Abstract
Purpose
Angiopoietin-2 (Ang-2) impairs endothelial integrity. The association of Ang-2 in the presence of oedema and outcome of patients with acute decompensated heart failure (ADHF) has not been investigated.
Methods and results
Angiopoietin-2 was measured in 132 ADHF patients, which were included in a monocentric, prospective trial (Clinicaltrials.gov: NCT01429857). Primary endpoint was all-cause death at 6-months. 20 healthy persons served as control group (HC). In ADHF patients, mean Ang-2 concentration at admission was significantly increased compared to HC (2,111 ± 117 vs. 971 ± 46 pg/ml, p = 0.0002). Ang-2 was increased in patients with compared to those without peripheral oedema (2,294 ± 140 vs. 1,540 ± 170 pg/ml; p = 0.009) and in patients with NYHA class III or IV symptoms compared to those with NYHA class II symptoms (2,256 ± 132 vs. 1,341 ± 380 pg/ml, p = 0.023). During the 6-month follow-up, 10 patients died. In survivors, Ang-2 significantly decreased at discharge compared to admission (2,046 ± 118 vs. 1,431 ± 93 pg/ml; p < 0.0001). Non-survivors showed no difference between Ang-2 concentration at admission and discharge (3,296 ± 594 vs. 2,909 ± 536 pg/ml). Ang-2 concentrations at discharge above 2,500 pg/ml were associated with an increased risk of death compared to Ang-2 concentrations below this threshold (Hazard ratio 8.8; 95 % confidence interval; 2.48–31.16, p < 0.001).
Conclusion
In ADHF patients, Ang-2 is significantly increased compared to healthy controls, shows a relationship in the presence of oedema and is a predictor of poor outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute decompensated heart failure (ADHF) is defined as rapid onset of, or change in, symptoms and signs of heart failure. It is a prevalent disease with a poor prognosis and a high socio-economic burden. Being a potentially life-threatening condition, it requires immediate medical attention and usually leads to urgent admission to hospital [1]. The pathophysiology of AHF and subsequent cardiogenic shock is characterized by a strong compensatory and maladaptive neurohormonal response with systemic vasoconstriction and fluid retention which, in turn, initiates a downward spiral resulting in tissue hypoperfusion, hypoxaemia, and systemic inflammatory response syndrome (SIRS) [2]. In this vicious circle, a deranged endothelial barrier function seems to play a central role. However, the underlying molecular mechanisms remain largely unknown. Endothelial barrier function is controlled by the endothelial specific Angiopoietin-(Ang)-Tie2 ligand-receptor system [3]. Binding of the agonist Ang-1 to the Tie2 receptor promotes vessel integrity, inhibits vascular leakage and suppresses inflammatory gene expression [4]. The counter-player Ang-2 inhibits binding of Ang-1 to Tie2 disrupting the Tie2 signaling resulting in impaired endothelial integrity and thus, in vascular leakage [5–7]. Furthermore, it is proinflammatory, promotes endothelial cell apoptosis and increases adhesion of neutrophils [8]. Ang-2 is stored in the Weibel–Palade bodies within the endothelial cells and is rapidly released upon various stimuli including inflammatory cytokines [5], activated platelets and leukocytes [6], and changes in blood flow as well as in oxygenation [9, 10]. It represents a prognostic marker reflecting endothelial dysfunction and organ injury in patients with acute lung injury and sepsis [11–13]. In patients with chronic heart failure, Ang-2 levels are significantly elevated compared to healthy controls and related to a reduced hemodynamic and functional status [14, 15]. Furthermore, Ang-2 is an independent predictor for incident heart failure in patients with acute myocardial infarction [16]. Recently, we were able to show a strong prognostic role of Ang-2 in 96 patients with cardiogenic shock (CS) [17]. Beyond this background, our hypothesis was that Ang-2 might be involved in the pathophysiology of ADHF. In the present study, we aimed to assess the prognostic role of Ang-2 in patients with ADHF admitted to our emergency department.
Methods
Patients and study design
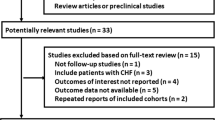
Angiopoietin-2 was measured in serum samples of 132 patients with ADHF, which were included in a prospective trial conducted in our department (Clinicaltrials.gov: NCT01429857). ADHF was clinically diagnosed on the basis in the presence of symptoms or signs of decompensated heart failure requiring intravenous diuretics, such as dyspnea, rales, pulmonary edema/vascular congestion on chest radiography, peripheral edema or ascites. The following exclusion criteria were defined: acute coronary syndrome, decompensation of non-cardiac cause, alternative cause for symptoms (chronic lung disease, anemia, pulmonary embolism) and severely impaired renal function (cystatin C GFR <15 ml/min). 20 healthy persons served as a control group (HC). The study was performed with approval of the local ethics committee and performed according to the guidelines of good clinical practice. Informed written consent was obtained from patient or substitute decision makers. The primary endpoint of the study was all-cause mortality at 6 months.
Laboratory measurements
Blood samples were taken under standardized conditions immediately after admission and at the day of discharge of the patients. The samples were centrifuged at 3,000g for 10 min at room temperature. Supernatants were stored in aliquots at −80 °C until further use. All Ang-2 and N-terminal fragment of the B-type natriuretic peptide (NT-pro-BNP) measurements were performed with commercially available enzyme-linked immunosorbent assays (ELISA) (Ang-2: R&D Systems, Minneapolis, MN, USA; NT-pro-BNP: Roche Diagnostics, Mannheim, Germany). For the Ang-2 assay, the detection limit is 21.3 pg/ml, the intra-assay variability 5.8 %, and the inter-assay variability 8.9 %. Renal function was assessed by measuring cystatin C GFR. High-sensitive troponin T (hsTnT) was measured with the Elecsys® Troponin T high-sensitive assay (Roche Diagnostics, Mannheim, Germany; 99th-percentile-cutoff 14 pg/ml).
Statistics
Data management and statistical analysis were performed with SPSS statistics version 20.0 and GraphPad Prism version 5.0. Two-sided p values <0.05 were considered statistically significant. Categorical variables are presented as percentage of patients and compared by χ 2 test. Continuous data are expressed as mean ± standard error of the mean, and compared by Student’s t test or Mann–Whitney test, as appropriate. Cumulative all-cause mortality throughout the 6-month follow-up period was assessed with the use of cox regression analysis with two groups stratified according to the Ang-2 concentration at discharge (cutoff value: 2,500 pg/ml). Receiver Operating Characteristic (ROC) analysis was performed to assess the discriminative power with respect to the primary endpoint.
Results
Baseline characteristics
Baseline characteristics of the enrolled patients are presented in Table 1. Patients had a mean age of 75 ± 1 years. Approximately half (47 %) of the patients were in sinus rhythm; mean systolic (SBP)/diastolic (DBP) blood pressure was 139 ± 3/73 ± 2 mmHg. Most (58 %) patients presented with a reduced left ventricular ejection fraction (LVEF) as cause of ADHF. The majority of patients complained class NYHA IV or NYHA III symptoms. Mean NT-proBNP was 6,136 ± 623 pg/ml. Patients were characterized by relevant comorbidities such as coronary artery disease (52 %), diabetes mellitus (43 %), arterial hypertension (72 %), and COPD (20 %). Overall, renal function was depressed with a mean glomerular filtration rate (GFR) assessed by cystatin C of 51 ± 2 ml/min. During the 6-month follow-up period, 10 patients (7.6 %) died. Most data such as age, sex, heart rate, medication, comorbidities as well as main clinical parameters including blood pressure and LVEF did not differ between survivors and non-survivors. However, non-survivors were characterized by a lower cystatin C GFR, higher NT-pro BNP and higher high-sensitive troponin T levels. Notably, non-survivors were less well treated at baseline, especially with diuretics.
Ang-2 concentration in ADHF
In ADHF patients, mean Ang-2 concentrations at admission were significantly increased compared to HC (2,111 ± 117 vs. 971 ± 46 pg/ml, p = 0.0002), Fig. 1a. Interestingly, ADHF patients with peripheral oedema (n = 100) had higher Ang-2 concentrations compared to those without peripheral oedema (2,294 ± 140 vs. 1,540 ± 170 pg/ml; p = 0.009), Fig. 1b. Furthermore, Ang-2 was elevated in patients with NYHA class III or IV compared to those with NYHA class I or II (2,256 ± 132 vs. 1,341 ± 380 pg/ml, p = 0.023), Fig. 1c.
Prognostic relevance of Ang-2 levels on admission and discharge
Ang-2 concentrations in survivors and non-survivors
Mean hospital stay was 13 ± 1 days. During the subsequent 6-month follow-up period, 10 patients (7.6 %) died. Figure 2a depicts the Ang-2 concentrations at admission and at discharge in the overall population as well as after stratification of the patients in survivors (n = 122) and non-survivors (n = 10) according to all-cause mortality during the 6-month follow-up. Ang-2 concentrations at admission were increased in non-survivors compared to survivors; however, this difference did not reach statistical significance (2,909 ± 536 vs. 2,046 ± 118 pg/ml, p = 0.104). At discharge, non-survivors had more than twofold higher Ang-2 concentrations compared to survivors (3,296 ± 594 vs. 1,431 ± 93 pg/ml, p < 0.001). In the overall population as well as in survivors, Ang-2 decreased at discharge compared to admission (overall: 1,572 ± 105 vs. 2,111 ± 117, p < 0.0001; survivors: 1,431 ± 93 vs. 2,046 ± 118 pg/ml; p < 0.0001). In non-survivors, however, we observed no difference in Ang-2 concentration at discharge compared to admission (3,296 ± 594 vs. 2,909 ± 536 pg/ml, p = 0.878), Fig. 2a.
a Ang-2 levels on admission and discharge in the overall population and after stratifying the patients in survivors and non-survivors according to all-cause mortality. b Cumulative incidence of the primary endpoint according to groups of patients stratified according to Ang-2 concentrations at admission and discharge. c Multivariate cox regression analysis for the primary endpoint according to Ang-2 concentration at discharge (below and above cutoff value of 2,500 pg/ml), adjusted for age, gender and cystatin C GFR. HR Hazard ratio, CI Confidence interval
Ang-2 concentrations and outcome
Patients were stratified in groups according to their Ang-2 concentration at admission (Ang-2_A) and at discharge (Ang-2_D). The cutoff value of 2,500 pg/ml was chosen since it was shown to be of prognostic relevance in CS [17] (Group 1: Ang-2_A <2,500 pg/ml; Ang-2_D <2,500 pg/ml; group 2: Ang-2_A >2,500 pg/ml; Ang-2_D <2,500 pg/ml: group 3: Ang-2_A >2,500 pg/ml; Ang-2_D >2,500 pg/ml; group 4: Ang-2_A <2,500 pg/ml; Ang-2_D >2,500 pg/ml). In the Kaplan–Meier analysis, patients with Ang-2 concentrations below 2,500 pg/ml at both time points had the best outcome whereas patients presenting with low Ang-2 at admission and increased Ang-2 at discharge had the worst prognosis, Fig. 2b.
In the ROC analysis, Ang-2 concentrations at discharge had a high diagnostic accuracy for the prediction of the primary endpoint (all-cause mortality) with an area under the curve (AUC) of 0.81 (95 % confidence interval (CI); 0.63–0.98; p = 0.001). An additional analysis was performed comparing the AUC of Ang-2 alone versus NT-pro BNP alone versus the combination of Ang-2 and NT-pro BNP. Herein, Ang-2 showed a trend towards a higher AUC compared to NT-pro BNP. The combination of Ang-2 and NT-pro BNP had a higher diagnostic accuracy than the respective variables alone, Table 2. However, this difference did not reach statistical significance. Ang-2 at admission as well as the observed delta of Ang-2 between admission and discharge did not show a significant predictive role in ROC analysis (admission: AUC 0.66; 95 % CI; 0.46–0.85; p = 0.1; delta: AUC 0.62; 95 % CI; 0.39–0.85; p = 0.2). Therefore, Ang-2 at discharge was used for further outcome analysis. Herein, Ang-2 concentrations at discharge above 2,500 pg/ml were associated with a profoundly increased risk of death compared to Ang-2 concentrations below this threshold (Hazard ratio (HR) 8.8; 95 % CI; 2.48–31.16, p < 0.001). This prognostic effect remained significant in a multivariate analysis adjusted for age, gender and renal function (HR 8.5; 95 % CI; 1.99–36.14, p = 0.004; Fig. 2c). Furthermore, the predictive role of Ang-2 was shown to be independent of NT-pro BNP, hsTnT and cystatin C GFR (HR 9.97; 95 % CI; 2.64–37.68, p < 0.001). Table 3 summarizes the results of the two regression models.
Discussion
In the pathophysiology of acute heart failure and subsequent cardiogenic shock, loss of vascular integrity plays a central role, initiating and perpetuating a downward spiral towards the development of multiorgan dysfunction syndrome [2, 18]. The Ang-Tie receptor ligand system is a pivotal regulator of vascular function [5, 6, 13, 19, 20]. Its mediator Ang-2 promotes vascular leakage [5] and could be involved in oedema formation. In previous studies, we have shown a prognostic impact of Ang-2 in patients with cardiogenic shock (CS) [17]. Herein, we show that this also holds true for patients with ADHF. Our data indicate (1) profoundly increased Ang-2 concentrations, (2) a relationship in the presence of peripheral oedema and NYHA class and (3) a negative prognostic impact of Ang-2 at discharge in patients with ADHF.
Angiopoietin-2 impairs endothelial integrity [5–7] and represents a marker for endothelial dysfunction and organ injury in acute lunge injury, sepsis, and cardiogenic shock [11–13]. Ang-2 levels are significantly elevated compared to healthy controls and related to disease severity in patients with stable chronic heart failure [14, 15]. Chong et al. showed, in a relatively small number of patients (n = 39) with acute heart failure, that Ang-2 concentrations were increased compared to controls [14]. In a study including 103 patients with acute myocardial infarction, Ang-2 concentrations were significantly higher in patients with compared to those without heart failure and represented an independent predictor for the incidence of heart failure [16]. Our study shows the increase of Ang-2 in the setting of ADHF in a larger cohort of patients. Herein, Ang-2 concentrations were elevated more than twofold in ADHF patients compared to HC. Interestingly, we observed increased Ang-2 levels in patients compared to those presenting without peripheral oedema. Since Ang-2 has been identified as a marker of capillary leakage, these results suggest that oedema in acute decompensated heart failure might not solely be mediated by the increased hydrostatic pressure. Rather, it might at least partly reflect a systemic endothelial barrier dysfunction involving Ang-2.
Furthermore, we observed increased Ang-2 levels in more (NYHA class III and IV) compared to less symptomatic patients (NYHA class I and II). This is in accordance with the findings of a smaller study conducted in patients with stable chronic HF, which showed a correlation between Ang-2 and the functional capacity (6 min walk distance, peak oxygen consumption) of the patients [15]. These results might suggest that tissue ischemia induced by the reduced cardiac output and/or the consecutive maladaptive mechanisms might be the trigger for the Ang-2 increase, promoting the above-mentioned vicious circle. This hypothesis is corroborated by in vitro studies showing that the exposure of endothelial cells to hypoxia induced Ang-2 expression [10]. However, the exact pathophysiological mechanism remains to be elucidated.
Prior studies have described a prognostic role of Ang-2 and mortality in sepsis [11–13, 21–23] as well as in cardiogenic shock [17]. In the present study, Ang-2 levels at admission were numerically elevated in non-survivors compared to survivors. However, this difference was much more pronounced and reached statistical significance only at the time of discharge. This finding is consistent with other investigations, which have also shown an association between the mortality and Ang-2 levels measured over time [13, 17, 23]. Importantly, we found a significant difference regarding the course of Ang-2 concentrations between admission and discharge with respect to mortality. While survivors were characterized by a decrease in Ang-2 over time, this decrease was absent in non-survivors. In the latter, we even observed a trend towards an increased Ang-2 concentration at discharge. These findings suggest that Ang-2 levels might be used as a marker of successful recompensation in ADHF patients. The prognostic relevance of increased Ang-2 concentrations at discharge is further corroborated by our Kaplan–Meier analyses revealing the worst prognosis for the group of patients presenting with low Ang-2 levels at admission and high Ang-2 levels at discharge and the ROC analyses. Furthermore, Ang-2 had a slightly higher AUC compared to NT-pro BNP and interestingly, the combination of Ang-2 and NT-pro BNP had a higher diagnostic accuracy than both parameters alone with an AUC of more than 0.9. The missing statistical significance might be at least partially explained by the low event rates in the examined population.
The negative prognostic effect of increased Ang-2 concentrations remained significant in a cox regression analysis adjusted for baseline risk (age, gender, renal function). Furthermore, its prognostic role was shown to be independent of the most important established prognosticators in ADHF, namely biomarkers of myocardial stress (hsTnT, NT-pro BNP) and renal function.
However, our study has some limitations. First and most importantly, we observed a very low event rate. In this setting, the results of the multivariate analyses should be interpreted with caution and may only be hypothesis generating. However, in our opinion, the results of this study strongly indicate an important prognostic role of Ang-2 in ADHF. Therefore, larger studies with a higher number of endpoints should be performed to investigate this issue. Furthermore, we did not record the presence or absence of oedema at discharge of the patients. This hampers further assessment of the quality of Ang-2 as a marker for recompensation.
In conclusion, Ang-2 concentrations are significantly increased in patients with ADHF compared to healthy controls. Furthermore, they are related in the presence of peripheral oedema as well as to NYHA functional class. Increased Ang-2 concentrations at discharge are predictors of a poor outcome in univariate analysis, and multivariate analysis suggests that their negative predictive value might be independent from baseline risk and from established biomarkers and prognosticators in ADHF. Thus, Ang-2 might be used as a marker of disease severity, as a measure for clinical recompensation, and potentially as a promising target in patients with ADHF.
References
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, Task Force for the D, Treatment of A, Chronic Heart Failure of the European Society of C, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, McDonagh T, Sechtem U, Bonet LA, Avraamides P, Ben Lamin HA, Brignole M, Coca A, Cowburn P, Dargie H, Elliott P, Flachskampf FA, Guida GF, Hardman S, Iung B, Merkely B, Mueller C, Nanas JN, Nielsen OW, Orn S, Parissis JT, Ponikowski P, Guidelines ESCCfP (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 14(8):803–869. doi:10.1093/eurjhf/hfs105
Reynolds HR, Hochman JS (2008) Cardiogenic shock: current concepts and improving outcomes. Circulation 117(5):686–697. doi:10.1161/CIRCULATIONAHA.106.613596
van Meurs M, Kumpers P, Ligtenberg JJ, Meertens JH, Molema G, Zijlstra JG (2009) Bench-to-bedside review: Angiopoietin signalling in critical illness—a future target? Crit Care 13(2):207. doi:10.1186/cc7153
Kim I, Kim HG, So JN, Kim JH, Kwak HJ, Koh GY (2000) Angiopoietin-1 regulates endothelial cell survival through the phosphatidylinositol 3′-Kinase/Akt signal transduction pathway. Circ Res 86(1):24–29
Fiedler U, Reiss Y, Scharpfenecker M, Grunow V, Koidl S, Thurston G, Gale NW, Witzenrath M, Rosseau S, Suttorp N, Sobke A, Herrmann M, Preissner KT, Vajkoczy P, Augustin HG (2006) Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat Med 12(2):235–239. doi:10.1038/nm1351
Fiedler U, Scharpfenecker M, Koidl S, Hegen A, Grunow V, Schmidt JM, Kriz W, Thurston G, Augustin HG (2004) The Tie-2 ligand angiopoietin-2 is stored in and rapidly released upon stimulation from endothelial cell Weibel-Palade bodies. Blood 103(11):4150–4156. doi:10.1182/blood-2003-10-3685
Scharpfenecker M, Fiedler U, Reiss Y, Augustin HG (2005) The Tie-2 ligand Angiopoietin-2 destabilizes quiescent endothelium through an internal autocrine loop mechanism. J Cell Sci 118(4):771–780. doi:10.1242/Jcs.01653
Ong T, McClintock DE, Kallet RH, Ware LB, Matthay MA, Liu KD (2010) Ratio of angiopoietin-2 to angiopoietin-1 as a predictor of mortality in acute lung injury patients. Crit Care Med 38(9):1845–1851. doi:10.1097/CCM.0b013e3181eaa5bf
Kumpers P, Nickel N, Lukasz A, Golpon H, Westerkamp V, Olsson KM, Jonigk D, Maegel L, Bockmeyer CL, David S, Hoeper MM (2010) Circulating angiopoietins in idiopathic pulmonary arterial hypertension. Eur Heart J 31(18):2291–2300. doi:10.1093/eurheartj/ehq226
Pichiule P, Chavez JC, LaManna JC (2004) Hypoxic regulation of angiopoietin-2 expression in endothelial cells. J Biol Chem 279(13):12171–12180. doi:10.1074/jbc.M305146200
Kumpers P, Lukasz A, David S, Horn R, Hafer C, Faulhaber-Walter R, Fliser D, Haller H, Kielstein JT (2008) Excess circulating angiopoietin-2 is a strong predictor of mortality in critically ill medical patients. Crit Care 12(6):R147. doi:10.1186/cc7130
Orfanos SE, Kotanidou A, Glynos C, Athanasiou C, Tsigkos S, Dimopoulou I, Sotiropoulou C, Zakynthinos S, Armaganidis A, Papapetropoulos A, Roussos C (2007) Angiopoietin-2 is increased in severe sepsis: correlation with inflammatory mediators. Crit Care Med 35(1):199–206. doi:10.1097/01.CCM.0000251640.77679.D7
Ricciuto DR, dos Santos CC, Hawkes M, Toltl LJ, Conroy AL, Rajwans N, Lafferty EI, Cook DJ, Fox-Robichaud A, Kahnamoui K, Kain KC, Liaw PC, Liles WC (2011) Angiopoietin-1 and angiopoietin-2 as clinically informative prognostic biomarkers of morbidity and mortality in severe sepsis. Crit Care Med 39(4):702–710. doi:10.1097/CCM.0b013e318206d285
Chong AY, Caine GJ, Freestone B, Blann AD, Lip GY (2004) Plasma angiopoietin-1, angiopoietin-2, and angiopoietin receptor tie-2 levels in congestive heart failure. J Am Coll Cardiol 43(3):423–428. doi:10.1016/j.jacc.2003.08.042
Eleuteri E, Di Stefano A, Tarro Genta F, Vicari C, Gnemmi I, Colombo M, Mezzani A, Giannuzzi P (2011) Stepwise increase of angiopoietin-2 serum levels is related to haemodynamic and functional impairment in stable chronic heart failure. Eur J Cardiovasc Prev Rehabil 18(4):607–614. doi:10.1177/1741826710389410
Chen S, Guo L, Chen B, Sun L, Cui M (2013) Association of serum angiopoietin-1, angiopoietin-2 and angiopoietin-2 to angiopoietin-1 ratio with heart failure in patients with acute myocardial infarction. Exp Ther Med 5(3):937–941. doi:10.3892/etm.2013.893
Link A, Pöss J, Rbah R, Barth C, Feth L, Selejan S, Böhm M (2013) Circulating angiopoietins and cardiovascular mortality in cardiogenic shock. Eur Heart J 34(22):1651–1662. doi:10.1093/eurheartj/ehs487
Werdan K, Russ M, Buerke M, Delle-Karth G, Geppert A, Schondube FA, German Cardiac S, German Society of Intensive C, Emergency M, German Society for T, Cardiovascular S, German Interdisciplinary Association of Intensive C, Emergency M, Austrian Society of C, German Society of A, Intensive Care M, German Society of Preventive M, Rehabilitation (2012) Cardiogenic shock due to myocardial infarction: diagnosis, monitoring and treatment: a German-Austrian S3 Guideline. Dtsch Arztebl Int 109(19):343–351. doi:10.3238/arztebl.2012.0343
Fiedler U, Augustin HG (2006) Angiopoietins: a link between angiogenesis and inflammation. Trends Immunol 27(12):552–558. doi:10.1016/j.it.2006.10.004
Thurston G, Rudge JS, Ioffe E, Zhou H, Ross L, Croll SD, Glazer N, Holash J, McDonald DM, Yancopoulos GD (2000) Angiopoietin-1 protects the adult vasculature against plasma leakage. Nat Med 6(4):460–463. doi:10.1038/74725
van der Heijden M, van Nieuw Amerongen GP, Koolwijk P, van Hinsbergh VW, Groeneveld AB (2008) Angiopoietin-2, permeability oedema, occurrence and severity of ALI/ARDS in septic and non-septic critically ill patients. Thorax 63(10):903–909. doi:10.1136/thx.2007.087387
Siner JM, Bhandari V, Engle KM, Elias JA, Siegel MD (2009) Elevated serum angiopoietin 2 levels are associated with increased mortality in sepsis. Shock 31(4):348–353. doi:10.1097/SHK.0b013e318188bd06
van der Heijden M, Pickkers P, van Nieuw Amerongen GP, van Hinsbergh VW, Bouw MP, van der Hoeven JG, Groeneveld AB (2009) Circulating angiopoietin-2 levels in the course of septic shock: relation with fluid balance, pulmonary dysfunction and mortality. Intensive Care Med 35(9):1567–1574. doi:10.1007/s00134-009-1560-y
Acknowledgements
We thank Nina Rebmann for excellent technical assistance.
Conflict of interest
JP, CU, PE, GF, SE, MB, AL have no conflicts of interest to declare. IK received speaker’s honoraria from Vifor Pharma, Boehringer Ingelheim and Novartis. FM is supported by Deutsche Hochdruckliga and Deutsche Gesellschaft für Kardiologie.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Pöss and C. Ukena contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Pöss, J., Ukena, C., Kindermann, I. et al. Angiopoietin-2 and outcome in patients with acute decompensated heart failure. Clin Res Cardiol 104, 380–387 (2015). https://doi.org/10.1007/s00392-014-0787-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0787-y