Abstract
Background
Coronary computed tomography angiography (CTA) is increasingly used as a test to rule out coronary artery disease (CAD) in patients with a low to intermediate pre-test probability of the disease. We used the database of the German CT registry, collected between 2009 and 2014 in a broad patient population, to analyze contemporary radiation dose associated with coronary CTA in clinical practice.
Patients and methods
The prospective observational registry included a total of 7061 patients ≥18 years, referred to 12 participating centers for a clinically indicated cardiac CT examination. All centers were cardiology units well experienced in CTA and used multi-slice CT scanners with at least 64 rows. Coronary CTA was performed in a subset of 5001 patients, 59.6 ± 11.8 years, body mass index (BMI) 26.9 ± 4.5 kg/m2, 38% females. Three time periods with approximately equal numbers of patients were created (01/09–03/10, 04/10–03/11, 04/11–07/14). The dose–length product of all examinations and derived effective dose in mSv (conversion factor k = 0.014) as well as the influence of patient characteristics on dose were compared for the three time periods.
Results
BMI and proportion of female patients remained stable over time, and mean heart rate decreased from 60.3 ± 9.0 to 58.5 ± 9.3 bpm from the first to the last time period (p < 0.001). Overall, the mean effective dose of coronary CTA was 3.6 mSv (Q1 1.8 mSv, Q3 7.4 mSv). Within the three time periods, it declined from 5.6 (2.7, 8.6) mSv during the first to 4.8 (2.1, 8.2) mSv during the second and 2.5 (1.3, 4.6) mSv during the last time period (p < 0.001). Paralleling the decline in radiation dose over time, the proportion of prospectively ECG-triggered examinations increased (68, 79, 83%; p < 0.001), and the proportion of examinations with retrospective gating and no tube current modulation decreased (5.3, 4.0, 1.6%; p < 0.001). Tube current (mAs) and voltage (kV) both decreased over time. In multivariable analysis, besides earlier time period, further independent predictors of an increased radiation dose were older age, higher heart rate, and higher BMI as well as the technical factors higher mAs, higher kV, and retrospective gating. At three sites, CT scanners with improved technology were installed during the last time period.
Conclusions
In current clinical practice among German cardiology units with specific expertise in cross-sectional cardiovascular imaging, overall radiation dose of coronary CTA was comparably low. Over time, a decline in radiation dose was demonstrated, probably due to a combination of improvements in data acquisition protocols and patient preparation as well as installation of new CT scanners with advanced technology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Computed tomography coronary angiography (coronary CTA) is increasingly used in the diagnostic workup of patients with suspected coronary artery disease (CAD). Current European guidelines support its use with a class IIa recommendation in patients with stable chest pain within the lower range of intermediate pre-test probability of CAD, i.e., between 15 and 50% [1]. Owing to its excellent sensitivity in detecting coronary plaque build-up, coronary CTA yields high negative predictive values. Accordingly, a high degree of certainty can be obtained with regard to the absence of CAD and respective prognostic implications [1]. However, in low-risk populations, radiation dose of medical imaging has been an issue [2,3,4].
There is a general consensus that radiation dose should be kept as low as achievable while maintaining diagnostic image quality. The Prospective Multicenter Study on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice I (PROTECTION I) sampled the radiation dose associated with coronary CTA as estimated at 50 world-wide sites in the year 2007 [5]. The CT scanners in use at the participating sites were 16- and 64-slice systems. A median radiation dose of 12 mSv was calculated. Of note, dose estimates of diagnostic invasive coronary angiography typically comprise 2–7 mSv [2, 4, 6], and 99mTc sestamibi myocardial perfusion imaging appears to be in the same range [2, 4, 7]. Since PROTECTION I, technical developments as well as novel imaging protocols have substantially reduced the radiation dose associated with coronary CTA [8], but are not applicable to all patients and may not have fully penetrated clinical practice. We, therefore, interrogated the German Cardiac CT Registry which included real-world data on more than 7000 patients between 2009 and 2014, regarding trends in radiation exposure of coronary CTA in clinical practice.
Patients and methods
The study was designed as a prospective observational registry for patients 18 years and older referred for a clinically indicated cardiac CT examination. The objectives of the registry were to collect data from a large all-comer cohort including indications for the examination, study parameters, safety, and therapeutic implications in clinical practice. Further objectives included assessment of downstream resource utilization following coronary CT angiography as well as analysis of radiation exposure. The project was financed by Stiftung Institut für Herzinfarktforschung (IHF, Ludwigshafen, Germany). Institutional review board approval was obtained from Landesärztekammer Rheinland-Pfalz.
All participating sites were cardiology units with adequate experience in the field of cardiac CT (at least 300 patients per year undergoing cardiac CT scans) and using a minimum equipment of 64-slice CT system. A total of 12 centers participated (see “Appendix”). The register was documented under ClincalTrials.gov (Identifier NCT01197703).
Patients
All consecutive patients at participating sites were included if meeting the inclusion criteria: age 18 years or older, referral for a clinically indicated cardiac CT examination, written informed consent for participating in the registry. Exclusion criteria included cardiac CT examinations performed within a specific research protocol and failure to provide informed consent.
Data collection and risk factors
The study patients underwent their cardiac CT examination as clinically indicated and ordered by referring physician. At the time of examination, data were collected prospectively including patient demographics, medical history, and standardized cardiovascular risk factors as determined by a structured patient interview in a web-based electronic case report form (CRF).
Body mass index (kg/m2) was calculated on the basis of height (m) and weight (kg). Diabetes was considered to be present if the patient was taking insulin or oral antidiabetic medication or if he or she had previously received such treatment and was currently controlling the condition through dietary modulation. A patient was considered to be hypertensive if he or she had received such a diagnosis on the basis of systemic blood pressure >140/90 mmHg, or was being treated with antihypertensive medications, dietary modulation, or both. Regarding family history, a patient was considered to have a positive family history if a history of coronary heart disease or stroke was present in first or second degree relatives (females at an age <65 years, males at an age <55 years). A patient who had stopped smoking more than 20 years ago was not considered to have smoking as a risk factor. Otherwise, he or she was classified as current smoker or previous smoker if having stopped >1 month before being interrogated. Pre-test probability of coronary artery disease (CAD) was calculated according to the recommendations given in the actual European guidelines [1].
Cardiac CT
Detailed information regarding indications for the cardiac CT examination, scan parameters and contrast protocol, study results (including results of coronary calcification exam and coronary CT angiography), complications and consequences were collected through a structured data base. Scan range (mm), tube current (mA, mAs), tube voltage (kV), and dose length product (DLP, mGy*cm) were part of the data base. Estimated effective radiation dose was calculated from DLP, applying a conversion factor of k = 0.014 for chest CT in adults [9].
Statistics
Statistical analyses were performed using SAS 9.3 software packages. Results are presented as mean ± standard deviation or median and quartile values. Categorical parameters are described by absolute numbers and percentages. To analyze trends over time, three periods with a comparable number of examinations were chosen, i.e., January 2009–March 31, 2010; April 1, 2010–March 31, 2011, and April 1, 2011–July 2014. Cochran-Armitage and Jonckheere-Terpstra tests were performed for comparing parameters between these defined time periods. Further, patients were classified into those with an estimated effective radiation dose above versus below the median, and comparisons were done by Chi square or Wilcoxon’s rank-sum test. Independent predictors were identified by logistic regression analysis.
Results
Out of a total of 7061 patients entered in the registry between January 2009 and July 2014, 5001 (71%) underwent a contrast-enhanced study of their coronary arteries (coronary CTA) and thus were eligible for the current analysis. Approximately, 45% of the patients were characterized as having angina pectoris (n = 2248), 68% of whom were thought of as having atypical angina pectoris. A low pre-test probability (PTP) <15% was observed in 8.4%, an intermediate PTP (15–50%) in 62.2%, and a high PTP >50% in 29.3%. These proportions remained largely stable over time with the only exception of slightly more patients with a PTP <15% and fewer patients with a high PTP during the last time interval (10.4 and 26.4%, respectively). Approximately, 18% had dyspnea >New York Heart Association (NYHA) II (n = 916). In 27% (n = 1373), a previous stress test had shown a pathological (n = 782) or inconclusive (n = 571) result. The vast majority of the stress tests, i.e., 94%, had been exercise stress electrocardiographic (stress ECG) tests.
Mean patient age was 59.6 ± 11.8 years, and 1874 were female (38%). BMI was 26.9 ± 4.5 kg/m2. Table 1 gives demographic and risk factor data of the overall patient group. Additionally, the demographic data are presented for the respective subgroups in the three time periods created for the analysis of changes over time. There were notable trends in risk factor exposure over time in that the proportion of current smokers increased whereas the prevalence of systemic hypertension decreased. Overall, the median number of risk factors per patient appeared relatively stable, i.e., between 2 and 3. Also, the percentage of female patients and the patients’ BMI remained stable over time. However, mean heart rate declined from 60.3 ± 9.0 bpm during the first to 58.5 ± 9.3 bpm during the last time interval (p < 0.001), probably reflecting increased efforts by the participating centers to control heart rate in preparation for data acquisition. The relative number of outpatient vs. inpatient examinations fluctuated over time, with no apparent continuous trend over time.
Among the 5001 patients undergoing coronary CTA, additional non-contrast-enhanced scans for quantifying coronary artery calcium (CAC) were performed in 3894 patients (78%). Overall, median estimated effective radiation dose associated with CAC scanning was 0.6 mSv. Over time, CAC-associated radiation dose decreased statistically significantly from 0.7 to 0.4 mSv (p < 0.001). As shown in Table 2, this may at least in part be explained by changes in data acquisition protocols, as the proportion of scans performed using retrospective gating decreased, and the proportion of scans using prospective triggering increased.
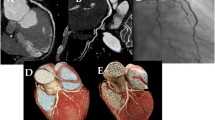
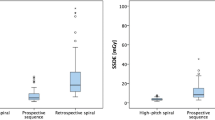
Coronary CTA itself was associated with a median estimated effective radiation dose of 3.6 (1.8, 7.4) mSv. Effective dose declined significantly over time, from a median of 5.6 mSv during the first to 2.5 mSv during the last period (p < 0.001, Fig. 1). DLP was reduced from a median of 397 mGy*cm to a median of 176 mGy*cm (p < 0.001). Details are given in Table 3. Similar as for CAC scanning, the proportion of CTA acquisitions with retrospective gating and no tube current modulation significantly declined from 5.3 to 1.6% (p < 0.001), and the proportion of prospectively ECG-triggered acquisitions increased from 67.5 to 82.2% (p < 0.001). The median scan range was not documented during the first time period. It was unchanged between the second and third time interval. Tube current slightly went down over time from a median of 380 mAs to a median of 338 mAs (p < 0.001). Similarly, tube voltage decreased significantly. The median values are given in Table 2. Mean tube voltage decreased from 116 ± 28 to 113 ± 11 kV.
Changes in CT technology available at the participating centers were not systematically documented in the registry. Upon request, three centers reported operating a new CT machine, one each in 2012, 2013, and 2014, respectively. Accordingly, these changes all became apparent during the last time period and might in part explain the significant reduction of radiation dose during that period. However, the decrease in radiation dose was observed homogeneously among the participating centers and thus cannot solely be attributed to variations in patient recruitment or scanner technology.
To identify potential influences on radiation dose, demographic differences were analyzed with the median effective radiation dose of 3.6 mSv as a threshold. Whereas during the first of the three time periods, radiation dose was >3.6 mSv in 63.8% of coronary CTA acquisitions; this was the case in only 57.8% during the second and 29.9% during the third time period. Patients receiving a radiation dose above the median were significantly older (60.8 ± 11.8 vs. 58.4 ± 11.7 years, p < 0.001), more frequently male (64.1 vs. 61.0%, p = 0.024), had a higher BMI (27.5 ± 4.7 vs. 26.3 ± 4.1 kg/m2, p < 0.001), and their heart rate was higher (61.0 ± 9.6 vs. 57.7 ± 8.5 bpm, p < 0.001). Among the technical parameters, acquisition mode (retrospective rather than prospective) was associated with an increased radiation dose as were higher tube current and tube voltage.
Figure 2 shows the results of a multivariable logistic regression analysis incorporating the above named patient-related and technical factors. Time period remained a significant predictor of radiation dose, possibly as a consequence of changes in scanner technology. Using tertiles (3 time periods), the odds ratio (OR) of receiving a radiation dose >3.6 mSv was 0.84 (p = 0.008). Independent patient-related factors were age (OR 1.11 per 10 years, p = 0.017), BMI (OR 1.72 per 10 units, p < 0.001), and heart rate (OR 1.56 per 10 units, p < 0.001). The technical parameters scan mode, tube current, and tube voltage also retained their significant association with radiation dose.
Discussion
The main finding of the current analysis is that between 2009 and 2014, radiation dose associated with coronary CTA in the German CT registry significantly declined from a median of 5.6 mSv to a median of 2.5 mSv. Compared with the international PROTECTION I study published in the year the current registry started patient enrolment, i.e. 2009 [5]; radiation dose was reduced by a factor of approximately 5 only 5 years later. The recently published prospective SCOT-HEART trial examined 4146 patients with suspected coronary artery disease and compared a standard diagnostic strategy usually including exercise stress ECG with a strategy additionally including coronary CTA [10]. The CTA technology at the 12 SCOT-HEART study centers mainly consisted of modern 320-row scanners, and the median effective radiation exposure associated with coronary CTA was 4.1 mSv. Accordingly, the current radiation dose data from the German CT registry are reassuring in that first, overall radiation dose was comparably low, and second, radiation dose significantly declined over time. This was documented in a clinical setting within a registry including a broad and unselected patient population. Corroborating these results are data on CAC scanning obtained in almost 80% of the coronary CTA patients in the current registry. In previous reports, CAC scanning had usually been associated with a radiation dose of approximately 1 mSv [11], even though very low dose protocols have achieved <0.5 mSv [12]. Currently, the median dose was only 0.6 mSv, and it significantly declined to 0.4 mSv over time.
Probably, a combination of changes in scanning protocols, improved patient preparation, and new CT technology (“hard ware”) explains the trend for lower radiation dose with time observed in the current study. The proportion of scanning protocols using prospective triggering rather than retrospective gating steadily increased, and if retrospective gating was still employed, tube current modulation was added to save radiation. Further, tube current and tube voltage were decreased. This likely accounts at least in part for the continuous decrease in radiation dose observed during the three time periods. Tube current modulation added to retrospective gating has been reported to reduce radiation by 28–44% [13, 14]. Prospective triggering as opposed to retrospective gating has been reported to reduce radiation by an additional 57–82% [15, 16]. Low kV- (tube voltage) settings have been used to achieve the sub-mSv radiation dose range with the latest CT scanner generation [8].
Heart rate reduction was apparently performed more intensely later than earlier during the registry. Prospective triggering depends upon heart rate control. In multivariable analysis, these two parameters both were predictive of estimated radiation dose.
Changes in CT technology were not systematically documented in the current registry. Upon request, three participating centers reported installation of new scanners after 2011, which probably added to the decline in radiation dose observed during the last time period. Indeed, although a number of technical parameters changed, time period per se remained a strong and independent predictor of lower radiation dose in multivariable analysis. Accordingly, factors we did not account for in our analysis must have influenced radiation dose, most probably the improvement in scanner technology achieved during the last time period. In addition, some demographic data were related to a lower radiation dose such as lower age, lower BMI, and (only in univariate analysis) female sex. These factors cannot explain the declining dose over time, as except for age, no concordant trends over time were observed.
Lower BMI was an independent predictor of a lower radiation dose whereas female sex was not. Female patients had a smaller body size, probably accounting for the significant association of female sex with a lower radiation dose in univariate but not multivariate analysis. Conversely, increases in radiation dose were observed with increasing age. This can most likely be explained by the reasoning of the treating physicians who considered the priority for radiation safety less compelling compared with younger patients.
Estimating the risk associated with a low radiation dose is difficult. On the basis of calculations presented by Gerber et al. [4], a single exposure to a dose of 2.5 mSv might translate into a lifetime risk of developing a fatal malignancy of 1/8000. Given that the background risk of a fatal malignancy ranges in the order of 1/5 [4], it appears impossible in practice to quantify the exceedingly low additional risk conferred by coronary CTA. A younger age of the patient at the time of exposure would increase the risks, whereas the risk after age 60 is thought to be negligible [3]. Perhaps, it is more meaningful to compare the dose with average annual background exposure due to cosmic rays, radon and other natural sources, which in fact is thought to equal approximately 2.5 mSv in Western Europe [17]. Indeed, the coronary CTA-associated dose estimates observed in the current registry compare favorably with the dose usually ascribed to invasive coronary angiography and cardiac nuclear studies [4].
Limitations
Centers participating in the German CT registry represent cardiology units with specific expertise in cross-sectional cardiovascular imaging. Small centers or those embedded in a different setting were not part of the registry, precluding general conclusions. The participating centers were asked to include all patients consecutively, but there were no on-site visits or computer algorithms available for verifying truly consecutive patient inclusion. Therefore, we cannot rule out that variations in radiation dose were a result of varying patterns of patient recruitment among centers with different radiation dosing. However, a homogenous decline in radiation dose across the participating centers argues against this suggestion. Although the registry was prospective in nature, the exact mechanisms underlying the reduction in radiation dose could not be elucidated. However, estimates were possible of the respective influence of demographics (probably very little), changes in scanning protocol, and patient preparation.
Conclusions
When analyzing potential risks and benefits of medical imaging, it is important to consider the pre-test likelihood of the disease being examined and the therapeutic means available to treat it in case the diagnosis is made. In the elderly population, CAD is highly prevalent, and effective treatment options such as revascularization and medical therapy are readily available. Although CAD mortality is declining in the western world, the public health burden imposed by the disease is still highly problematic. On the individual patient level, preventive therapy is difficult, because global risk calculators are imprecise, and clinical symptoms as a warning sign are frequently absent [18]. Approximately, 1/3 of all patients suffer an acute coronary syndrome as the first manifestation of CAD [19]. This explains why current guidelines consider imaging methods for enhanced risk stratification, including CAC scanning, with a Class IIb indication [20]. Coronary CTA has usually been used to examine symptomatic patients with suspected CAD or, less frequently, patients awaiting non-coronary cardiac or extra-cardiac interventions [21]. Prospectively, it may also hold promise for prognostic improvements in selected patients at risk of advanced coronary atherosclerosis. In the SCOT-HEART trial, the use of coronary CTA compared favorably with exercise stress ECG in patients examined for suspected CAD [10]. The (possible) benefits of coronary CTA need to be weighed against the potential risks associated with its use. It is reassuring that in current clinical practice among German cardiology units with specific expertise in cross-sectional cardiovascular imaging, overall radiation dose of coronary CTA was comparably low, and a further decline could be demonstrated in recent years.
References
Montalescot G, Sechtem U, Achenbach S et al (2013) 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34:2949–3003 (erratum in: Eur Heart J 2014;35:2260–2261)
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ (2007) Radiation dose to patients from cardiac imaging. Circulation 116:1290–1305
Einstein AJ, Henzlova MJ, Rajagopalan S (2007) Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298:317–323
Gerber TC, Carr JJ, Arai AE et al (2009) Ionizing radiation in cardiac imaging. science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation 119:1056–1065
Hausleiter J, Meyer T, Hermann F et al (2009) Estimated radiation dose associated with cardiac CT angiography. JAMA 301:500–507
Hunold P, Voigt FM, Schmermund A et al (2003) Radiation exposure during cardiac CT: effective doses at multi-detector row CT and electron-beam CT. Radiology 226:145–152
Perrin M, Djaballah W, Moulin F et al (2015) Stress-first protocol for myocardial perfusion SPECT imaging with semiconductor cameras: high diagnostic performances with significant reduction in patient radiation doses. Eur J Nucl Med Mol Imaging 42:1004–1011
Hell MM, Bittner D, Schuhbäck A et al (2014) Prospectively ECG-triggered high-pitch coronary angiography with third-generation dual-source CT at 70 kVp tube voltage: feasibility, image quality, radiation dose, and effect of iterative reconstruction. J Cardiovasc Comput Tomogr 8:418–425
Bongartz G, Golding SJ, Jurik AG et al (2004) European guidelines for multislice computed tomography. Funded by the European Commission. Contract number FIGM-CT2000-20078-CT-TIP, March 2004. http://www.msct.eu/CT_Quality_Criteria.htm. Accessed 19 Oct 2016
SCOT-HEART investigators (2015) CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 385:2383–2391 (erratum in: Lancet 2015;385:2354)
Husmann L, Herzog BA, Burger IA et al (2010) Usefulness of additional coronary calcium scoring in low-dose CT coronary angiography with prospective ECG-triggering impact on total effective radiation dose and diagnostic accuracy. Acad Radiol 17:201–206
Marwan M, Mettin C, Pflederer T et al (2013) Very low-dose coronary artery calcium scanning with high-pitch spiral acquisition mode: comparison between 120-kV and 100-kV tube voltage protocols. J Cardiovasc Comput Tomogr 7:32–38
Poll LW, Cohnen M, Brachten S, Ewen K, Mödder U (2002) Dose reduction in multi-slice CT of the heart by use of ECG-controlled tube current modulation (“ECG pulsing”): phantom measurements. Rofo 174:1500–1505
Gerber TC, Stratmann BP, Kuzo RS, Kantor B, Morin RL (2005) Effect of acquisition technique on radiation dose and image quality in multidetector row computed tomography coronary angiography with submillimeter collimation. Invest Radiol 40:556–563
Gopal A, Mao SS, Karlsberg D et al (2009) Radiation reduction with prospective ECG-triggering acquisition using 64-multidetector computed tomographic angiography. Int J Cardiovasc Imaging 25:405–416
Arnoldi E, Johnson TR, Rist C et al (2009) Adequate image quality with reduced radiation dose in prospectively triggered coronary CTA compared with retrospective techniques. Eur Radiol 19:2147–2155
European Commission In: De Cort M, Tollefsen T, Marsano A, Gitzinger C (eds) EUR 23950—environmental radioactivity in the european community 2004–2006. Office for Official Publications of the European Communities 2009, Luxembourg. https://rem.jrc.ec.europa.eu/RemWeb/Reports.aspx, Accessed 23 Oct 2016
Erbel R, Budoff M (2012) Improvement of cardiovascular risk prediction using coronary imaging: subclinical atherosclerosis, the memory of lifetime risk factor exposure. Eur Heart J 33:1201–1213
Löwel H, Meisinger C, Heier M, Hörmann A, von Scheidt W (2005) Herzinfarkt und koronare Sterblichkeit in Süddeutschland. Deutsches Ärzteblatt 103:A616–A622
Piepoli MF, Hoes AW, Agewall S et al (2016) 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in clinical practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 37:2315–2381
Opolski MP, Kim WK, Liebetrau C et al (2015) Diagnostic accuracy of computed tomography angiography for the detection of coronary artery disease in patients referred for transcatheter aortic valve implantation. Clin Res Cardiol 104:471–480
Acknowledgements
Funding was provided by Stiftung Institut für Herzinfarktforschung, Ludwigshafen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Axel Schmermund, Mohamed Marwan, and Stephan Achenbach have received speaker honoraria from Siemens Healthineers Deutschland, manufacturer of cardiac CT machines.
Appendix
Appendix
Centers participating in the German cardiac CT registry in alphabetical order:
-
Cardioangiologisches Centrum Bethanien, Frankfurt,
-
Deutsches Herzzentrum, Munich,
-
Elisabeth Krankenhaus Essen,
-
Herzzentrum Bogenhausen, Munich,
-
Kerckhoff Klinik, Bad Nauheim,
-
Klinikum am Eichert, Göppingen,
-
Klinikum Ludwigshafen,
-
Klinikum Traunstein,
-
Universitätsklinikum Erlangen,
-
Universitätsklinikum Gießen,
-
Universitätsklinikum Heidelberg,
-
Universitätsklinikum Tübingen.
Rights and permissions
About this article
Cite this article
Schmermund, A., Marwan, M., Hausleiter, J. et al. Declining radiation dose of coronary computed tomography angiography: German cardiac CT registry experience 2009–2014. Clin Res Cardiol 106, 905–912 (2017). https://doi.org/10.1007/s00392-017-1136-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1136-8