Abstract
Background
Early repolarization pattern (ER) gained attention as a risk factor for ventricular arrhythmia and sudden cardiac death in the general population. While electrocardiographic abnormalities are frequent findings in stroke patients, data on ER pattern in this population are lacking.
Methods
We assessed the prevalence of ER pattern in consecutive acute stroke patients at a tertiary stroke center. Functional outcome after 90 days was analyzed to determine the effect of an ER pattern on mortality. Multivariate logistic regression analysis was used to identify factors associated with an ER pattern.
Results
Out of 1141 consecutive stroke patients 771 patients remained for analysis after application of exclusion criteria. ER was observed in 62 (8.04 %) patients. ER was more prevalent among subjects with intracerebral and subarachnoidal hemorrhage (13.0 %) than among patients with ischemic stroke (7.0 %; p = 0.024). Multiple regression analysis revealed QRS-duration (OR 0.972 95 % CI 0.950–0.994, p = 0.012), QT-duration (OR 1.009, 95 % CI 1.004–1.014, p = 0.001) and mechanical ventilation on admission (OR 0.320, 95 % CI 0.136–0.752, p = 0.009) as independent predictors for ER. Overall ER on admission was not associated with increased mortality at 3-month follow-up (ER 11.3 % vs. non-ER 9.2 %; p = 0.582).
Conclusions
ER is frequently found among patients with acute cerebrovascular events and is more prevalent in patients with hemorrhagic compared to ischemic events. Our study yields no evidence that ER is associated with worse outcome or mortality after stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Electrocardiographic abnormalities and cardiac arrhythmias are frequent findings in patients with acute stroke and may complicate the course of cerebrovascular disorders [1]. Although many changes may result from cardiac comorbidities and coexisting vascular risk factors, cerebral lesions themselves were shown to disturb central autonomic control [2] resulting in impaired cardiac function and even sudden death [3–6]. These mechanisms are further supported by post-mortem analyses in patients with ischemic stroke, as lethal ECG abnormalities were associated with focal myocytolysis in absence of coronary artery disease [7]. Moreover, several experimental models linked elevated plasma norepinephrine levels after stroke to impaired cardiac function [8, 9] and lesions in the right insular cortex were associated with disturbance of cardiac repolarization [10, 11]. This unique and complex interaction has led to the use of the term “heart–brain-connection” [9]. ECG changes have been reported primarily in patients suffering from intracerebral hemorrhage [12] and subarachnoid hemorrhage [13], but case series also revealed abnormalities in up to 76 % of ischemic stroke patients [14, 15]. Common ECG changes during the acute phase of stroke include QT-prolongation, ST-segment, T wave and U wave abnormalities [11, 16], bundle branch block [15], but also more serious complications like tachy- and bradycardic arrhythmia [17]. Moreover, several studies reported an impact of abnormalities on ECG on stroke outcome at 3 months [18–20]. Recently, early repolarization, a common electrocardiographic finding that was considered to be benign for decades, gained attention as a risk factor for increased cardiac mortality and also sudden cardiac arrest in otherwise healthy young patients [21, 22]. Though one case report draw attention to a possible link between alteration of the ER pattern and infarction of the left insular cortex [23], systematic data on the prevalence of ER patterns in patients with acute cerebrovascular events are still lacking. The aim of the current study was therefore to determine the overall prevalence of ER pattern in acute stroke patients and to clarify, if ER pattern is related to mortality.
Methods
Study design and patient inclusion
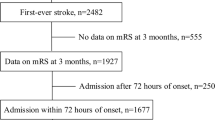
Consecutive patients with acute ischemic or hemorrhagic stroke admitted to the Department of Neurology at the University Hospital Erlangen, Germany between February 2011 and January 2012 (n = 1141) were prospectively included in this study. The study was approved by the local ethics committee of the Medical faculty, University of Erlangen-Nuremberg. The diagnosis of stroke was established on the basis of clinical findings and diagnostic imaging in accordance with current guidelines [24]. A detailed medical history and clinical information were obtained from every patient. Stroke severity was assessed on admission using the National Institutes of Health Stroke Scale (NIHSS) [25]. Cardiovascular stroke unit work-up with echocardiography, sonography of cerebral arteries, risk-factor stratification and laboratory testing was performed following current recommendations [26, 27]. A 12-lead ECG was recorded with a sensitivity of 10 mm/mv and a paper speed of 50 mm/s in all stroke patients within 1–4 h after admission to our emergency department. Patients with implanted pacemaker, significant ventricular conduction delay (QRS >120 ms) as well as atrial fibrillation were excluded from analysis [21, 22]. Pre-admission data and outcome measure were evaluated using the modified Rankin Scale (mRS) [28]. The mRS at 3 months was obtained by a structured telephone interview which was conducted by two scale trained and certified physicians (T.B., B.K.).
Analysis of electrocardiography
An experienced physician manually evaluated all ECGs. Routine ECG parameters were analyzed according to current guidelines [29]. QTc was calculated with the Bazett’s formula as QT√R–R [30]. For diagnosis of an early repolarization pattern the following criteria were applied: elevation of the J-point more than 0.1 mV in at least 2 inferior or lateral leads [31]. The pattern was classified as either notched with a positive J deflection inscribed on the S wave or slurred with a flat transition from QRS to ST-segment [21, 32]. Additionally, ER was coded according to the recently published classification: horizontal/descending or concave/rapidly ascending, defined as more than 0.1 mV elevation of ST-segment within 100 ms after the J-point or a permanent elevated ST-segment of more than 0.1 mV [31, 33]. Two additional investigators reviewed all ECGs with suspected ER and the diagnosis of ER was limited to cases, where it was confirmed by the consensus of all three physicians.
Statistical analysis
Data were processed using the Office 2010 (Microsoft Corp.) software package, statistical analysis was performed with SPSS 21.0 (SPSS Inc.). Normality of distribution was tested using the Kolmogorov–Smirnov and Shapiro–Wilk tests. Normal distributed data are presented as mean ± SD (compared using Student T test), other data as median and interquartile ranges (compared using Mann–Whitney-U-Test). The Pearson-χ 2 and Fisher’s exact test were used to compare categorized variables. Parameters reaching a statistical trend in univariate testing (p < 0.1) were included into the stepwise backwards logistic regression model with prevalence of ER as the dependent variable. The level of significance was set a priori at p < 0.05. Statistical tests were two-sided.
Results
Baseline characteristics, admission status and laboratory values
1141 patients with acute stroke were treated in our tertiary stroke center from February 2011 to January 2012. Baseline study 12-lead ECGs on admission were available for analysis in 1062 of the 1141 patients. In 79 cases the ECG was of insufficient quality for evaluation of ER in the judgement of the ECG evaluators and was excluded from our analysis. In addition, patients with atrial fibrillation and atrial flutter (n = 181, 19.4 %), implanted cardiac pacemaker (n = 22) and significant ventricular conduction delay (n = 63) were excluded. 771 patients remained for analysis, of whom 633 patients had ischemic stroke, 90 patients intracerebral hemorrhage and 48 patients subarachnoid hemorrhage. Baseline characteristics of the study cohort are shown in Table 1 (for baseline characteristics stratified by ER and type of stroke please see Supplementary Table 1). Patients with ER showed a significant higher rate of mechanical ventilation on admission (ER 17.7 % vs. non-ER 3.8 %, p < 0.001), especially in patients with intracerebral hemorrhage (ER 70 % vs. non-ER 13.8 %, p < 0.001). Diabetes mellitus was less prevalent among patients with ER (16.1 % vs. non-ER 29.8 %, p = 0.023). None of the other laboratory parameters showed a significant association with the presence of ER on admission (please see Supplementary Table 2).
Electrocardiographic analysis and prevalence of early repolarization pattern
Electrocardiographic characteristics are presented in Table 1 (for stratification by type of stroke please see Supplementary Table 3). Overall 8.0 % of patients were presented with ER on admission. ER was observed in 7.0 % of patients with ischemic stroke and in 11.1 and 16.7 % in patients with intracerebral and subarachnoid hemorrhage, respectively. Thus, the prevalence of ER was significantly higher in patients with hemorrhagic stroke (ICH/SAH) than in ischemic stroke (p = 0.024). As the hospital is a tertiary stroke center, 18.3 % of patients were transferred from another hospital. The mean time between stroke onset and recording of an ECG was 322 (127–974) min in patients who arrive at our hospital at first and 2406 (1332–7722) min in transferred patients. Though this time difference had no impact on the appearance of an ER pattern (p = 0.488).
Typical examples of ECGs from subjects of the study group with either a slurred or notched ER pattern are shown in Fig. 1. The proportion of a slurred pattern (67.7 %, n = 41) was higher than a notched pattern (32.3 %; n = 21). Among these subjects, the elevation was observed in the inferior leads in 35 subjects (56.5 %) and in the lateral leads in 35 subjects (56.5 %). 51 (82.3 %) of the ER patterns showed a horizontal/descending pattern, while 11 (17.7 %) presented an ascending/upsloping pattern.
Predictors of early repolarization
As shown in Table 1, patients with ER had a significant lower heart rate (65.5 vs. 70.0/min; p = 0.005), shorter QRS-duration (80 vs. 90 ms; p = 0.009) and longer QT-duration (400 vs. 390 ms; p < 0.001). In addition to those parameters type of stroke, NIHSS-score, mechanical ventilation on admission, diabetes, hypertension and age showed a trend in univariate analysis and were included into a linear regression model with ER as the dependent variable. QRS-duration (OR 0.972; 95 % CI 0.950–0.994; p = 0.012), QT-duration (OR 1.009; 95 % CI 1.004–1.014; p = 0.001) as well as mechanical ventilation on admission (OR 0.320; 95 % CI 0.136–0.752; p = 0.009) remained as independent predictors of ER (Table 2).
Association of ER with functional outcome and mortality
Functional outcome and mortality for the entire cohort is presented in Table 1. There was no association of ER and functional outcome for the entire cohort or in any of the subgroups. Also the mortality rate after 90 days revealed no difference between patients with and without ER (11.3 vs. 9.2 %, p = 0.582) in the entire cohort. Analysis of the malignant ER pattern with a horizontal/descending pattern did not reveal a difference in terms of mortality (p = 0.746). Subgroup analysis showed an increased mortality rate in ICH patients with ER (50 vs. 16.3 %, p = 0.026). However, patients with ER were clinically more severely affected and had presented with a worse NIHSS-score [38 (8–40) vs. 9 (5–17), p = 0.011] as well as higher rate of mechanical ventilation on admission (ER 70 % vs. non-ER 13.8 %, p < 0.001). Due to the low number of patients multivariate logistic regression was not feasible in this subgroup.
Discussion
Cardiac arrhythmias are a frequent and potentially fatal complication in the acute phase after stroke [1, 5, 17]. Recently, ER pattern emerged as a risk factor for sudden cardiac death in healthy adults [21]. A multitude of studies were published about the prevalence of ER and the associated risk of cardiac death in the general population as well as in various diseases [21, 22, 33–39]. Our data represent the first systematic evaluation in acute stroke patients. ER was a frequent finding in our cohort but we found no evidence of an association with mortality. Several important aspects emerge from the data.
ER pattern are common among stroke patients
Overall prevalence of ER was 8.0 %, ranging from 7.0 % in patients with ischemic stroke to higher rates of 11.1 and 16.7 % in patients with intracerebral and subarachnoidal hemorrhage, respectively. According to a recently published meta-analysis the prevalence of ER in the general population varies from 0.9 to 31 % depending on the cohort and the mean age with a higher prevalence in younger patients. It has to be noted that with a mean age between 38 and 55 years in the included studies, cohorts in the meta-analysis were younger compared to ours as well as other typical stroke cohorts [40, 41].
Mechanical ventilation on admission, QRS-duration and QT-prolongation are independent predictors of the presence of an ER pattern
In concordance with other studies we demonstrated that ER is related to a slower heart rate. Time-dependent recovery of Ito from inactivation may be one possible mechanism [36, 42, 43]. In logistic regression model QRS-duration, QT-duration as well as intubation on admission demonstrated a significant association with occurrence of ER. While QRS-duration was significantly shorter in patients with ER in our cohort, other studies yield conflicting results. Several authors reported a slight increase or no relationship in QRS-duration [21, 32], while others also show a shorter QRS-duration [36]. Watanabe et al. reported that a shorter QTc interval might be associated with ER and share common cardiac channel genetic mutations with short QT syndrome. We were unable to reproduce this finding as ER positive patients showed comparable QTc times to non-ER patients. QT time was even slightly longer in patients with ER.
Association of ER and mortality after stroke
A number of studies suggested a relationship between ER and sudden cardiac death, a complication that also occurs in early phases after ischemic stroke [21, 22, 32, 40]. Although we found a significant prevalence of ER in our study population, there was no evidence that ER may act as a surrogate parameter identifying patients at risk for sudden cardiac death after stroke. Recently, Tikkanen et al. [33] classified ER into two different groups based on the ST-segment: a benign ER pattern with rapidly ascending ST-segment and a horizontal/descending ST-segment morphology. However, our study did not discover an effect of a malignant ER pattern with horizontal/descending ST-segment morphology on mortality after stroke.
Limitations
The main limitation is the single center design of our study. Although we present the first systematic evaluation of prevalence and impact of ER in a stroke population, the analysis was limited due to the low number of events especially sudden cardiac deaths. Our study population represents a typical population on a Stroke Unit; therefore, many patients had to be excluded mainly due to the presence of atrial fibrillation. Since our follow-up was limited to 3 months we were not able to capture events that may occur later. However, previous studies suggest that the most vulnerable phase for cardiac complications will be the acute to subacute setting after stroke.
Conclusions
Our results demonstrate that ER is frequently seen among acute stroke patients and is more prevalent in hemorrhagic than in ischemic stroke. There was no evidence that ER is a surrogate parameter identifying patients at risk for cardiac complications after stroke.
References
Klingelhofer J, Sander D (1997) Cardiovascular consequences of clinical stroke. Baillieres Clin Neurol 6:309–335
Prosser J, MacGregor L, Lees KR, Diener HC, Hacke W, Davis S (2007) Predictors of early cardiac morbidity and mortality after ischemic stroke. Stroke 38:2295–2302
Christensen H, Boysen G, Johannesen HH (2004) Serum-cortisol reflects severity and mortality in acute stroke. J Neurol Sci 217:175–180
Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ (1977) Prognostic value of the stress response following stroke. JAMA J Am Med Assoc 238:1374–1376
Soros P, Hachinski V (2012) Cardiovascular and neurological causes of sudden death after ischaemic stroke. Lancet Neurol 11:179–188
Koppikar S, Baranchuk A, Guzman JC, Morillo CA (2013) Stroke and ventricular arrhythmias. Int J Cardiol 168:653–659
Tobias SL, Bookatz BJ, Diamond TH (1987) Myocardial damage and electrocardiographic changes in acute cerebrovascular hemorrhage: a report of three cases and review. Heart Lung J Crit Care 16:521–526
Micieli G, Cavallini A (2008) The autonomic nervous system and ischemic stroke: a reciprocal interdependence. Clin Auton Res 18:308–317
Samuels MA (2007) The brain-heart connection. Circulation 116:77–84
Oppenheimer S (2006) Cerebrogenic cardiac arrhythmias: cortical lateralization and clinical significance. Clin Auton Res 16:6–11
Katsanos AH, Korantzopoulos P, Tsivgoulis G, Kyritsis AP, Kosmidou M, Giannopoulos S (2013) Electrocardiographic abnormalities and cardiac arrhythmias in structural brain lesions. Int J Cardiol 167:328–334
Cropp GJ, Manning GW (1960) Electrocardiographic changes simulating myocardial ischemia and infarction associated with spontaneous intracranial hemorrhage. Circulation 22:25–38
Byer E, Ashman R, Toth LA (1947) Electrocardiograms with large, upright T waves and long Q-T intervals. Am Heart J 33:796–806
Fentz V, Gormsen J (1962) Electrocardiographic patterns in patients with cerebrovascular accidents. Circulation 25:22–28
Khechinashvili G, Asplund K (2002) Electrocardiographic changes in patients with acute stroke: a systematic review. Cerebrovasc Dis 14:67–76
Goldstein DS (1979) The electrocardiogram in stroke: relationship to pathophysiological type and comparison with prior tracings. Stroke 10:253–259
Kallmunzer B, Breuer L, Kahl N, Bobinger T, Raaz-Schrauder D, Huttner HB et al (2012) Serious cardiac arrhythmias after stroke: incidence, time course, and predictors–a systematic, prospective analysis. Stroke 43:2892–2897
Christensen H, Fogh Christensen A, Boysen G (2005) Abnormalities on ECG and telemetry predict stroke outcome at 3 months. J Neurol Sci 234:99–103
Dogan A, Tunc E, Ozturk M, Kerman M, Akhan G (2004) Electrocardiographic changes in patients with ischaemic stroke and their prognostic importance. Int J Clin Pract 58:436–440
Providencia R, Barra S, Paiva L (2013) Atrial fibrillation, elevated troponin, ischemic stroke and adverse outcomes: understanding the connection. Clin Res Cardiol Off J Ger Card Soc 102:701–711
Haissaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L et al (2008) Sudden cardiac arrest associated with early repolarization. N Engl J Med 358:2016–2023
Sinner MF, Reinhard W, Muller M, Beckmann BM, Martens E, Perz S, et al. (2010) Association of early repolarization pattern on ECG with risk of cardiac and all-cause mortality: a population-based prospective cohort study (MONICA/KORA). PLoS Med 7: e1000314
Kallmunzer B, Kuramatsu J, Breuer L, Engelhorn T, Kohrmann M (2011) Early repolarisation syndrome and ischemic stroke: is there a link? Cerebrovasc Dis 31:414–415
Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:870–947
Kasner SE (2006) Clinical interpretation and use of stroke scales. Lancet Neurol 5:603–612
European Stroke Organisation (ESO) Executive Committee (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack. Cerebrovasc Dis 25: 457–507
Laufs U, Hoppe UC, Rosenkranz S, Kirchhof P, Bohm M, Diener HC et al (2010) Cardiological evaluation after cerebral ischaemia : consensus statement of the Working Group Heart and Brain of the German Cardiac Society-Cardiovascular Research (DGK) and the German Stroke Society (DSG). Clin Res Cardiol Off J Ger Cardiac Soc 99:609–625
Sulter G, Steen C, De Keyser J (1999) Use of the Barthel index and modified Rankin scale in acute stroke trials. Stroke 30:1538–1541
O’Keefe JH (2002) The complete guide to ECGs. 2nd ed. Royal Physicians Press, Oak
Villa A, Bacchetta A, Milani O, Omboni E (2001) QT interval prolongation as predictor of early mortality in acute ischemic stroke patients. Am J Emerg Med 19:332–333
Tikkanen JT, Junttila MJ, Anttonen O, Aro AL, Luttinen S, Kerola T et al (2011) Early repolarization: electrocardiographic phenotypes associated with favorable long-term outcome. Circulation 123:2666–2673
Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA et al (2009) Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med 361:2529–2537
Tikkanen JT, Huikuri HV (2013) Early repolarization ECG pattern in the Finnish general population. J Electrocardiol 46:439–441
Walsh JA 3rd, Ilkhanoff L, Soliman EZ, Prineas R, Liu K, Ning H et al (2013) Natural history of the early repolarization pattern in a biracial cohort: CARDIA (Coronary Artery Risk Development in Young Adults) Study. J Am Coll Cardiol 61:863–869
Furukawa Y, Yamada T, Morita T, Iwasaki Y, Kawasaki M, Kikuchi A et al (2013) Early repolarization pattern associated with sudden cardiac death: long-term follow-up in patients with chronic heart failure. J Cardiovasc Electrophysiol 24:632–639
Hajhosseiny R, Rajani R, Khavandi K, Sebag FA, Mashayekhi S, Wright M et al (2013) The prevalence of electrocardiographic early repolarization in an adult cohort with chronic kidney disease and its impact upon all-cause mortality and progression to dialysis. Front Physiol 4:127
Noseworthy PA, Weiner R, Kim J, Keelara V, Wang F, Berkstresser B, et al. (2011) Early repolarization pattern in competitive athletes: clinical correlates and the effects of exercise training. Circ Arrhythm Electrophysiol 4: 432–440
Rollin A, Maury P, Bongard V, Sacher F, Delay M, Duparc A et al (2012) Prevalence, prognosis, and identification of the malignant form of early repolarization pattern in a population-based study. Am J Cardiol 110:1302–1308
Uberoi A, Jain NA, Perez M, Weinkopff A, Ashley E, Hadley D et al (2011) Early repolarization in an ambulatory clinical population. Circulation 124:2208–2214
Wu SH, Lin XX, Cheng YJ, Qiang CC, Zhang J (2013) Early repolarization pattern and risk for arrhythmia death: a meta-analysis. J Am Coll Cardiol 61:645–650
Greenfield JC Jr, Rembert JC (2013) The prevalence of lateral lead early repolarization in otherwise normal electrocardiograms as a function of age. J Electrocardiol 46:334–335
Antzelevitch C, Yan GX (2010) J wave syndromes. Heart Rhythm 7:549–558
Benito B, Guasch E, Rivard L, Nattel S (2010) Clinical and mechanistic issues in early repolarization of normal variants and lethal arrhythmia syndromes. J Am Coll Cardiol 56:1177–1186
Conflict of interest
The authors report no disclosures relevant to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bobinger, T., Kallmünzer, B., Kopp, M. et al. Prevalence and impact on outcome of electrocardiographic early repolarization patterns among stroke patients: a prospective observational study. Clin Res Cardiol 104, 666–671 (2015). https://doi.org/10.1007/s00392-015-0831-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0831-6