block was further investigated in the following years, leading to the first described in-human catheter ablation in 1982. In a study by Scheinman et al., five patients suffering from drug refractory supraventricular tachycardia received a permanent pacemaker followed by AV junction ablation using high-energy DC shocks [14]. From this point, the use of the electrode catheters was no longer limited to diagnostic electrophysiological studies alone, and DC ablation was applied in ablation of accessory pathways [15], atrial tachycardias [16], and ventricular tachycardias [17].
While these early results of high-energy DC catheter ablation appeared potentially promising, the occurrence of significant adverse events, including cardiac tamponade and sudden death, were major drawbacks of the technique [18,19,20,21]. High-energy DC shocks were associated with arcing, gas formation and shockwave generation leading to barotrauma [22,23,24].
In the late 1980s, radiofrequency (RF) energy for catheter ablation was introduced. In the early 1990s, many studies on RF ablation followed, showing better efficacy and safety in ablation of accessory pathways, atrial flutter, modification of the AV junction in AV nodal reentrant tachycardia and ventricular tachycardia [25,26,27,28,29]. The use of RF catheter ablation skyrocketed, and high-energy DC ablation became abandoned.
History of atrial fibrillation ablation
While insights obtained from electrophysiological studies led to surgical and catheter-based treatment of several supraventricular tachyarrhythmias, such as WPW syndrome and AV nodal reentrant tachycardia, treatment options for more complex arrhythmias like AF were limited to drugs or pacemaker implantation followed by AV junction ablation. In 1987, the first surgical strategy for AF treatment was reported by Cox and colleagues. Their group performed computerized mapping of atrial fibrillation in animals and man, eventually leading to the development of a surgical procedure for the treatment of drug refractory AF, known as the surgical Maze procedure [30, 31]. The original Maze procedure involved creation of multiple surgical incisions in the left and right atrium during open heart surgery. The rationale for the Maze procedure was derived from experimental studies by Allessie and Schuessler [32, 33]. Allessie et al. experimentally validated Moe’s multiple wavelet hypothesis by mapping the activation pattern in isolated canine atria during rapid pacing-induced cholinergic atrial fibrillation [34,35,36]. Complete mapping of both atria was performed, and it was estimated that a critical number of four to six simultaneously present wavelets were required to maintain AF. Although the underlying mechanisms involved in the initiation and perpetuation of AF were incompletely understood, the main goal of the initial Maze procedure was to compartmentalize the atria, thereby creating an electrical maze, using the “cut and sew” technique or alternative means of creating linear lesions of electrical block in both atria to eliminate reentrant wavelets and restore SR or an atrial rhythm within the atrial myocardium [30]. Further improvements to the surgical technique eventually resulted in the Cox Maze III procedure, which is still used today [37]. Long-term follow-up of 198 patients with paroxysmal and persistent AF who underwent a Cox Maze III procedure showed that 95% were AF free after a mean follow-up of 5.3 years. Major complications occurred in 12%, including two perioperative deaths [38]. Due to the complex and invasive nature of the Maze procedure several investigators in the early 90s tried to replicate the ablation lesion sets using the catheter. Morillo et al. performed a study with 22 dogs in which structural remodeling of the atria was achieved by rapid pacing for 6 weeks, resulting in inducibility of sustained AF. In 11 of the dogs, attempted cryoablation of an area in the posterior left atrium resulted in restoration of sinus rhythm and non-inducibility of AF [39]. In that same year, Elvan et al. published a study in which AF was induced by burst pacing in 27 dogs. The creation of epicardial and endocardial RF ablation lesions targeting the left and right atrium, the superior vena cava, and transverse sinus resulted in reduced inducibility of AF (by high doses of methacholine) [40]. In the mid-90s, feasibility of CA as treatment of AF in humans was reported by Haïssaguerre et al. The ablation involved the creation of multiple linear lesions in the right atrium using RF energy. After ablation AF could not be induced with pacing, and during short-term follow-up of 3 months the patient remained free of arrhythmias without antiarrhythmic drugs [41]. The first patient series on catheter ablation of AF soon followed. In a study by Swartz et al. patients with chronic AF received RF CA in both the left and right atria [42]. Arrhythmia-free survival after 12 months was considered satisfying; however, the complication rate was high including pericardial effusion and cerebrovascular accidents. In a study by Haïssaguerre et al. 45 patients with paroxysmal AF received RF ablation with the creation of linear lesions mainly in the right atrium. Follow-up showed a poor 1-year arrhythmia-free survival, but no serious complications were observed [43]. Long-term follow-up of clinical trials that applied transcatheter linear ablation lesions in the right atrium in a Maze-like approach showed limited success [44, 45]. An historically important AF ablation approach targeting foci that triggered AF was reported by Jaïs et al. These arrhythmogenic foci were found near the sinus node, at the coronary sinus ostium, and at the ostium of the left and right sided pulmonary veins, and were successfully eliminated by RF ablation [46]. In 1998, Haïssaguerre and colleagues published their milestone study on ablation of AF initiating triggers that were mainly localized in the pulmonary veins (PVs) and which could be successfully eliminated using CA [7]. These findings led to a different approach of AF ablation, focusing on the elimination of AF triggers, and the Maze-like linear lesions in the right atrium became abandoned. Subsequently, a method was developed to electrically isolate AF triggers in the PVs by creation of circumferential ablation lesions in the PVs, now known as pulmonary vein isolation (PVI) [47].
Many studies on electrical isolation of the PVs as treatment for AF followed, and currently PVI has become the cornerstone treatment in catheter-based ablation of AF [8]. Randomized trials showed better efficacy rates for RF ablation compared to antiarrhythmic drugs [48,49,50]. Furthermore, PVI resulted in better quality of life compared to drug therapy [51]. However, AF recurrence after ablation was still frequently observed, especially in patients with persistent and long-standing persistent AF. In patients with persistent forms of AF, it was recognized that triggers that initiated and maintained AF frequently originated outside the PVs, including the PV antrum, the posterior wall of the LA, the superior vena cava, the crista terminalis, the coronary sinus, ligament of Marshall and the left atrial appendage [8]. Ablation strategies were adapted to wider ablations at the PV antrum, also known as wide-area circumferential ablation (WACA), and strategies complementary to PVI were investigated [52]. These strategies included linear lesions in the left and right atria, ablation of the left atrial appendage, and ablation of complex fractionated atrial electrograms (CFAE) [53, 54]. Some observational studies have suggested a beneficial effect of additional ablations on treatment outcome [55, 56]. However, results from the randomized STAR AF II trial demonstrated that additional ablation lines or CFAE ablation did not result in better efficacy in patients with persistent AF [57]. Whether selected groups of patients benefit from these additional ablation strategies remains uncertain and subject for future research.
Rationale behind AF ablation
The major impact of AF on cardiovascular morbidity and mortality has driven researchers and physicians to find ways to restore and maintain sinus rhythm. It is generally accepted that the pathophysiology of AF includes a trigger to initiate AF, a substrate to maintain AF, and modulating risk factors, ultimately resulting in progression to more persistent forms of AF [58]. Over the years, AF ablation strategies have targeted elimination of AF triggers or modification of the arrhythmogenic substrate. Ablation lesions are created to produce non-conductive tissue isolating triggers that initiate AF, and interrupt arrhythmogenic pathways in patient-specific AF substrate, or modulate autonomic innervation of the atria [7, 59, 60].
Recent results from the randomized CABANA trial comparing ablative therapy to medical therapy for the treatment of AF showed no significant benefit of CA over medical therapy in reduction of the composite end point of death, disabling stroke, serious bleeding, or cardiac arrest [61]. However, treatment crossover and lower event rates than anticipated might have affected the disappointing results of the CABANA trial. Of note, the trial did show more favorable quality of life outcomes at 12 months following CA compared to medical therapy [62]. Therefore, whether AF ablation can reduce morbidity or mortality remains unclear. Meanwhile, symptom reduction and QOL improvement remain the primary indication for catheter ablation [8].
AF ablation and heart failure
Recent studies suggested AF ablation with restoration of sinus rhythm can improve morbidity and mortality in patients with heart failure. The AATAC study comparing CA with amiodarone resulted in reduction of hospitalization and mortality in persistent AF patients with heart failure [63]. The prospectively randomized CASTLE-AF trial reported similar results, in which CA of AF resulted in a lower rate of hospitalization and mortality in patients with heart failure compared to medical therapy [64].
Present AF ablation techniques and energy sources
3D mapping and creation of a transmural and contiguous ring of scar tissue around the PVs with point-by-point RF ablation can be technically challenging, particularly at less experienced centers. Over the past years, different 3D mapping and catheter ablation systems using various energy sources have been developed to improve catheter handling, thereby enhancing safety, efficiency and efficacy of these ablation procedures. Among these are balloon-based technologies using a variety of energy sources, circular multielectrode, and contact force tip electrode systems. For surgical ablation, clamp devices have been developed to improve lesion quality. In this section, we will review different ablation technologies that are used for AF ablation.
Radiofrequency point-by-point ablation
RF myocardial ablation is a thermal-mediated method in which localized heat generation is used to create tissue necrosis and formation of ablation lesions. Continuous lesions are created in a point-by-point manner usually guided by a dedicated 3D electro-anatomical mapping system. The thermal effect is generated by delivering an electrical current through myocardial tissue from the tip electrode of the ablation catheter to a large dispersive electrode patch (unipolar) or between a pair of electrodes from adjacent ablation catheters (bipolar), causing resistive heating of the underlying tissue at the electrode tip (unipolar) or resistive heating of tissue between two catheter electrodes (bipolar). Myocardial cells become irreversibly damaged when exposed to temperatures of 50 °C or higher, leading to necrosis and eventually to nonconducting myocardial fibrotic scar tissue. If the temperature at the electrode exceeds 100 °C, boiling of blood occurs, resulting in clot and char formation [65]. If the intramyocardial temperatures exceeds 100 °C, boiling of tissue can lead to steam formation (pop lesion) potentially causing intramyocardial rupture and tissue perforation [66]. Factors that affect lesion size include electrode size, temperature, electrode–tissue contact, power and duration of RF energy delivery [65, 67]. Furthermore, heat loss to circulating blood on endocardial side and to epicardial coronaries can compromise lesion formation [65]. RF ablation lesions in PVI often consist of a combination of myocardial necrosis and tissue edema, often resulting in partially reversible myocardial lesions [68]. This latter can appear as irreversible lesions but lead to PV-reconnection later, which is associated with recurrence of atrial arrhythmias after ablation [69,70,71]. Higher power RF energy delivery can increase lesion size and depth but also increases the risk of temperature rise and char formation and collateral damage to structures such as esophagus and phrenic nerve. To allow higher power RF energy delivery, saline irrigation of the catheter tip electrode was developed to improve conductive heating of the underlying tissue while reducing temperature rise in the circulating blood. Saline-irrigated RF ablation results in deeper and larger lesions [66]. Currently, point-by-point RF ablation is most commonly performed using ablation catheter tip electrode irrigation with saline. To improve electro-tissue contact, catheters have been developed that are capable of measuring contact force between the catheter tip and tissue during ablation [72, 73]. RF ablation catheters with a contact force sensor improved outcome of AF ablation in the hands of experienced operators. Contact force of more than 10 g was associated with higher rates of arrhythmia-free survival [74].
Although point-by-point RF ablation is the most commonly applied technique to achieve PVI, the procedure remains technically challenging, even in experienced centers. Potential complications associated with the RF point-by-point ablation technique include cardiac tamponade (0.2–5%) [8, 75], stroke and transient ischemic attack (0–2%) [8, 76], esophageal damage including atrio-esophageal fistulae (0.02–0.11%) [8, 77], and PV stenosis (< 1%) [8, 78].
Multielectrode circumferential RF catheter
Multielectrode circumferential RF ablation catheters were designed to make PVI procedures less complex and time consuming. The currently available multielectrode PV ablation catheters contain nine to ten electrodes with a circular configuration when deployed. These catheters can be navigated to the PV ostium by fluoroscopy, enabling both mapping and ablation. The circumferential placement of the electrodes allows the creation of a circular ablation lesion at the PV ostium after multiple applications, eventually resulting in PVI. The first-generation multielectrode catheter is no longer in use due to its association with asymptomatic cerebral embolisms, which was related to overlap of the first and tenth electrode leading to tissue and blood overheating causing thromboembolisms [79, 80]. Currently, one multielectrode circumferential ablation catheter system is available for clinical practice; the second-generation gold multielectrode ablation catheter (PVAC GOLD™, Medtronic, Minneapolis, MN, USA) containing 9 gold-plated electrodes. PVI with the use of PVAC multielectrode ablation was associated with significantly shorter procedure, fluoroscopy, and radiofrequency energy times [81]. However, comparison of multielectrode PVAC PVI to standard point-by-point irrigated RF ablation PVI showed conflicting data; some studies showed comparable outcomes while others significantly lower long-term atrial arrhythmia-free survival with the PVAC. Currently, available data on efficacy of multielectrode PVAC ablation are scarce and conflicting. Therefore, more prospective and randomized studies on this subject are needed.
Cryoballoon ablation
In cryoballoon ablation (Arctic Front Advance™, Medtronic, Inc., Minneapolis, MN, USA; POLARx™ Cryoablation Catheter, Boston Scientific, Marlborough, MA, USA), PVI is achieved by freezing tissue using a pressurized balloon that occludes the PV ostium and injecting liquid nitrous oxide as refrigerant into the balloon. Freezing tissue below − 40 °C causes irreversible cell death due to freezing of intracellular water that results in irreversible disruption of organelles and cell membranes [82]. The commonly used second-generation cryoballoon (Arctic Front Advance, Medtronic, Inc. Minneapolis, MN, USA) catheter has a refrigerant injection system with 8 injection jets. The catheter has a lumen that can be used to pass a guide wire or a mapping catheter to guide balloon position and record PV potentials during ablation. The balloon catheter can be placed at the PV ostia without the use of 3D electro-anatomic navigation systems, and the balloon design allows circumferential ablation in a so called ‘single shot’ manner. The aim of this balloon design was to shorten and simplify PVI ablation procedures. Cryoablation has become the most frequently used alternative energy source to RF for AF ablation. In the multicenter randomized Fire and Ice trial, cryoballoon and point-by-point RF ablation were shown to be equally effective and safe for the treatment of paroxysmal AF [83]. However, procedure duration and left atrial dwell time were shorter in the cryoballoon group, whereas fluoroscopy time was shorter in the RF group [83]. The most commonly reported complication in cryoballoon ablation is phrenic nerve injury with a reported incidence between 2 and 5%, fortunately often of temporary nature [84, 85]. Recently, presented results from the YETI registry containing data from 5371 patients treated with second-generation cryoballoon shows an incidence of phrenic nerve injury incidence of 3.9%, of which 57.5% were resolved at the end of the procedure. After 12 months, most of the phrenic nerve injuries were recovered, with an incidence of persistent phrenic nerve injury of only 0.08% [86].
Laser balloon
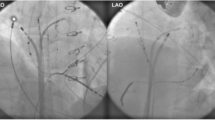
Laser balloon ablation (Heartlight™, CardioFocus, Marlborough, MA, USA) is a balloon-based technology using laser energy to create circumferential cell necrosis and achieve PVI. The laser balloon consists of a compliant balloon that fits into the PVs irrespective of variability in PV sizes and shapes. Unique to the device is the incorporation of a fiber optic endoscope to provide direct visualization of the target tissue in the antrum of the PVs [87]. Once positioned in the PV, the laser source emits energy to the exposed PV antral tissue. The intensity of the laser energy application can be titrated from 5.5 to 12 W, usually during 20–30 s for the formation of each ablation lesion. Lower laser energy setting is usually applied to reduce the risk of heating blood and charring when the occlusion is suboptimal and blood is present in the targeted ablation field. Laser energy output is also lowered when the targeted tissue is in the vicinity of the esophagus or phrenic nerve. Higher laser energy dose can be applied to the remaining PV segments resulting in more durable PVI lesions [88]. A frequently observed complication in laser balloon ablation is phrenic nerve injury, fortunately often of a temporary nature [89]. In a meta-analysis, efficacy and safety of the laser balloon were comparable to other AF ablation techniques [89]. (Fig. 1).
Timeline of key findings in catheter ablation of atrial fibrillation research. AF atrial fibrillation, AV atrioventricular, DC direct current, PVI pulmonary vein isolation, SR sinus rhythm. AATAC Ablation versus Amiodarone for Treatment of AF in Patients With Congestive Heart Failure and an Implanted ICD/CRTD, CABANA Catheter Ablation versus Antiarrhythmic Drug Therapy for Atrial Fibrillation, CASTLE-AF Catheter Ablation versus Standard Conventional Therapy in Patients with Left Ventricular Dysfunction and AF, FIRE&ICE Cryoballoon or Radiofrequency Ablation for Paroxysmal AF. STAR-AF II trial the Substrate and Trigger Ablation for Reduction of AF Trial Part II
Future ablation strategies and technologies
Over the past years, advances have been made in catheter-based AF ablation technologies and strategies. Achieving durable PVI lesions safely and rapidly remains challenging. Driven by AF recurrences after ablation and the occurrence of severe complications including cerebral embolism, esophageal damage, phrenic nerve palsy, investigators continue their search for more effective and safe ablation strategies and technologies.
Ablation line contiguity index
Although contact force-guided PVI is associated with improved arrhythmia-free outcome compared to conventional RF, reconnection of the PVs after ablation is still observed. The PV reconnection is explained by discontiguous and insufficient lesion depth in the circular lesion sets. Optimized and protocolized ablation strategies are developed aiming at creating contiguous and transmural RF lesions that might improve PV isolation durability.
The ablation line contiguity index (ablation index) is a novel measure assessing both contiguity and lesion depth, which can be used as a measure to detect weak spots in the set of created PV antral ablation lesions and LA anterior lines [90, 91]. The ablation index incorporates ablation contact force, time, and power in one marker using a weighted formula, and provides an accurate estimation of lesion depth [92]. Studies that used target values of 550 for anterior and 400 for posterior LA regions demonstrated to prevent PV reconnection [93, 94]. The measure has been integrated in automated lesions tagging software for 3D electro-anatomic mapping to visualize lesion ablation index and target values. Performing contact force RF ablation according to a specific ablation protocol that incorporates the ablation index improved procedural and 1 year outcome of contact force PVI while shortening procedure time [95, 96].
High-power short-duration RF ablation
Recent studies investigated higher RF energy output with shorter pulses in AF ablation to improve safety and create more durable lesions [97,98,99]. This high-power short-duration (HPSD) ablation strategy comprises the use of higher RF power (45–50 W) and shorter duration of each RF energy application (5–15 s) instead of conventional lower RF power (25–30 W) and longer duration of applications (30–60 s). With HPSD, the short duration of RF energy application results in more local resistive heating and local atrial tissue destruction without conductive heating of more distant tissues, such as the esophagus, preventing collateral damage [99, 100].
The HPSD ablation strategy has been shown to improve contiguity and transmurality of atrial linear lesions in animal models [97]. Furthermore, HPSD was associated with shorter procedural and RF time compared with conventional RF ablation and, appears to be a safe approach [98,99,100]. Recent studies have investigated even higher power settings. PVI is achieved with 90 W applications for 4 s per ablation point, with a computerized algorithm modulating power to maintain target temperature [97, 101]. A first-in-human study showed feasibility of achieving PVI with 90 W HPSD ablation in 52 patients. At 3 month follow-up, 49 patients (94.2%) were in sinus rhythm, and the occurrence of serious adverse events was low (3.8%) [101]. In another recently published study, a HPSD ablation protocol with 70 W for 5–7 s was compared to conventional (30–40 W for 20–40 s) ablation, in patients undergoing PVI for paroxysmal AF. The HPSD group showed significantly less AF recurrences 1 year after ablation, with 83.1% freedom from AF compared to 65.1% in the conventional group. Safety profiles were similar between the groups, and significantly shorter radiofrequency and procedural time were observed with HPSD [102].
Novel technologies in multielectrode RF balloon ablation
Several multielectrode RF balloon catheters have been developed for PVI. Similar to point-by-point RF ablation, PVI is achieved by RF energy resulting in thermal injury. The balloon design aims to shorten and simplify PVI ablation procedures. Data on these multielectrode RF balloon systems are limited to experimental and first-in-human studies. The Heliostar multielectrode RF balloon catheter (Biosense Webster Inc, Irvine, CA, USA) contains 10 gold-plated and irrigated electrodes mounted around a balloon in a circular configuration. The RF balloon is advanced to the left atrium using an over-the-wire design and positioned at the PV ostia. Different RF energy settings can be programmed for each individual electrode to control temperature during ablation, particularly at sites that are in vicinity of sensitive structures (e.g. phrenic nerve and esophagus). This device allows the operator to create circumferential PVI lesions in a single shot manner without the need for catheter extensive manipulation, while preventing collateral damage. First-in-human results from the RADIANCE trial, showed feasibility and safety of achieving PVI in 39 patients with paroxysmal AF. Acute PVI was achieved in all the patients, and 79.6% of the PVs was isolated with a single application. In this limited series, one case of phrenic nerve palsy was observed [103].
The Luminize™, another RF balloon system (Boston Scientific, Marlborough, MA, USA) formerly known as the Apama RF balloon (Apama Medical Inc, Campbell, CA, USA), is an over-the-wire balloon catheter, containing 12 proximal (equatorial) electrodes and 6 distal electrodes. The technology incorporates four built-in cameras and LED illumination that allows direct visualization of the targeted area of interest for ablation. Furthermore, both mapping and pacing from the ablation electrodes are possible. The first-in-human results presented at the European Heart Rhythm Association Congress (Lisbon, Portugal, 2019) demonstrated safety and efficacy in achieving PVI in patients with paroxysmal AF [104]. Successful PVI was achieved in 98% of all the PVs and no serious adverse events were observed during a follow up of 30 days.
The Globe system (The Globe® system, Kardium Inc., Burnaby, BC, Canada) is a multielectrode catheter containing globe-shaped expanding array of 122 electrodes that can be deployed in the left atrium. Each individual electrode can perform sensing, pacing, and measurement of tissue contact, temperature and impedance. Ablation is achieved using RF energy that can be applied on each individual electrode up to 24 electrodes simultaneously. The catheter is designed to combine diagnostic mapping capabilities of basket catheters with the simplicity of the use of balloon catheters for ablation. First-in-human experience showed that PV isolation could be performed using this new multielectrode array catheter [105]. The safety and efficacy of the catheter are still under investigation.
Although feasibility and safety were shown for these novel multielectrode RF balloon catheters, more patient data and long-term follow-up are warranted. Furthermore, randomized studies are needed to assess the potential benefit regarding procedural time, safety and efficacy of these novel catheters compared to other (balloon based) ablation techniques.
Irreversible electroporation
Irreversible electroporation (IRE), also referred to as pulsed field ablation, is a novel nonthermal ablative modality in which ultrarapid (< 1 s) electrical fields (monophasic waveforms 900–1000 V and biphasic waveforms, 800–2000 V per application) are applied to target tissue. This approach destabilizes cell membranes by forming irreversible nanoscale pores and leakage of cell contents, culminating in cell death [106]. Importantly, various tissues have specific characteristic thresholds to field strengths that induce necrosis by electroporation. Of note, myocardial tissue has the lowest threshold and is thus most sensitive tissue for irreversible electroporation. Therefore, in contrast to any other energy source, IRE spares collateral structures such as the esophagus, arteries and nerves while effectively ablating myocardial tissue. Potential benefits of IRE include the tissue selectivity of the ablation, and the rapid delivery of the energy, potentially resulting in shorter procedure times. Experimental data demonstrated that IRE can be a safe treatment modality for ablation in the vicinity of important structures such as the coronary arteries, the right phrenic nerve, and the esophagus, consistent with the tissue selectivity data derived from animal studies [107,108,109]. The first-in-human experience with IRE ablation for PVI in patients with AF was recently reported [110, 111]. Feasibility of achieving acute PVI by IRE ablation was shown using different catheter designs, including a 14-polar circular catheter [110] and an over-the-wire catheter with a deployable basket containing 20 separate electrodes [112].
Low-intensity collimated ultrasound
Low-intensity collimated ultrasound (LICU) (VytronUS, Inc., Sunnyvale, California) is a novel ablation technique designed to integrate anatomic mapping and ablation capabilities in a single catheter [113]. The catheter contains an irrigated tip with an ultrasound transducer. The catheter tip allows automatic construction of two- and three-dimensional maps of the scanned left atrial area of interest with a maximal depth of 40 mm. Ablation is performed using a highly collimated ultrasound beam that is absorbed by the atrial tissue and results in thermal injury with an estimated maximum depth of 17 mm. Ablation is performed with the support of a robotic system after definition of the ablation trajectories on a two-dimensional map by the operator. Feasibility of producing continuous transmural lesions in PVI ablation was shown in a porcine model [113]. However, available data on this novel ablation technique are limited to an experimental study. Results from the first-in-human study are awaited (Table 1).
Conclusion
Catheter ablation is an established treatment option for AF. Isolation of the PVs is the gold standard of catheter ablation of AF, but reconnection and conduction from the PVs is the dominant mechanism of recurrences of AF after PVI, especially in patients with paroxysmal AF. Novel technologies are under evaluation that have a great potential to facilitate creation of durable lesions with permanent PVI after a single ablation procedure. However, many of these novel technologies need to be tested clinically in well powered RCTs.
References
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim Y-H, McAnulty JHJ, Zheng Z-J, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJL (2014) Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129(8):837–847
Dorian P, Jung W, Newman D, Paquette M, Wood K, Ayers GM, Camm J, Akhtar M, Luderitz B (2000) The impairment of health-related quality of life in patients with intermittent atrial fibrillation: implications for the assessment of investigational therapy. J Am Coll Cardiol 36(4):1303–1309
Miyasaka Y, Barnes ME, Bailey KR, Cha SS, Gersh BJ, Seward JB, Tsang TSMM (2007) Mortality trends in patients diagnosed with first atrial fibrillation: a 21 year community-based study. J Am Coll Cardiol 49(9):986–992
Kannel WB, Wolf PA, Benjamin EJ, Levy D (1998) Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 82(8A):2N-9N
Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, Wolf PA, D’Agostino RB, Murabito JM, Kannel WB, Benjamin EJ, D’Agostino RB, Murabito JM, Kannel WB, Benjamin EJ (2003) Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 107(23):2920–2925
Sheikh A, Patel NJ, Nalluri N, Agnihotri K, Spagnola J, Patel A et al (2015) Trends in hospitalization for atrial fibrillation: epidemiology, cost, and implications for the future. Prog Cardiovasc Dis 58(2):105–116
Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G et al (1998) Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med 339(10):659–666
Calkins H, Hindricks G, Cappato R, Kim Y-H, Saad EB, Aguinaga L et al (2017) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Hear Rhythm 14(10):e275-444
Durrer D, Schoo L, Schuilenburg RM, Wellens HJ (1967) The role of premature beats in the initiation and the termination of supraventricular tachycardia in the Wolff-Parkinson-White syndrome. Circulation 36:644–662
Morris SN, Zipes DP (1973) His bundle electrocardiography during bidirectional tachycardia. Circulation 48(1):32–36
Wellens HJ, Durrer D (1975) The role of an accessory atrioventricular pathway in reciprocal tachycardia. Observations in patients with and without the Wolff-Parkinson-White syndrome. Circulation 52(1):58–72
Wellens HJ (1978) Value and limitations of programmed electrical stimulation of the heart in the study and treatment of tachycardias. Circulation 57(5):845–853
Vedel J, Frank R, Fontaine G, Fournial JF, Grosgogeat Y (1979) Permanent intra-hisian atrioventricular block induced during right intraventricular exploration. Arch Mal Coeur Vaiss 72(1):107–112
Scheinman MM, Morady F, Hess DS, Gonzalez R (1982) Catheter-induced ablation of the atrioventricular junction to control refractory supraventricular arrhythmias. JAMA 248(7):851–855
Morady F, Scheinman MM (1984) Transvenous catheter ablation of a posteroseptal accessory pathway in a patient with the Wolff-Parkinson-White syndrome. N Engl J Med 310(11):705–707
Silka MJ, Gillette PC, Garson A, Zinner A (1985) Transvenous catheter ablation of a right atrial automatic ectopic tachycardia. J Am Coll Cardiol 5(4):999–1001
Hartzler GO (1983) Electrode catheter ablation of refractory focal ventricular tachycardia. J Am Coll Cardiol 2(6):1107–1113
Fisher JD, Brodman R, Kim SG, Matos JA, Elizabeth Brodman L, Wallerson D, Waspe LE (1984) Attempted nonsurgical electrical ablation of accessory pathways via the coronary sinus in the Wolff-Parkinson-White syndrome. J Am Coll Cardiol 4(4):685–694
Warin JF, Haissaguerre M, Lemetayer P, Guillem JP, Blanchot P (1988) Catheter ablation of accessory pathways with a direct approach. Results in 35 patients. Circulation 78(4):800–815
Evans GT, Scheinman MM, Zipes DP, Benditt D, Camm AJ, El-Sherif N, Fisher J, Fontaine G, German L, Hartzler G, Josephson M, Morady F, Ruskin J (1986) Catheter ablation for control of ventricular tachycardia: a report of the percutaneous cardiac mapping and ablation registry. Pacing Clin Electrophysiol 9(6):1391–1395
Rosenqvist M, Lee MA, Moulinier L, Springer MJ, Abbott JA, Wu J, Langberg JJ, Griffin JC, Scheinman MM (1990) Long-term follow-up of patients after transcatheter direct current ablation of the atrioventricular junction. J Am Coll Cardiol 16(6):1467–1474
Coltorti F, Bardy GH, Reichenbach D, Greene HL, Thomas R, Breazeale DG, Alferness C, Ivey TD (1985) Catheter-mediated electrical ablation of the posterior septum via the coronary sinus: electrophysiologic and histologic observations in dogs. Circulation 72(3):612–622
Bardy GH, Ivey TD, Coltorti F, Stewart RB, Johnson G, Greene HL (1988) Developments, complications and limitations of catheter-mediated electrical ablation of posterior accessory atrioventricular pathways. Am J Cardiol 61(4):309–316
Bardy GH, Coltorti F, Stewart RB, Greene HL, Ivey TD (1988) Catheter-mediated electrical ablation: the relation between current and pulse width on voltage breakdown and shock-wave generation. Circ Res 63(2):409–414
Jackman WM, Wang X, Friday KJ, Roman CA, Moulton KP, Beckman KJ, McClelland JH, Twidale N, Hazlitt HA, Prior MI, Margolis PD, Calame JD, Overholt ED, Lazzara R (1991) Catheter ablation of accessory atrioventricular pathways (Wolff–Parkinson–White Syndrome) by radiofrequency current. N Engl J Med 324(23):1605–1611
Kuck KH, Schlüter M, Geiger M, Siebels J, Duckeck W (1991) Radiofrequency current catheter ablation of accessory atrioventricular pathways. Lancet (London, England) 337(8757):1557–1561
Calkins H, Sousa J, El-Atassi R, Rosenheck S, de Buitleir M, Kou WH, Kadish AH, Langberg JJ, Morady F (1991) Diagnosis and cure of the Wolff-Parkinson-White syndrome or paroxysmal supraventricular tachycardias during a single electrophysiologic test. N Engl J Med 324(23):1612–1618
Hindricks G (1993) The Multicentre European Radiofrequency Survey (MERFS): complications of radiofrequency catheter ablation of arrhythmias. The Multicentre European Radiofrequency Survey (MERFS) investigators of the Working Group on Arrhythmias of the European Society of C. Eur Heart J. 14(12):1644–1653
Scheinman MM (1995) NASPE survey on catheter ablation. Pacing Clin Electrophysiol 18(8):1474–1478
Cox JL, Canavan TE, Schuessler RB, Cain ME, Lindsay BD, Stone C, Smith PK, Corr PB, Boineau JP (1991) The surgical treatment of atrial fibrillation. II. Intraoperative electrophysiologic mapping and description of the electrophysiologic basis of atrial flutter and atrial fibrillation. J Thorac Cardiovasc Surg 101(3):406–426
Sundt TM, Camillo CJ, Cox JL (1997) The maze procedure for cure of atrial fibrillation. Cardiol Clin 15(4):739–748
Schuessler RB, Grayson TM, Bromberg BI, Cox JL, Boineau JP (1992) Cholinergically mediated tachyarrhythmias induced by a single extrastimulus in the isolated canine right atrium. Circ Res 71(5):1254–1267
Schuessler RB, Kawamoto T, Hand DE, Mitsuno M, Bromberg BI, Cox JL, Boineau JP (1993) Simultaneous epicardial and endocardial activation sequence mapping in the isolated canine right atrium. Circulation 88(1):250–263
Allessie MA, Bonke FI, Schopman FJ (1977) Circus movement in rabbit atrial muscle as a mechanism of tachycardia. III. The “leading circle” concept: a new model of circus movement in cardiac tissue without the involvement of an anatomical obstacle. Circ Res 41(1):9–18
Allessie M, Lammers W, Smeets J, Bonke F, Hollen J (1982) Total mapping of atrial excitation during acetylcholine-induced atrial flutter and fibrillation in the isolated canine heart. In: Olsson SB, Schlepper M (eds) Kulbertus HE. Atr Fibrillation Molndal, Sweden Lindgren Soner, pp 4–62
Allessie M, Lammers W, Bonke F, Hollen J (1985) Experimental evaluation of Moe’s multiple wavelet hypothesis of atrial fibrillation. In: Jalife J (ed) Zipes DP. Card Electrophysiol Arrhythmias New York, Grune Strat, pp 265–275
Cox JL, Jaquiss RDB, Schuessler RB, Boineau JP (1995) Modification of the maze procedure for atrial flutter and atrial fibrillation. J Thorac Cardiovasc Surg 110(2):485–495
Prasad SM, Maniar HS, Camillo CJ, Schuessler RB, Boineau JP, Sundt TM, Cox JL, Damiano RJ (2003) The Cox maze III procedure for atrial fibrillation: long-term efficacy in patients undergoing lone versus concomitant procedures. J Thorac Cardiovasc Surg 126(6):1822–1827
Morillo CA, Klein GJ, Jones DL, Guiraudon CM (1995) Chronic rapid atrial pacing. Structural, functional, and electrophysiological characteristics of a new model of sustained atrial fibrillation. Circulation 91(5):1588–1595
Elvan A, Pride HP, Eble JN, Zipes DP (1995) Radiofrequency catheter ablation of the atria reduces inducibility and duration of atrial fibrillation in dogs. Circulation 91(8):2235–2244
Haïssaguerre M, Gencel L, Fischer B, Le Métayer P, Poquet F, Marcus FI, Clémenty J (1994) Successful catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 5(12):1045–1052
Swartz JF, Pellersels G, Silvers J, Patten L, Cervantez D (1993) A catheter-based curative approach to atrial fibrillation in humans [abstract]. Circulation 88(Suppl I):I-335
Haïssaguerre M, Jaís P, Shah DC, Gencel L, Pradeau V, Garrigues S, Chouairi S, Hocini M, Métayer P, Roudaut R, Clémenty J (1996) Right and left atrial radiofrequency catheter therapy of paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 7(12):1132–1144
Jais P, Shah DC, Takahashi A, Hocini M, Haissaguerre M, Clementy J (1998) Long-term follow-up after right atrial radiofrequency catheter treatment of paroxysmal atrial fibrillation. Pacing Clin Electrophysiol 21(11):2533–2538
Natale A, Leonelli F, Beheiry S, Newby K, Pisano E, Potenza D, Rajkovich K, Wides B, Cromwell L, Tomassoni G (2000) Catheter ablation approach on the right side only for paroxysmal atrial fibrillation therapy: long-term results. Pacing Clin Electrophysiol 23(2):224–233
Jaïs P, Haïssaguerre M, Shah DC, Chouairi S, Gencel L, Hocini M, Cle´menty J (1997) A focal source of atrial fibrillation treated by discrete radiofrequency ablation. Circulation 95(3):572–576
Pappone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, Vicedomini G, Salvati A, Dicandia C, Mazzone P, Santinelli V, Gulletta S, Chierchia S (2000a) Circumferential radiofrequency ablation of pulmonary vein ostia. Circulation 102(21):2619–2628
Krittayaphong R, Raungrattanaamporn O, Bhuripanyo K, Sriratanasathavorn C, Pooranawattanakul S, Punlee K, Kangkagate C (2003) A randomized clinical trial of the efficacy of radiofrequency catheter ablation and amiodarone in the treatment of symptomatic atrial fibrillation. J Med Assoc Thai 86(Suppl 1):S8-16
Wazni OM, Marrouche NF, Martin DO, Verma A, Bhargava M, Saliba W et al (2005) Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation. JAMA 293(21):2634
Jaïs P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, Hocini M, Extramiana F, Sacher F, Bordachar P, Klein G, Weerasooriya R, Clémenty J, Haïssaguerre M (2008) Catheter ablation versus antiarrhythmic drugs for atrial fibrillation. Circulation 118(24):2498–2505
Pappone C, Rosanio S, Augello G, Gallus G, Vicedomini G, Mazzone P, Gulletta S, Gugliotta F, Pappone A, Santinelli V, Tortoriello V, Sala S, Zangrillo A, Crescenzi G, Benussi S, Alfieri O (2003) Mortality, morbidity, and quality of life after circumferential pulmonary vein ablation for atrial fibrillation: outcomes from a controlled nonrandomized long-term study. J Am Coll Cardiol 42(2):185–197
Pappone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, Vicedomini G, Salvati A, Dicandia C, Mazzone P, Santinelli V, Gulletta S, Chierchia S (2000b) Circumferential radiofrequency ablation of pulmonary vein ostia: a new anatomic approach for curing atrial fibrillation. Circulation 102(21):2619–2628
Nademanee K, McKenzie J, Kosar E, Schwab M, Sunsaneewitayakul B, Vasavakul T, Khunnawat C, Ngarmukos T (2004) A new approach for catheter ablation of atrial fibrillation: mapping of the electrophysiologic substrate. J Am Coll Cardiol 43(11):2044–2053
Jaïs P, Hocini M, Hsu LF, Sanders P, Scavee C, Weerasooriya R, Macle L, Raybaud F, Garrigue S, Shah DC, Le MP, Clémenty J, Haïssaguerre M (2004) Technique and results of linear ablation at the mitral isthmus. Circulation 110(19):2996–3002
Scherr D, Khairy P, Miyazaki S, Aurillac-Lavignolle V, Pascale P, Wilton SB et al (2015) Five-year outcome of catheter ablation of persistent atrial fibrillation using termination of atrial fibrillation as a procedural endpoint. Circ Arrhythmia Electrophysiol 8(1):18–24
Zhao Y, Di Biase L, Trivedi C, Mohanty S, Bai R, Mohanty P et al (2016) Importance of non-pulmonary vein triggers ablation to achieve long-term freedom from paroxysmal atrial fibrillation in patients with low ejection fraction. Hear Rhythm 13(1):141–149
Verma A, Jiang C, Betts TR, Chen J, Deisenhofer I, Mantovan R, Macle L, Morillo CA, Haverkamp W, Weerasooriya R, Albenque J-P, Nardi S, Menardi E, Novak P, Sanders P, STAR AF II Investigators (2015) Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med 372(19):1812–1822
Kottkamp H, Schreiber D (2016) The substrate in “early persistent” atrial fibrillation: arrhythmia induced, risk factor induced, or from a specific fibrotic atrial cardiomyopathy? JACC Clin Electrophysiol 2(2):140–142
Narayan SM, Krummen DE, Clopton P, Shivkumar K, Miller JM (2013) Direct or coincidental elimination of stable rotors or focal sources may explain successful atrial fibrillation ablation. J Am Coll Cardiol 62(2):138–147
Chen P-S, Chen LS, Fishbein MC, Lin S-F, Nattel S (2014) Role of the autonomic nervous system in atrial fibrillation. Circ Res 114(9):1500–1515
Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE et al (2019) Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation. JAMA 321(13):1261
Mark DB, Anstrom KJ, Sheng S, Piccini JP, Baloch KN, Monahan KH, Daniels MR, Bahnson TD, Poole JE, Rosenberg Y, Lee KL, Packer DL; CABANA Investigators (2019) Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 321(13):1275–1285
Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D et al (2016) Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device: results from the AATAC multicenter randomized trial. Circulation 133(17):1637–1644
Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, Merkely B, Pokushalov E, Sanders P, Proff J, Schunkert H, Christ H, Vogt J, Bansch D (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 378(5):417–427
Haines DE (1993) The biophysics of radiofrequency catheter ablation in the heart: the importance of temperature monitoring. Pacing Clin Electrophysiol 16(3):586–591
Nakagawa H, Yamanashi WS, Pitha JV, Arruda M, Wang X, Ohtomo K, Beckman KJ, McClelland JH, Lazzara R, Jackman WM (1995) Comparison of in vivo tissue temperature profile and lesion geometry for radiofrequency ablation with a saline-irrigated electrode versus temperature control in a canine thigh muscle preparation. Circulation 91(8):2264–2273
Yokoyama K, Nakagawa H, Shah DC, Lambert H, Leo G, Aeby N, Ikeda A, Pitha JV, Sharma T, Lazzara R, Jackman WM (2008) Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ Arrhythm Electrophysiol 1(5):354–362
Arujuna A, Karim R, Caulfield D, Knowles B, Rhode K, Schaeffter T, Kato B, Rinaldi CA, Cooklin M, Razavi R, O’Neill MD, Gill J (2012) Acute pulmonary vein isolation is achieved by a combination of reversible and irreversible atrial injury after catheter ablation: evidence from magnetic resonance imaging. Circ Arrhythm Electrophysiol 5(4):691–700
Gerstenfeld EP, Callans DJ, Dixit S, Zado E, Marchlinski FE (2003) Incidence and location of focal atrial fibrillation triggers in patients undergoing repeat pulmonary vein isolation: implications for ablation strategies. J Cardiovasc Electrophysiol 14(7):685–690
Callans DJ, Gerstenfeld EP, Dixit S, Zado E, Vanderhoff M, Ren J-F, Marchlinski FE (2004) Efficacy of repeat pulmonary vein isolation procedures in patients with recurrent atrial fibrillation. J Cardiovasc Electrophysiol 15(9):1050–1055
Buist TJ, Adiyaman A, Smit JJJ, Ramdat Misier AR, Elvan A (2018) Arrhythmia-free survival and pulmonary vein reconnection patterns after second-generation cryoballoon and contact-force radiofrequency pulmonary vein isolation. Clin Res Cardiol. 107(6):498–506
Natale A, Reddy VY, Monir G, Wilber DJ, Lindsay BD, McElderry HT, Kantipudi C, Mansour MC, Melby DP, Packer DL, Nakagawa H, Zhang B, Stagg RB, Boo LM, Marchlinski FE (2014) Paroxysmal AF catheter ablation with a contact force sensing catheter. J Am Coll Cardiol 64(7):647–656
Kuck K-H, Reddy VY, Schmidt B, Natale A, Neuzil P, Saoudi N, Kautzner J, Herrera C, Hindricks G, Jaïs P, Nakagawa H, Lambert H, Shah DC (2012) A novel radiofrequency ablation catheter using contact force sensing: toccata study. Hear Rhythm 9(1):18–23
Reddy VY, Dukkipati SR, Neuzil P, Natale A, Albenque J-P, Kautzner J, Shah D, Michaud G, Wharton M, Harari D, Mahapatra S, Lambert H, Mansour M (2015) Randomized, controlled trial of the safety and effectiveness of a contact force-sensing irrigated catheter for ablation of paroxysmal atrial fibrillation. Circulation 132(10):907–915
Deshmukh A, Patel NJ, Pant S, Shah N, Chothani A, Mehta K et al (2013) In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010. Circulation 128(19):2104–2112
Wazni OM, Rossillo A, Marrouche NF, Saad EB, Martin DO, Bhargava M et al (2005) Embolic events and char formation during pulmonary vein isolation in patients with atrial fibrillation: impact of different anticoagulation regimens and importance of intracardiac echo imaging. J Cardiovasc Electrophysiol 16(6):576–581
Pappone C, Oral H, Santinelli V, Vicedomini G, Lang CC, Manguso F, Torracca L, Benussi S, Alfieri O, Hong R, Lau W, Hirata K, Shikuma N, Hall B, Morady F (2004) Atrio-esophageal fistula as a complication of percutaneous transcatheter ablation of atrial fibrillation. Circulation 109(22):2724–2726
Tamborero D, Mont L, Nava S, de Caralt TM, Molina I, Scalise A, Perea RJ, Bartholomay E, Berruezo A, Matiello M, Brugada J (2005) Incidence of pulmonary vein stenosis in patients submitted to atrial fibrillation ablation: a comparison of the selective segmental ostial ablation vs the circumferential pulmonary veins ablation. J Interv Card Electrophysiol 14(1):21–25
Herrera Siklódy C, Deneke T, Hocini M, Lehrmann H, Shin DI, Miyazaki S, Henschke S, Fluegel P, Schiebeling-Römer J, Bansmann PM, Bourdias T, Dousset V, Hassaguerre M, Arentz T (2011) Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. J Am Coll Cardiol 58(7):681–688
Haines DE, Stewart MT, Ahlberg S, Barka ND, Condie C, Fiedler GR, Kirchhof NA, Halimi F, Deneke T (2013) Microembolism and catheter ablation I: a comparison of irrigated radiofrequency and multielectrode-phased radiofrequency catheter ablation of pulmonary vein ostia. Circ Arrhythmia Electrophysiol 6(1):16–22
Boersma LV, van der Voort P, Debruyne P, Dekker L, Simmers T, Rossenbacker T, Balt J, Wijffels M, Degreef Y (2016) Multielectrode pulmonary vein isolation versus single tip wide area catheter ablation for paroxysmal atrial fibrillation: a multinational multicenter randomized clinical trial. Circ Arrhythm Electrophysiol 9(4):e003151
De Ponti R (2005) Cryothermal energy ablation of cardiac arrhythmias 2005: state of the art. Indian Pacing Electrophysiol J 5(1):12–24
Kuck K-H, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KRJ, Elvan A, Arentz T, Bestehorn K, Pocock SJ, Albenque J-P, Tondo C (2016) Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med 374(23):2235–2245
Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG, Dubuc M, Reddy V, Nelson L, Holcomb RG, Lehmann JW, Ruskin JN, STOP AF Cryoablation (2013) Investigators cryoballoon. Ablation of pulmonary veins for paroxysmal atrial fibrillation. J Am Coll Cardiol 61(16):1713–1723
Kuck K-H, Furnkranz A, Chun KRJ, Metzner A, Ouyang F, Schluter M, Elvan A, Lim HW, Kueffer FJ, Arentz T, Albenque J-P, Tondo C, Kuhne M, Sticherling C, Brugada J (2016) Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur Heart J 37(38):2858–2865
Heeger C, Pott A, Rillig A, Metzner A, Cay S, Grosse N, Miyazaki S, Arash A, Ehrlich J, Wirth H, Tscholl V, Kuck K, Dahm T, Tilz R (2019) Phrenic nerve injury during pulmonary vein isolation using the second-generation cryoballoon: first results of the worldwide YETI registry. Abstract presented at: European Heart Rhythm Association Congress, Lisbon, Portugal.
Dukkipati SR, Cuoco F, Kutinsky I, Aryana A, Bahnson TD, Lakkireddy D, Woollett I, Issa ZF, Natale A, Reddy VY (2015) Pulmonary vein isolation using the visually guided laser balloon: a prospective, multicenter, and randomized comparison to standard radiofrequency ablation. J Am Coll Cardiol 66(12):1350–1360
Bordignon S, Chun K-RJ, Gunawardene M, Urban V, Kulikoglu M, Miehm K, Brzank B, Schulte-Hahn B, Nowak B, Schmidt B (2013) Energy titration strategies with the endoscopic ablation system: lessons from the high-dose vs. low-dose laser ablation study. EP Eur 15(5):685–689
Reynolds MR, Zheng Q, Doros G (2018) Laser balloon ablation for AF: a systematic review and meta-analysis. J Cardiovasc Electrophysiol 29(10):1363–1370
El Haddad M, Taghji P, Phlips T, Wolf M, Demolder A, Choudhury R, Knecht S, Vandekerckhove Y, Tavernier R, Nakagawa H, Duytschaever M (2017) Determinants of acute and late pulmonary vein reconnection in contact force-guided pulmonary vein isolation: identifying the weakest link in the ablation chain. Circ Arrhythmia Electrophysiol 10(4):e004867
Santoro F, Metzner A, Brunetti ND, Heeger CH, Mathew S, Reissmann B, Lemeš C, Maurer T, Fink T, Rottner L, Inaba O, Kuck KH, Ouyang F, Rillig A (2019) Left atrial anterior line ablation using ablation index and inter-lesion distance measurement. Clin Res Cardiol 108(9):1009–1016
Nakagawa H, Jackman WM (2014) The role of contact force in atrial fibrillation ablation. Journal of Atrial Fibrillation. 7:78–84 ((CardioFront LLC))
Das M, Loveday JJ, Wynn GJ, Gomes S, Saeed Y, Bonnett LJ, Waktare JEP, Todd DM, Hall MCS, Snowdon RL, Modi S, Gupta D (2017) Ablation index, a novel marker of ablation lesion quality: prediction of pulmonary vein reconnection at repeat electrophysiology study and regional differences in target values. Europace 19(5):775–783
Hussein A, Das M, Riva S, Morgan M, Ronayne C, Sahni A, Shaw M, Todd D, Hall M, Modi S, Natale A, Dello Russo A, Snowdon R, Gupta D (2018) Use of ablation index-guided ablation results in high rates of durable pulmonary vein isolation and freedom from arrhythmia in persistent atrial fibrillation patients. Circ Arrhythm Electrophysiol 11(9):e006576
Phlips T, Taghji P, El Haddad M, Wolf M, Knecht S, Vandekerckhove Y, Tavernier R, Duytschaever M (2018) Improving procedural and 1 year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. EP Eur. 20(FI_3):f419–f427
Pranata R, Vania R, Huang I (2019) Ablation-index guided versus conventional contact-force guided ablation in pulmonary vein isolation—systematic review and meta-analysis. Indian Pacing Electrophysiol J 19(4):155–160
Barkagan M, Contreras-Valdes FM, Leshem E, Buxton AE, Nakagawa H, Anter E (2018) High-power and short-duration ablation for pulmonary vein isolation: safety, efficacy, and long-term durability. J Cardiovasc Electrophysiol 29(9):1287–1296
Winkle RA, Mohanty S, Patrawala RA, Mead RH, Kong MH, Engel G, Salcedo J, Trivedi CG, Gianni C, Jais P, Natale A, Day JD (2019) Low complication rates using high power (45–50 W) for short duration for atrial fibrillation ablations. Hear Rhythm 16(2):165–169
Vassallo F, Cunha C, Serpa E, Meigre LL, Carloni H, Simoes A, Hespanhol D, Lovatto CV, Batista W, Serpa R (2019) Comparison of high-power short-duration (HPSD) ablation of atrial fibrillation using a contact force-sensing catheter and conventional technique: initial results. J Cardiovasc Electrophysiol 30(10):1877–1883
Ali-Ahmed F, Goyal V, Patel M, Orelaru F, Haines DE, Wong WS (2019) High-power, low-flow, short-ablation duration—the key to avoid collateral injury? J Interv Card Electrophysiol 55(1):9–16
Reddy VY, Grimaldi M, De Potter T, Vijgen JM, Bulava A, Duytschaever MF, Martinek M, Natale A, Knecht S, Neuzil P, Pürerfellner H (2019) Pulmonary vein isolation with very high power, short duration, temperature-controlled lesions: the QDOT-FAST trial. JACC Clin Electrophysiol 5(7):778–786
Kottmaier M, Popa M, Bourier F, Reents T, Cifuentes J, Semmler V, Telishevska M, Otgonbayar U, Koch-Büttner K, Lennerz C, Bartkowiak M, Kornmayer M, Rousseva E, Brkic A, Grebmer C, Kolb C, Hessling G, Deisenhofer I (2020) Safety and outcome of very high-power short-duration ablation using 70 W for pulmonary vein isolation in patients with paroxysmal atrial fibrillation. Eur Eur pacing, arrhythmias, Card Electrophysiol J Work groups Card pacing, arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol 22(3):388–393
Reddy VY, Schilling R, Grimaldi M, Horton R, Natale A, Riva S, Tondo C, Kuck K-H, Neuzil P, McInnis K, Bishara M, Zhang B, Govari A, Abdelaal A, Mansour M (2019) Pulmonary vein isolation with a novel multielectrode radiofrequency balloon catheter that allows directionally tailored energy delivery: short-term outcomes from a multicenter first-in-human study (RADIANCE). Circ Arrhythm Electrophysiol 12(12):e007541
Al-Ahmad A. Assessment of the safety and performance of a novel RF balloon catheter system t [Internet]. Abstract presented at: European Heart Rhythm Association Congress, Lisbon, Portugal. 2019; Available from: https://esc365.escardio.org/Congress/EHRA-2019/Late-breaking-trials-1/191500-assessment-of-the-safety-and-performance-of-a-novel-rf-balloon-catheter-system-to-isolate-pulmonary-veins-results-of-the-multicenter-af-ficient-1-trial
Kottkamp H, Moser F, Rieger A, Schreiber D, Pönisch C, Trofin M (2017) Global multielectrode contact mapping plus ablation with a single catheter: preclinical and preliminary experience in humans with atrial fibrillation. J Cardiovasc Electrophysiol 28(11):1247–1256
Gallagher JJ, Svenson RH, Kasell JH, German LD, Bardy GH, Broughton A, Critelli G (1982) Catheter technique for closed-chest ablation of the atrioventricular conduction system. N Engl J Med 306(4):194–200
du Pre BC, van Driel VJ, van Wessel H, Loh P, Doevendans PA, Goldschmeding R, Wittkampf FH, Vink A (2013) Minimal coronary artery damage by myocardial electroporation ablation. Eur Eur pacing, arrhythmias, Card Electrophysiol J Work groups Card pacing, arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol 15(1):144–149
van Driel VJHM, Neven K, van Wessel H, Vink A, Doevendans PAFM, Wittkampf FHM (2015) Low vulnerability of the right phrenic nerve to electroporation ablation. Hear Rhythm 12(8):1838–1844
Neven K, van Es R, van Driel V, van Wessel H, Fidder H, Vink A, Doevendans P, Wittkampf F (2017) Acute and long-term effects of full-power electroporation ablation directly on the porcine esophagus. Circ Arrhythm Electrophysiol 10(5):e004672
Loh P, van Es R, Groen MHA, Neven K, van Driel VJ, van Wessel H, Doevendans PA, Wittkampf FHM. Pulmonary vein isolation by irreversible electroporation: first-in-human experience. [Internet]. Abstract presented at: heart rhythm society scientific sessions. May 10 2019. San Francisco, CA.; 2019; Available from: https://www.abstractsonline.com/pp8/#!/5753/presentation/22439
Reddy VY, Neuzil P, Koruth JS, Petru J, Funosako M, Cochet H, Sediva L, Chovanec M, Dukkipati SR, Jais P (2019) Pulsed field ablation for pulmonary vein isolation in atrial fibrillation. J Am Coll Cardiol 74(3):315–326
Reddy VY, Koruth J, Jais P, Petru J, Timko F, Skalsky I, Hebeler R, Labrousse L, Barandon L, Kralovec S, Funosako M, Mannuva BB, Sediva L, Neuzil P (2018) Ablation of atrial fibrillation with pulsed electric fields. JACC Clin Electrophysiol 4(8):987–995
Koruth JS, Schneider C, Avitall B, Ribeiro L, Dukkipati S, Walcott GP, Phillips P, McElderry HT, Reddy VY (2015) Pre-clinical investigation of a low-intensity collimated ultrasound system for pulmonary vein isolation in a porcine model. JACC Clin Electrophysiol 1(4):306–314
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Buist, T.J., Zipes, D.P. & Elvan, A. Atrial fibrillation ablation strategies and technologies: past, present, and future. Clin Res Cardiol 110, 775–788 (2021). https://doi.org/10.1007/s00392-020-01751-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01751-5