Abstract
Background
Elevated C-reactive protein (CRP) is associated with adverse outcomes in heart failure (HF) patients. Beta-blocker therapy may lower CRP levels.
Methods and results
To assess if the changes of high-sensitivity (hs) CRP levels in HF patients over 12-week titration with beta-blockers correlate with functional capacity, plasma hs-CRP levels were measured in 488 HF patients [72.1 ± 5.31 years, LVEF 40% (33/50)]. Hs-CRP, NT-proBNP and 6-min-walk-test (6MWT) were assessed at baseline and at week 12. Patients were divided based on hs-CRP changes (cut-off > 0.3 mg/dl) into low–low (N = 225), high–high (N = 132), low–high (N = 54), high–low (N = 77) groups. At baseline, median hs-CRP concentration was 0.25 (0.12/0.53) mg/dl, NT-proBNP 551 (235/1455) pg/ml and average 6MWT distance 334 ± 105 m. NT-proBNP changes were significantly different between the four hs-CRP groups (P = 0.011). NT-proBNP increased in the low–high group by 30 (− 14/88) pg/ml and decreased in the high–low group by − 8 (− 42/32) pg/ml. 6MWT changes significantly differed between groups [P = 0.002; decrease in the low–high group (− 18 ± 90 m) and improvement in the low–low group (24 ± 62 m)].
Conclusion
After beta-blocker treatment, hs-CRP levels are associated with functional capacity in HF patients. Whether this represents a potential target for intervention needs further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic inflammation plays a significant role in the pathophysiology of heart failure (HF). C-reactive protein (CRP) is a marker of inflammation and tissue damage [1]. There is broad evidence suggesting that CRP levels are increased in HF regardless of etiology [2], and several studies have shown the relation between elevated CRP levels and poor prognosis in HF [3]. It is also known that lowering of inflammatory biomarkers in these patients can reduce the cardiovascular risk [4].
CRP levels can be influenced by cardiovascular drugs. In particular, beta-blockers are associated with the lowering of CRP levels [5]. Besides clinical events, improved functional capacity is a critical patient-centered outcome in HF patients. The 6-min walk test (6MWT) is a submaximal exercise evaluation that has been validated in patients with HF [6].
In this analysis, we sought to assess if the changes of hs-CRP levels in HF patients over 12-week titration with beta-blockers correlate with the changes in functional capacity.
Methods
Study population
This is a sub-study of the cardiac insufficiency bisoprolol study in elderly (CIBIS-ELD), a multicenter, randomized, double-blind trial with elderly patients with stable chronic HF. Rationale and design of the CIBIS-ELD trial was published previously [7]. Briefly, patients were eligible if they were older than 65, with current HF diagnosis and symptoms consistent with NYHA II or above. All patients were randomized in a 1:1 fashion to either bisoprolol or carvedilol. In this analysis, plasma levels of hs-CRP and NT-proBNP were measured in 488 patients of the CIBIS-ELD trial. Beta-blocker naïve and patients treated with maximum 1/4th of the target dose were randomized to bisoprolol vs. carvedilol and doses were up-titrated to the target or maximally tolerated dose during 12 weeks. Patients who had an infection or white blood cell count > 10,000,000/ml were excluded from this analysis. NT-proBNP and hs-CRP levels were assessed at baseline and after 12 weeks (follow-up). At the same time, LVEF and results of the 6MWT were documented at baseline and after 12 weeks. Authors confirm that the investigation conforms to the principles outlined in the Declaration of Helsinki. The national and locally appointed ethics committees have approved the research protocol and written informed consent has been obtained from all subjects.
Laboratory measurements
CRP is produced in the liver and its levels are relatively stable, which means it can be accurately measured. CRP is traditionally measured down to concentrations of 3–5 mg/l, but with the development of high-sensitivity (hs) techniques, hs-CRP can be measured down to concentrations around 0.3 mg/l [8]. For this analysis, blood samples were taken at baseline and during after 12 weeks. All blood samples were centrifuged within 1 h after collection and the resulting sera were frozen at − 80 °C until analyzed. Levels of hs-CRP and NT-proBNP were determined using commercially available assays (Elecsys, Roche Diagnostics, Basel, Switzerland).
Statistical analysis
We have defined four groups, depending on the hs-CRP level at baseline and at follow-up (after 12 weeks). The cut-off for the groups has been set at 0.3 mg/dl. We chose this cut-off according to the American Heart Association and US. Center for Disease Control and Prevention, who have defined the following risk groups: low risk < 0.1 mg/dl, average risk 0.1–0.3 mg/dl and high risk > 0.3 mg/dl [9]. Therefore, four groups have been identified: (1) low hs-CRP at baseline and low at follow-up (low–low), (2) high hs-CRP at baseline and high at follow-up (high–high), (3) low hs-CRP at baseline and high at follow-up (low–high), (4) high hs-CRP at baseline and low at follow-up (high–low). Raw data for NT-proBNP and hs-CRP have been log-transformed prior to analysis, as they follow a log-normal distribution. Differences between baseline and follow-up are computed from raw values. Change in walking distance was tested by a multifactorial ANOVA with CRP group change, age, gender, NYHA, BMI, blood pressure, baseline walking distance, CAD and left ventricular ejection fraction (LVEF) as independent variables. Analyzes were performed using R version 3.4.0.
Results
Baseline characteristics
Study population comprised of 64% male with the mean age of 72.1 ± 5.31 years. At baseline, patients were predominantly in NYHA Class II, and the median LVEF was 40 (33/50)%. Almost half of the patients (43%) had HF of ischemic etiology and 40% had previous myocardial infarction. The average distance of the 6MWT at baseline was 334 ± 105 m. 40% of the patients were beta-blocker pre-treated prior to the study. However, no statistically significant differences in changes of hs-CRP, 6MWT, and NT-proBNP were shown between beta-blocker naive and patients who were previously treated with beta-blockers.
Table 1 presents baseline characteristics of the patients.
Biomarkers
Out of the total 488 patients, 225 were in the low–low group, 132 in the high–high, 54 in the low–high, and 77 in the high–low group. Each group had equal distribution of patients randomized to bisoprolol or carvedilol (P = 0.973 between the groups). Median (Quartile 1/Quartile 3) concentrations of hs-CRP were 0.25 (0.12/0.53) mg/dl at baseline and 0.23 (0.12/0.45) mg/dl at follow-up. NT-proBNP levels were 551 (235/1455) pg/ml at baseline and 573 (231/1546) pg/ml at follow-up. Detailed biomarker levels throughout the four groups are presented in the Table 2.
The relative change of NT-proBNP from baseline to follow-up was analyzed between the four previously defined groups. We showed that there is a statistically significant difference in the relative NT-proBNP change between four groups (P = 0.011; Fig. 1). The overall relative change of NT-proBNP from baseline (BL) to follow-up (FU) in the complete analyzed population was Δ % FU-BL NT-proBNP = 5 (− 28/54).
The biggest decrease of NT-proBNP was seen in the high–low group [Δh→l% FU-BL NT-proBNP = − 8 (− 42/32)], and the biggest increase in the low–high group [Δl→h % FU-BL NT-proBNP = 30 (− 14/88)]. The relative change of the NT-proBNP in the low–low was close to the one determined in the entire analyzed population [Δl→l % FU-BL NT-proBNP = 5 (− 28/51)], and the relative change in the high–high group was Δh→h % FU-BL NT-proBNP = 2 (− 25/56).
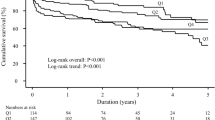
CRP changes and functional capacity
At baseline, average distance for the 6MWT was 334 ± 105 m. After 12 weeks, the average distance was 348 ± 99 m in the overall population. The absolute change in 6MWT results from baseline to follow-up was significantly different between the four defined groups (P = 0.002; Fig. 2), with the overall change of Δ 6MWT = 15 ± 68 m (P = 0.002 between the groups). The biggest increase in 6MWT distance between baseline and follow-up was in the low–low group (Δl→l 6MWT = 24 ± 62 m), while the biggest decrease occurred in the low–high group (Δl→h 6MWT = − 18 ± 90 m). The changes from baseline to follow-up in the high–high and the high–low group were close to the overall change (Δh→h 6MWT = 15 ± 69 m and Δh→l 6MWT = 14 ± 62 m).
We further tested several potential predictors (CRP group change, age, gender, NYHA, BMI, blood pressure, baseline walking distance, CAD and LVEF) in a linear model with change in 6MWT distance as the independent variable (Table 3). Affiliation to one of the groups (CRP group change) was significantly related (P = 0.008). The distance at baseline was positively related to change (longer distance at baseline was related to the improvement, while the shorter distance at baseline was related to worsening). The impact of gender was marginally significant with males showing greater improvement.
Discussion
In this analysis of the CIBIS-ELD trial, we have found that the relative change of NT-proBNP is associated with the change in hs-CRP from baseline to follow-up and that the change in 6MWT distance is associated with the change in hs-CRP from baseline to follow-up.
Recently, inflammation is getting more and more recognition in the pathogenesis and development of heart failure. Correlation between elevated inflammatory mediators and adverse clinical outcomes has been explored and proved in previous research [10]. In this analysis, the patients were divided into four groups depending on whether the hs-CRP level was low or high at baseline and after 12 weeks.
Beta-blockers are guideline-recommended treatment for HF patients. Anti-inflammatory role of beta-blockers has been very modestly evaluated so far. A recent study in beta-blocker-naïve HFrEF patients who were given carvedilol for 12 months showed a global decrease of inflammatory biomarkers [11]. In another study, CRP levels were measured in a group of 96 outpatients with HF, and it was shown that beta-blockers reduced serum CRP by 37.5% [12]. The patients whose data we analyzed were randomized to beta-blockers and we have shown that the hs-CRP levels have overall decreased, from 0.25 (0.12/0.53) mg/dl at baseline to 0.23 (0.12/0.45) mg/dl at follow-up. In 57% of the analyzed patients, hs-CRP levels decreased during the 12 weeks of treatment. We tested to check if the type of beta-blocker assigned (bisoprolol vs. carvedilol) influences the decrease in the inflammatory marker, but it seems that selectivity of the beta-blocker did not play a role, as each hs-CRP-defined group had similar distribution of patients randomized to bisoprolol and carvedilol.
Circulating natriuretic peptides, and particularly B-type natriuretic peptide (BNP) and N-terminal pro B-type natriuretic peptide (NT-proBNP) have been extensively used for evaluating the disease status in HF patients. They are currently recognized as the gold standard of predictive markers in HF patients [13]. Our results showed that the relative change of NT-proBNP was associated with the change in hs-CRP. It is also interesting that in the high–low group, in which the hs-CRP level went from above 0.3 mg/dl to below this cut-off in 12 weeks, NT-proBNP levels also decreased significantly. Contrary to that, in the low–high group, together with the hs-CRP level increase, the NT-proBNP levels increased as well.
Further, we showed that with the increase of hs-CRP levels from baseline to follow-up, the 6MWT distance decreases. On the other hand, the results of the 6MWT were better after 12 weeks of beta-blocker treatment in the other groups (low–low, high–low and high–high), where the hs-CRP levels did not increase. Despite our expectations to show the biggest improvement in the high–low group, the biggest improvement was shown in the low–low group. The improvement in the high–high and high–low groups was comparable. However, looking into the 6MWT results after the 12-week treatment, patients in the high–low group had better 6MWT results (339 ± 84 m), when compared to the high–high group (332 ± 97 m).
There were no previous studies exploring this correlation. However, some of the previous trials have explored the correlation between exercise and inflammatory status in patients with cardiac diseases [14, 15]. Results from the National Health and Nutrition Examination Survey (NHANES) have shown that even in healthy individuals with elevated CRP (> 0.3 mg/dl), heart recovery rate after intense exercise is worse compared to those whose CRP levels were in normal ranges [16]. One study published earlier this year concluded that there is an association between inflammatory biomarkers and differential effect of exercise on functional capacity in HF patients [17]. Another study carried out in HF patients explored the effects of 12-week treatment with methotrexate to the results of the 6MWT. These researches did not find any significant changes in 6MWT results in the methotrexate group [18]. Further, a recent analysis of a KORA-Age trial, showed that higher concentrations of inflammatory markers (IL-6 and hs-CRP) in elderly individuals with and without cardiac disease are associated with lower levels of muscular strength [19]. This is somewhat in accordance with our results.
However, based on our findings, we could assume that combination of NT-proBNP and hs-CRP could serve as a good predictor of functional capacity.
The results show that hs-CRP seems to be a good predictor of functional capacity in HF patients. This could mean that the control of inflammation might be beneficial in patients with higher hs-CRP levels.
References
Koenig W (2013) High-sensitivity C-reactive protein and atherosclerotic disease: from improved risk prediction to risk-guided therapy. Int J Cardiol 168(6):5126–5134
van Empel V, Brunner-La Rocca HP (2015) Inflammation in HFpEF: key or circumstantial? Int J Cardiol 189:259–263
Huynh K, Van Tassell B, Chow SL (2015) Predicting therapeutic response in patients with heart failure: the story of C-reactive protein. Expert Rev Cardiovasc Ther 13(2):153–61
Ridker PM, Everett BM, Thuren T, CANTOS Trial Group et al (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131
Prasad K (2006) C-reactive protein lowering agents. Cardiovasc Drug Rev 24(1):33–50
Rostagno C, Gensini GF (2008) Six-minute walk test: a simple and useful test to evaluate functional capacity in patients with heart failure. Intern Emerg Med 3(3):205–12
Düngen HD, Apostolović S, Inkrot S, CIBIS-ELD Investigators, Subproject Multicenter Trials in the Competence Network Heart Failure et al (2008) Bisoprolol vs. carvedilol in elderly patients with heart failure: rationale and design of the CIBIS-ELD trial. Clin Res Cardiol 97(9):578–86
Silva D, Pais de Lacerda A (2012) High-sensitivity C-reactive protein as a biomarker of risk in coronary artery disease. Rev Port Cardiol 31(11):733–45
Pearson TA, Mensah GA, Alexander RW, Centers for Disease Control and Prevention; American Heart Association et al (2003) Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107(3):499–511
Van Linthout S, Tschöpe C (2017) Inflammation—cause or consequence of heart failure or both? Curr Heart Fail Rep. https://doi.org/10.1007/s11897-017-0337-9
Nessler J, Nessler B, Golebiowska-Wiatrak R et al (2013) Serum biomarkers and clinical outcomes in heart failure patients treated de novo with carvedilol. Cardiol J 20(2):144–51
Joynt KE, Gattis WA, Hasselbald V et al (2004) Effect of angiotensin-converting enzyme inhibitors, beta-blockers, statins, and aspirin on C-reactive protein levels in outpatients with heart failure. Am J Cardiol 93:783–785
Francis GS, Felker GM, Tang WH (2016) A test in context: critical evaluation of natriuretic peptide testing in heart failure. J Am Coll Cardiol 67(3):330–337
Dopheide JF, Geissler P, Rubrech J et al (2016) Influence of exercise training on proangiogenic TIE-2 monocytes and circulating angiogenic cells in patients with peripheral arterial disease. Clin Res Cardiol 105(8):666–76. https://doi.org/10.1007/s00392-016-0966-0
Dopheide JF, Scheer M, Doppler C et al (2015) Change of walking distance in intermittent claudication: impact on inflammation, oxidative stress and mononuclear cells: a pilot study. Clin Res Cardiol 104(9):751–63. https://doi.org/10.1007/s00392-015-0840-5
Kuo HK, Gore JM (2015) Relation of heart rate recovery after exercise to insulin resistance and chronic inflammation in otherwise healthy adolescents and adults: results from the National Health and Nutrition Examination Survey (NHANES) 1999–2004. Clin Res Cardiol 104(9):764–72 https://doi.org/10.1007/s00392-015-0843-2
Fernandes-Silva MM, Guimarães GV et al (2017) Inflammatory biomarkers and effect of exercise on functional capacity in patients with heart failure: insights from a randomized clinical trial. Eur J Prev Cardiol 24(8):808–817
Moreira DM1, Vieira JL, Gottschall CA (2009) The effects of METhotrexate therapy on the physical capacity of patients with ISchemic heart failure: a randomized double-blind, placebo-controlled trial (METIS trial). J Card Fail 15(10):828–34
Volaklis KA,Halle M, Koenig W et al (2015) Association between muscular strength and inflammatory markers among elderly persons with cardiac disease: results from the KORA-age study. Clin Res Cardiol 104(11):982–9. https://doi.org/10.1007/s00392-015-0867-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Butler: Consultant to Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, Janssen, Novartis, Relypsa, Trevena, ZS Pharma, Stealth Peptide, Medtronic, Merck, CVRx, Luitpold, and Vifor.
Rights and permissions
About this article
Cite this article
Radenovic, S., Loncar, G., Busjahn, A. et al. Systemic inflammation and functional capacity in elderly heart failure patients. Clin Res Cardiol 107, 362–367 (2018). https://doi.org/10.1007/s00392-017-1195-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1195-x