Abstract
Background
We compared the long-term prognostic value of coronary artery calcium (CAC) scanning, coronary computed tomographic angiography (CCTA), and stress single-photon emission computed tomography myocardial perfusion imaging (MPI) in patients with suspected coronary artery disease (CAD).
Methods and Results
A total of 164 patients were studied. CAC score was measured according to the Agatston method and patients were categorized into 3 groups (0, 1-300, and >300). The following events were recorded: cardiac death, nonfatal infarction, and unstable angina requiring revascularization. Follow-up was 95% complete during a mean period of 82 ± 34 months. During follow-up, 22 events occurred (14% cumulative event rate). Event-free survival decreased with worsening of CAC score category (P < .001) and it was worse (P < .001) in patients with significant CAD (≥50% stenosis) and in those with stress-induced ischemia (summed difference score >2). At multivariable analysis, CAC (P = .001) and ischemia (P = .012) were independent predictors of events. MPI data added prognostic information to a model including clinical variables, CAC and CCTA findings, increasing the global Chi-square from 36.2 to 41.9 (P = .013). The decision curve analyses in patients with CAC score >0 indicate that the prognostic model including MPI resulted in a higher net benefit across a wide range of decision threshold probabilities.
Conclusions
CAC and MPI, but not CCTA, are independent predictors of cardiac events. Stress MPI appears to improve risk stratification over clinical variables, CAC scanning and CCTA findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current approach to coronary artery disease (CAD) is based on anatomic and functional imaging.1 Coronary artery calcium (CAC) scoring, coronary artery computed tomography angiography (CCTA), and stress myocardial perfusion imaging (MPI) are commonly used for risk stratification and treatment choice in patients with suspected CAD. In particular, measurement of CAC is considered reasonable for cardiovascular risk assessment in asymptomatic adults at intermediate risk.2 On the other hand, prior studies evaluating the value of CCTA and MPI in patients with stable CAD found comparable results in terms of long-term outcomes.3-5 It has also been showed that CAC score and stress MPI provide independent and complementary prediction of cardiac risk.6,7 However, cardiac CT and MPI provide information regarding different aspects of the disease, atherosclerotic and ischemic changes, respectively. Therefore, these techniques complement each other. Yet, to date there has been no comparison of CAC scanning, CCTA and stress MPI for risk stratification in the same cohort of patients. The purpose of this study was to compare the long-term prognostic value of CAC, CCTA, and stress MPI in patients with suspected CAD. The incremental prognostic value of each technique compared with clinical variables was also evaluated.
Methods
Patients
From December 2006 to March 2010, we prospectively enrolled 164 consecutive outpatients (mean age 62 ± 12 years, male gender 67%) at low to intermediate pre-test likelihood of CAD undergoing cardiac CT and stress MPI within one month from each other as part of their diagnostic program. The treating physician ordered the two tests based on clinical grounds. For each patient, the presence of coronary risk factors and angina symptoms was noted. Hypertension was defined as a blood pressure ≥140/90 mm Hg or the use of anti-hypertensive medication. Dyslipidemia was defined as total cholesterol level ≥6.2 mmol/L or treatment with cholesterol lowering medication. Patients were classified as having diabetes if they were receiving treatment with oral hypoglycemic drugs or insulin. Pre-test probability of CAD was calculated by extended Diamond-Forrester model.8 The probability of CAD was analyzed as aggregate descriptors of the following clinical data: age, gender, hypertension, diabetes, dyslipidemia, smoking history, and angina symptoms. Pre-test probability of CAD was considered low when <.15, intermediate between .15 and .85, and high when >.85. Exclusion criteria were documented history of CAD defined as previous percutaneous coronary intervention, coronary artery bypass graft surgery or myocardial infarction, coronary revascularization performed within 2 months after imaging tests. Patients with atrial fibrillation, pacemaker or prosthetic valve, iodine allergy, severe loss of renal function, symptomatic asthma, and pregnancy were also excluded. All patients gave written informed consent to the study protocol.
CT Imaging
All patients were scanned with a 64-slice CT (Lightspeed VCT, GE Healthcare, Milwaukee, WI, USA). Patients with heart rate >65 bpm received intravenous beta-blockers (5-10 mg atenolol). First, patients underwent non-enhanced prospective electrocardiographic (ECG) gated sequential scan to measure the calcium score. Thereafter, patients were injected with 60-80 mL of contrast medium (Iomeron 400, Bracco, Milan, Italy) in an antecubital vein at a high flow rate (5 mL/s) followed by a saline flush and coronary CT angiography was performed by using retrospective ECG gating with ECG-based tube current modulation. The collimation was 64 × 9 × .625 mm; gantry rotation time was 350 ms, tube current was 600-mA, and voltage was 100-120 kV, depending on patient size. Synchronization of the scan with contrast medium arrival was achieved by using the bolus tracking technique (region of interest in ascending aorta) with an increment of 100 Hounsfield units (HU) relative to baseline value.9 Axial reconstructions were transferred to a dedicated workstation (Advantage Workstation, GE Healthcare, Milwaukee, WI, USA) for post-processing and subsequent analysis. At CAC score analysis calcium was defined as the presence of at least 3 contiguous pixels with a density >130 HU. The total calcium burden in the coronary arteries was quantified based on the scoring algorithm proposed by Agatston et al.10 and predefined calcium score categories (0, 1-300, and >300) were used.11 Axial images, multiplanar reconstructions, and curved multi planar reformations were used for coronary evaluation. Two experienced cardiac radiologists who were blinded each other and unaware of the clinical history of the patients independently assessed CTCA images. In the case of disagreement (12% of the scans), a consensus decision was reached after a joint reading session. The coronary arteries were divided into 16 segments according to the modified American Heart Association classification.12 Coronary atherosclerotic lesions were quantified for stenosis by visual estimation. Stenoses were categorized as non-significant (<50% luminal narrowing) and significant (≥50% luminal narrowing). Modified Duke CAD index, an angiographic score integrating proximal CAD, plaque extent, and left main disease, was also constructed.13
MPI
All patients underwent same-day Tc-99 m sestamibi exercise stress and rest MPI according to the recommendations of the European Association of Nuclear Medicine and European Society of Cardiology,14 as previously described in detail.15 In all patients, beta-blocking medications and calcium antagonists were withheld for 48 h and long-acting nitrates for 12 h before testing. Imaging was performed using a dual-head rotating gamma camera (E.CAM, Siemens Medical Systems, Hoffman Estates, IL, USA) equipped with a low-energy, high-resolution collimator and connected with a dedicated computer system. No attenuation or scatter correction was used. An automated software program (e-soft, 2.5, QGS/QPS, Cedars-Sinai Medical Center, Los Angeles, CA) was used to calculate the scores incorporating the extent and severity of perfusion defects, using standardized segmentation of 17 myocardial regions.16 Briefly, this commercial package determines reconstruction limits for the projection dataset, reconstruct the projection images into transaxial images using standard filtered back projection, and then reorient the transaxial images into short-axis images. LV contours were checked visually and manually adjusted if the computer-generated automatic contours were found to be incorrect. Quantitative defect extent and severity were defined from sex-specific normal limits, and summed stress score was obtained by adding the scores of the 17 segments (0 = normal to 4 = absent perfusion) of the stress images. A similar procedure was applied to the resting images to calculate the summed rest score. The summed difference score (SDS) represents the difference between the stress and rest scores and is used as an index of ischemic burden: SDS < 2, no ischemia; 2-6, mild ischemia; >6, moderate-severe ischemia.17 CCTA and MPI images were also analyzed combined with regard to morphologically significant lesions (≥50%) and reversible perfusion defects. Patients were assigned to one of the following three categories: (1) matched: reversible MPI defect in a territory subtended by a coronary artery with a significant stenosis at CCTA; (2) unmatched: any unmatched pathological finding from CCTA and/or MPI; and (3) normal: normal CCTA or any luminal narrowing <50% and no defect by MPI.
Follow-up Data
Patient follow-up was obtained by use of a questionnaire that was assessed by a phone call to all patients and general practitioners or cardiologists and by review of hospital or physicians’ records by individuals blinded to the patient’s test results. The outcome was a composite end point of cardiac death, nonfatal myocardial infarction, or unstable angina requiring coronary revascularization whichever occurred first. The cause of death was confirmed by review of death certificate, hospital chart, or physician’s records. Two physicians reviewed each death, rescreened medical records when appropriate, and resolved disparity by consensus. Death was considered to be of cardiac origin if the primary cause was defined as acute myocardial infarction, congestive heart failure, valvular heart disease, sudden cardiac death, cardiac interventional/surgical procedure related. Myocardial infarction was defined when ≥2 of the following 3 criteria were met: chest pain or equivalent symptom complex, positive cardiac biomarkers, or typical electrocardiographic changes.18 Two patients experiencing noncardiac death and four undergoing late elective revascularization not due to unstable angina were censored at the time of death or at the time of revascularization, respectively. The date of the last examination or consultation was used to determine the length of follow-up.
Statistical Analysis
Continuous data are expressed as mean ± standard deviation and categorical data as percentage. Comparison between groups was performed with unpaired t test and Chi-square test as appropriate. A P value < .05 was considered statistically significant. The ln(CAC + 1) score transformation was used to adjust for the rightward skew of the data and to reduce heteroscedasticity. Survival analysis was performed by univariable and multivariable Cox proportional hazard regression analysis. Only variables showing a P value < .01 at univariable analysis were considered for multivariable analysis. Annualized event rates were expressed as the number of patients having event as a proportion of the number of patients at risk divided by the number of patient-years follow-up. Event-free survival curves were obtained by the Kaplan-Meier method and compared with the log-rank test. The incremental prognostic value of clinical data and imaging findings was assessed considering variables in hierarchical order. The estimation of the potential additive value of SDS over the model including pre-test probability of CAD, ln(CAC + 1) and modified Duke CAD index was also assessed comparing the clinical net benefit curves obtained with decision curve analysis.19,20 The usefulness of SDS in reducing the number of false positive at the same number of true positive prediction was also evaluated and graphically represented. All the analyses were performed using STATA version 14.0 for Windows (StataCorp LP, College Station, TX).
Results
Patient Characteristics and Outcome
Of the 164 patients enrolled, follow-up data were not available for 9 patients (5%). The mean age of patients lost at follow-up was 63 ± 10 years and the prevalence of cardiovascular risk factors comparable to those of the 156 patients with available follow-up data. The median follow-up was 82 ± 34 months. During follow-up, 22 events occurred (14% cumulative event rate). The events were cardiac death in 4 patients, nonfatal myocardial infarction in 2 and unstable angina requiring revascularizations in 16. In the overall study population, 80 (51%) patients were at low and 76 (49%) at intermediate pre-test likelihood of CAD.
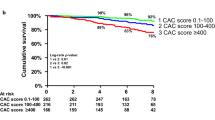
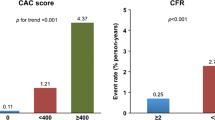
Clinical characteristics and imaging findings of patients with and without events are reported in Table 1. Coronary calcium score, extent and severity of CAD, and SDS were significantly higher in patients with events than in those without. Among patients with events, 15 (68%) had stress-induced ischemia compared with 35 (26%) without events (P < .001). In particular, stress-induced ischemia was mild in 13 and moderate-severe in 2 patients with events, and mild in 27 and moderate-severe in 8 patients without events. The prevalence of significant CAD by CCTA and stress-induced ischemia by MPI in each CAC score category is depicted in Figure 1. The event-free survival curves according to calcium score category, CAD severity and stress-induced ischemia are reported in Figure 2. As showed, event-free survival decreased with worsening of CAC score category (P for trend <.001) and it was worse in patients with significant CAD (P < .001) and in those with stress-induced ischemia (P < .001). Of note, no patients with calcium score of 0 suffered events at follow-up. When these patients were excluded from the analysis, the most favorable event-free survival was found in the normal followed by the unmatched group (unmatched pathological finding from CCTA and/or MPI), whereas the matched group (reversible MPI defect in a territory subtended by a coronary artery with a significant stenosis at CCTA) had the most unfavorable outcome (P for trend <.001) (Figure 3).
Event-free survival curves by Kaplan-Meier analysis in patients with CAC score >0 assigned to one of the following three categories: (1) matched: reversible MPI defect in a territory subtended by a coronary artery with a significant stenosis at CCTA; (2) unmatched: any unmatched pathological finding from CCTA and/or MPI; and (3) normal: normal CCTA or any luminal narrowing <50% and no defect by MPI
Predictors of Events
Significant predictors of events at univariable and multivariable Cox regression analyses are reported in Table 2. To eliminate redundancy and avoid model overfitting, only calcium score, SDS, and Duke CAD index were included in the multivariable model. As shown, calcium score (P = .001) and SDS (P = .012) were independent predictors of events. The results of incremental analysis are reported in Figure 4. Stress-induced ischemia added prognostic information to a model including in hierarchical order clinical variables, CAC score and CCTA findings, increasing the global Chi-square from 36.2 to 41.9 (P = .013). Conversely, CCTA data did not provide incremental prognostic information over the model including clinical data, CAC score, and MPI findings (global Chi square from 38.9 to 41.9, P = .075).
Clinical Benefit
The decision curve analyses in patients with CAC score >0 indicate that the prognostic model including MPI resulted in a higher net benefit across a wide range of decision threshold probabilities (approximately 25% to 50% risk of cardiac events) (Figure 5). As example, after 60 months of follow-up, using an event-free survival probability of 40% as a threshold, the net benefit of the full model was .05, which is superior to .02 for the model without MPI. The net benefit increase of .03 has a ready clinical interpretation, indicating that including MPI in the model is the equivalent of a strategy that found 3 events per hundred patients after 60 months of follow-up without increasing the number false positive event. Conversely, at the same probability threshold of 40%, the net reduction in false positive is about 63 per 100 patients for the model including MPI compared to 58 per 100 patients for the model without (Figure 4). Thus, at this threshold, including MPI in the model is the equivalent of a strategy that reduced the false positive rate of 5% without missing the prediction of any cardiac events.
(A) Decision curves graphically representing net benefit (y-axis) for the model without (dashed orange line) and with (solid green line) MPI data in a range of decision threshold probabilities (x-axis) in patients with CAC score >0. The blue (treat all) and purple (treat none) solid lines represent making the same decision in all patients. (B) Reduction in false positive rate for the model without (dashed orange line) and with (solid green line) MPI data
Discussion
To the best of our knowledge, this is the first study comparing the long-term prognostic value of CAC scanning, CCTA and stress MPI in the same subjects with suspected CAD. We found that CAC and MPI, but not CCTA, are independent predictors of cardiac events. In addition, functional data by stress MPI improve risk stratification over clinical variables, CAC scanning and CCTA findings.
CAC score provides a quantitative measurement of the overall coronary atherosclerotic burden21 and is a strong predictor of cardiac events. The prognostic value of the CAC score has been consistently found in several studies. A zero CAC score is a consistent predictor of very low risk for cardiac events22,23 while event rates increase incrementally according to CAC score among those with abnormal CAC scans.24,25 Moreover, CAC scanning provides incremental information for predicting outcomes when considering all other available clinical information. In a large study population, CAC scanning has been shown to provide strong net reclassification improvement for the prediction of cardiac events, far outweighing that provided by other potential screening tests for CAD.26 CCTA and MPI are alternatively used in clinical practice, but the choice of the most appropriate prognostic approach is still debated. The prognostic value of MPI and CCTA for the occurrence of hard events is similar, while CCTA is more associated with events when coronary revascularization is considered.5 CCTA has a high negative predictive value for suspected CAD and a high prognostic value in patients with low to intermediate probability of CAD while MPI leads the coronary intervention, by detecting ischemia and assessing the severity of CAD.27-29 The results of the present study indicate that event-free survival decreased with worsening of CAC score category and it was worse in patients with significant CAD and in those with stress-induced ischemia. Noteworthy, no patients with calcium score of 0 suffered events at follow-up. When only patients with CAC > 0 were considered, the most favorable event-free survival was found in the normal followed by the unmatched group, whereas the matched group had the most unfavorable outcome. These findings suggest that combined anatomical and functional assessment may allow improved risk stratification in patients with suspected CAD.
The relationship between CAC score and coronary vascular function has not been fully investigated. Recently, Assante et al.30 in a large cohort of patients with suspected CAD and normal myocardial perfusion found that CAC provides incremental information over established CAD risk factors for predicting coronary vascular dysfunction. Chang et al.6 showed, in a population of 1175 asymptomatic subjects that underwent both CAC determination and stress MPI imaging, that CAC and MPI are independent and complementary in prediction of cardiac events over a follow-up of 7 years. Of note, we found that CAC and stress-induced ischemia were independent predictors of events also including CCTA findings in the multivariable Cox regression analysis. Chang et al.6 proposed to perform CAC scanning in patients at intermediate or high clinical risk for CAD with normal SPECT result. Our findings show that a CAC of 0 boasts a great value in identification of patients at low probability of cardiac events, suggesting to perform further evaluation only in patients with CAC > 0.
The decision curve analysis indicates that the incremental prognostic value of MPI data over clinical variables, CAC and CCTA findings translates into a clinically relevant benefit that could change clinical decision making. The prognostic model including MPI resulted in a higher net benefit across a wide range of decision threshold probabilities including the range between 25% and 50% risk of cardiac events.
Some limitations of our study should be acknowledged. First, our study was performed at a single center in a small number of patients at low to intermediate pre-test likelihood of CAD, which makes it uncertain whether results will be equally applicable to general clinical practice. In addition, according to the average low cardiac risk of the population, the events were weighted towards the “soft” event of unstable angina with revascularization. Studies in larger series are warranted to confirm our results.
New Knowledge Gained
CAC and MPI, but not CCTA, are independent predictors of cardiac events. The decision curve analyses in patients with CAC score >0 indicate that the prognostic model including MPI resulted in a higher net benefit across a wide range of decision threshold probabilities. These findings also confirm that the major predictors of events are the extent of atherosclerosis (best assessed with CAC) and extent of myocardial ischemia (as assessed by MPI or other imaging modalities).
Conclusion
The results of this study suggest that patients with suspected CAD without CAC do not need further cardiac imaging investigations. Stress MPI appears to improve risk stratification over clinical variables, CAC scanning, and CCTA findings. Combined information from CCTA and MPI might allow risk stratification in patients with suspected CAD and documented coronary calcium.
Abbreviations
- CAD:
-
Coronary artery disease
- CAC:
-
Coronary artery calcium
- CCTA:
-
Coronary artery computed tomography angiography
- MPI:
-
Myocardial perfusion imaging
- ECG:
-
Electrocardiographic
- HU:
-
Hounsfield units
- SDS:
-
Summed difference score
References
Naya M, Tamaki N. Stress MPI, coronary CTA, and multimodality for subsequent risk analysis. J Nucl Cardiol. 2016;23:198–201.
Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, American College of Cardiology Foundation, American Heart Association, et al. ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;2010:e50–103.
Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. New Engl J Med. 2015;372:1291–300.
Hlatky MA, Shilane D, Hachamovitch R, Dicarli MF, Investigators S. Economic outcomes in the study of myocardial perfusion and coronary anatomy imaging roles in coronary artery disease registry: The SPARC study. J Am Coll Cardiol. 2014;63:1002–8.
Cantoni V, Green R, Acampa W, Petretta M, Bonaduce D, Salvatore M, et al. Long-term prognostic value of stress myocardial perfusion imaging and coronary computed tomography angiography: A meta-analysis. J Nucl Cardiol. 2016;23:185–97.
Chang SM, Nabi F, Xu J, Peterson LE, Achari A, Pratt CM, et al. The coronary artery calcium score and stress myocardial perfusion imaging provide independent and complementary prediction of cardiac risk. J Am Coll Cardiol. 2009;54:1872–82.
Engbers EM, Timmer JR, Ottervanger JP, Mouden M, Knollema S, Jager PL. Prognostic value of coronary artery calcium scoring in addition to single-photon emission computed tomographic myocardial perfusion imaging in symptomatic patients. Circ Cardiovasc Imaging. 2016;9:e003966.
Genders TS, Steyerberg EW, Hunink MG, Nieman K, Galema TW, Mollet NR, et al. Prediction model to estimate presence of coronary artery disease: Retrospective pooled analysis of existing cohorts. BMJ. 2012;344:e3485.
Cademartiri F, Nieman K, van der Lugt A, Raaijmakers RH, Mollet N, Pattynama PM, et al. Intravenous contrast material administration at 16-detector row helical CT coronary angiography: Test bolus versus bolus-tracking technique. Radiology. 2004;233:817–23.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45.
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975;51(4 Suppl):5–40.
Naya M, Murthy VL, Blankstein R, Sitek A, Hainer J, Foster C, et al. Quantitative relationship between the extent and morphology of coronary atherosclerotic plaque and downstream myocardial perfusion. J Am Coll Cardiol. 2011;58:1807–16.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, European Association of Nuclear Medicine (EANM), et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT, CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;2015:1929–40.
Petretta M, Acampa W, Evangelista L, Daniele S, Ferro A, Cuocolo A. Impact of inducible ischemia by stress SPECT (IDIS) investigators. Impact of inducible ischemia by stress SPECT in cardiac risk assessment in diabetic patients: Rationale and design of a prospective, multicenter trial. J Nucl Cardiol. 2008;15:100–4.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–42.
Sharir T, Germano G, Kang X, Lewin HC, Miranda R, Cohen I, et al. Prediction of myocardial infarction versus cardiac death by gated myocardial perfusion SPECT: Risk stratification by the amount of stress-induced ischemia and the post-stress ejection fraction. J Nucl Med. 2001;42:831–7.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Joint ESC/ACCF/AHA/WHF task force for the universal definition of myocardial infarction. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35.
Vickers AJ, Elkin EB. Decision curve analysis: A novel method for evaluating prediction models. Med Decis Making. 2006;26:565–74.
Vickers AJ, Cronin AM, Elkin EB, Gonen M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak. 2008;8:53.
Rumburger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157–62.
Budoff MJ, McClelland RL, Nasir K, Greenland P, Kronmal RA, Kondos GT, et al. Cardiovascular events with absent or minimal coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J. 2009;158:554–61.
Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, et al. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging. 2009;2:692–700.
Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: Observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–70.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45.
Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–95.
Abdulla J, Asferg C, Kofoed KF. Prognostic value of absence or presence of coronary artery disease determined by 64-slice computed tomography coronary angiography a systematic review and meta-analysis. Int J Cardiovasc Imaging. 2011;27:413–20.
Hulten EA, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC. Prognostic value of cardiac computed tomography angiography: A systematic review and meta-analysis. J Am Coll Cardiol. 2011;57:1237–47.
Naya M, Tamaki N. Stress MPI, coronary CTA, and multimodality for subsequent risk analysis. J Nucl Cardiol. 2016;23:198–201.
Assante R, Zampella E, Arumugam P, Acampa W, Imbriaco M, Tout D, et al. Quantitative relationship between coronary artery calcium and myocardial blood flow by hybrid rubidium-82 PET/CT imaging in patients with suspected coronary artery disease. J Nucl Cardiol 2016 Jan 15. [Epub ahead of print].
Disclosure
The authors have indicated that they have no financial conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-016-0719-5.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nappi, C., Nicolai, E., Daniele, S. et al. Long-term prognostic value of coronary artery calcium scanning, coronary computed tomographic angiography and stress myocardial perfusion imaging in patients with suspected coronary artery disease. J. Nucl. Cardiol. 25, 833–841 (2018). https://doi.org/10.1007/s12350-016-0657-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0657-2