Abstract
Background
Vitamin K antagonists (VKAs) are susceptible to drug–drug interactions. Non-VKA oral anticoagulants (NOACs) have a decreased sensitivity to pharmacokinetic interactions and might be therefore considered superior in patients treated with multiple drugs. The objective of this study was to compare the risk of serious bleeding associated with interacting drugs in German nursing home residents treated with VKA or NOAC.
Methods
Using claims data of new nursing home residents aged ≥ 65 years (2010–2014) we conducted separate nested case–control analyses within two cohorts of patients treated with VKA or NOAC, respectively. Cases were defined as patients hospitalized for serious bleeding. For each case, up to 20 controls were selected by risk-set sampling. Conditional logistic regression was used to obtain confounder-adjusted odds ratios (aORs) and 95% confidence intervals (CI) for the risk of bleeding associated with VKA or NOAC use and interacting drugs compared with the use of the respective oral anticoagulant alone.
Results
Among 127,227 new nursing home residents, 16,804 patients received oral anticoagulation. Based on 372 cases and 7281 matched controls, the highest risk of bleeding in VKA users was observed for the concomitant use of antibiotics (aOR 3.00; CI 2.11–4.27) vs. VKA use alone, followed by non-steroidal anti-inflammatory drugs (1.66; 1.13–2.43). Among 243 NOAC cases and 4776 matched controls, elevated risks for bleeding were observed for the use of heparins (2.05; 1.25–3.36) and platelet inhibitors (1.92; 1.36–2.72).
Conclusions
Concomitant medication needs to be prescribed cautiously and monitored closely in nursing home residents treated with oral anticoagulants.
Graphic Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral anticoagulants used to treat and prevent thromboembolic diseases are widely prescribed [1,2,3,4]. As with all antithrombotic drugs, effective therapy has to be balanced against the risk of bleeding. According to a recent analysis, oral anticoagulants are the drug class most commonly involved in emergency department visits for adverse drug events in the United States mainly because of bleeding events [5]. For all oral anticoagulants, drug interactions are known and require vigilance and often, intervention [6]. Especially the vitamin K antagonists (VKA) used for more than 60 years are susceptible to drug–drug or drug–food interactions via pharmacodynamic and pharmacokinetic mechanisms [7, 8]. While a pharmacodynamic interaction occurs when interacting drugs have either additive or opposing effects, pharmacokinetic interactions include the inhibition or induction of the other drug’s metabolism via the cytochrome P450 (CYP) pathway and efflux pumps such as P-glycoproteins (P-gp) [6, 9].
In recent years, non-vitamin k antagonist oral anticoagulants (NOACs) have been developed which have a decreased sensitivity to pharmacokinetic interactions [10] and might be therefore considered superior in patients treated with multiple drugs. While most drug interactions with VKAs can be detected by deviations of the international normalized ratio (INR), regular measurements of NOAC plasma concentrations or biological effects, either via quantitative or qualitative methods, are not available in routine practice, although several patient subgroups could benefit from these tests [11]. Consequently, drug interactions increasing or decreasing the anticoagulant effects of NOACs will be detected only if complications, either bleeding or thromboembolic events, occur [12].
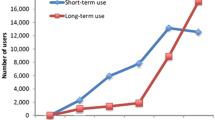
In Germany, NOAC prescriptions increased substantially in the last years [4, 13]. Among other populations, NOACs are also increasingly prescribed to nursing home residents, who are typically characterized by a high prevalence of indications requiring anticoagulation [14,15,16]. Moreover, considering age and common conditions such as a decreased renal function, an elevated risk of bleeding may be assumed in these very vulnerable patients. Further, comorbidities involving several treatments may lead to polypharmacy including long-term, short-term, and as-needed medication. A recent study found polypharmacy (5–9 drugs) in 53.3% and excessive polypharmacy (≥ 10 drugs) in 16.4% of German nursing home residents [17].
Our study aimed to compare drug interactions leading to bleeding events between VKA and NOAC users in the vulnerable population of nursing home residents.
Methods
Data source
We used data from the DAK-Gesundheit, a large statutory health insurance (SHI) provider enrolling over 6 million persons (about 7% of the German population). The provided data include complete demographic characteristics as well as information on hospital admissions, outpatient physician visits, and outpatient prescriptions. Hospital data encompass the dates of admission and discharge with their corresponding diagnoses. Outpatient diagnoses including the diagnostic certainty (confirmed/suspected/ruled out/status post) are reimbursed on a quarterly basis and therefore can only be referred to a quarter of a year and not to an exact date. All diagnoses are coded according to the German modification of the International Classification of Diseases (ICD-10 GM). Prescription data contain prescribed drugs reimbursed by the SHI, which can be linked to the anatomical–therapeutic–chemical (ATC) code and the defined daily dose (DDD). In-hospital medication is not included in the data.
Source population and study cohorts
The source population encompassed new nursing home residents from 2010 to 2014 aged 65 years or older with a continuous insurance period of at least 1 year before nursing home admission. Two study cohorts were established: patients were included in the cohort of VKA users if they received at least one prescription of the vitamin K antagonists phenprocoumon (ATC code: B01AA04) or warfarin (B01AA03) during their nursing home stay. Patients treated with the factor Xa inhibitors rivaroxaban (B01AF01, B01AX06) or apixaban (B01AF02) or the direct thrombin inhibitor (factor IIa) dabigatran (B01AE07) were included in the cohort of NOAC users. As done in a previous study, NOACs used for orthopedic indications were excluded [16]. Depending on the first class of oral anticoagulant prescribed in the nursing home, a patient was assigned to either the cohort of VKA users or the cohort of NOAC users. The date of the first prescription was used as cohort entry, whereas cohort exit was set as the first of the following: (1) end of the first continuous treatment episode with the respective class of oral anticoagulant, (2) end of study period, (3) end of insurance including death, or (4) hospitalization for bleeding.
Since the initial phase of anticoagulation has been associated with an increased risk of bleeding [18], we distinguished between incident and prevalent oral anticoagulant use at cohort entry. Patients were classified as incident oral anticoagulant users if they had not received an oral anticoagulant prescription in the year before cohort entry, whereas the other patients were considered prevalent users. Prevalent users were excluded from their respective study cohort if they had switched the class of oral anticoagulant with nursing home entry, since switching was found to be influenced by aspects such as intended higher effectiveness and safety [16].
Prescriptions’ durations starting with the prescription date were estimated by the number of prescribed DDDs, assuming that patients received 0.75 DDDs per day, which, for example, corresponds to 2.25 mg phenprocoumon or 15 mg rivaroxaban. This assumption was based on preliminary analyses using the time from the first prescription until the day before the last prescription as well as the number of prescribed DDDs excluding the last prescription for VKAs and NOACs, respectively. Allowing a grace period of maximum 14 days, subsequent prescriptions were considered as continuous treatment. In case patients switched their class of oral anticoagulant before a prescription’s estimated end, the respective treatment episode was assumed to have ended on the day before the switch.
Definition of cases and controls
Within the two study cohorts, we conducted separate nested case–control studies. Cases were defined as any bleeding leading to hospitalization (as reflected by the main discharge diagnosis) and were categorized as intracerebral, gastrointestinal, urogenital, and other serious bleeding (Supplemental Table 1). The day of the hospital admission was determined as index day. Up to 20 controls were matched to each case by age (± 2 years), sex, and treatment status at the time of cohort entry (incident or prevalent use) using risk-set sampling. Therefore, an index day was assigned to each control resulting in the same length of follow-up as for the corresponding case. Patients could serve as controls for multiple cases and were eligible to be selected as controls before becoming a case [19].
Interacting drugs and confounder assessment
Based on literature on potential drug interactions with oral anticoagulants [6, 20,21,22], concomitant use of the following drugs was assessed: heparins including derivatives (ATC code: B01AB), platelet inhibitors (B01AC), non-selective non-steroidal anti-inflammatory drugs (NSAIDs, M01A, excluding M01AH), antibiotics (J01) and antimycotics (imidazole and triazole derivatives, J02AB, J02AC), selective serotonin reuptake inhibitors (SSRIs, N06AB), and amiodarone/dronedarone (C01BD01, C01BD07). Further, use of proton pump inhibitors (PPI, A02BC) was assessed to account for treatment or prophylaxis of upper gastrointestinal (GI) problems. Assuming a daily dose of one DDD, a potential drug–drug interaction resulting in hospital admission for bleeding was assumed if the drug supply overlapped the index day.
Potential confounders associated with an increased risk of bleeding including hypertension, renal or liver impairment, stroke (ischemic or unspecified), and bleeding history (or a predisposition thereof) were assessed from confirmed outpatient diagnoses in the two quarters preceding the quarter of the index day (Supplemental Table 1). Further, the care level (range: 0/1 (limited daily living skills/substantial need of care) to 3 (most severe need of care) [23]) was determined in this time period. Finally, we assessed whether patients received oral anticoagulation because of atrial fibrillation (AF) at cohort entry [16]. As recommended for pharmacoepidemiological studies using observational routinely collected health data, the study timelines are illustrated in Fig. 1 [24].
Statistical analysis
Bleeding rates per 100 person-years were calculated for each class of oral anticoagulants stratified by sex and bleeding site. Considering potential confounders, adjusted odds ratios (aORs) and 95% confidence intervals (CIs) of hospitalization for bleeding associated with current use of each potentially interacting drug were calculated using conditional logistic regression. We used the logistic procedure (SAS 9.4, SAS Institute Inc., Cary, NC, USA), specified a significance level of 0.05, and included the predefined drugs and confounders as fixed variables. For each analysis, the reference category was current non-use of the respective potentially interacting drug at the index date.
Subgroup and sensitivity analyses
Subgroup analyses were based on (1) patients with a recorded diagnosis of AF at cohort entry and (2) those without a respective diagnosis, respectively. Since individual substances of the VKA and NOAC groups differ with respect to their pharmacokinetic profiles, we further included analyses based on the individual agents. In sensitivity analyses, daily doses of (1) 1.5 and (2) 0.5 DDDs were assumed for the determination of continuous treatment with oral anticoagulants. As proposed by Ihle et al., we further calculated the prescribed daily dose (PDD) for every prescription with a subsequent prescription [25]. After stratifying the PDDs’ percentiles by ATC code and by sorting the prescription periods by descending PDD, the percentiles were ranked. The 20th percentile therefore represented the daily dose’s upper range and the 80th percentile the daily dose’s lower range, respectively [25]. Characteristics of study drugs and the daily doses resulting from these exposure assumptions are displayed in Supplemental Table 3.
Last, daily doses of (1) 0.75 and (2) 1.5 DDDs were assumed for the interacting medication.
Results
Cohort characteristics and bleeding rates
From 127,227 new nursing home residents, 16,804 users of oral anticoagulants were determined; baseline characteristics for these users have been described previously [16]. A total of 927 patients were excluded because they switched oral anticoagulant class when entering the nursing home, resulting in two cohorts of (1) 9739 VKA and (2) 6138 NOAC users.
Bleeding rates were higher in patients treated with VKAs (9.68; 95% CI 8.73–10.72 per 100 person-years) than in those receiving NOACs (7.85; 95% CI 6.89–8.90 per 100 person-years, Table 1). In both user cohorts, rates were higher in males and in patients aged 85 or older. In VKA users, the bleeding rate was slightly higher in patients with AF than in those with other indications, whereas the picture was reversed in NOAC-treated patients. Neither comparison reached statistical significance. Considering bleeding sites, rates for intracerebral bleeding were significantly higher in users of VKA (1.16, 95% 0.85–1.56 per 100 person-years) than in those receiving NOACs (0.48; 95% CI: 0.27–0.80 per 100 person-years) as were the rates for other bleeding (Supplemental Fig. 1). In contrast, GI and urogenital bleeding were slightly less common in users of VKA than in those receiving NOAC treatment without reaching statistical significance.
On a cohort basis, about 77% of VKA and NOAC users had a diagnosis of AF. Venous thromboembolism (VTE) and acute coronary syndrome (ACS) were significantly less common in patients treated with VKA than in those receiving NOACs (12.7% vs. 16.8% and 7.5% vs. 8.6%, respectively, Supplemental Table 2). In contrast, a prosthetic heart valve was significantly more often found in VKA than in NOAC users (4.7% vs. 1.4%).
The nested case–control study of VKA users included 372 cases and 7281 controls with a mean age of 84.2 years. Nearly 72% were female and about 34% had a care level of 2 or 3 (Table 2). Among 243 NOAC cases and 4776 matched controls (mean age: 85.1 years), 76% were female and 45% had a care level higher than 1.
Interactions
In VKA users, bleeding was associated with concomitant NSAID treatment (aOR 1.66; 95% CI 1.13–2.43), heparins (1.48; 1.09–2.00) and PPIs (1.31; 1.06–1.63, Table 2). The highest aOR, however, was observed for co-treatment with antibiotics (3.00; 2.11–4.27). Among antibiotic drugs, the highest risks were observed for sulfonamides (crude OR: 8.75; 3.6–21.27), cephalosporins (3.56; 1.85–6.84), and quinolones (3.44; 1.67–7.08, data not shown). A significantly decreased risk, however with wide confidence intervals, was observed for amiodarone.
In NOAC users, an increased risk of bleeding was observed when patients were co-prescribed platelet inhibitors (1.92; 1.36–2.72) or heparins (2.05; 1.25–3.36). With aORs of 1.93 (1.48–2.52) and 2.85 (2.05–3.95) in VKA and NOAC users, respectively, previous bleeding or the predisposition thereof was the only condition significantly increasing the risk of bleeding. With respect to prescribing frequencies, heparins were far more often prescribed to VKA users, whereas PPIs were more commonly used by NOAC users compared with VKA-treated patients.
VKA users with AF revealed a similar trend compared to the overall study population, however, with higher aORs 2.02; 1.32–3.10 (NSAIDs), 1.61; 1.13–2.30 (heparins), and 3.53; 2.39–5.12 (antibiotics). They further had a significantly increased risk for concomitant use of platelet inhibitors (1.83; 1.28–2.62, Table 3). In contrast, NOAC users with AF revealed significantly elevated aORs of bleeding only for concomitant administration of platelet inhibitors (1.72; 1.14–2.59). In VKA users without AF, no significantly increased risks were observed when patients were co-prescribed one or more of the respective potentially interacting medication. In NOAC users without AF, platelet inhibitors and heparin revealed significantly increased risks of bleeding (2.37; 1.22–4.59 and 2.53; 1.10–5.81, respectively).
Considering daily oral anticoagulant doses of 0.5 or 1.5 DDDs revealed similar risks compared with our main exposure definition (Supplemental Table 4). Using different percentiles of the PDD to calculate exposure with oral anticoagulants revealed similar results for VKAs with the exception that the use of platelet inhibitors was also associated with an increased risk of bleeding (50th and 80th percentile, Supplemental Table 5). For NOAC users, the analyses based on the 50th and 80th percentiles yielded similar results compared with the main analysis. When using the 20th percentile, however, no significantly increased risks were observed for any of the included drugs. Applying different exposure definitions for comedication revealed similar results compared with the main analysis (Supplemental Table 6, respectively).
On a substance basis, risks for the mainly used substances phenprocoumon and rivaroxaban mirrored the overall results (again with the exception that use of platelet inhibitors was associated with a significantly increased risk of bleeding in phenprocoumon users, Supplemental Table 7). Differences were found for dabigatran and apixaban with respect to non-selective NSAIDs and antibiotics, respectively. However, these were based on comparatively low numbers of cases and controls.
Discussion
In this study, we compared VKA and NOAC use with respect to their risks for drug interactions leading to hospitalization for bleeding in nursing home residents. Overall, bleeding rates were higher in VKA users than in those receiving NOACs and the spectrum of interacting drugs differed between the two classes of oral anticoagulants.
Bleeding rates
We found higher bleeding rates compared with other studies not focused on nursing home residents, which is probably due to our patients’ older age and condition. Overall rates were lower in NOAC users with significantly decreased rates for intracerebral bleeding, whereas rates were slightly higher for GI or urogenital bleeding in these patients. Here our results are consistent with findings from previous trials reporting similar or lower rates of major bleeding in NOAC-treated patients [26,27,28,29,30,31], lower rates of intracerebral bleeding, and similar or higher rates for GI bleeding [26,27,28] compared with warfarin. Several studies using data from routine clinical practice in AF patients reported similar findings using warfarin [32,33,34,35] or phenprocoumon [36, 37] as comparator.
Bleeding rates were higher in men mainly influenced by their higher rates for urogenital bleeding, although a recent meta-analysis did not find a difference in the risk of major bleeding between anticoagulated men and women [38].
Interactions
Pharmacodynamic interactions affect all oral anticoagulants and might be more easily anticipated than interactions via pharmacokinetic mechanisms. In this context, agents which inhibit platelet function including antiplatelet drugs, NSAIDs, and SSRIs [12] are of great interest. These drugs differ with respect to indications, duration of use, and available alternatives.
Clinical situations requiring the use of antiplatelet drugs in addition to anticoagulants include short/intermediate-term (e.g., following percutaneous coronary intervention) and long-term (e.g. ACS) indications [39]. These regimens have been associated with increased risks of bleeding for dual and particular triple therapy [40,41,42]. Although we did not distinguish between single and dual platelet inhibition, the increased risks observed in VKA- and NOAC-treated patients with AF corroborate that these combinations are hazardous and should be conducted very carefully. The elevated risks found in NOAC users without AF might have been attributed to use in indications such as ACS for which in 2013 low-dose rivaroxaban as the only NOAC was approved in combination with antiplatelet drug regimens. However, the respective strength (2.5 mg) which became available in 2014 was used by only one patient in our study. Therefore, our findings almost exclusively depict use of products with higher strengths, which might have attributed to the increased risks of bleeding.
Besides their ability to impair platelet function, NSAIDs are known to damage the gastrointestinal mucosa via inhibition of cyclooxygenase (COX)-1 which leads to elevated bleeding risks, particularly of the upper GI tract [43]. Therefore, the necessity of NSAID therapy in users of oral anticoagulants should be evaluated and if long-term combined anticoagulant–NSAID treatment is required, the use of COX-2-specific agents or adding gastroprotective drugs is advised [6]. In our study, NOAC users seemed to be less affected by NSAID interactions. However, a higher proportion of PPI use was found in these patients. This might indicate an increased physicians’ awareness with respect to GI bleeding which has been reported for rivaroxaban and dabigatran in clinical trials [26, 27] and other studies using data from clinical practice [36, 37] when compared with VKA. This awareness might have led to increased PPI co-prescribing [44]. The increased risk observed with PPI use in VKA-treated patients which has been also been reported by another German study [20], might either hint at an interaction which, however, is not supported by recent studies [44, 45] or—more likely—could be attributed to increased PPI prescribing in persons who are per se at high risk for GI bleeding.
In this present analysis, concomitant use of SSRIs did not yield significantly increased risks for bleeding in VKA or NOAC users. The rather low SSRI use in our nursing home setting can probably be attributed to the German preference to use tricyclic antidepressants in elderly persons [46].
The combined use of oral anticoagulants and heparins is either indicated only for a short “bridging period” (VKA) or contraindicated (NOAC) and therefore depicts special clinical situations. Since VKAs need time to unfold their full effect, the initial heparin co-treatment is used if an immediate anticoagulation is required. This heparin–VKA overlap has been associated with increased bleeding risks [47, 48], which have also been observed in this present analysis underlining the caution that should be applied to the bridging procedure. In contrast, due to their quick onset, heparin bridging is not required when initiating NOACs in patients with AF and concomitant/overlapping heparin–NOAC use is contraindicated. Therefore, the increased risks of bleeding observed overall and in the subgroup of patients without AF were unexpected. Since our exposure times were based on prescriptions, it was not possible to deduce if, for example, VTE management was initiated with heparins (which is required if the NOAC is dabigatran) and then switched to NOACs or if treatment actually overlapped. However, difficulties with the adaption of NOAC treatment following VTE were found by a registry-based study reporting that nearly 29% of NOAC (mainly rivaroxaban) users received a heparin overlap indicating that guidelines for NOAC/rivaroxaban initiation after VTE were often not adhered to in clinical practice [49]. Given the increased risks observed in our analyses, the appropriate NOAC use is of paramount importance in these vulnerable populations.
In contrast to drugs which affect hemostasis, an impairment of coagulation by (mainly short-term) medication used to treat acute infections is less obvious. Further, the treating specialists such as pulmonologists or urologists might not be involved in monitoring coagulation. VKA interactions with several antibiotics are well known from the literature and can be attributed to pharmacokinetic and pharmacodynamic mechanisms. The latter include, among other things, the reduction of the vitamin K producing intestinal flora or the direct inhibition of vitamin K-dependent coagulation factors. In our analyses, we found elevated risks for bleeding in VKA users with antibiotic treatment implicating the same groups of drugs as in previous studies [20, 21]. These findings underline that the use of antibiotics such as sulfonamides or quinolones in VKA-treated patients should be avoided or at least monitored closely. In contrast and as reflected in our study, NOACs have been reported to be less susceptible to pharmacokinetic interactions.
Amiodarone is known to interact with VKAs, therefore our results were unexpected, however, since they were based on only a few cases, the results should be interpreted with caution. A possible explanation might be the awareness of this interaction and the resulting vigilant anticoagulation management [6]. In addition, a high amiodarone loading dose might have led to a reduced VKA dose [50] which might have been maintained. Whether these patients on the other hand had lower INR values than intended on the index day could not be determined with our data. Furthermore, amiodarone may have converted atrial fibrillation to sinus rhythm, leading to a less frequent prescription of VKA. This again may explain our finding of lower risk of bleeding in patients receiving amiodarone.
Strengths and limitations
The main strength of this study is the well-defined and large cohort of patients receiving treatment with oral anticoagulants. As a limitation, indications cannot be directly linked to prescriptions but have to be estimated from coded diagnoses [16]. As previously discussed, for a small proportion of patients, multiple diagnoses (e.g., of AF and VTE) were found and nearly 14% of patients had none of the examined diagnoses recorded [16]. Further, bleeding events could not be checked against medical charts, however, a high validity of our outcome definition based on hospital discharge diagnoses can be assumed.
Another limitation is that German claims data do not include prescribed daily doses and therefore exposure durations have to be estimated. Due to inter- and intra-individual differences, VKA dosing is more variable compared with the fixed-dosed NOACs. However, in our elderly study population, dose reductions in NOAC users were common. Our definition of 0.75 DDDs per day, which corresponded to the definition used by Abbas et al. (phenprocoumon) [21], was based on preliminary analyses from the overall cohort and mainly influenced by the most commonly used products phenprocoumon 3 mg and rivaroxaban 15 mg [16]. However, sensitivity analyses based on different exposure definitions for treatment with oral anticoagulants and comedication did not change our overall results, with the exception of the comparatively high daily dose resulting from the 20th percentile of the prescribed daily dose. In the nursing home setting, it is likely that medication is prescribed and dispensed as needed rather than stock piled by the patient. Further, an enhanced compliance might be assumed as medication is usually ordered, organized, and administered by the nursing home staff [51, 52] compared to outpatients living in their own homes. Since in-hospital medication is not included in the data, these findings solely reflect treatment in the outpatient setting.
With respect to the examined comedication, we might have underestimated concomitant use of NSAIDs, since lower doses of, e.g., ibuprofen or diclofenac can be bought over the counter without a medical prescription in Germany. The same applies to low-dose acetylsalicylic acid which is also often obtained without prescription.
Moreover, it was not possible to assess whether, in case of VKA-treated patients, INR values were monitored and doses were adapted accordingly. However, as previously discussed in our study, medical care of nursing home residents usually takes place in the nursing home instead of the physician’s office which probably hampers even established laboratory tests such as INR monitoring [16].
Conclusions and implications
In conclusion, we found lower bleeding rates in NOAC users than in those receiving VKAs with significantly decreased rates for intracerebral bleeding. This suggests that the findings from previous studies can be transferred to the population of nursing home residents treated with oral anticoagulants. Further, our study shows that comedication needs to be prescribed cautiously and when possible monitored closely in these patients. Although NOACs appeared to be less affected by interactions via pharmacokinetic mechanisms, pharmacodynamic interactions seemed to play a similar role and require cautious use. Especially the switch from parenteral anticoagulants to NOACs seems to be critical in these vulnerable patients and should be conducted very carefully.
References
Barnes GD, Lucas E, Alexander GC, Goldberger ZD (2015) National trends in ambulatory oral anticoagulant use. Am J Med 128:1300–1305.e2. https://doi.org/10.1016/j.amjmed.2015.05.044
Loo SY, Dell’Aniello S, Huiart L, Renoux C (2017) Trends in the prescription of novel oral anticoagulants in UK primary care. Br J Clin Pharmacol 83:2096–2106. https://doi.org/10.1111/bcp.13299
Gadsbøll K, Staerk L, Fosbøl EL et al (2017) Increased use of oral anticoagulants in patients with atrial fibrillation: temporal trends from 2005 to 2015 in Denmark. Eur Heart J 38:899–906. https://doi.org/10.1093/eurheartj/ehw658
Hein L, Wille H (2018) Antithrombotika und Antihämorrhagika. Arzneiverordnungs-report 2018. Springer, Berlin, pp 401–421
Shehab N, Lovegrove MC, Geller AI et al (2016) US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA 316:2115. https://doi.org/10.1001/jama.2016.16201
Vazquez SR (2018) Drug-drug interactions in an era of multiple anticoagulants: a focus on clinically relevant drug interactions. Blood 132:2230–2239. https://doi.org/10.1182/blood-2018-06-848747
Pharma GmbH MEDA, Co KG (2018) Marcumar. Summary of products characteristics. Fachinfo-Service, Frankfurt
Squibb Bristol-Myers (2017) Coumadin. Summary of products characteristics. Fachinfo-Service, Frankfurt
Snyder BD, Polasek TM, Doogue MP (2012) Drug interactions: principles and practice. Aust Prescr. https://doi.org/10.18773/austprescr.2012.037
Gelosa P, Castiglioni L, Tenconi M et al (2018) Pharmacokinetic drug interactions of the non-vitamin K antagonist oral anticoagulants (NOACs). Pharmacol Res 135:60–79. https://doi.org/10.1016/j.phrs.2018.07.016
Zotz RB, Weißbach L (2017) Monitoring of NOAC. Med Klin Intensivmed Notfmed 112:92–98. https://doi.org/10.1007/s00063-016-0249-6
Stöllberger C (2017) Drug interactions with new oral anticoagulants in elderly patients. Expert Rev Clin Pharmacol. https://doi.org/10.1080/17512433.2017.1370369
Hohnloser SH, Basic E, Nabauer M (2019) Uptake in antithrombotic treatment and its association with stroke incidence in atrial fibrillation: insights from a large German claims database. Clin Res Cardiol. https://doi.org/10.1007/s00392-019-01437-7
Reardon G, Pandya N, Nutescu EA et al (2013) Incidence of venous thromboembolism in nursing home residents. J Am Med Dir Assoc 14:578–584. https://doi.org/10.1016/j.jamda.2013.02.003
Sinnaeve PR, Brueckmann M, Clemens A et al (2012) Stroke prevention in elderly patients with atrial fibrillation: challenges for anticoagulation. J Intern Med 271:15–24. https://doi.org/10.1111/j.1365-2796.2011.02464.x
Jobski K, Hoffmann F, Herget-Rosenthal S, Dörks M (2018) Use of oral anticoagulants in German nursing home residents: drug use patterns and predictors for treatment choice. Br J Clin Pharmacol 84:590–601. https://doi.org/10.1111/bcp.13474
Dörks M, Herget-Rosenthal S, Schmiemann G, Hoffmann F (2016) Polypharmacy and renal failure in nursing home residents: results of the inappropriate Medication in Patients with Renal Insufficiency in Nursing Homes (IMREN) Study. Drugs Aging 33:45–51. https://doi.org/10.1007/s40266-015-0333-2
Palareti G, Cosmi B (2009) Bleeding with anticoagulation therapy—who is at risk, and how best to identify such patients. Thromb Haemost. https://doi.org/10.1160/TH08-11-0730
Wacholder S, Silverman DT, McLaughlin JK, Mandel JS (1992) Selection of controls in case-control studies. III. Design options. Am J Epidemiol 135:1042–1050
Jobski K, Behr S, Garbe E (2011) Drug interactions with phenprocoumon and the risk of serious haemorrhage: a nested case–control study in a large population-based German database. Eur J Clin Pharmacol 67:941–951. https://doi.org/10.1007/s00228-011-1031-6
Abbas S, Ihle P, Harder S, Schubert I (2014) Risk of bleeding and antibiotic use in patients receiving continuous phenprocoumon therapy. Thromb Haemost 111:912–922. https://doi.org/10.1160/TH13-09-0723
Chang SH, Chou IJ, Yeh YH et al (2017) Association between use of non–vitamin K oral anticoagulants with and without concurrent medications and risk of major bleeding in nonvalvular atrial fibrillation. JAMA J Am Med Assoc 318:1250–1259. https://doi.org/10.1001/jama.2017.13883
Büscher A, Wingenfeld K, Schaeffer D (2011) Determining eligibility for long-term care-lessons from Germany. Int J Integr Care 11:e019. https://doi.org/10.5334/ijic.584
Langan SM, Schmidt SA, Wing K et al (2018) The reporting of studies conducted using observational routinely collected health data statement for pharmacoepidemiology (RECORD-PE). BMJ 363:k3532. https://doi.org/10.1136/bmj.k3532
Ihle P, Krueger K, Schubert I et al (2019) Comparison of different strategies to measure medication adherence via claims data in patients with chronic heart failure. Clin Pharmacol Ther. https://doi.org/10.1002/cpt.1378
Connolly SJ, Ezekowitz MD, Yusuf S et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation.[Erratum appears in N Engl J Med. 2010 Nov 4;363(19):1877]. N Engl J Med. https://doi.org/10.1056/NEJMoa0905561
Patel MR, Mahaffey KW, Garg J et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365:883–891. https://doi.org/10.1056/NEJMoa1009638
Granger CB, Alexander JH, McMurray JJV et al (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365:981–992. https://doi.org/10.1056/NEJMoa1107039
Agnelli G, Buller HR, Cohen A et al (2013) Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med 369:799–808. https://doi.org/10.1056/NEJMoa1302507
Investigators EINSTEIN, Bauersachs R, Berkowitz SD et al (2010) Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 363:2499–2510. https://doi.org/10.1056/NEJMoa1007903
EINSTEIN–PE Investigators, Büller HR, Prins MH et al (2012) Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 366:1287–1297. https://doi.org/10.1056/nejmoa1113572
Sjögren V, Byström B, Renlund H et al (2017) Non-Vitamin K oral anticoagulants are non-inferior for stroke prevention but cause fewer major bleedings than well-managed warfarin: a retrospective register study. PLoS One. https://doi.org/10.1371/journal.pone.0181000
Yao X, Abraham NS, Sangaralingham LR et al (2016) Effectiveness and safety of dabigatran, rivaroxaban, and apixaban versus warfarin in nonvalvular atrial fibrillation. J Am Heart Assoc. https://doi.org/10.1161/JAHA.116.003725
Larsen TB, Skjøth F, Nielsen PB et al (2016) Comparative effectiveness and safety of non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. https://doi.org/10.1136/bmj.i3189
Lip GYH, Keshishian A, Kamble S et al (2016) Real-world comparison of major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban, or warfarin: a propensity score matched analysis. Thromb Haemost. https://doi.org/10.1160/TH16-05-0403
Ujeyl M, Köster I, Wille H et al (2018) Comparative risks of bleeding, ischemic stroke and mortality with direct oral anticoagulants versus phenprocoumon in patients with atrial fibrillation. Eur J Clin Pharmacol. https://doi.org/10.1007/s00228-018-2504-7
Hohnloser SH, Basic E, Nabauer M (2017) Comparative risk of major bleeding with new oral anticoagulants (NOACs) and phenprocoumon in patients with atrial fibrillation: a post-marketing surveillance study. Clin Res Cardiol. https://doi.org/10.1007/s00392-017-1098-x
Takach Lapner S, Cohen N, Kearon C (2014) Influence of sex on risk of bleeding in anticoagulated patients: a systematic review and meta-analysis. J Thromb Haemost. https://doi.org/10.1111/jth.12529
Floyd CN, Ferro A (2017) Indications for anticoagulant and antiplatelet combined therapy. BMJ. https://doi.org/10.1136/bmj.j3782
Hansen ML, Sørensen R, Clausen MT et al (2010) Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. https://doi.org/10.1001/archinternmed.2010.271
Oldgren J, Wallentin L, Alexander JH et al (2013) New oral anticoagulants in addition to single or dual antiplatelet therapy after an acute coronary syndrome: a systematic review and meta-analysis. Eur Heart J 34:1670–1680. https://doi.org/10.1093/eurheartj/eht049
Duerschmied D, Brachmann J, Darius H et al (2018) Antithrombotic therapy in patients with non-valvular atrial fibrillation undergoing percutaneous coronary intervention: should we change our practice after the PIONEER AF-PCI and RE-DUAL PCI trials? Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1242-2
Bjarnason I, Scarpignato C, Holmgren E et al (2018) Mechanisms of damage to the gastrointestinal tract from nonsteroidal anti-inflammatory drugs. Gastroenterology 154:500–514. https://doi.org/10.1053/j.gastro.2017.10.049
Ray WA, Chung CP, Murray KT et al (2018) Association of oral anticoagulants and proton pump inhibitor cotherapy with hospitalization for upper gastrointestinal tract bleeding. JAMA 320:2221. https://doi.org/10.1001/jama.2018.17242
Henriksen DP, Stage TB, Hansen MR et al (2015) The potential drug–drug interaction between proton pump inhibitors and warfarin. Pharmacoepidemiol Drug Saf. https://doi.org/10.1002/pds.3881
Jobski K, Schmedt N, Kollhorst B et al (2017) Characteristics and drug use patterns of older antidepressant initiators in Germany. Eur J Clin Pharmacol 73:105–113. https://doi.org/10.1007/s00228-016-2145-7
Bouillon K, Bertrand M, Boudali L et al (2016) Short-term risk of bleeding during heparin bridging at initiation of vitamin K antagonist therapy in more than 90 000 patients with nonvalvular atrial fibrillation managed in outpatient care. J Am Heart Assoc 1:1. https://doi.org/10.1161/JAHA.116.004065
Siegal D, Yudin J, Kaatz S et al (2012) Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.112.105221
Bauersachs R, Agnelli G, Gitt AK et al (2017) The role of heparin lead-in in the real-world management of acute venous thromboembolism: the PREFER in VTE registry. Thromb Res 157:181–188. https://doi.org/10.1016/j.thromres.2017.07.029
Holm J, Lindh JD, Andersson ML, Mannheimer B (2017) The effect of amiodarone on warfarin anticoagulation: a register-based nationwide cohort study involving the Swedish population. J Thromb Haemost. https://doi.org/10.1111/jth.13614
Lochner S, Kirch W, Schindler C (2012) Managing hypertension among nursing-home residents and community-dwelling elderly in Germany: a comparative pharmacoepidemiological study. Eur J Clin Pharmacol. https://doi.org/10.1007/s00228-011-1195-0
Hughes CM, Goldie R (2009) “I just take what i am given”: adherence and resident involvement in decision making on medicines in nursing homes for older people: a qualitative survey. Drugs Aging. https://doi.org/10.2165/00002512-200926060-00007
Acknowledgements
The authors thank the DAK-Gesundheit for providing the data for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jobski, K., Hoffmann, F., Herget-Rosenthal, S. et al. Drug interactions with oral anticoagulants in German nursing home residents: comparison between vitamin K antagonists and non-vitamin K antagonist oral anticoagulants based on two nested case–control studies. Clin Res Cardiol 109, 465–475 (2020). https://doi.org/10.1007/s00392-019-01526-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01526-7