Abstract
Aims
The recommendation for the use of the intra-aortic balloon pump (IABP) as adjunct in patients with cardiogenic shock undergoing primary PCI in current guidelines is controversial. We sought to investigate the use and impact of the outcome of IABP in current practice of percutaneous coronary interventions in Germany.
Methods and results
Between January 2006 and December 2011, a total of 55,008 consecutive patients with acute coronary syndromes undergoing PCI in 41 hospitals were enrolled into the prospective Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte registry. Of these, 22,039 had STEMI and 32,969 had NSTEMI, and cardiogenic shock was observed in 1,435 (6.5 %) and 478 (1.4 %), respectively. Of the total of 1,913 patients with shock, 487 (25.5 %) were treated with IABP. In-hospital mortality with and without IABP was 43.5 and 37.4 %. In the multivariate analysis, the use of IABP was associated with a strong trend for an increased mortality (odds ratio 1.45, 95 % CI 1.15–1.84).
Conclusion
In the current clinical practice in Germany, IABP is used only in one quarter of patients with cardiogenic shock treated with primary PCI. We observed no benefit of IABP on outcome, which supports the findings of the randomized IABP-Shock II trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the use of early revascularization therapy, cardiogenic shock is the major cause of death in patients admitted with acute myocardial infarction and associated with a mortality of around 40–50 % [1–3]. One mechanical measure to improve hemodynamics in cardiogenic shock is the intra-aortic balloon pump (IABP). IABP was introduced in 1968 and improves systemic and coronary diastolic blood pressure and reduces afterload and myocardial work [4]. These effects are believed to improve myocardial recovery during ischemia and reperfusion and, ultimately reduce mortality in patients with cardiogenic shock. Current ESC guidelines support the use of IABP (class 1c recommendation) in patients with cardiogenic shock [5]. However, a recent meta-analysis has questioned the value of IABP, especially in patients with primary PCI [6]. The recent guidelines of the German Cardiac society for cardiogenic shock are neutral regarding the recommendation for IABP in connection with primary PCI for shock [7]. Therefore, we sought to investigate the use of IABP in a large cohort of patients undergoing PCI for cardiogenic shock in Germany.
Methods
The Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte(ALKK) PCI registry
The ALKK PCI registry is a prospective registry that was initiated in 1992 to monitor quality control and contains all consecutive procedures of the participating hospitals on an intention-to-treat basis [8, 9]. Data were obtained by standardized questionnaires in the 41 participating hospitals, including the information about the medical history (prior coronary interventions, CHF, diabetes mellitus, and renal insufficiency) indication for the procedure, the adjunctive antithrombotic therapy, the procedure itself (target vessel, success rate, stent used, etc.), and the complications until hospital discharge. All data were analyzed centrally at the Karl Ludwig Neuhaus Datenzentrum, Ludwigshafen, Germany.
Patient selection
All patients receiving PCI were included on an intention-to-treat basis. We analyzed data of consecutive patients with ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI). For this analysis, we selected patients with cardiogenic shock before the start of the intervention.
Definitions
NSTEMI was diagnosed in the presence of the two following criteria: persistent angina pectoris for ≥20 min and an elevation of troponin T or I. Raised levels were considered those exceeding the upper normal level at the local laboratory at each participating site.
STEMI was diagnosed in the presence of the two following criteria: persistent angina pectoris ≥20 min and ST-segment elevation of 1 mm in ≥2 standard leads or ≥2 mm in ≥2 contiguous precordial leads or the presence of a left bundle branch block. It was later confirmed by the elevation of enzymes (creatinine kinase and its MB isoenzyme, aspartate aminotransferase, and lactic dehydrogenase) to at least twice the normal value.
Cardiogenic shock was diagnosed in patients with systolic blood pressure <90 mmHg, heart rate >100 bpm, and clinical signs of organ hypoperfusion.
Statistical methods
All analyses were performed using the SAS© statistic package, Version 9.1 (Cary, NC, USA). Data are presented as absolute numbers or percentage. Whenever possible, percentages were used to describe patient populations. The frequencies of categorical variables in four age groups were compared by Pearson–Fisher χ2 test and by calculating odds ratios (OR) and 95 % CI. Continuous variables were compared by Mann–Whitney–Wilcoxon test. p values <0.05 were considered significant. (All p values are results of two-tailed tests).
A multivariate regression analysis for independent predictors of inhospital mortality was performed including age, gender, left main PCI, triple vessel disease, diabetes, and renal insufficiency. These values were calculated from the available cases. The computations were performed using the SAS system release 9.1 on a personal computer (SAS Institute, Inc., Cary, NC, USA).
Results
Between January 2006 and December 2011, a total of 55,008 consecutive patients with acute coronary syndromes undergoing PCI in 41 hospitals were enrolled into the registry. Of these, 22,039 had STEMI and 32,969 had NSTEMI, and cardiogenic shock was observed in 1,435 (6.5 %) and 478 (1.4 %), respectively. Of the total 1,913 patients with shock, 487 (25.5 %) were treated with IABP. The rate of shock patients treated with IABP was 26.0 % in patients with STEMI and 22.0 % in patients with NSTEMI, respectively. The rate of the use of IABP per hospital is shown in Fig. 1.
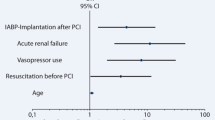
The baseline variables of patients treated with and without IABP are given in Table 1. The angiographic features and procedural details of the patients are shown in Table 2. Thrombus aspiration was used in 30.3 versus 13.2 % of patients with and without IABP. The patients were treated with an intensive antithrombotic therapy (Table 3) with a higher use of GP IIb/IIIA inhibitors and bivalirudin in the IABP group. During PCI, inotropes were given in 81.8 % of patients with and 97.2 % of patients without IABP (p < 0.001), respectively. The inhospital events are shown in Fig. 2. Renal failure requiring dialysis occurred in 6.1 versus 4.7 % (p = 0.4) of the patients. Independent predictors of inhospital mortality are shown in Fig. 3. Here IABP was associated with an increased mortality (odds ratio 1.45, 95 % CI 1.15–1.84).
Discussion
Early revascularization therapy has been shown to improve the outcome of patients with acute myocardial infarction complicated by cardiogenic shock. However, mortality in these patients remains high [3, 10–15]. While current ESC-guidelines recommend the use of IABP in patients with cardiogenic shock [5], the recent shock guidelines of the German cardiac society are neutral in the recommendation [7]. In clinical practice, the utilization rate of IABP is low (15–30 %) [4, 10–14]. In our analysis with data from a large cohort of shock patients from Germany, the use of IABP was 25 % with no difference between the use in STEMI and NSTEMI. We observed large differences in the use of IABP between the hospitals ranging from 0 to 70 %. However, one reason for the overall low utilization rate of IABP in Germany might be that interventionalists are not fully convinced about the beneficial effect of IABP on top of early revascularization therapy. This skepticism is supported by a recent meta-analysis which found no mortality benefit of the IABP in patients with STEMI complicated by cardiogenic shock treated with primary PCI [6], but an increase in major bleeding complications and stroke (Fig. 3).
Until recently, the only randomized clinical trial performed with IABP in primary PCI for shock was small and did not show any differences in the primary surrogate endpoints or any clinical endpoints [15]. Two other trials performed in high-risk patients with STEMI without cardiogenic shock did not show any beneficial effects on the routine use of IABP either [16, 17].
The results of our analysis support these findings. Anything than IABP as adjunct to primary PCI was associated with an adverse outcome. In experimental models and human experience, IABP increased the myocardial perfusion and improved hemodynamics, [18, 19]. Our findings are supported by the results of a larger cohort of patients in the NRMI registry [11]. Here, the use of IABP was associated with an increase in mortality after primary PCI in cardiogenic shock (956/2035 vs. 401/955). The mortality difference remained significant even after the adjustment for confounding factors. The same was true in an analysis of the European Heart Survey of PCI [20] and a very recent analysis of the National Cardiovascular Data Registry in the United States [21]. We can only speculate about the reasons for this increase in mortality. A possibility is that a systemic inflammation response to the device, and another explanationis that the increase in bleeding complications due to local complications at the catheterization insert site.
An interesting finding in our analysis was that patients treated with IABP were more likely to be treated with GP IIb/IIIa inhibitors, bivalirudin, thrombectomy devices, multivessel PCI, and drug-eluting stents. It seems that IABP as an adjunct to PCI is used by more “aggressive” interventionalists using more intense antithrombotic regimens and an approach of more immediate complete revascularization.
Our findings are supporting the results of the recently published IAPB-Shock II trial in which 600 patients with myocardial infarction complicated by cardiogenic shock and intended PCI were randomized to IABP or standard therapy [22]. The primary outcome of 30 day mortality did not differ between the two groups. Although IABP use was safe and not associated with an increase in complications such as sepsis, vascular complications, or bleedings, neither mortality nor any secondary endpoints were improved with IABP use. Secondary endpoints included hemodynamic parameters (blood pressure and heart rate) pre- and post revascularization, serum lactate levels measured every 8 h for 48 h, inflammatory markers, Simplified Acute Physiology Score-II (SAPS-II) measured daily during intensive care treatment, and serial creatinine-level and creatinine-clearance using the Cockcroft-Gault-formula.13 Furthermore, process of care outcomes such as time to hemodynamic stabilization, dose and duration of catecholamine therapy, requirement for renal replacement therapy, length of intensive care unit stay, requirement and length of mechanical ventilation, and requirement for active (percutaneous or surgical) left ventricular assist device implantation or heart transplantation were assessed and did not differ between the two groups.
Limitations
As always in registries a selection bias cannot fully be ruled out. Therefore, even after the adjustment for confounding for baseline variables, we cannot be sure that we were able to adjust for every factor which might have influenced the results.
Conclusions
In current clinical practice in Germany, IABP is used only in one quarter of patients with cardiogenic shock treated with primary PCI. However, we did not observe any hint for a beneficial effect of IABP on outcome, supporting the data of the recently published randomized IABP-Shock II trial. Therefore, IABP should not be considered as a routine treatment in patients with cardiogenic shock and early revascularization therapy.
References
Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM (1999) Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med 340:1162–1168
Hochman JS, Sleeper LA, Webb JG et al (1999) Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med 341:625–634
Zeymer U, Vogt A, Zahn R, Weber MA, Tebbe U, Gottwik M, Bonzel T, Senges J, Neuhaus KL (2004) Predictors of in-hospital mortality in 1333 patients with acute myocardial infarction complicated by cardiogenic shock treated with primary percutaneous coronary intervention (PCI). Eur Heart J 25:322–328
Moulopoulos S, Stamatelopoulos S, Petrou P (1986) Intraaortic balloon assistance in intractable cardiogenic shock. Eur Heart J 7:396–403
Van de Werf F, Bax J, Betriu A et al (2008) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the task force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology. Eur Heart J 23:2909–2945
Sjauw KD, Engstrom AE, Vis MM et al (2009) A systematic review and meta-analysis of intra aortic balloon pump therapy in ST-elevation myocardial infarction: should we change the guidelines? Eur Heart J 30:459–468
Werdan K, Russ M, Buerke M et al (2011) Deutsch-österreichische S3 Leitlinie: infarktbedingter kardiogener Schock—Diagnose, Monitoring und Therapie. Kardiologe 5:166–224
Neuhaus KL (1996) Qualitätssicherung bei Koronararteriendilatation. Dt Ärztebl 93:2642–26444
Zeymer U, Zahn R, Hochadel M et al (2005) Indikationen und Komplikationen bei Herzkatheterdiagnostik und percutaner coronarer Intervention im Jahr 2003. Ergebnisse des Qualitätssicherungs-Registers der Arbeitsgemeinschaft Leitende kardiologische Krankenhausärzte (ALKK). Z Kardiol 94:392–398
Jeger RV, Harkness SM, Ramanathan K et al (2006) Emergency revascularization in patients with cardiogenic shock on admission: a report from the SHOCK trial and registry. Eur Heart J 27:664–670
Hollenberg SM (2004) Recognition and treatment of cardiogenic shock. Semin Respir Crit Care Med 25:661–671
Babaev A, Frederick PD, Pasta DJ et al (2005) Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA 294:448–454
Barron HV, Every NR, Parsons LS et al (2001) The use of intra-aortic balloon counterpulsation in patients with cardiogenic shock complicating acute myocardial infarction: data from the National Registry of Myocardial Infarction 2. Am Heart J 14:933–939
Stone GW, Ohman EM, Miller MF et al (2003) Contemporary utilization and outcomes of intra-aortic balloon counterpulsation in acute myocardial infarction: the benchmark registry. J Am Coll Cardiol 4:1940–1945
Prodzinsky R, Lemm H, Swyter M et al (2010) Intra-aortic balloon counterpulsation in patients withacute myocardial infarction complicated by cardiogenic shock—the prospective, randomised iabp shock trial for attenuation of multi-organ dysfunction syndrome. Crit Care Med 38:152–160
Stone GW, Marsalese D, Brodie BR et al (1997) A prospective, randomized evaluation of prophylactic intraaortic balloon counterpulsation in high risk patients with acute myocardial infarction treated with primary angioplasty. Second primary angioplasty in myocardial infarction (PAMI-II) trial investigators. J Am Coll Cardiol 29(7):1459–1467
Patel M, Smalling R, Thiele H et al (2011) Intra-aortic balloon counterpulsation and infarct size in patients with acute anterior myocardial infarction without shock. JAMA 306:1329–1337
Nanas JN, Moulopoulos SD (1994) Counterpulsation: historical background, technical improvements, hemodynamic and metabolic effects. Cardiology 84:156–167
Ohman EM, Hochman JS (2001) Aortic counterpulsation in acute myocardial infarction: physiologically important but does the patient benefit? Am Heart J 141:889–892
Zeymer U, Bauer T, Hamm CW et al (2011) Use and impact of intra-aortic balloon pump on mortality in patients with acute myocardial infarction complicated by cardiogenic shock: results of the Euro Heart Survey on PCI. EuroIntervention 7:437–441
Curtis JP, Rathore SS, Wang Y et al (2012) Use and effectiveness of intra-aortic balloon pumps among patients undergoing high risk percutaneous coronary intervention: insights from the National Cardiovascular Data Registry. Circ Cardiovasc Qual Outcomes 5:21–30
Thiele H, Zeymer U, Neumann F et al (2012) Intraaortic balloon support for myocardial infarctioncomplicated by cardiogenic shock. N Engl J Med 367(14):1287–1296
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zeymer, U., Hochadel, M., Hauptmann, KE. et al. Intra-aortic balloon pump in patients with acute myocardial infarction complicated by cardiogenic shock: results of the ALKK-PCI registry. Clin Res Cardiol 102, 223–227 (2013). https://doi.org/10.1007/s00392-012-0523-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0523-4